Abstract
Pathological enlargement of tongue is caused by several conditions and diseases. In several instances, surgery remains the only viable option for complete cure. Persistent bleeding, compromised neuro-motor-sensory functions during the postoperative period are the most common complaints encountered after macroglossia correction. The tongue is a muscular organ, whose complex neuroanatomy is being unraveled slowly. Various types of macroglossia resections in unique clinical situations have been proposed by several clinicians till date. There has never been unanimously accepted resection for the treatment of macroglossia. This review article attempts to preview the cosmetic and functional components for resection designs.
Keywords: Beckwith-Wiedemann syndrome, macroglossia, neuroanatomy, tongue resection, tongue musculature
INTRODUCTION
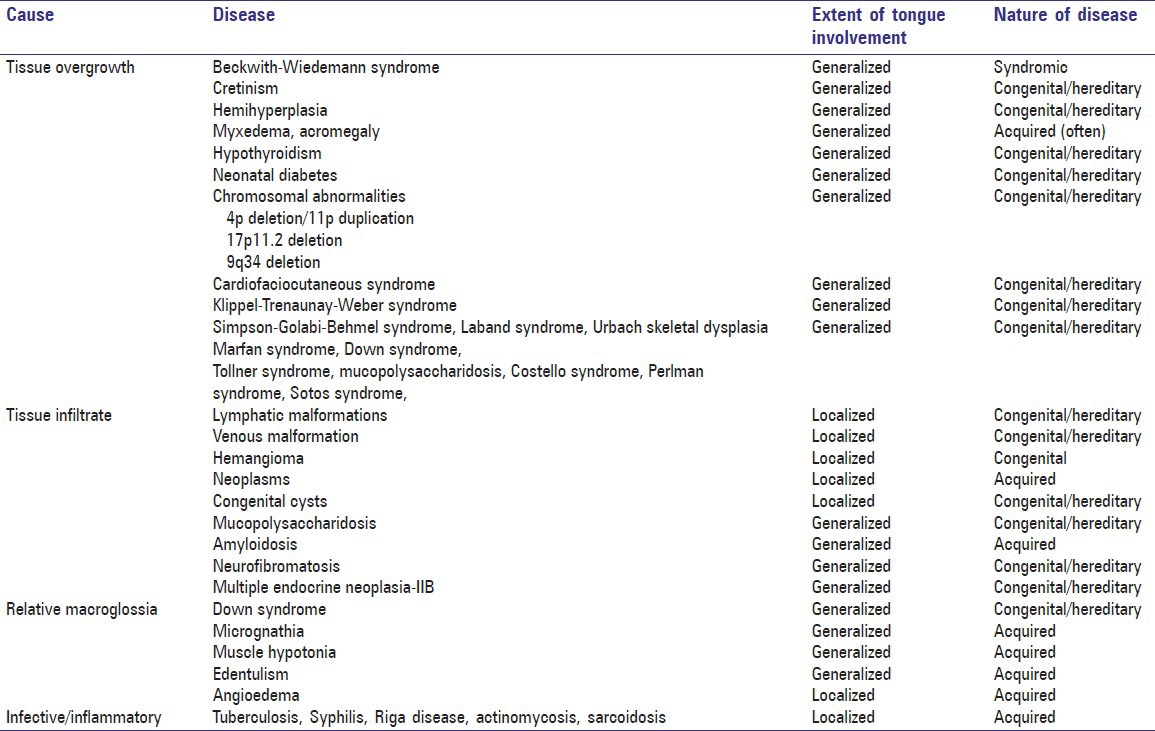
Macroglossia is a generalized term used to describe the tongue that protrudes beyond the teeth during natural resting posture. It creates an artificial, persistent, impression of teeth on lateral borders of the tongue when the patients slightly open their mouth.[1,2,3,4,5,6] Myer's and Vogel's classification are used to subdivide macroglossia. Myer classification, based upon extent of involvement, subdivides macroglossia into generalized or localized.[5] Based on etiology, Vogel classification divides macroglossia into true or relative.[6] When a primary disorder of tongue tissue leads to macroglossia, it is termed as true and when affected secondarily such as by amyloidosis, it is referred to as relative macroglossia. The list of causes and nature for macroglossia is given in Table 1.[1,2,3,4,5,6]
Table 1.
