Abstract
Medication adherence has received a great deal of attention over the past several decades; however, its definition and measurement remain elusive. The authors propose a new definition of medication self-management that is guided by evidence from the field of health literacy. Specifically, a new conceptual model is introduced that deconstructs the tasks associated with taking prescription drugs; including the knowledge, skills and behaviors necessary for patients to correctly take medications and sustain use over time in ambulatory care. This model is then used to review and criticize current adherence measures as well as to offer guidance to future interventions promoting medication self-management, especially among patients with low literacy skills.
Taking prescribed medicine has long been recognized as one of the most essential self-care activities performed by patients to promote their health. Medication non-adherence is estimated to cost the U.S. health care system more than $100 billion annually and is linked to more than 125,000 deaths each year (Bosworth et al., 2011; Ernst & Grizzle, 2001). As prescription drug use in the United States continues to rise, the salience of promoting safe, appropriate medication use will only become even more important from a public health perspective (Gu, Dillon, & Burt, 2010). Gaining a concrete understanding of patient roles and responsibilities in outpatient settings is necessary to develop and implement comprehensive strategies to support these behaviors.
Although medication adherence has received an unprecedented amount of attention over the past several decades, its definition and measurement continue to remain elusive (Andrade, Kahler, Frech, & Chan, 2006; Cramer et al., 2008; Farmer, 1999; Haynes et al., 2005; Osterberg & Blaschke, 2005). Debates over the correct terminology to use to describe related behaviors are common (Cramer et al., 2008; Steiner & Earnest, 2000). Consequently, its measurement is often challenging, cumbersome, and costly (Farmer, 1999). As a result, adherence is typically operationalized as a limited set of behaviors, such as filling a prescription or taking doses of a medication. This emphasis has, over time, simplified the way we think of medication use and has directed attention away from the diverse series of steps a patient must take to self-manage medications in ambulatory care (Osterberg & Blaschke, 2005). Simplistic conceptualizations of medication use have become even more problematic as patients are increasingly being prescribed multiple medications (Gu et al., 2010). To take these multidrug regimens safely and appropriately, patients must engage in a number of behaviors that vary in complexity and require an even greater knowledge and skill set (Wolf, Curtis, et al., 2011).
Herein, we propose a new definition of medication use that is guided by relatively recent yet extensive evidence that has emerged from the field of health literacy. Specifically, we introduce a new conceptual model that deconstructs the tasks associated with taking prescription drugs, including the knowledge, skills and behaviors necessary for patients to correctly take medications and to sustain proper use over time in ambulatory care. The field of health literacy in its entirety has made invaluable contributions to this particular topic of research inquiry and to the broader mission of understanding the cognitive and psychosocial demands that are placed on patients as a result of performing requisite health behaviors.
“Unintentional Nonadherence”: The Role of Health Literacy
Evidence suggests that health literacy, or “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions,” plays a significant role in determining how well patients can manage medication regimens in ambulatory care (Institute of Medicine, 2004; Kutner, Greenberg, Jin, Paulsen, & White, 2006). Findings from the health literacy component of the 2003 National Assessment of Adult Literacy indicate that more than 75 million Americans have basic or below basic health literacy skills and are likely to experience difficulties taking prescription drugs safely and appropriately (Kutner et al., 2006). Supporting these results, a substantial number of the more than 500 original investigations examining health literacy skills and health outcomes have targeted medication use, and found a relationship between health literacy and individuals' understanding of prescription instructions, knowledge of their medication's purpose and side effects, ability to correctly use an inhaler or other device, and adherence to a regimen over time (Davis, Wolf, Bass, Thompson, et al., 2006; Kalichman et al., 2008; Muir et al., 2006; Williams, Baker, Honig, Lee, & Nowlan, 1998; Wolf, Davis, Tilson, Bass, & Parker, 2006).
Although the field of health literacy has produced valuable research demonstrating the association between patient literacy skills and a number of medication-related behaviors and outcomes, it has also influenced the way in which health behaviors are conceptualized (DeWalt, Berkman, Sheridan, Lohr, & Pignone, 2004; Institute of Medicine, 2004). The proficiency of an individual to perform a set of self-care behaviors—not just their motivation or activation to manage their personal health—has been given greater recognition with this new field of study. What has followed has been a greater appreciation for the complexity of demands placed on patients by a health care system (Institute of Medicine, 2004). This perspective has shifted the focus from viewing the root cause of problems with nonadherence being the patient (i.e., lack of desire or interest) to the quality and navigability of health systems and the way in which health information is provided to patients (Institute of Medicine, 2004; Parker & Ratzan, 2010).
