Abstract
Introduction:
So much has been written by so many about secondary procedures in cleft surgery that testify not only the complexity and variable expression of cleft deformity itself but also the need to find methods of primary surgery that will reduce, if not avoid, adverse effects on all the structures and functions involved and affected. It must be the principal aim of cleft surgeon to restore the deformed and displaced regional anatomy to as close to normality as possible, whether or not true hypoplasia exists. The pathogenesis of secondary deformities is related to specific features as: the presence of scar tissues into the cleft basal bone area, that inhibits alveolar growth; scarring of palatal soft tissue, that inhibits growth and causes palatal orientation of dentoalveolar elements; and the exceeding lip tension, that may inhibits maxillary growth along dentoalveolar structures.
Materials and Methods:
From 2008 to 2011 at the Department of Cranio-Maxillo-Facial Surgery, Santo Spirito Hospital, Rome 25 patients (21 males and 4 females) who had undergone previous surgery for unilateral cleft lip and palate (UCLP) and bilateral cleft lip and palate (BCLP) were enrolled in our study. Diagnosis of deformity was made by means of a cephalometric and photographic analysis (Arnett), gipsometry and a radiological assessment (orthopantomography, lateral and frontal cephalometric X-rays). Moreover, every patient was studied with a temporomandibular joint (TMJ) tomography, TMJ magnetic resonance imaging (MRI) and a computerized gnatography to better evaluate potential TMJ dysfunctions. The surgical procedures adopted simultaneously were: Total or segmental maxillomandibular osteotomies, genioplasty, rhinoplasty, labioplasty, and application of facial prosthesis. Every patient received a postoperative questionnaire to evaluate his/her satisfaction with the surgery performed.
Results:
The surgical procedures adopted were Le Fort I osteotomy and bilateral sagittal split osteotomy (BSSO) in 16 patients (65%) and only Le Fort I osteotomy in 9 patients (35%). A relapse of malformation occurred in 4.5% of cases. Concerning the patient questionnaire, 96% of patients were satisfied with the jaw surgery and favorable for combined surgery, 88% were satisfied with lip-nose surgery, and finally 76% would advise to a friend.
Conclusions:
Simultaneous correction of the deformities is indicated as to avoid several surgical distresses for the patient, to improve facial aesthetic and function in one surgical step, and to reduce risk of psychological consequences.
Keywords: Cleft lip and palate, maxillomandibular osteotomies, rhinoplasty, secondary surgery
INTRODUCTION
The field of cleft lip and palate surgery is full of controversy for several reasons. First, final assessment of treatment results must wait until the child is fully grown, as surgical maneuvers in children may have an important influence on facial growth. This long endpoint of treatment makes trials of different therapeutic options a very lengthy process. Another important factor is the difficulty of distinguishing whether a deformity is due to an inherent defect in tissues themselves or is a secondary effect of surgery. For example, is the deficiency in midfacial growth due to the tissues being hypoplastic and lacking in normal growth potential or is it an unwanted side effect of surgery on palate at an early age? A lack of uniformity in the choice of treatment modalities in a particular center, as well as changes of treatment protocol or random selection of treatment type with changing vogues in surgery, further hampers critical assessment and comparison of results.
As Ralph Millard said: “Know the normal, find it and place it in normal position, throw away nothing until it is proved useless, borrow from an area of excess to correct an area of need only when it can be afforded, do not get shackled in routine but look at each case individually […]”. According to the Authors (AA), any primary surgery may influence soft and hard tissues growth determining a typical facial feature. These deformities results in aesthetic and functional disturbances.
If we analyze natural history of facial growth in cleft lip and palate patients, we may observe the following features: A reduction of forces that oppose expansion (loss of bone and lip continuity) and a prevalence of expansive forces (tongue pressure and facial growth factors). Thus, an expansion of middle third of the face in horizontal dimension, with an almost normal sagittal growth, a normocclusion in molar and premolar regions with a normal dental eruption (except in the cleft area) occurs.[1,2,3] Once the primary surgery takes place, clinical features shows an abnormal growth of basal and alveolar maxillary bone combined with a horizontal incongruence of dentoalveolar arches which result in a complete malocclusion not limited to cleft area. Therefore, even if a good primary surgery has been performed, job is probably not over as secondary treatment has to deal with following specific issues: Dentoskeletal deformities, lip deformities, nose deformities, and hard and soft palate deformities[2,3,4,5,6,7,8,9,10] [Figures 1–3].