The spectrum of cause and nature of diseases that produces macroglossia
Macroglossia compromises airway by obstruction and often leads to obstructive sleep apnea. It hinders growth of the adjacent tissues leading to uncoordinated anatomical relationship causing malocclusion, making speech and mastication problematic. Recurrent upper respiratory tract infection compromises the general health while uncontrolled drooling of saliva predisposes to angular chelitis and supra added bacterial/fungal infections. In addition, normal psychological and social well being and interaction are often affected. Hence treatment is aimed at controlling the entire problem. When an accurate underlying cause such as an endocrine abnormality or neoplasia is identified, the preliminary step will be to treat the underlying cause.[1]
In case of syndromes and genetic conditions, only symptomatic surgery for esthetic and functional purpose is possible. In such cases, the goal of surgical intervention will be to reduce the bulk of tongue with maximum possible preservation of form, motor, and sensory function. In that situation, the rate of enlargement of tongue, age, gender, nature of disease process, other accompanying systemic abnormalities need to be considered before planning the surgery.[7,8]
Surgical interventions for anterior two-third macroglossia began without an understanding of the cause and proceeded with crude forms of resection till the past century. With more understanding of the neuroanatomy of the tongue, vasculature, innervations, healing of muscles after surgery, understanding of surgical approach, and design has undergone rapid evolution.[8,9] The aim of this review manuscript is to summarize the relevant neuroanatomy, resection design, and treatment algorithm for the macroglossia treatment involving the anterior two-third section of the tongue from personal experience using cases.
DIMENSIONS OF TONGUE IN MACROGLOSSIA
Macroglossia could occur due to varying etiology [Table 1]. Depending on the cause and stage of the condition, the dimension could vary. For example, prolonged edentulism causes increase in the width of tongue while syndromes such as Marfans and Ehler–Danlos syndromes may have excessive long tongue without other abnormalities. Accumulation of amyloid and proliferation of tissues as in neoplasia and hypertrophy will cause increase of the tongue thickness (height). Irrespective of the dimensional change, with the progression of disease, the tongue mass increases, requiring surgical intervention. Certain diseases like endocrine abnormalities and syndromes leads to increase in overall dimension of the tongue.[1,10]
Hence it should be a part of the work up for macroglossia that the exact cause is identified.[10] Clinical history, examination, basic imaging techniques will suffice to identify the etiology. However, at certain times, chromosomal and genetic studies may be essential to establish the diagnosis. A magnetic resonance imaging (MRI) may be helpful to identify the dimensions as well as the tumor margins. In certain cases, such as lingual thyroid and amyloidosis, an incisional biopsy may be useful.[1] The accurate dimensional measurement of tongue, especially the anterior tongue, will be an useful guidance for surgical planning and assist in deciding resection designs.
Resection designs for macroglossia
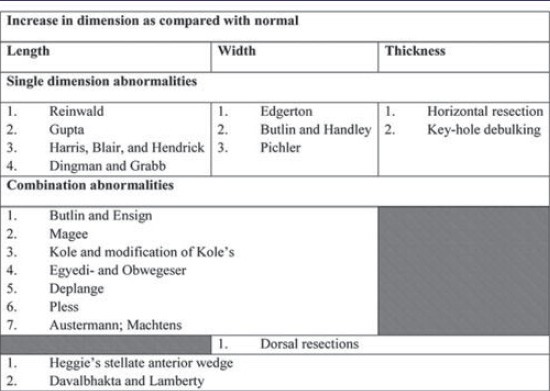
The main stay of surgical treatment of macroglossia is to provide a tongue that can function in the most efficient aspect in terms of form and function. The primitive surgical designs were to reduce the extensions of the tongue in terms of length and width. Peripheral trimming and reduction techniques such as those of Butlin, Ensin, Harris, Blair, Hendrick, Edgerton, Dingman, Grabb, and Gupta were aimed at reducing the length and the width of the tongue. The modifications of Krunchinsky, Mixter, and Harda were designed to preserve the tip of the tongue, a vital area for taste sensation and speech. Then the advanced key-hole procedures such as those of the modification of Kole's incision, Davalbhatka, and Heggies were aimed at preserving the function at the same time reducing the bulk of the tongue in all the three dimensions [Table 2, Figures 1 and 2].[8,10,11,12,13,14,15,16,17,18,19]
Table 2.