In addition to enhancing our understanding, the field of health literacy has provided valuable guidance on how interventions should be designed to better account for patient knowledge and skills (Doak, Doak, & Root, 1996; Institute of Medicine, 2004; Pignone, DeWalt, Sheridan, Berkman, & Lohr, 2005). The first step in developing a health literacy–informed intervention is often to deconstruct the health behavior in question (Wolf et al., 2009). This process of breaking down the health behavior enables the researcher to gain a full understanding of its various components. This helps to identify tasks that may present the most difficulty for patients with limited literacy skills as well as to ascertain what information is crucial for patients to engage in the behavior (Doak et al., 1996). In terms of medication use, there are a number of steps patients must take to manage a drug regimen safely and effectively in outpatient care. Understanding these steps can advance the field, better informing future interventions and ensuring that selected measures of medication use are appropriate.
Deconstructing Medication Self-Management: Defining the Model
Numerous terms, including adherence, self-management, compliance, concordance, and persistence, are routinely used to describe patients' use of prescribed medications over time (Cramer et al., 2008; Osterberg & Blaschke, 2005). Although the similarities and differences between each term have been discussed extensively in scientific literature, no one term or definition has been universally accepted (Osterberg & Blaschke, 2005; Steiner & Earnest, 2000). For our conceptual model, we have elected to use the term medication self-management and to define it as “the extent to which a patient takes medication as prescribed, including not only the correct dose, frequency and spacing, but also its continued, safe use over time.”
Considering this definition, it is possible to deconstruct medication self-management to identify the series of steps a patient must take to safely and effectively take their medications in ambulatory care (see Figure 1). Because the focus of this model is on outpatient settings, the model begins after the physician encounter and assumes that the patient has been prescribed a medication that they are responsible for self-administering.
Figure 1.
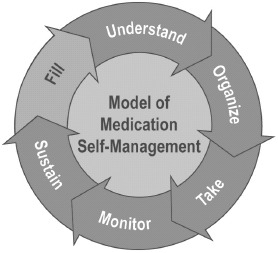
Model of medication self-management. (Color figure available online.)
Step 1: Fill
After the physician encounter, the first step that patients must take to self-manage their Rx regimen is to fill and pick up their prescription. Evidence suggests that this step is often not taken, because approximately a quarter (24%) of prescriptions for new medications are never filled (Fischer et al., 2011; Fischer et al., 2010). Drug cost, poor understanding of why the drug is necessary, and fear of side effects have been cited as potential root causes of this phenomenon; poor provider–patient communication is likely to lead to misunderstandings (Dimatteo, 2004; Golin, DiMatteo, & Gelberg, 1996; Kennedy, Tuleu, & Mackay, 2008). Furthermore, with the recent implementation of e-prescribing, patients are less likely to receive tangible reminders of new medications, such as a written prescription on a prescriber's pad. With fewer prompts, patients may be even less likely to fill new, electronically prescribed medications, at least initially (Bergeron et al., in press).
Step 2: Understand
Once the patient obtains his or her medication, the next step is to learn how to take the drug safely and appropriately. The ability to name, identify, and understand how to take medications in one's medication regimen is a fundamental yet often overlooked part of medication self-management. Patients must be able to track what they are taking, why they are taking it, and how it should be taken to ensure safe and effective use. This has become increasingly difficult given that patients' drugs are frequently changed by prescribers and/or switched for generic alternatives by their insurer (Catz, Kelly, Bogart, Benotsch, & McAuliffe, 2000; Colley & Lucas, 1993). In addition, patients taking complex regimens may have trouble differentiating instructions for each drug (Hoffman & Proulx, 2003). Studies have reported that almost 75% of primary care patients cannot accurately identify their medication regimen, and almost half (46%) misinterpret either the dose (i.e., how many pills to take) or timing (i.e., when to take each dose daily) of a prescription (Davis, Wolf, Bass, Thompson, et al., 2006; Persell, Bailey, Tang, Davis, & Wolf, 2010). Patients with limited health literacy skills have been consistently shown to have greater difficulty understanding medication instructions (Davis, Wolf, Bass, Thompson, et al., 2006; Wolf, Curtis, et al., 2011).
