Abstract
Introduction:
Lack of sufficient bone height along maxillary sinus poses significant difficulty for placement of implants in edentulous maxillary jaw. Minimally invasive sinus augmentation is an effective solution for this problem. The manuscript intends to present long period results of such augmentation using direct (DSAT) and indirect (ISAT) minimally invasive sinus augmentation technique (SAT) from a single center.
Materials and Methods:
Records of patients who required minimally invasive sinus augmentation to increase residual bone height for implant placement fulfilling predetermined exclusion and inclusion criteria. Only patients with follow-up records for at least a year were considered. Both DSAT and ISAT were employed for sinus augmentation. The age, gender, period of edentulousness, alveolus thickness at crestal level during the pre- and postoperative assessment, implant length, and diameter of implants were collected from case histories. Descriptive statistics, Chi-square, paired test, and one way analysis of variance (ANOVA) was used appropriately. P ≤ 0.05 was considered as significant.
Results:
There were 197 implants placed and mean age of the group was 40.2 ± 10.7 years. There was a slight male predilection (54.3%). The gain in bone height as expressed in percentage after a year was 134.6%. On comparing the length of residual alveolar bone (RAB) at start and end of study, ISAT had a mean preoperative height of 7.88 mm while postoperative height was 13.22 mm. For DSAT, the mean height at start of treatment was 3.94 mm while at the end it was 10.13 mm. The mean increase in height was 6.19 mm. For both cases, P was 0.000.
Discussion:
Age, gender, and period of edentulism did not influence the outcome. The alveolar width appears to differ and influence the outcome. When alveolar width increases, wider diameter implants can be placed by compromising height. Thus it is a clinical acumen that would be extremely helpful to gauge the outcome of the condition.
Keywords: Alveolar bone height, dental implants, minimally invasive sinus augmentation, sinus surgery
INTRODUCTION
Successful dental implant placement in non-dentate area of maxillary posterior region requires sufficient training. They pose all challenges that are inherent to this region. The maxilla is made up of spongy bone and has one of the least dense bones in oral cavity.[1] Periodontal disease stimulated teeth loss causes accentuated bone deficiency, both in height and width by significant resorption of alveolar bone. Time period of tooth loss leads to absence of continuous bone stimulation that was earlier provided by dentition. Bone remodeling in the region is further complicated by post extraction bone resorption, pneumatization of maxillary sinuses, and poor quality of residual alveolar bone.[2]
In the immediate time period after maxillary posterior tooth extraction, initial decrease in alveolar width is by resorption and/or loss of buccal bone. With continuous bone remodeling, absence of stimulation, loss of bone height, and density leads to an increase in antral pneumatization. The maxillary sinus pneumatization is caused by progressive hallowing out of alveolar process of apical aspect mediated by osteoclasts and by increase in positive intra-antral pressure. In such a situation, the residual vertical bone height is decreased making standard implant placement difficult.[1,2]
To adapt, circumvent, and treat this local physiological as well as anatomical limitation; maxillary sinus floor elevation has become an important preplacement procedure in dental implant treatment planning. Various methodologies have evolved to increase the thickness of maxillary sinus floor. The treatment goal of all such procedures is to increase residual bone height. Few of the technique involve simple, minimal elevation of maxillary sinus membrane, Schneiderian membrane, while other include placement of various type of grafts including allografts, autografts, bone morphogenetic proteins, and hydroxyapatite crystals.[3,4,5]
The success of minimally invasive sinus augmentation and dental implant placement relies on selection of technique of placement, graft material, if necessary and adequate preoperative planning besides the skill of operator. There are two main ways of reaching sinus membrane; a direct one and an indirect method of sinus augmentation. The direct sinus augmentation technique (DSAT) involves direct visualization and manipulation of Schneiderian membrane while the other method indirectly (ISAT) manipulates the membrane. Both these method have delineated indication and contraindication. The factors that contribute to survival rate of sinus augmentation and dental implant placement are still the subject of discussion.[5]
This aim of present study is to present 1-year outcome of maxillary sinus augmentation procedure performed in a single center using the standard technique. Comparison of bone graft, the technique and gain in bone height at the end of year is also presented.