Type of resections for Macroglossia and dimensions altered
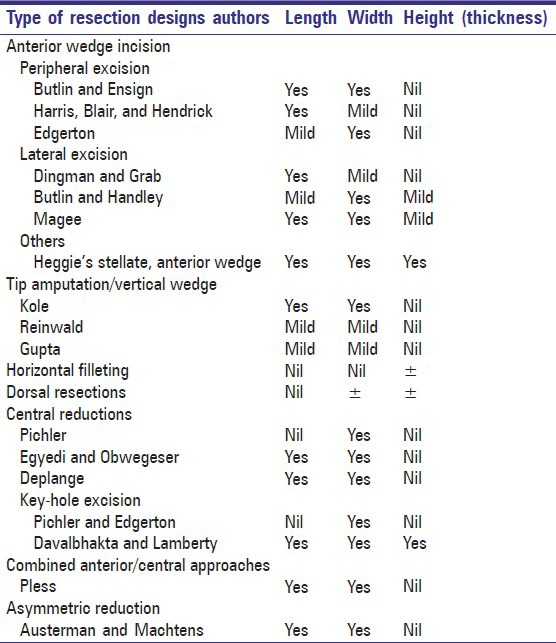
Figure 1.
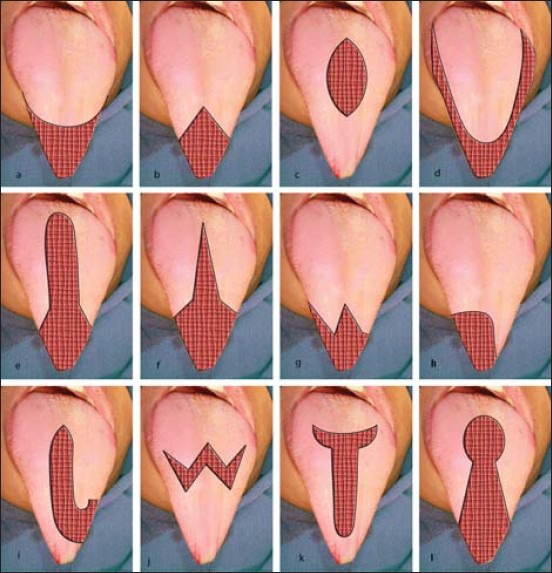
Incision pattern for Anterior 2/3rd Macroglossia. (a) Pichler, (b) Harris, Blair, and Hendrick, (c) Pichler–Edgerton, Central Reduction, (d) Butlin and Ensign, (e) Egyedi and Obwegeser, (f) Kole, Davalbhakta and Lamberty, (g and h) Austerman and Machtens, (i) Kruchinsky, (j) Mixter, (k) Harda and Enomoto, (l) Morgan et al. and Kacker et al.[10,11,12,13,14,15,16,17,18,19,20]
Figure 2.
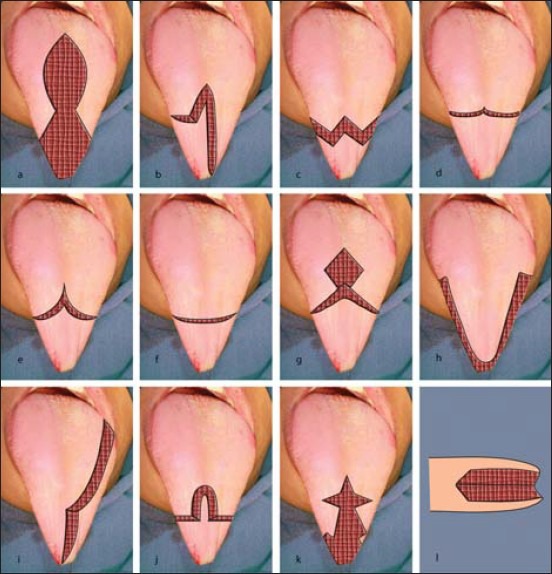
Incision pattern for Anterior 2/3rd Macroglossia. (a) Modified key-hole, (b) Pless, (c) Modification of Mixter, (d) Rheinwald, (e) Kole, (f) Gupta, (g) Deplange, (h) Dingman and Grab, (i) Magee, (j) Egyedi and Obwegeser, (k) Stellate- Anterior wedge, (l) Butlin-Handley[10,11,12,13,14,15,16,17,18,19,20]
In cases where minimum reduction is needed, peripheral excision remains a natural choice and can be effectively employed. In cases where anterior two-thirds of tongue alone is enlarged, sacrifice of the tip shall be considered. However, loss of taste sensation should be informed and appropriate decision should be taken. When only length is an issue, wedge incision-based resections offer better surgery. Combination resections are useful when the condition is generalized and involves all three dimensions.