Step 3: Organize
In addition to understanding how to take a medication correctly, it is essential for patients to organize and plan their medication use around their daily schedule. Given that almost 40% of older adults are now taking five or more prescription medications, integrating a new medication into an existing regimen and efficiently organizing this regimen has become increasingly important (Gu et al., 2010). Consolidating medication use is likely to promote adherence. Studies have repeatedly shown a link between dosing frequency and medication use; the greater the dosing frequency, the less likely patients are to consistently take medication (Coleman et al., 2012; Saini, Schoenfeld, Kaulback, & Dubinsky, 2009). Despite this, a recent study demonstrated that many patients unnecessarily overcomplicate medication use by not consolidating a complex regimen so that it can be taken the minimum number of times per day (Wolf, Curtis, et al., 2011). On average, patients in this study dosed a multidrug regimen seven times daily (range = 4–14) when it could have been correctly dosed in four. Perhaps not surprisingly, patients with limited literacy skills were more likely to overcomplicate the hypothetical regimen. Organization and planning is important even among adults taking a single medication; tying medication use to a specific time, place, and/or daily activity supports consistent use (Liu & Park, 2004).
Step 4: Take
Estimates indicate that patients take fewer than 50% of the doses that they are prescribed (Haynes et al., 2005). Forgetfulness, unclear label instructions, side effects, lack of regimen familiarity, lack of symptoms, and loss of interest may be potential determinants of failure to take medications correctly and consistently (Farber et al., 2003; Wu, Moser, Lennie, & Burkhart, 2008). In addition, patients may take less medication than prescribed to conserve their medication supply and reduce drug-related costs (Piette, Heisler, & Wagner, 2004).
Step 5: Monitor
To ensure safe use, patients must be vigilant when taking medicine and be aware of the safety profiles of medicines in their regimen (Institute of Medicine, 2006). Knowledge of potential side effects, risks, and warnings allows patients to connect symptoms to medication use and seek appropriate action before an adverse drug event (Institute of Medicine, 2006). Yet, past studies have found that 54% of patients struggle to comprehend common warnings associated with medicines, and less than 10% routinely attend to this information (Davis, Wolf, Bass, Middlebrooks, et al., 2006; Wolf et al., 2006). In one study, patients with limited health literacy skills were 3.4 times more likely to misunderstand warning labels than were patients with adequate health literacy (Davis, Wolf, Bass, Middlebrooks, et al., 2006).
Step 6: Sustain
The final step of effective medication self-management is to sustain safe and appropriate medication use throughout the duration of the prescription. Despite the importance of this step, evidence suggests that patients often reduce or discontinue use of their medications over time, with deleterious effects (Ho et al., 2006; McHorney & Spain, 2011). Busy lifestyles, unpleasant side effects, and perceptions that a medication is ineffective or no longer necessary are frequent root causes of discontinuation (McHorney & Spain, 2011; Park et al., 1999). In addition, patients may be unaware of the need to refill and continue a medication due to inadequate provider-patient counseling. The evidence on the relationship between health literacy and sustained medication use is mixed; some studies have shown a strong relationship between limited literacy skills and poor adherence, while other have shown no relationship or even an inverse association (Gazmararian et al., 2006; Kalichman et al., 2008; Muir et al., 2006; Paasche-Orlow et al., 2006).
Implications for Measurement
A model of medication self-management, such as the one proposed, provides a far more comprehensive examination of the range of tasks, that individuals must successfully perform to manage their medication regimen. In addition to advancing our understanding, this model can also be used to demonstrate how currently available measures of adherence are inadequate.