MATERIALS AND METHODS
This retrospective study included records of all consecutive patients seeking dental implant who required maxillary sinus augmentation. The study period was June 2008-May 2011. In these patients FDA approved, self-threaded titanium implants had been placed in a single stage and followed-up for at least a year ±4 weeks. These patients initially presented with edentulous; atrophic maxillary arch either due to physiological aging, trauma, or periodontal conditions and patients presenting with one or more missing teeth in posterior maxillary arch, either unilaterally or bilaterally. In all 182 patients, 197 implants were placed along the augmented sinus. Patients with systemic illness/systemic drugs that would affect postoperative healing; patients with poor oral hygiene, chronic smokers, psychiatric illness, and preexisting sinus problem were excluded from the study. The age, gender, period of edentulousness, alveolus thickness at crestal level at the pre-operative assessment, implant length, and diameter of implant were collected from case history.
Direct sinus augmentation technique (DSAT)
After identifying the residual alveolar bone (RAB) height in imaging studies, only those cases that has RAB height 5 mm or below was considered for this technique. Autogenous bone grafts was harvested by shaving the mandibular bone from external oblique ridge area or chin area. A bone mill was used to grind the bone shaving into fine particles. After adequate local anesthesia and preparation, a surgical incision was placed on the crest of RAB at most appropriate area, with vertical releasing curvilinear incisions flaring into the vestibule. Full-thickness, subperiosteal labial, and palatal flaps were raised, reflected. Care was taken to keep the base of flap broad as well as adequate buccal and palatal tissue for closure. After elevation, the anterolateral wall of maxillary sinus was visualized. Care was taken to identify and protect infraorbital nerve, if encountered. The dimension of osteotomy was determined based on clinical and radiographic examinations as well as the extent of edentulous span. A buccal bone window was made on exposed wall of maxillary sinus using a postage stamp method. The bony wall was gently manipulated with sinus membrane elevators without damaging Schneiderian membrane.
The previously obtained graft material was then placed and packed. The implant was placed on same sitting with help of a stent which was positioned, then removed, and the site was checked for appropriate faciolingual and mesiodistal positioning [Figures 1 and 2]. Any obvious abnormal crestal defects required slight modification of the position. A pilot drill of 2 mm in diameter was then drilled in marked implant site on RAB to establish depth and axis of implant recipient site. The implant was placed with its axis parallel to occlusal forces. Paralleling pins were employed as necessary to check parallelism of drill holes. The drills were used in a standard reduction gear hand piece along with a physiodispenser enabling copious saline irrigation to prevent excessive heat generation. The drill was used at the speed of 800-1,000 rpm. Drills with gradually increasing diameters were used to enlarge implant recipient site till the desired diameter corresponding to implant's diameter was reached. Implants were then placed into the prepared site using a torque wrench. 3-0 Vicryl sutures were used to close the surgical wound. Antibiotic coverage, pain killers, and nasal decongestants were prescribed for 5 days. The patients were monitored on a periodic basis, both clinically and radiologically.
Figure 1.