Care should be exercised while manipulating the muscle. On raising the tongue mucosal resection after the mucosal incision, the muscle fibers will be visualized. Irrespective of the resection design selected, when a muscle fiber is injured, the entire perimysial unit shall be removed so that fibrosis may not set in at a later time. Compartmental removal of muscle fiber is stressed on, when involved similar to that of oncosurgeries.[20]
The aim of the glossoplasty will be to reduce the excessive dimension. When length is to be reduced, anteriorly placed peripheral incisions and resection design will be an ideal choice. When width is to be decreased, peripheral shaving would be ideal. When thickness or height of muscle becomes involved, the choice of resection needs to be critically assessed. Advocates of various resections have listed the advantages and disadvantages of all resections and most notably the anterior wedge reduction (AWR) versus central resection (CR) type of surgeries. Several resections create a poor form by the formation of a ‘pointy’ sharp tongue tip, asymmetry and issues with the reduction of the thickness of muscle. Innervations and blood supply would also be a problem though the latter is compensated by the richly innervated and collateral supply. Similarly, the issue of tongue rising at meeting point of incisions creates issues with the surface of tongue.[8]
Often, during debulking of the tongue, manipulation needs to be limited to the dorsal aspect of the tongue than the ventral surface to avoid injuring the lingual nerves, arteries, and Hypoglossal (HG) nerves.[18,21] The muscles involved in each area of the tongue are listed in Table 3.[22] Each and every segment has different muscles, which are involved.[22] Peripheral reduction will involve manipulation of styloglossus and probably hyoglossus. Resection that involves reduction of the tongue tip would need to manipulate the transverse and inferior longitudinal muscle fibers. Horizontal filleting will involve reduction of the core muscles – transverse, genioglossus and vertical fibers as well as the superficial longitudinal muscles. Superior longitudinal muscle run in groups hence, it will be easier for the removal of the entire group. Central reduction besides the core muscle will involve manipulation of superior longitudinal group of fibers. The AWR procedure will involve manipulation of the vertical, superior, inferior longitudinal, transverse, and genioglossus in varying degrees depending upon the type of resections. The double stellate resection and stellate anterior wedge resections will involve debulking with substantial removal of the core muscles along the body as well as the tip of the tongue.[22,23]
Table 3.
Position of tongue muscles
Probably the success of the AWR type of resections owes to the debulking of segments of core muscles. As much of the fiber groups are retained without being manipulated, the loss in function tends to be less with adequate form. The nerve supply is not disturbed much as in the antero-posterior dimension, the chorda-tympani and lingual nerve often travel inferiorly in the center and arise toward the tip as they come closer to the tip. In the medio-lateral dimension, the chorda-tympani supplies the central part of the tongue, while the lingual nerve caters to the lateral surface. In most of the resection designs, either one part is retained, which ensures sensory function of the tongue. As lingual nerve is placed deeper, it is often spared in most of the resections. The lingual arteries and ranine arteries lie very deep and closer to the fibrous septum and hence preserved in most of the conditions. This is often a crucial factor that is a must to ensure sufficient blood supply. While selecting the resection design and deciding the extension of depth of incision, it should not include the lingual vessels, else, necrosis of the tip would happen.[24]
Certain AWR resections have an inherent manipulation of both the chorda-tympani and lingual nerves that may cause loss of sensation particularly along the mid dorsal part of the tongue.[19] Resection design that spares either the chorda-tympani or lingual nerve would be ideal. Certain extended resection designs may create artificial raising or a shallow area owing to abnormal excessive rotation of the tongue. Hence acute change of direction and long axis resection needs to be avoided.