For example, direct measures of adherence, which involve drug assays to evaluate the presence of the drug or a metabolite in blood or other bodily fluid, may be the most definitive proof that a drug has been taken (Farmer, 1999; Osterberg & Blaschke, 2005). However, these analyses do not convey exactly when and how a medicine was taken (Osterberg & Blaschke, 2005). Also, these metrics (a) are not available for all drugs and (b) are costly and invasive. Although biologic measures would work well with patients regardless of their literacy skills and may be the gold standard for determining whether a medication has been taken, they provide little to no information on patients' ability to fill, understand, organize, or monitor their medication use. Objective measures, such as pharmacy claims data or pill counts, have the benefit of appearing unbiased and are, in most instances, more feasible and cost effective than direct, biologic measures (Farmer, 1999). Pharmacy records are often used to determine whether patients have completed the fill step on the appropriate date. Although a necessary first step, filling a medication does not equate to taking a medicine safely and appropriately. This is therefore a limited view that does not consider the subsequent tasks that are crucial components of medication self-management. Pill counts involve calculating the expected vs. actual number of pills left in a patient's Rx container. A central assumption of this method is that any missing pills have not only been taken by the patient, but have been taken correctly, as prescribed. This may not be suitable for patients with limited literacy skills, as it assumes that patients can complete the understand step described above (Wolf et al., 2006). Last, electronic monitoring, which has become available through technology such as the Medication Event Monitoring System (MEMS), has become an increasingly popular method of objectively measuring adherence in research settings. MEMS caps electronically record the exact date and time that an Rx container is opened; this methodology assumes that opening a container equates to taking the medication inside. Under these assumptions, MEMS caps can offer detailed reports on when patients take a medication and if they sustain use over time. However, they cannot provide exact information on how much medication, if any, is taken by a patient (i.e., the understand step) or how regimens are managed (i.e., the organize step) unless MEMS caps are placed on all medications in a patient's regimen. It is unfortunate that the cost of MEMS caps is often prohibitive, especially for patients taking multiple drugs; the method is often unsuitable for clinical applications and small research studies (Farmer, 1999).
Next, self-report measures are inexpensive, quick to administer and can be used to identify psychosocial barriers and facilitators affecting patient adherence (Farmer, 1999; Osterberg & Blaschke, 2005). As such, they are the most commonly used method of assessing adherence in clinic settings and are also used in many research studies (Garber, Nau, Erickson, Aikens, & Lawrence, 2004). However, evidence indicates that self-report often overestimates adherence and may be affected by social desirability and recall bias, affecting their usefulness (Garber et al., 2004). A number of self-report measures exist, each with their own strengths and limitations. Medication diaries or self-administered questionnaires have been shown to produce results that are more consistent with objective measures (Garber et al., 2004). However, these may not be suitable for patients with low literacy skills as reading and filling out forms can be particularly challenging for these patients (Institute of Medicine, 2004). Administered questionnaires can vary greatly in terms of questions asked and potential response options; each would need to be reviewed individually to determine their concordance with the model and appropriateness for patients with literacy challenges. Broadly speaking, many common self-report measures examine psychosocial barriers and beliefs about medication-taking (i.e., the Morisky scale, the Medication Adherence Rating Scale); these scales are essentially measuring factors that commonly influence a patient's ability or desire to take or sustain medication use without considering many of the other steps in the model (Morisky, Green, & Levine, 1986; Thompson, Kulkarni, & Sergejew, 2000). Others ask patients to recall the number of pills taken or doses missed for a particular medication, therefore focusing on the take step (Jerant, DiMatteo, Arnsten, Moore-Hill, & Franks, 2008; Wolf, Bennett, Davis, Marin, & Arnold, 2005). The framing of such measures may be problematic, as patients are often unaware of the correct dosage of a medication (i.e., the understand step) and may therefore respond inaccurately to questions about missed doses.
To our knowledge, no existing measure of medication self-management is able to address the full range of tasks patients face in order to successfully manage medication regimens. Given the criticism that has been directed at each of the current measures, many believe that multiple measures should be used to triangulate around the behavior (Institute of Medicine, 2008; Liu et al., 2001). This can be problematic, as methods are not entirely clear on how to reconcile and incorporate the findings from these very diverse tools. And even in this instance, clinically meaningful information pertaining to the nature of self-management problems are difficult to collate, leaving health care providers and researchers alike with insufficient information to formulate effective responses to the problem. For example, cost incentives for refills or switching to generic alternatives may help patients afford to fill their prescriptions, but would not address issues around misunderstanding. Nor would basic education about a new medication accommodate patients' needs to more efficiently consolidate their entire regimen into a daily schedule.