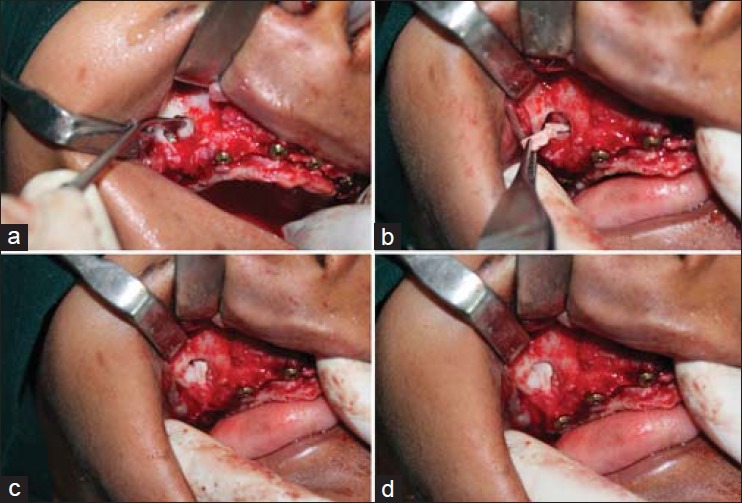
Direct sinus lift with simultaneous implant placement with use of autogenous bone graft (a) In-fracturing and lifting of lateral window of right maxillary sinus, (b) Autogenous bone harvested from donor site being placed in newly created space, (c) Bone packed in the window, (d) Sinus floor augmented and implant placed
Figure 2.
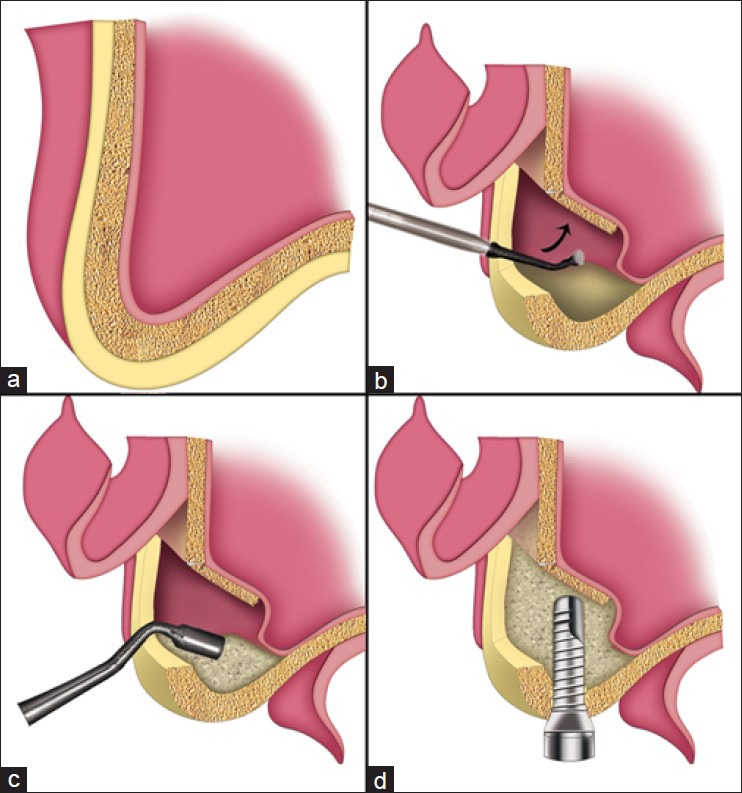
Line diagrams illustrating direct sinus lift with simultaneous implant placement, (a) Atrophic posterior maxilla with residual bone height between sinus floor and alveolar crest inadequate for placement of dental implant, (b) Lateral wall of sinus in-fractured and membrane is elevated, (c) Grafted bone is densely packed in space created after lifting the membrane, (d) Augmented maxillary sinus with implant placed
Indirect sinus augmentation technique (ISAT)
Cases with RAB height of 6-8 mm were taken for indirect sinus augmentation. The RAB to receive the implant was exposed under local anesthesia and perforated using a small rounded drill. A pilot drill was placed in marked implant site to establish the axis of implant recipient site. Following the pilot drill, subsequently increasing diameter of drills were used to enlarge implant recipient site till the desired diameter corresponding to implant diameter was reached. The height of drill was maintained 2 mm short of sinus floor. The indirect sinus lift was done by insertion of correct caliber osteotome and working up through successively greater instrument diameters, until the sinus floor was fractured and elevated up. The sinus floor was carefully fractured, separated from the Schneiderian membrane avoiding damage to membrane using a surgical mallet with controlled force. If required, autogenous graft material was inserted within the socket. The material was displaced apically with help of larger-diameter instruments, thereby lifting the membrane and condensing graft material between the latter and sinus floor. The implant was then placed immediately in the prepared site [Figures 3–5]. 3-0 Vicryl sutures were used to close the surgical wound. Antibiotic coverage, pain killers, and nasal decongestants were prescribed for 5 days. The patients were monitored on a periodic basis both clinically and radiologically.