DISCUSSION
Majority of the debulking procedures employed midline access for AWR or CR.[12] The underlying disease process that causes the macroglossia determines the outcome of the surgery. The dimensions of the tongue – the length, width, and thickness as well as the treatment goal expected determine the tongue resection design.
Table 2 provides the various types of resection designs and the change in dimensions they offer. In addition to this, the extent of debulking, needs to preserve taste sensation, and vasculature preservation alters the choices of the surgeon. Besides these factors, certain other factors influence the outcome of the surgery. The preservation of tongue tip is a crucial decision. The natural esthetics of tongue is lost when tip is sacrificed. Preserving of tongue tip is absolutely essential for preserving the taste sensation as well as for excellent form and function. In personal experience, cases where tip of tongue have been preserved had better patient acceptance besides excellent results. The reason for this phenomenon lies in the local anatomy. The midline area of the natural tongue is made of fibrous septum. When the tip is reconstructed, bundles of the bilateral muscle group of tongue are often approximated. This fails to provide synchronous function.
Case 1, depicted in Figure 3, is a typical presentation of a nonsyndromic, tongue enlargement, with normal tissues involving its length and width. A modified resection design incorporating the Pichler's central reduction, modified key-hole, and Kole's approach were incorporated to form a rough clover shaped design. The anterior portion of the design was approximated along the midline. This helped to reduce the width of the tongue. The posterior margin was approximated at the midline. The approximation at the posterior margin helped to reduce the length of the tongue. As the bulk was adequate, no trimming was performed. Tip preservation was achieved by this choice of design.
Figure 3.
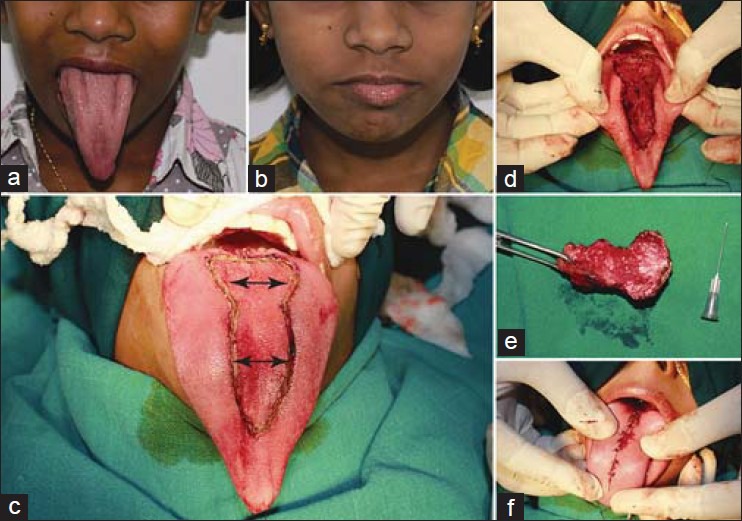
Clinical images of case 1 (a) Note the increased dimension of length and width preoperatively, (b) Postoperative facial profile, (c) Resection design, (d) Resected area, (e) Resected specimen, (f) Sutures placed
Case 2, shown, is a typical case of congenital storage abnormality. The patient shown here is affected with congenital Beckwith–Wiedemann syndrome [Figure 4]. The baby had protruded tongue that was hindering masticatory function as well as the airway. Debulking in all the dimensions was planned. A modified version of the Butlin and Ensign design was employed. Tip sacrifice with AWR was planned considering the age and growth potential. The Butlin and Ensign design resection was carried along with central debulking, a design very similar to that of Higgie AA. The resected tongue was sutured along the midline. This design spared lingual vessels and taste sensation and ensuring debulking in all the dimensions. Tip resection had to be carried out owing to the extraordinary length of the tongue, which was protruding even when normal. Owing to this the taste sensation was compromised as well as the form and function.
Figure 4.