Figure 1.

(a, b) Frontal and oral views of a bilateral cleft lip and palate after primary surgery
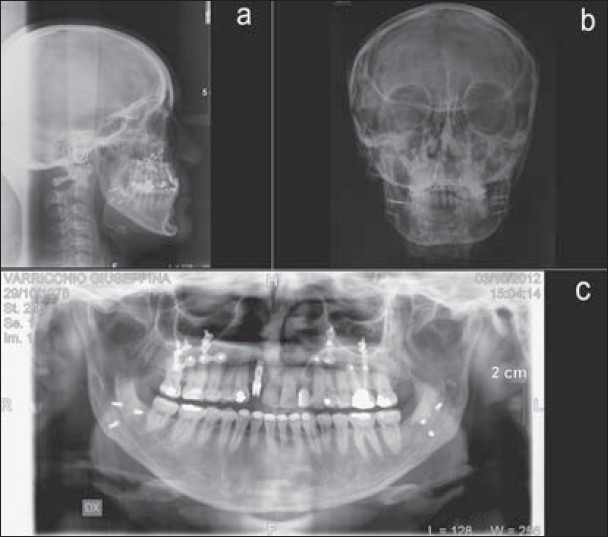
Figure 3.
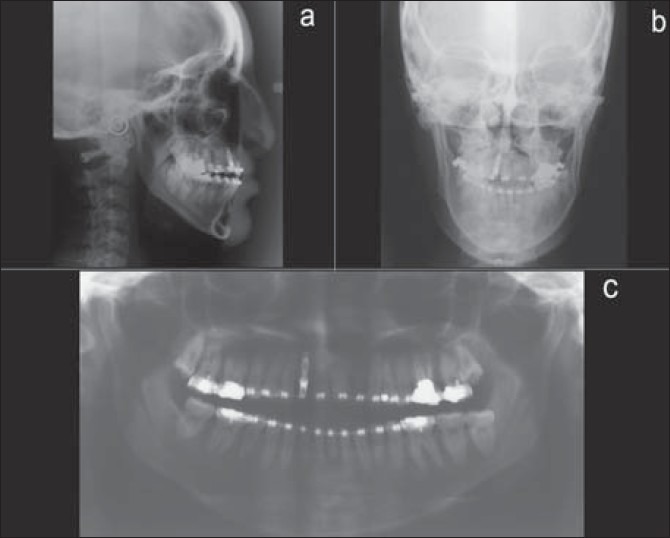
(a-c) Preoperative lateral and frontal cephalometric X-Rays and orthopantomography
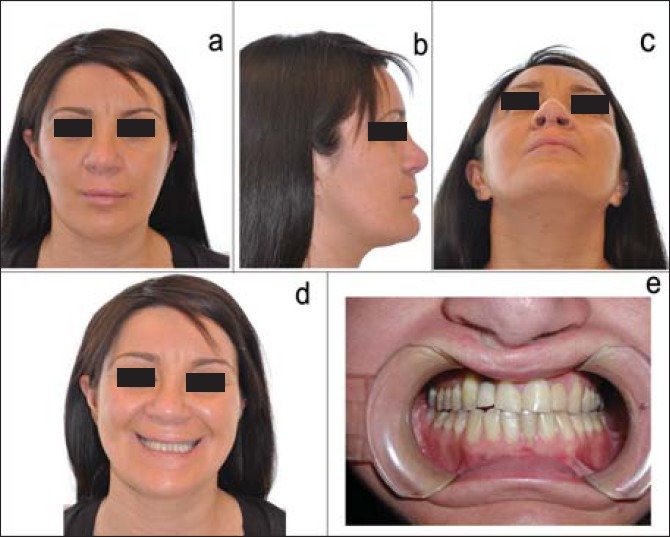
Figure 2.