Figure 3.
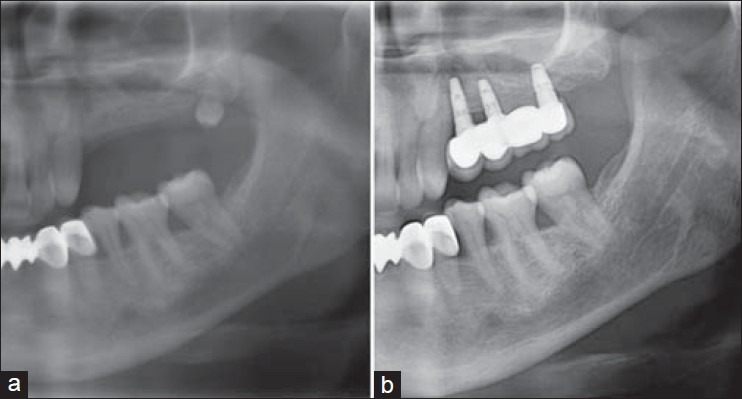
Pre- and postoperative orthopantomograph (OPG) in a case treated with indirect sinus lift and bone graft for implant placement, (a) Insufficient residual bone, (b) After prosthetic rehabilitation following indirect sinus lift, bone grafting, and implant placement
Figure 5.
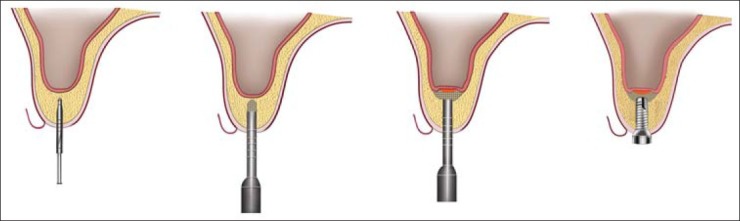
Sequential steps in indirect sinus augmentation technique; implant site prepared starting from small diameter to large diameter drills, sinus floor fractured, elevated, and bone graft placed in the resultant space and immediate implant placement
Figure 4.
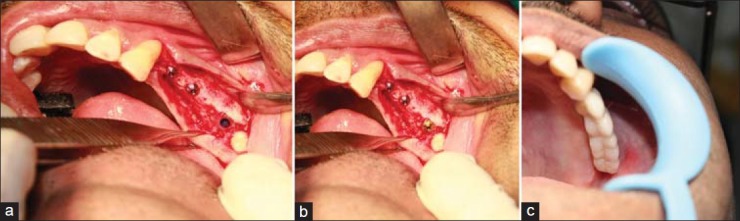
(a) Implant recipient site prepared using drills, (b) Implant placed in prepared site, (c) After rehabilitation with prosthesis
Measurements
Digital panoramic radiographs and radiovisiography records (accounted for distortion/magnification) taken using repeatedly calibrated machines were used for screening examinations and treatment planning. In radiographs, height of the residual bone was measured in imaging records three times and average taken as preoperative height. The height of bone was estimated in the same region of implant after a year and taken as 1 year postoperative bone height. The gain in bone height was expressed as a percentage of increase in bone height (new height - old height) divided by the old bone height.
All the data thus collected were entered and analyzed using Statistical Package for Social Service, version 17.0 (SPSS Inc, IBM, IL, USA). Descriptive data are presented. Chi-square test and paired t-test was used to compare the difference between direct and indirect technique. One way analysis of variance (ANOVA) was employed to identify the mean between continuous outcome variables. P ≤ 0.05 was taken as significant.