Next Steps: Better-Informed Interventions
We believe that a new assessment is needed, one that not only identifies that a concern exists, but also offers precise detail as to the nature of the medication self-management problem. A more comprehensive assessment of medication self-management would not only be novel in terms of its measurement capabilities, but also could serve as an integral component of a multifaceted intervention strategy. Embedding use of this tool into routine clinical care would help create a signal to a provider that their patient is having difficulty managing their medication regimen and could identify the specific steps of medication self-management that are the most challenging. Given the increasing adoption of electronic health records and available consumer technologies that can be leveraged in health care with ease, we may find ample opportunity to create medication self-management clinical tools that can be well-informed to confirm adequate patient understanding and proper use at routine intervals. The need for an improved medication self-management assessment is coupled with a complimentary need to map difficulties associated with each of the described steps to appropriate intervention responses. As with any proposed recommendation for diagnostic assessment or screening program, these steps need to be properly accompanied with evidence-based intervention strategies that can be prescribed if a problem were identified. Evidence is available describing interventions to respond to problems related to many of the various patient tasks, although additional research is clearly warranted. (Davis et al., 2009; Wolf, Davis, et al., 2011).
Overall, comprehensive, multifaceted strategies are likely needed to promote medication self-management, particularly given the complexity of the behavior. Our conceptual model can help advance thinking around medication use and more fully appreciate the complexity and challenges inherent with medication self-management. This model, in turn, will hopefully offer a fresh perspective and better guide the development of intervention strategies by identifying key targets for intervention (i.e., fill, understand, organize, take, monitor, sustain). Certain strategies have been shown to be efficacious in research studies; for example, improved prescription labeling can increase patient understanding and organizing of drug regimens while reminder systems can assist patients in remembering to fill, take, and sustain medication use (Bailey, Sarkar, Chen, Schillinger, & Wolf, 2012; Davis et al., 2009; Mahtani, Heneghan, Glasziou, & Perera, 2011; Newell, Bowman, & Cockburn, 1999). Identifying the best combinations of these and other strategies is essential to promoting safe and appropriate medication use, especially among patients with limited literacy skills.
References
- Andrade S. E., Kahler K. H., Frech F., Chan K. A. Methods for evaluation of medication adherence and persistence using automated databases. Pharmacoepidemiology and Drug Safety. 2006;15:565–574. doi: 10.1002/pds.1230. [DOI] [PubMed] [Google Scholar]
- Bailey S. C., Sarkar U., Chen A. H., Schillinger D., Wolf M. S. Evaluation of language concordant, patient-centered drug label instructions. Journal of General Internal Medicine. 2012;27:1707–1713. doi: 10.1007/s11606-012-2035-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergeron A. R., Webb J., Serper M., Federman A. D., Shrank W. H., Russell A., Wolf M. S. A local perspective of the impact of electronic prescribing on medication use in ambulatory care. American Journal of Managed Care. (In press) [PubMed]
- Bosworth H. B., Granger B. B., Mendys P., Brindis R., Burkholder R., Czajkowski S. M., Granger C. B. Medication adherence: A call for action. American Heart Journal. 2011;162:412–424. doi: 10.1016/j.ahj.2011.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catz S. L., Kelly J. A., Bogart L. M., Benotsch E. G., McAuliffe T. L. Patterns, correlates, and barriers to medication adherence among persons prescribed new treatments for HIV disease. Health Psychology. 2000;19:124–133. [PubMed] [Google Scholar]