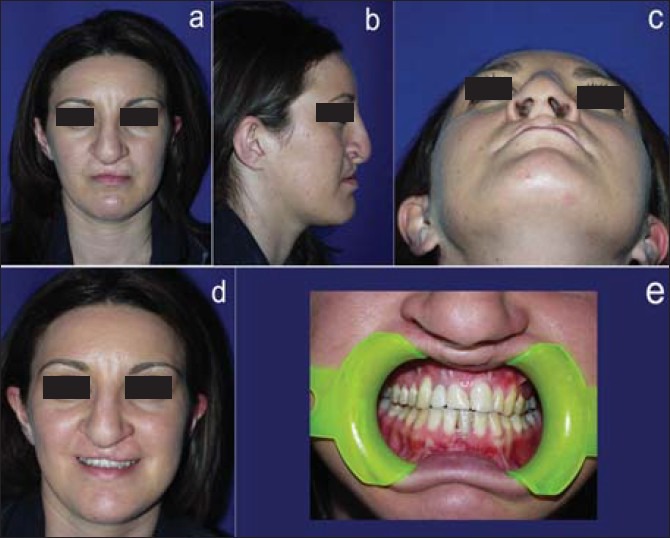
(a-e) 33-yrs old female affected by bilateral cleft lip and palate secondary deformity with a dento-skeletal class III and nose deformity. Preoperative frontal, lateral, axial, frontal smile and intraoral images
MATERIALS AND METHODS
From 2008 to 2011; at the Department of Cranio-Maxillo-Facial Surgery, Santo Spirito Hospital, Rome; 25 patients (21 males and 4 females) who had undergone previous surgery for unilateral cleft lip and palate (UCLP) and bilateral cleft lip and palate (BCLP) were enrolled in our study. All patients were over 18 years of age and were affected by a class III malocclusion (16 pts) and facial asymmetry (9 pts). Diagnosis of the deformity was made by means of a cephalometric and photographic analysis (Arnett) and gipsometry and a radiological assessment (orthopantomography, lateral and frontal cephalometric X-rays). Moreover, every patient was studied with a temporomandibular joint (TMJ) tomography, TMJ magnetic resonance imaging (MRI), and a computerized gnatography to better evaluate potential TMJ dysfunctions. The surgical procedures adopted simultaneously were: Total or segmental maxillomandibular osteotomies, genioplasty, rhinoplasty, labioplasty, and application of facial prosthesis. The short follow-up was at 1, 6, and 12 months after surgery and long-term follow-up at 24 months consisting in: A clinical evaluation (cephalometric analysis and photographic study), a morphostructural evaluation with orthopantomography and lateral and frontal cephalometric X-rays, and a functional evaluation with a computerized gnatography. Finally, every patient received a postoperative questionnaire to evaluate his/her satisfaction with the surgery performed.
RESULTS
In the immediate postoperative period, no patients showed signs of infections of surgical wounds or other major complications. The surgical procedures adopted were Le Fort I osteotomy and bilateral sagittal split osteotomy (BSSO) in 16 patients (65%) and only Le Fort I osteotomy in patients (35%). A relapse of malformation occurred in 4.5% of cases. Every patient was treated with rubber bands for almost 2 weeks after surgery to reestablish new occlusion and muscle function [Figures 4–10]. Concerning the patient questionnaire, 96% of patients were satisfied with the jaw surgery and favorable for combined surgery, 88% were satisfied with lip-nose surgery, and finally 76% would advise to a friend.
Figure 4.