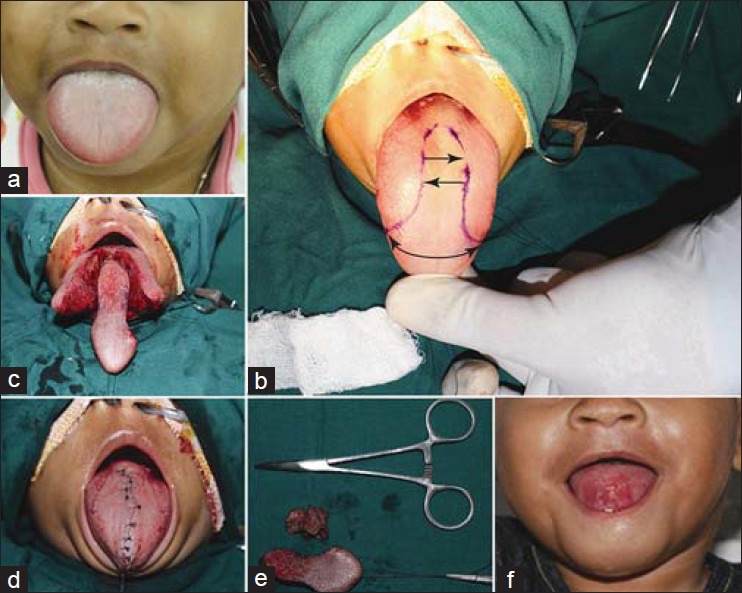
Clinical images of case 2 (a) Preoperative view, (b) Marking for incision, (c) Intraoperative photograph, (d) Suturing done, (e) Resected specimen, (f) Postoperative view
Case 3 is another common presentation [Figure 5], where the patient is affected with Down's syndrome. The length and width were larger. A modified, short version of the Harda and Enomoto type of resection design was employed. The modified design resembled a blunt tipped heart shape. The central median was designed in such a way that it was placed deeply. The approximation was performed away from the midline, toward the arms of the symbol. The blunt tip ensured close approximation without dog-ear defect. The design ensured preservation of bulk, tip of the tongue, vasularity, and lateral part of tongue sensation.
Figure 5.
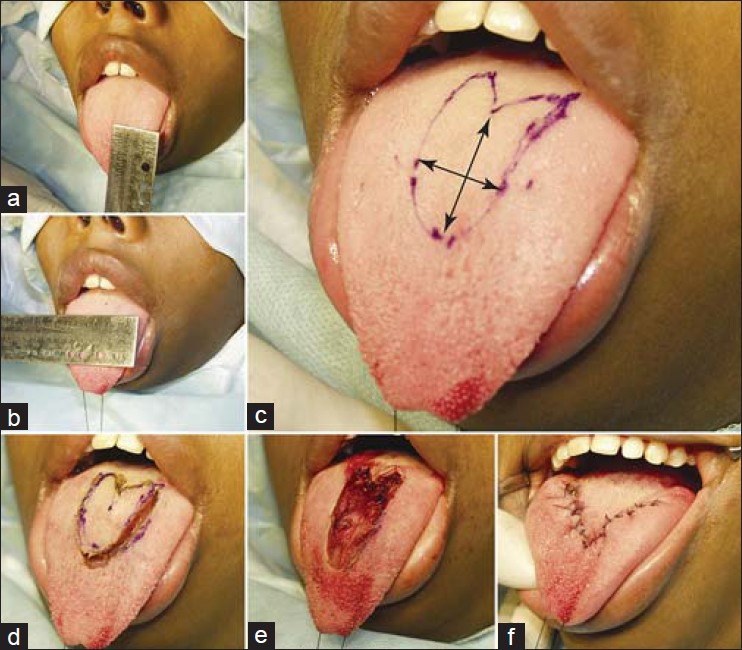
Clinical images of case 3 (a and b) Preoperative assessment length and width, (c) Resection design, (d and e) Intraoperative view, (f) Sutures placed
From general consensus of literature,[11,12,13,14,15,16,17,18] it is known that preserving the tip and the lateral borders of the tongue yields better results as these areas are of vital importance. Moreover, in most instances, the postoperative shape of the tip of the tongue plays a vital role in patient's satisfaction. Preservation of natural tip (devoid of abnormality) ensures cosmetic acceptance along with retaining of vital taste sense. Preservation of lateral borders prevents abnormal fibrosis of tongue musculature. All designs that comply to these principles, yield better patient acceptance, form and function at later stage.