- Coleman C. I., Limone B., Sobieraj D. M., Lee S., Roberts M. S., Kaur R., Alam T. Dosing frequency and medication adherence in chronic disease. Journal of Managed Care Pharmacy. 2012;18:527–539. doi: 10.18553/jmcp.2012.18.7.527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colley C. A., Lucas L. M. Polypharmacy: The cure becomes the disease. Journal of General Internal Medicine. 1993;8:278–283. doi: 10.1007/BF02600099. [DOI] [PubMed] [Google Scholar]
- Cramer J. A., Roy A., Burrell A., Fairchild C. J., Fuldeore M. J., Ollendorf D. A., Wong P. K. Medication compliance and persistence: terminology and definitions. Value Health. 2008;11:44–47. doi: 10.1111/j.1524-4733.2007.00213.x. [DOI] [PubMed] [Google Scholar]
- Davis T. C., Federman A. D., Bass P. F., Jackson R. H., Middlebrooks M., Parker R. M., Wolf M. S. Improving patient understanding of prescription drug instructions. Journal of General Internal Medicine. 2009;24:57–62. doi: 10.1007/s11606-008-0833-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis T. C., Wolf M. S., Bass P. F., Middlebrooks M., Kennen E., Baker D. W., Parker R. M. Low literacy impairs comprehension of prescription drug warning labels. Journal of General Internal Medicine. 2006;21:847–851. doi: 10.1111/j.1525-1497.2006.00529.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis T. C., Wolf M. S., Bass P. F., Thompson J. A., Tilson H. H., Neuberger M., Parker R. M. Literacy and misunderstanding prescription drug labels. Annals of Internal Medicine. 2006;145:887–894. doi: 10.7326/0003-4819-145-12-200612190-00144. [DOI] [PubMed] [Google Scholar]
- DeWalt D. A., Berkman N. D., Sheridan S., Lohr K. N., Pignone M. P. Literacy and health outcomes: A systematic review of the literature. Journal of General Internal Medicine. 2004;19:1228–1239. doi: 10.1111/j.1525-1497.2004.40153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimatteo M. R. The role of effective communication with children and their families in fostering adherence to pediatric regimens. Patient Education and Counseling. 2004;55:339–344. doi: 10.1016/j.pec.2003.04.003. [DOI] [PubMed] [Google Scholar]
- Doak C. C., Doak L. G., Root J. H. Teaching patients with low literacy skills. Philadelphia, PA: Lippincott; 1996. [Google Scholar]
- Ernst F. R., Grizzle A. J. Drug-related morbidity and mortality: Updating the cost-of-illness model. Journal of the American Pharmaceutical Association. 2001;41:192–199. doi: 10.1016/s1086-5802(16)31229-3. [DOI] [PubMed] [Google Scholar]
- Farber H. J., Capra A. M., Finkelstein J. A., Lozano P., Quesenberry C. P., Jensvold N. G., Lieu T. A. Misunderstanding of asthma controller medications: Association with nonadherence. Journal of Asthma. 2003;40:17–25. doi: 10.1081/jas-120017203. [DOI] [PubMed] [Google Scholar]
- Farmer K. C. Methods for measuring and monitoring medication regimen adherence in clinical trials and clinical practice. Clinical Therapeutics. 1999;21:1074–1090. doi: 10.1016/S0149-2918(99)80026-5. [DOI] [PubMed] [Google Scholar]
- Fischer M. A., Choudhry N. K., Brill G., Avorn J., Schneeweiss S., Hutchins D., Shrank W. H. Trouble getting started: Predictors of primary medication nonadherence. American Journal of Medicine. 2011;124 doi: 10.1016/j.amjmed.2011.05.028. [DOI] [PubMed] [Google Scholar]
- Fischer M. A., Stedman M. R., Lii J., Vogeli C., Shrank W. H., Brookhart M. A., Weissman J. S. Primary medication non-adherence: Analysis of 195,930 electronic prescriptions. Journal of General Internal Medicine. 2010;25:284–290. doi: 10.1007/s11606-010-1253-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garber M. C., Nau D. P., Erickson S. R., Aikens J. E., Lawrence J. B. The concordance of self-report with other measures of medication adherence: A summary of the literature. Medical Care. 2004;42:649–652. doi: 10.1097/01.mlr.0000129496.05898.02. [DOI] [PubMed] [Google Scholar]
- Gazmararian J. A., Kripalani S., Miller M. J., Echt K. V., Ren J., Rask K. Factors associated with medication refill adherence in cardiovascular-related diseases: a focus on health literacy. Journal of General Internal Medicine. 2006;21:1215–1221. doi: 10.1111/j.1525-1497.2006.00591.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golin C. E., DiMatteo M. R., Gelberg L. The role of patient participation in the doctor visit. Implications for adherence to diabetes care. Diabetes Care. 1996;19:1153–1164. doi: 10.2337/diacare.19.10.1153. [DOI] [PubMed] [Google Scholar]