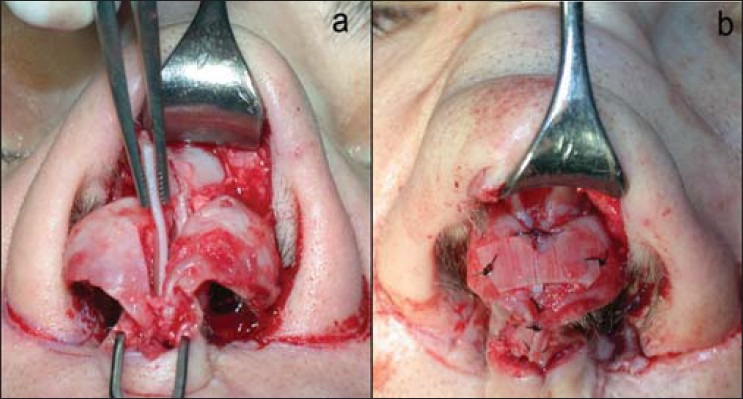
(a-b) Particulars of the simultaneous surgery: Open Rhinoplasty
Figure 10.
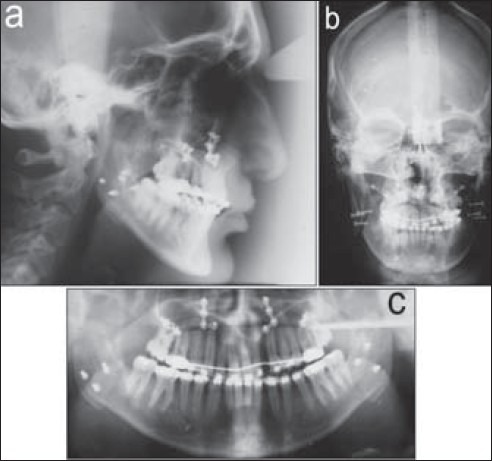
(a-c) Postoperative lateral and frontal cephalometric X-rays and orthopantomography
Figure 5.
(a-e) Postoperative frontal, lateral, axial, frontal smile and intraoral images after Le Fort I osteotomy (upward 1 mm, forward 1 mm right, 3 mm left), bilateral sagittal split osteotomy, open rhinoplasty and upper lip coleman graft
Figure 6.
(a-c) Postoperative lateral and frontal cephalometric X-rays and orthopantomography
Figure 7.
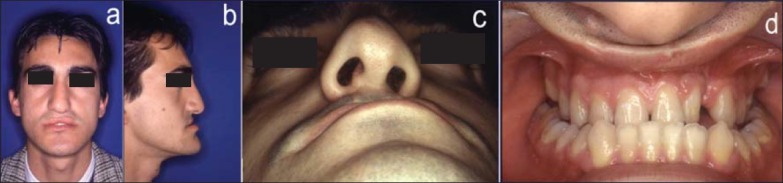
(a-d) 23 yrs old male affected by a lip-nose secondary deformity and vertical and horizontal maxillary hypoplasia and right hemimandibular elongation
Figure 8.
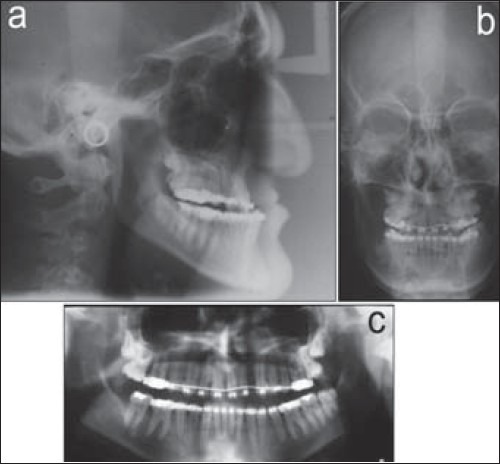
(a-c) Preoperative lateral and frontal cephalometric X-rays and orthopantomography
Figure 9.

