Abstract
Congenital muscular torticollis (CMT) is a rare congenital musculoskeletal disorder characterized by unilateral shortening of the sternocleidomastoid muscle (SCM). It presents in newborn infants or young children with reported incidence ranging from 0.3% to 2%. Owing to effective shortening of SCM on the involved side there is ipsilateral head tilt and contralateral rotation of the face and chin. This article reports a case of CMT in a 3½-year-old male child successfully managed by surgical release of the involved SCM followed by physiotherapy.
Keywords: Congenital, sternocleidomastoid muscle, tenotomy, torticollis
INTRODUCTION
The term torticollis is derived from the Latin words tortus, meaning “twisted” and collum, meaning “neck.” Tubby in 1912 first defined it as “a deformity, congenital or acquired in origin, characterized by lateral inclination of the head to shoulder, with torsion of the neck and deviation of the face.”[1] Congenital muscular torticollis (CMT) is a painless condition caused due to unilateral shortening of the sternocleidomastoid muscle (SCM) usually presenting during infancy. It is seen in 0.3-1.9% of all live births.[2] Due to effective shortening of SCM on the involved side there is ipsilateral head tilt and contralateral rotation of the face and chin.
Numerous theories have been proposed, but the true etiology of CMT remains uncertain. Various causes implicated for CMT includes intrauterine crowding or vascular phenomenon, fibrosis from peripartum bleeds, compartment syndrome, primary myopathy of the SCM and traumatic delivery.[3,4]
When diagnosed early, CMT can be managed conservatively, seldom requiring surgery. In children older than 1 year, corrective surgery has both cosmetic and functional benefits, the best outcomes being obtained between the ages of 1 and 4.[5] This article reports a case of CMT successfully managed by bipolar SCM tenotomy.
CASE REPORT
A 3½-year-old male child presented with the complaint of neck stiffness and restricted head movement. On examination head tilt to the right with chin deviation to the left was noted [Figure 1]. There was a significant restriction of neck movement, especially on lateral rotation. There was no obvious facial asymmetry. On palpation right SCM muscle was non-tender, taut and cord like. No lump or mass could be palpated along the entire muscle length. Systemic evaluation revealed no abnormality. Radiographs of the cervical spine, hips and lower extremities were normal. No neurological or ophthalmologic deficit could be elicited. Based on the above findings, a clinical diagnosis of CMT was established.
Figure 1.

Preoperative clinical photograph showing the child with congenital muscular torticollis affecting the right sternocleidomastoid muscle
Physiotherapy was started for the patient to achieve SCM muscle stretching. However, after 8 weeks of exercise, there was no improvement in the condition. Subsequently release of unilateral SCM by bipolar tenotomy was planned. Patient was prepared and taken up for the surgery under general anesthesia. A 2 cm incision was made below the mastoid on the right side. The attachment of SCM muscle to mastoid bone was identified and completely stripped from its bony attachment, protecting the underlying vital structures and overlying greater auricular nerve. A transverse incision of about 2.5 cm was placed above the clavicle-sternum junction on the right side and the platysma was incised. Both the heads of SCM were identified and then divided under direct vision together with deep fascia. The muscle was allowed to retract. The Sternal end was sutured to the clavicular cut end in an oblique line using 4/0 vicryl suture. Hemostasis was attained and skin closed by 4/0 prolene. Complete neck extension was achieved without any strain [Figure 2].
Figure 2.
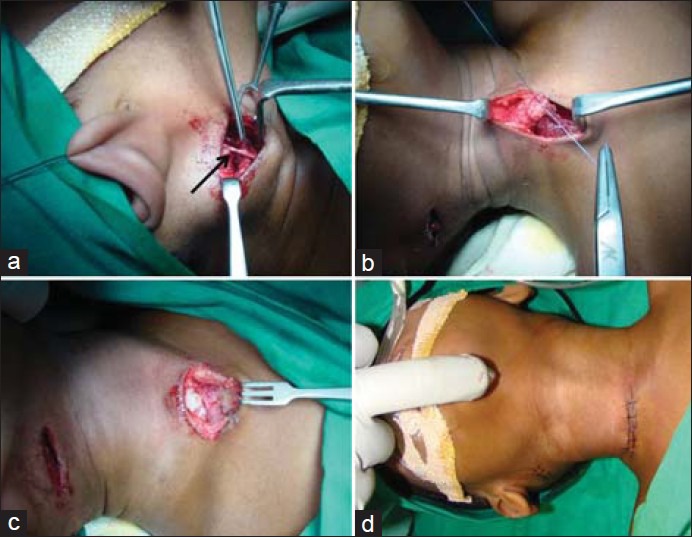
Intraoperative photographs. (a) Incision place over mastoid region, the overlying greater auricular nerve (arrow) was identified and protected during dissection. (b) Bot h the clavicular and sternal heads of the sternocleidomastoid muscle were identified and then divided. Sternal end was then sutured to the clavicular cut end in an oblique line to achieve muscle lengthening. (c) The excised lower end of SCM. (d) Closure done and complete neck extension was achieved without any strain intraoperatively
Patient was immobilized in the corrected position with adjustable torticollis brace from third postoperative day [Figure 3]. Simultaneously, the patient was referred to physiotherapist and a rigorous regimen of exercise involving head and neck manipulation through the full range of motion was given for a period of 12 weeks, 3 times every week. Patient at 12 months review shows the complete range of head and neck movements with no head tilt and neck stiffness [Figure 4].
Figure 3.