- Gu Q., Dillon C. F., Burt V. L. Prescription drug use continues to increase: U.S. prescription drug data for 2007–2008. Atlanta, GA: National Center for Health Statistics; 2010. [PubMed] [Google Scholar]
- Haynes R. B., Yao X., Degani A., Kripalani S., Garg A., McDonald H. P. Interventions for enhancing medication adherence (Review) Cochrane Database of Systematic Reviews. 2005;2005:4. doi: 10.1002/14651858.CD000011.pub2. [DOI] [PubMed] [Google Scholar]
- Ho P. M., Spertus J. A., Masoudi F. A., Reid K. J., Peterson E. D., Magid D. J., Rumsfeld J. S. Impact of medication therapy discontinuation on mortality after myocardial infarction. Archives of Internal Medicine. 2006;166:1842–1847. doi: 10.1001/archinte.166.17.1842. [DOI] [PubMed] [Google Scholar]
- Hoffman J. M., Proulx S. M. Medication errors caused by confusion of drug names. Drug Safety. 2003;26:445–452. doi: 10.2165/00002018-200326070-00001. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Health literacy: A prescription to end confusion. Washington, DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- Institute of Medicine. Preventing medication errors. Washington, DC: National Academies Press; 2006. [Google Scholar]
- Institute of Medicine. Methodological challenges in biomedical HIV prevention trials. Washington, DC: National Academies Press; 2008. [Google Scholar]
- Jerant A., DiMatteo R., Arnsten J., Moore-Hill M., Franks P. Self-report adherence measures in chronic illness: Retest reliability and predictive validity. Medical Care. 2008;46:1134. doi: 10.1097/MLR.0b013e31817924e4. [DOI] [PubMed] [Google Scholar]
- Kalichman S. C., Pope H., White D., Cherry C., Amaral C. M., Swetzes C., Kalichman M. O. Association between health literacy and HIV treatment adherence: Further evidence from objectively measured medication adherence. Journal of the International Association of Physicians in AIDS Care. 2008;7:317–323. doi: 10.1177/1545109708328130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy J., Tuleu I., Mackay K. Unfilled prescriptions of medicare beneficiaries: Prevalence, reasons, and types of medicines prescribed. Journal of Managed Care Pharmacy. 2008;14:553–560. doi: 10.18553/jmcp.2008.14.6.553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kutner M., Greenberg E., Jin Y., Paulsen C., White S. The health literacy of America‘s adults: Results from the 2003 National Assessment of Adult Literacy. Washington, DC: National Center for Education Statistics: U.S. Department of Education; 2006. [Google Scholar]
- Liu H., Golin C. E., Miller L. G., Hays R. D., Beck C. K., Sanandaji S., Wenger N. S. A comparison study of multiple measures of adherence to HIV protease inhibitors. Annals of Internal Medicine. 2001;134:968–977. doi: 10.7326/0003-4819-134-10-200105150-00011. [DOI] [PubMed] [Google Scholar]
- Liu L. L., Park D. C. Aging and medical adherence: The use of automatic processes to achieve effortful things. Psychology and Aging. 2004;19:318–325. doi: 10.1037/0882-7974.19.2.318. [DOI] [PubMed] [Google Scholar]
- Mahtani K. R., Heneghan C. J., Glasziou P. P., Perera R. Reminder packaging for improving adherence to self-administered long-term medications. Cochrane Database of Systematic Reviews. 2011;2012:CD005025. doi: 10.1002/14651858.CD005025.pub3. [DOI] [PubMed] [Google Scholar]
- McHorney C. A., Spain C. V. Frequency of and reasons for medication non-fulfillment and non-persistence among American adults with chronic disease in 2008. Health Expectations. 2011;14:307–320. doi: 10.1111/j.1369-7625.2010.00619.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morisky D. E., Green L. W., Levine D. M. Concurrent and predictive validity of a self-reported measure of medication adherence. Medical Care. 1986;24:67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- Muir K. W., Santiago-Turla C., Stinnett S. S., Herndon L. W., Allingham R. R., Challa P., Lee P. P. Health literacy and adherence to glaucoma therapy. American Journal of Ophthalmology. 2006;142:223–226. doi: 10.1016/j.ajo.2006.03.018. [DOI] [PubMed] [Google Scholar]
- Newell S. A., Bowman J. A., Cockburn J. D. A critical review of interventions to increase compliance with medication-taking, obtaining medication refills, and appointment-keeping in the treatment of cardiovascular disease. Preventive Medicine. 1999;29:535–548. doi: 10.1006/pmed.1999.0579. [DOI] [PubMed] [Google Scholar]