(a-d) Frontal, lateral, axial and oral views after Le Fort I osteotomy (2 mm forward, 3 mm upward), sagittal split osteotomy, open rhinoplasty and cheiloplasty with tongue graft
DISCUSSION
So much has been written by so many about secondary procedures in cleft surgery that testify not only the complexity and variable expression of cleft deformity itself but also the need to find methods of primary surgery that will reduce, if not avoid, adverse effects on all the structures and functions involved and affected. It must be the principal aim of cleft surgeon to restore deformed and displaced regional anatomy to as close to normality as possible, whether or not true hypoplasia exists.[4,5,6] Only in this way restoration of function might be reasonably expected, thus enabling optimal growth and development. Primary surgical methods encompassing these ideals should, theoretically, reduce frequently observed sequelae of both cleft deformity and surgery and so, in turn, the need of secondary surgery. In reality, even in the most favorable circumstances, secondary surgery will be required.[7,8,9]
Ideally, secondary deformities of cleft lip and palate are therefore best managed by adopting a method of primary surgery that not only recognizes inherent problems, but prevents them from occurring. Veau introduced the concept of embryological surgery (embodied somewhat later by Millard): The surgeon must have a full understanding of all anatomic elements involved in cleft deformity, should seek to improve surgical methods where failure seems to be apparent and must make every attempt to restore to normality all tissues involved in cleft and, above all, underlying musculature, rather than just confining activity to overlying skin. Moreover, Delaire's anatomic studies and subsequent development of a surgical technique confirmed presence of a median cellular septum which establishes a functional connection between lip and premaxilla in the midline, inserting into the interincisive suture, and drawing together anterior midline structures of the midface. Further studies by Joos using MRI confirmed the relationship of anterior facial musculature to underlying structures and further stressed importance of early restoration of these structures if one has to reduce the need for multiple secondary procedures.[11,12,13]
Other significant contributions to correction of secondary deformities have been made by surgeons emphasizing the importance of early correction of lip-nose deformity, all of whom, like Delaire, adopt a radical approach to correction of nasal cartilaginous deformity as part of their primary procedure. In this way not only further interventions are potentially reduced but also later corrections might be based on a sound anatomic foundation and do not compound an already incorrect previous repair.[14,15,16]
The pathogenesis of secondary deformities is related to specific features as: The presence of scar tissues into cleft basal bone area, that inhibits alveolar growth; scarring of palatal soft tissue, that inhibits growth and causes palatal orientation of dentoalveolar elements; the exceeding lip tension, that may inhibit maxillary growth along dentoalveolar structures. Clinically, it is possible to observe obvious signs of failure of midfacial growth, in terms of an horizontal disproportion of dentoalveolar arches and malocclusion not limited to cleft area, collapse or deviation of nasal structures and evidence of muscle dysfunction including an inability to protrude the upper lip, whether symmetrically or asymmetrically; persistent oronasal fistulae, recurrent bouts of secretory otitis media, and failure of normal speech and language development. All these complications of dysfunction are equally important and need to be corrected at the earliest possible opportunity. Clearly; the earlier secondary revisional procedures are carried out; the less will be the adverse effect on growth, development, and psychological concerns.[8,9,10,11,12,13,14,15,16,17,18,19,20,21] However, even when growth has ceased, every opportunity to improve dysfunction should be taken. Moreover as Ralph Millard said: “If the secondary surgeon could be guided by such simple, sound dicta as: Never make the same mistake twice; two wrongs do not make a right; when in doubt, don’t! The tertiary surgeon would have little or nothing to do”.
According to the AA, simultaneous surgery should be performed with the aim of reducing surgical stress of the patient, improving aesthetic and functional outcomes in one surgical step and reducing risk of psychological consequences. Furthermore, simultaneous surgery should be performed at the end of facial growth (17 years in females and 18 years in males), but should be avoided in case of wide bone loss in cleft areas and velopharyngeal insufficiency.[22,23,24,25]
CONCLUSION
Of major importance in management of cleft lip and palate is the adoption of a primary surgical approach that will minimize those sequelae commonly associated with surgery; an approach which will also promote function; and therefore, growth and development. Despite the availability of several techniques and the significant improvements in primary correction, mostly in bilateral cleft lip and palate, secondary deformities and lip revision commonly occur.