Based on a single center experience, I propose a classification of efficient management of macroglossia [Table 4]. In cases where length of the tongue is abnormal, resection designs of Reinwald or Gupta or Harris, Blair, Hendrick or Dingman and Grabb can be employed. In situations where abnormal width is a primary concern, Edgerton/Butlin and Handley/Pichler design or their modification can be employed. For isolated thickness abnormalities, horizontal resections and key-hole debulking procedures are recommended. For situations where the length and width abnormalities occur, Butlin and Ensign or Magee or Kole or Egyedi-Obwegeser or Deplange or Pless or Austermann or Machtens designs and their modifications offer solution. For abnormally wide and thick tongue, dorsal resections are the only choice. In rare situations, when the length, width, and thickness are abnormal, Heggie's Stellate anterior wedge or Davalbhakta and Lamberty design offer best possible solution.
Table 4.
Classification of resection design for macroglossia
It has been already documented that there is no single ideal tongue resection procedure, rather the procedure needs to be customized considering the etiology, age, gender, existing dimension, and postoperative form/dimension desired.[8] Such individual approach gives more pleasing results than the predetermined ones. In case of older individuals with mild to moderate enlargement, peripheral surgical trimming is ideal to prevent loss of taste as well as speech abnormalities. In case of extreme enlargement, AWR and CR can be chosen but with caution. The underlying disorder has to be corrected.
CONCLUSION
The goal of the tongue reduction surgery is to primarily reduce the enlarged tongue while ensuring adequate taste sensation, speech, and masticatory functions. Three modifications of the popular tongue debulking techniques have been described. Evolving tongue research in terms of neuroanatomy, innervations, muscular functional models, and muscle healing have to be incorporated in to the clinical practice. Concise, relevant neuroanatomy, and physiology that determines the outcome of resection designs has been discussed. It is imperative that a surgeon understands and employs this knowledge while choosing the appropriate resection design for customized macroglossia treatments. In absence of such translation, the meaning of resection design will lack scientific rationale.
Footnotes
Source of Support: Nil
Conflict of Interest: No
REFERENCES
- 1.Prada CE, Zarate YA, Hopkin RJ. Genetic Causes of Macroglossia: Diagnostic Approach. Pediatrics. 2012;129:e431–37. doi: 10.1542/peds.2011-1732. [DOI] [PubMed] [Google Scholar]
- 2.Weiss LS, White JA. Macroglossia: A review. J La State Med Soc. 1990;142:13–6. [PubMed] [Google Scholar]
- 3.Ueyama Y, Mano T, Nishiyama A, Tsukamoto G, Shintani S, Matsumura T. Effects of surgical reduction of the tongue. Br J OralMaxillofac Surg. 1999;37:490–5. doi: 10.1054/bjom.1999.0196. [DOI] [PubMed] [Google Scholar]
- 4.Ruscello DM, Douglas C, Tyson T, Durkee M. Macroglossia: A case study. J Commun Disord. 2005;38:109–22. doi: 10.1016/j.jcomdis.2004.06.001. [DOI] [PubMed] [Google Scholar]
- 5.Myer CM, 3rd, Hotaling AJ, Reilly JS. The diagnosis and treatment of macroglossia in children. Ear Nose Throat J. 1986;65:444–8. [PubMed] [Google Scholar]
- 6.Vogel JE, Mulliken JB, Kaban LB. Macroglossia: A review of the condition and a new classification. Plast Reconstr Surg. 1986;78:715–23. [PubMed] [Google Scholar]
- 7.Marino MY, Vincente GM, Chua AH. Coblation for Congenital Macroglossia in Beckwith-Wiedemann Syndrome. Philipp J Otolaryngol Head Neck Surg. 2008;23:38–42. [Google Scholar]