RESULTS
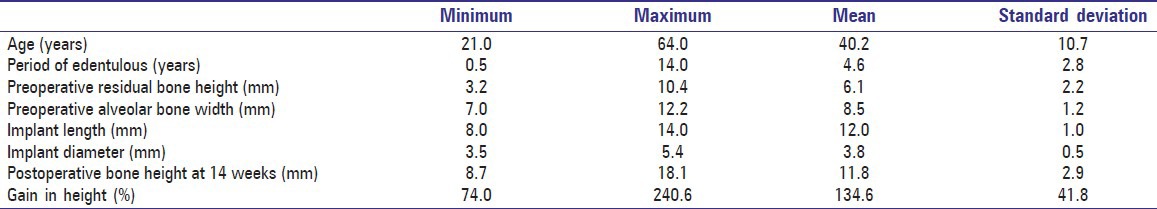
Of the 197 instances of implant placement through ISAT and DSAT, the mean age of the group was 40.2 ± 10.7 years. There was a slight male predilection (54.3%). Based on age group, 23.4% belonged to age below 30 years, 26.4% in 31-40 years, and 33.55% in 41-50 years. Of all, 112 cases (56.9%) required grafts. The most common cause of tooth loss was dental caries, periodontal diseases accounting for 88% of cases. The mean period of edentulism was 4.6 ± 2.8 years. The overall RAB was 4.6 mm, while alveolus width was 8.5 mm. Among the study group, average length of implant used was 12 mm with a diameter of 3.8 mm. This differed with the technique. The gain in bone height as measured in percentage after a year was 134.6% [Table 1].
Table 1.
Demographic and clinical features of study population
On comparing ISAT (n = 108) and DSAT (n = 89), the gender and age distribution in study population was not significant. The placement of graft was significant between ISAT and DSAT [Table 2]. On comparing the mean age between ISAT and DSAT, difference was not statistically significant (P = 0.271). The mean period of edentulous also did not appear to influence (P = 0.87). The difference in alveolar width was significant between ISAT and DSAT cases (P = 0.01). The mean length and diameter of implant used was also statistically significant (P = 0.000 and 0.007, respectively). The gain in bone height expressed as percentage of original RAB height at end of 1 year for ISAT was 99.52% while for DSAT it was 177.22%. This difference was statistically significant. [Table 3]. In the indirect sinus lift (ISL) method, when graft was used, the mean gain percentage was 115.52 ± 6.04%; while when no grafts were used, the gain in height was 95.2 ± 11.36%.
Table 2.
Comparison of gender, age, and graft use among techniques for minimally invasive sinus augmentation
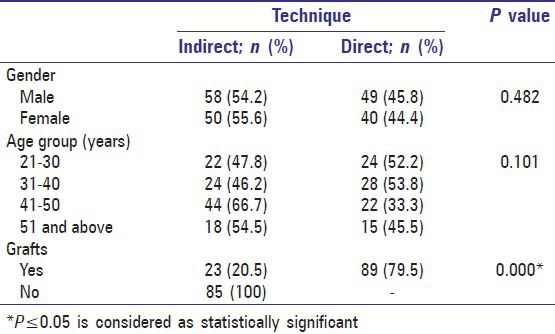
Table 3.