Finally, according to the AA, simultaneous correction of deformities is indicated as to avoid several surgical distresses for patient, to improve facial aesthetic and function in one surgical step, and to reduce the risk of psychological consequences.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Broome M, Herzog G, Hohlfeld J, de Buys Roessingh A, Jaques B. Influence of the primary cleft palate closure on the future need for orthognathic surgery in unilateral cleft lip and palate patients. J Craniofac Surg. 2010;21:1615–8. doi: 10.1097/SCS.0b013e3181ef2eed. [DOI] [PubMed] [Google Scholar]
- 2.Voshol IE, van der Wal KG, van Adrichem LN, Ongkosuwito EM, Koudstaal MJ. The frequency of le fort I osteotomy in cleft patients. Cleft Palate Craniofac J. 2012;49:160–6. doi: 10.1597/09-224. [DOI] [PubMed] [Google Scholar]
- 3.Meazzini M, Lematti L, Mazzoleni F, Rabbiosi D, Bozzetti A, Brusati R. Vertical excess of the premaxilla in bilateral cleft lip and palate patients: A protocol for treatment. J Craniofac Surg. 2010;21:499–502. doi: 10.1097/SCS.0b013e3181cffb4d. [DOI] [PubMed] [Google Scholar]
- 4.Jeblaoui Y, Morand B, Brix M, Lebeau J, Bettega G. Maxillary distraction complications in cleft patients. Rev Stomatol Chir Maxillofac. 2010;111:e1–6. doi: 10.1016/j.stomax.2010.04.005. [DOI] [PubMed] [Google Scholar]
- 5.Chua HD, Whitehill TL, Samman N, Cheung LK. Maxillary distraction versus orthognathic surgery in cleft lip and palate patients: Effects on speech and velopharyngeal function. Int J Oral Maxillofac Surg. 2010;39:633–40. doi: 10.1016/j.ijom.2010.03.011. [DOI] [PubMed] [Google Scholar]
- 6.Chua HD, Hägg MB, Cheung LK. Cleft maxillary distraction versus orthognathic surgery--which one is more stable in 5 years? Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:803–14. doi: 10.1016/j.tripleo.2009.10.056. [DOI] [PubMed] [Google Scholar]
- 7.Chong DK, Portnof JE, Xu H, Salyer KE. Reviewing the orthognathic surgical care of the patient with cleft lip and palate: The single surgeon experience. J Craniofac Surg. 2009;20(Suppl 2):1895–904. doi: 10.1097/SCS.0b013e3181b6c69f. [DOI] [PubMed] [Google Scholar]
- 8.Tindlund RS, Holmefjord A, Eriksson JC, Johnson GE, Vindenes H. Interdisciplinary evaluation of consecutive patients with unilateral cleft lip and palate at age 6, 15, and 25 years: A concurrent standardized procedure and documentation by plastic surgeon; speech and language pathologist; ear, nose, and throat specialist; and orthodontist. J Craniofac Surg. 2009;20(Suppl 2):1687–98. doi: 10.1097/SCS.0b013e3181b3edb5. [DOI] [PubMed] [Google Scholar]
- 9.Daskalogiannakis J, Mehta M. The need for orthognathic surgery in patients with repaired complete unilateral and complete bilateral cleft lip and palate. Cleft Palate Craniofac J. 2009;46:498–502. doi: 10.1597/08-176.1. [DOI] [PubMed] [Google Scholar]
- 10.Meazzini MC, Giussani G, Morabito A, Semb G, Garattini G, Brusati R. A cephalometric intercenter comparison of patients with unilateral cleft lip and palate: Analysis at 5 and 10 years of age and long term. Cleft Palate Craniofac J. 2008;45:654–60. doi: 10.1597/07-098.1. [DOI] [PubMed] [Google Scholar]
- 11.Wolford LM, Cassano DS, Cottrell DA, El Deeb M, Karras SC, Goncalves JR. Orthognathic surgery in the young cleft patient: Preliminary study on subsequent facial growth. J Oral Maxillofac Surg. 2008;66:2524–36. doi: 10.1016/j.joms.2008.06.104. [DOI] [PubMed] [Google Scholar]