- 8.Heggie AA, Vujcich NJ, Portnof JE, Morgan AT. Tongue reduction for macroglossia in Beckwith Wiedemann syndrome: Review and application of new technique. Int J Oral Maxillofac Surg. 2013;42:185–91. doi: 10.1016/j.ijom.2012.09.003. [DOI] [PubMed] [Google Scholar]
- 9.Kier WM, Smith KK. Tongues, tentacles and trunks. The biomechanics of muscular hydrostats. Zool J Linn Soc. 1985;83:307–24. [Google Scholar]
- 10.Mason RM, Serafin D. The Tongue: Multidisciplinary considerations. In: Serafin D, Georigiade NG, editors. Pediatric Plastic Surgery. 1st ed. St. Louis: C.V. Mosby; 1984. pp. 711–32. [Google Scholar]
- 11.Perkins JA. Overview of macroglossia and its treatment. Curr Opin Otolaryngol Head Neck Surg. 2009;17:460–65. doi: 10.1097/MOO.0b013e3283317f89. [DOI] [PubMed] [Google Scholar]
- 12.Kauffman Y, Cole P, McKnight A, Hatef DA, Hollier L, Edmonds J. A modified keyhole technique for correction of macroglossia. Plast Reconstr Surg. 2008;122:1867–69. doi: 10.1097/PRS.0b013e31818cc3ab. [DOI] [PubMed] [Google Scholar]
- 13.Hettinger PC, Denny AD. Double Stellate tongue reduction: A new method of treatment for macroglossia in patients with Beckwith-Wiedemann Syndrome. Ann Plast Surg. 2011;67:240–4. doi: 10.1097/SAP.0b013e3181f77a83. [DOI] [PubMed] [Google Scholar]
- 14.Kacker A, Honrado C, Martin D, Ward R. Tongue reduction in Beckwith-Weidemann syndrome. Int J Ped otorhinolaryngol. 200;3:1–7. doi: 10.1016/s0165-5876(00)00280-9. [DOI] [PubMed] [Google Scholar]
- 15.Gasparini G, Saltarel A, Carboni A, Maggiulli F, Becelli R. Surgical Management of macroglossia: Discussion of 7 cases. Oral Surg Oral Med Oral Pathol Oral radiol Endod. 2002;94:566–71. doi: 10.1067/moe.2002.127583. [DOI] [PubMed] [Google Scholar]
- 16.Wu CI, Chen PKT, Lin MS, Chou EK, Chang SCN. The modified method of tongue reduction in Beckwith-Wiedmann Syndrome. J Plast Surg Asso R.O.C. 2008;17:390–8. [Google Scholar]
- 17.Jian X. Surgical Management of Lymphangiomatous or Lymphangiohemangiomatous Macroglossia. J Oral Maxillofac Surg. 2005;63:15–19. doi: 10.1016/j.joms.2004.04.024. [DOI] [PubMed] [Google Scholar]
- 18.Kadouch DJ, Maas SM, Dubois L, van der Horst. Surgical treatment of macroglossia in patients with Beckwith–Wiedemann syndrome: A 20-year experience and review of the literature. Int J Oral Maxillofac Surg. 2012;41:300–8. doi: 10.1016/j.ijom.2011.10.021. [DOI] [PubMed] [Google Scholar]
- 19.Calabrese L, Giugliano G, Bruschini R, Ansarin M, Navach V, Grosso E, et al. Compartmental surgery in tongue tumours: Description of a new surgical technique. Acta Otorhinolaryngol Ital. 2009;29:259–64. [PMC free article] [PubMed] [Google Scholar]
- 20.Perkins JA, Shcherbatyy V, Liu Z. Morphologic and histologic outcomes of tongue reduction surgery in a animal model. Otolaryngol Head Neck Surg. 2008;139:291–7. doi: 10.1016/j.otohns.2008.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Saigusa H, Tanuma K, Yamashita K, Aino L, Saigusa M, Niimi S. Fiber arrangements of the vertical lingual muscle in human adult subjects. Eur J Anat. 2012;16:177–83. [Google Scholar]
- 22.Mu L, Sanders I. Human Tongue Neuroanatomy: Nerve Supply and Motor Endplates. Clin Anat. 2010;23:777–91. doi: 10.1002/ca.21011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hiiemae KM, Palmer JB. Tongue movements in feeding and speech. Crit Review Oral Biol Med. 2003;14:413–29. doi: 10.1177/154411130301400604. [DOI] [PubMed] [Google Scholar]
- 24.Scherbatyy V, Perkins JA, Liu Z. Internal Kinematics of the tongue following volume reduction. Anat Rec (Hoboken) 2008;291:886–93. doi: 10.1002/ar.20699. [DOI] [PMC free article] [PubMed] [Google Scholar]