One way analysis of variance (ANOVA) for comparison among techniques for minimally invasive sinus augmentation
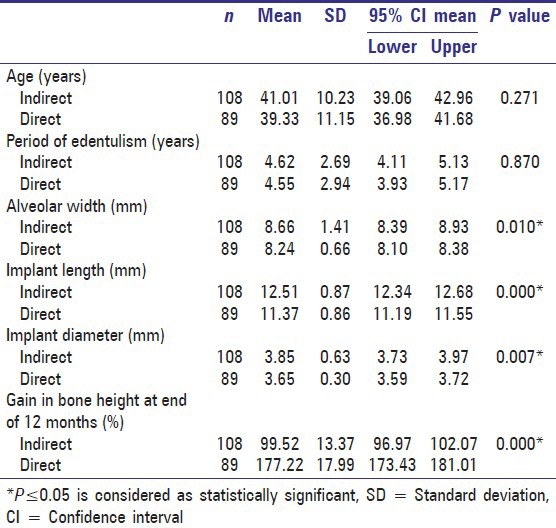
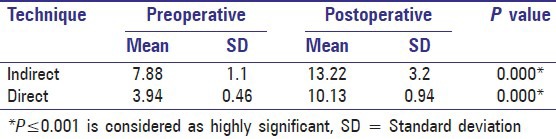
On comparing length of the RAB at start and end of study, ISAT had a mean preoperative height of 7.88 mm while postoperative height was 13.22 mm. The mean increase in height was 5.34 mm. This difference was statistically significant. Similarly for DSAT, mean height at start of treatment was 3.94 mm; while at the end it was 10.13 mm. The mean increase in height was 6.19 mm. For both cases, P was 0.000 [Table 4].
Table 4.
Comparison of pre- and postoperative bone height for minimally invasive sinus augmentation
DISCUSSION
Edentulous maxillary segment has several anatomical and physiological limitations such as deficiency of spongy maxillary alveolar bone, increased pneumatization of the maxillary sinuses, and faster negative remodeling in absence of continuous pressure on periodontium. These factors render rehabilitation of the region very challenging. Owing to limited RAB, sinus floor elevation is seen as a prerequisite for dental implant placement.[3] The sinus elevation procedure has an integral invasive surgical procedure that could pose surgical morbidity as well as increase cost of treatment. The ISAT procedure performed with 5-8 mm thick RAB is less invasive and less costly for predictable implant placement.[2] For ridges with 3-5 mm thick RAB, surgical modalities as those proposed by Summers,[6] Fugazzotto,[7] and Toffler[8] provides less traumatic and less costlier alternatives especially in compromised single molar sites.
In the present study, sinus augmentation is done either by standard DSAT or ISAT as a single step procedure. During and after placements of dental implants, no significant complications were reported. These results were consistent with the findings of Graziani F et al.[9] They compared implant survival following sinus floor augmentation and estimated the survival rate between 75 and 100% both for nonaugmented and augmented areas. Similarly, Milan Jurisic et al., and Diana and Rao estimated a high success rate in their immediate and delayed implant placements on 61 patients and 11 patients, respectively.[3,10]
The number of steps in surgery did not appear to influence outcome of the study as reported by Watzek.[11] Hence, in the present study only single stage surgery was considered as the number of steps did not appear to critically influence outcome of primary and secondary stability of implant. The single most important criteria for selecting an ISAT are the RAB being 6 mm or more. When RAB was above 12 mm, sinus augmentation was not required. When RAB is 5 mm and less, DSAT is preferred as the graft needs to be placed. Minimum thickness requires increased RAB for implant placement. Hence, grafts were always placed in DSAT cases. In the grey zone of 5-6 mm, depending on other factors such as period of edentulism, alveolar width, and age of patients; the technique was chosen. It was observed that shorter implants with wide diameters were apt for patients who had thicker alveolar ridges. This ensured both primary and secondary stability of implants during the early and late phases. The aim of this study was to describe outcome of the ISAT and DSAT at end of a year. It is observed that the height is gained much with DSAT. This difference probably comes from two factors; the placement of graft in all cases of DSAT, and the second factor is the RAB height itself. As the gain in bone height is small, percentage change is obscured by this mathematical calculation.
Age, gender, and period of edentulism did not influence the outcome [Table 2]. The alveolar width appears to differ and influence the outcome. When height of RAB is reduced, alveolar width will increase [Table 3]. When the width increases, wider diameter implants can be placed compromising height. This could be related to increase in surface area with increasing diameter. Thus, it is a clinical acumen that would be extremely helpful to gauge outcome of the condition. Irrespective of the technique, there was a significant difference between preoperative and at the end of the treatment with significant value [Table 4]. The DSAT gave a better increase in height than ISAT. This could be attributed to use of grafts.