- 12.Chigurupati R. Orthognathic surgery for secondary cleft and craniofacial deformities. Oral Maxillofac Surg Clin North Am. 2005;17:503–17. doi: 10.1016/j.coms.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 13.Ruiz-Rodríguez R, López-Noriega JC. Reoperations in cleft lip and cleft palate treatment. Oral Maxillofac Surg Clin North Am. 2011;23:169–76. doi: 10.1016/j.coms.2010.12.002. viii. [DOI] [PubMed] [Google Scholar]
- 14.Nakamura N, Sasaguri M, Okawachi T, Nishihara K, Nozoe E. Secondary correction of bilateral cleft lip nose deformity-Clinical and three-dimensional observations on pre- and postoperative outcome. J Craniomaxillofac Surg. 2011;39:305–12. doi: 10.1016/j.jcms.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 15.Chaithanyaa N, Rai KK, Shivakumar HR, Upasi A. Evaluation of the outcome of secondary rhinoplasty in cleft lip and palate patients. J Plast Reconstr Aesthet Surg. 2011;64:27–33. doi: 10.1016/j.bjps.2010.03.044. [DOI] [PubMed] [Google Scholar]
- 16.Wang TD. Secondary rhinoplasty in unilateral cleft nasal deformity. Clin Plast Surg. 2010;37:383–7. doi: 10.1016/j.cps.2009.12.013. [DOI] [PubMed] [Google Scholar]
- 17.Gosain AK, Fathi AH. Assessment of secondary cleft rhinoplasty using resorbable plates at the age of primary school. J Craniofac Surg. 2009;20(Suppl 2):1801–5. doi: 10.1097/SCS.0b013e3181b5d4c0. [DOI] [PubMed] [Google Scholar]
- 18.Nakamura N, Okawachi T, Nishihara K, Hirahara N, Nozoe E. Surgical technique for secondary correction of unilateral cleft lip-nose deformity: Clinical and 3-dimensional observations of preoperative and postoperative nasal forms. J Oral Maxillofac Surg. 2010;68:2248–57. doi: 10.1016/j.joms.2009.06.012. [DOI] [PubMed] [Google Scholar]
- 19.Smolka K, Eggernsperger N, Iizuka T, Smolka W. Evaluation of secondary functional cheilorhinoplasty during growth of cleft patients with residual lip and nasal deformities. J Oral Maxillofac Surg. 2008;66:2577–84. doi: 10.1016/j.joms.2008.06.044. [DOI] [PubMed] [Google Scholar]
- 20.Vanwijck R, Bayet B, Roffé JL, Compère JF, Benateau H. Labial sequels after uni- and bilateral cleft lip repair. Rev Stomatol Chir Maxillofac. 2007;108:265–74. doi: 10.1016/j.stomax.2007.06.016. [DOI] [PubMed] [Google Scholar]
- 21.Yin NB, Gao F, Wang YQ, Song T, Li HD. Correction of secondary bilateral complete cleft lip and whistling deformities: The advance and rearrangement of the bilateral lip tissues. Aesthetic Plast Surg. 2011;35:750–5. doi: 10.1007/s00266-011-9682-3. [DOI] [PubMed] [Google Scholar]
- 22.Hellings PW, Hens G, Schoenaers J, Jorissen M, Vander Poorten V. Unique approach to secondary cleft-lip rhinoplasty in facial plastic surgery. B-ENT. 2010;6(Suppl 15):97–101. [PubMed] [Google Scholar]
- 23.Jung DH, Chang GU, Baek SH, Lee YK, Choi JY. Subnasale flap for correction of columella base deviation in secondary unilateral cleft lip nasal deformity. J Craniofac Surg. 2010;21:146–50. doi: 10.1097/SCS.0b013e3181c46bd8. [DOI] [PubMed] [Google Scholar]
- 24.Kim YS, Cho HW, Park BY, Jafarov M. A comparative study of the medial crura of alar cartilages in unilateral secondary cleft nasal deformity: The validity of medial crus elevation. Ann Plast Surg. 2008;61:404–9. doi: 10.1097/SAP.0b013e318168db1c. [DOI] [PubMed] [Google Scholar]
- 25.Mutaf M, Günal E, Türkmen A, Sunay M. Correction of tethered upper lip deformity following bilateral cleft lip repair. Ann Plast Surg. 2011;66:627–32. doi: 10.1097/SAP.0b013e3181eb33fc. [DOI] [PubMed] [Google Scholar]