- Osterberg L., Blaschke T. Adherence to medication. New England Journal of Medicine. 2005;353:487–497. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- Paasche-Orlow M. K., Cheng D. M., Palepu A., Meli S., Faber V., Samet J. H. Health literacy, antiretroviral adherence, and HIV-RNA suppression: A longitudinal perspective. Journal of General Internal Medicine. 2006;21:835–840. doi: 10.1111/j.1525-1497.2006.00527.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park D. C., Hertzog C., Leventhal H., Morrell R. W., Leventhal E., Birchmore D., Bennett J. Medication adherence in rheumatoid arthritis patients: Older is wiser. Journal of the American Geriatrics Society. 1999;47:172–183. doi: 10.1111/j.1532-5415.1999.tb04575.x. [DOI] [PubMed] [Google Scholar]
- Parker R., Ratzan S. C. Health literacy: A second decade of distinction for Americans. Journal of Health Communication. 2010;15(Suppl. 2):20–33. doi: 10.1080/10810730.2010.501094. [DOI] [PubMed] [Google Scholar]
- Persell S. D., Bailey S. C., Tang J., Davis T. C., Wolf M. S. Medication reconciliation and hypertension control. American Journal of Medicine. 2010;123:e189–e115. doi: 10.1016/j.amjmed.2009.06.027. [DOI] [PubMed] [Google Scholar]
- Piette J. D., Heisler M., Wagner T. H. Cost-related medication underuse: Do patients with chronic illnesses tell their doctors? Archives of Internal Medicine. 2004;164:1749–1755. doi: 10.1001/archinte.164.16.1749. [DOI] [PubMed] [Google Scholar]
- Pignone M., DeWalt D. A., Sheridan S., Berkman N., Lohr K. N. Interventions to improve health outcomes for patients with low literacy. A systematic review. Journal of General Internal Medicine. 2005;20:185–192. doi: 10.1111/j.1525-1497.2005.40208.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saini S. D., Schoenfeld P., Kaulback K., Dubinsky M. C. Effect of medication dosing frequency on adherence in chronic diseases. American Journal of Managed Care. 2009;15:e22–e33. [PubMed] [Google Scholar]
- Steiner J. F., Earnest M. A. The language of medication-taking. Annals of Internal Medicine. 2000;132:926–930. doi: 10.7326/0003-4819-132-11-200006060-00026. [DOI] [PubMed] [Google Scholar]
- Thompson K., Kulkarni J., Sergejew A. A. Reliability and validity of a new Medication Adherence Rating Scale (MARS) for the psychoses. Schizophrenia Research. 2000;42:241–247. doi: 10.1016/s0920-9964(99)00130-9. [DOI] [PubMed] [Google Scholar]
- Williams M. V., Baker D. W., Honig E. G., Lee T. M., Nowlan A. Inadequate literacy is a barrier to asthma knowledge and self-care. Chest. 1998;114:1008–1015. doi: 10.1378/chest.114.4.1008. [DOI] [PubMed] [Google Scholar]
- Wolf M. S., Bennett C. L., Davis T. C., Marin E., Arnold C. A qualitative study of literacy and patient response to HIV medication adherence questionnaires. Journal of Health Communication. 2005;10:509–517. doi: 10.1080/10810730500228631. [DOI] [PubMed] [Google Scholar]
- Wolf M. S., Curtis L. M., Waite K., Bailey S. C., Hedlund L. A., Davis T. C., Wood A. J. Helping patients simplify and safely use complex prescription regimens. Archives of Internal Medicine. 2011;171:300–305. doi: 10.1001/archinternmed.2011.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf M. S., Davis T. C., Curtis L. M., Webb J. A., Bailey S. C., Shrank W. H., Wood A. J. Effect of standardized, patient-centered label instructions to improve comprehension of prescription drug use. Medical Care. 2011;49:96–100. doi: 10.1097/MLR.0b013e3181f38174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf M. S., Davis T. C., Tilson H. H., Bass P. F., 3rd, Parker R. M. Misunderstanding of prescription drug warning labels among patients with low literacy. American Journal of Health-System Pharmacy. 2006;63:1048–1055. doi: 10.2146/ajhp050469. [DOI] [PubMed] [Google Scholar]
- Wolf M. S., Wilson E. A. H., Rapp D. N., Waite K. R., Bocchini M. V., Davis T. C., Rudd R. E. Literacy and learning in healthcare. Pediatrics. 2009;124:S275–S281. doi: 10.1542/peds.2009-1162C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu J. R., Moser D. K., Lennie T. A., Burkhart P. V. Medication adherence in patients who have heart failure: A review of the literature. Nursing Clinics of North America. 2008;43:133–153. doi: 10.1016/j.cnur.2007.10.006. vii-viii. [DOI] [PubMed] [Google Scholar]