The outcome of sinus augmentation procedure for implant placement has been presented from a single center. It appears from the study that case selection and graft placement plays an important role in determining outcome of augmentation procedure. Owing to placement of graft, RAB height regained through DSAT is higher.
CONCLUSION
The present study identified that with a wider alveolus, shorter implant with greater diameter can be used safely, probably owing to increased surface area causing more osseointegration. The study also identified that result of sinus augmentation depends on surgeon's acumen and experience. The goal of any dental implant surgeon is to use a cost-effective, short duration, less risky, simple, and highly predictable outcome procedure. Advanced and extensive surgical techniques often increase treatment duration and costs with no absolute prediction of result. Use of minimally invasive technique such as DSAT and ISAT provides cost affordable, less risky, and predictable results as compared to invasive procedures. The techniques employed in this manuscript has facilitated implant placement in areas of limited bone height, improved primary stability, high implant success in posterior maxilla, simple, and minimally invasive surgery with increased success and case acceptance.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Raja SV. Management of the posterior maxilla with sinus lift: Review of techniques. J Oral Maxillofac Surg. 2009;67:1730–4. doi: 10.1016/j.joms.2009.03.042. [DOI] [PubMed] [Google Scholar]
- 2.Toffler M. Minimally invasive sinus floor elevation procedures for simultaneous and staged implant placement. N Y State Dent J. 2004;70:38–44. [PubMed] [Google Scholar]
- 3.Daniel D, Rao SG. Evaluation of increase in bone height following maxillary sinus augmentation using direct and indirect technique. J Dent Implant. 2012;2:26–31. [Google Scholar]
- 4.Wallace SS, Froum SJ. Effect of maxillary sinus augmentation on the survival of endosseous dental implants. A systematic review. Ann Periodontol. 2003;1:328–43. doi: 10.1902/annals.2003.8.1.328. [DOI] [PubMed] [Google Scholar]
- 5.Pal US, Sharma NK, Singh RK, Mahammad S, Mehrotra D, Singh N, et al. Direct vs. indirect sinus lift procedure: A comparison. Natl J Maxillofac Surg. 2012;3:31–7. doi: 10.4103/0975-5950.102148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Summers RB. The osteotome technique: Part 3-less invasive methods for elevation of the sinus flow. Compend Contin Educ Dent. 1994;15:698–708. [Google Scholar]
- 7.Fugazzotto PA. The modified trephine/osteotome sinus augmentation technique: Technical considerations and discussion of indications. Implant Dent. 2001;10:259–64. doi: 10.1097/00008505-200110000-00009. [DOI] [PubMed] [Google Scholar]
- 8.Toffler M. Staged sinus augmentation using a crestal core elevation procedure and modified osteotomes to minimize membrane perforation. Pract Proced Aesthet Dent. 2002;14:767–74. [PubMed] [Google Scholar]
- 9.Graziani F, Donos N, Needleman I, Gabriele M, Tonetti M. Comparison of implant survival following sinus floor augmentation procedures with implants placed in pristine posterior maxillary bone: a systematic review. Clin Oral Implants Res. 2004;15:677–82. doi: 10.1111/j.1600-0501.2004.01116.x. [DOI] [PubMed] [Google Scholar]
- 10.Jurisic M, Markovic A, Radulovic M, Brkovic BM, Sándor GK. Maxillary sinus floor augmentation: comparing osteotome with lateral window immediate and delayed implant placements: An interim report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:820–7.11. doi: 10.1016/j.tripleo.2008.04.025. [DOI] [PubMed] [Google Scholar]
- 11.Watzek G, Weber R, Bernhart T, Ulm C, Haas R. Treatment of patients with extreme maxillary atrophy using sinus floor augmentation and implants: Preliminary results. Int J Oral Maxillofac Surg. 1998;27:428–34. doi: 10.1016/s0901-5027(98)80031-3. [DOI] [PubMed] [Google Scholar]