Torticollis brace worn by the patient postoperatively
Figure 4.

At 12 months postoperative photographs showing straight neck with a normal range of neck movement
DISCUSION
CMT is a distinct entity, the primary pathological characteristics of which are limited to the SCM. It is also sometimes referred to as wry-neck, stiff-neck, caput obstipum, crooked-neck and twisted-neck.
The reported incidence of CMT varies from 0.3% to 2% with overall incidence that can be as high as 1 in 250 live births.[6,7,8] Cheng in a review of 624 cases of infantile torticollis reported slight male predominance of 3:2. The right side was more commonly affected.[6]
The etiology of CMT and pathophysiology behind SCM impairment is still unknown. Prominent theories behind SCM muscle impairment in CMT include intrauterine crowding, muscle trauma during a difficult delivery, soft-tissue compression leading to compartment syndrome and congenital abnormalities of soft-tissue differentiation within the SCM muscle. Histologic studies of resected surgical specimens have demonstrated edema, degeneration of SCM muscle fibers and fibrosis.[9]
The most common presentation of child with CMT is a head tilt toward the affected side and the chin pointing to the contralateral side. Plagiocephaly is reported in up to 90% of children with CMT. With continued unilateral weight bearing, the skull base and cranium deform so that the vertex view reveals a parallelogram shaped head. If not treated it may lead to craniofacial growth deformity in adult. Children with CMT can be subdivided into three clinical subgroups. Group 1 is the sternocleidomastoid tumor group, which consists of torticollis with a palpable pseudotumor or swelling in the body of SCM. This is a hard, movable mass within the substance of the SCM noted at birth. This mass is usually located in the middle to lower third of the sternal portion of SCM. The pseudotumor usually becomes large after its first noted and then slowly resolves over a period of 5-21 months. This is the most common presentation and contributes to 28.2-47.2% of diagnosed cases of CMT in infants.[10] Group 2, known as muscular torticollis, consists of torticollis with tightness of the SCM, but no palpable tumor. The last group, Group 3 (also known as POST), is a postural torticollis without a mass or tightness of the SCM, as seen in this case.[11] In an alternative system of classification, pseudotumor of infancy and CMT are described as a separate diagnosis.[12]
Though SCM contracture is the most common cause of torticollis in children, other congenital and developmental causes should be ruled out. Other causes of torticollis in children have been classified as osseous (occipitocervical dysfunction, cervical vertebral dysfunction), nonosseous (Sandifer syndrome) and neurogenic (central nervous system tumors, ocular torticolis).[13]
Ultrasound is the imaging modality of choice for radiographic evaluation of CMT. The normal SCM on ultrasound presents as a hypoechoic mass with echogenic lines, indicating muscle fascicles running throughout its length. The presence of a SCM tumor affects not only the size of the muscle noted on ultrasound, but also its signal intensity. CMT muscles tend to be more hyperechogenic.[9]
Treatment of infants with torticollis is guided by the age of infant, the severity of torticollis, the diagnosis of plagiocephaly and the presence of associated neuromuscular or orthopedic impairment. Approximately, 50-70% of SCM tumors resolve spontaneously during the 1st year of life with the minimal residual defect.[9] Detailed evaluation to confirm the diagnosis and routine follow-up to study its progression is essential at this stage. Early physical therapy is initiated if there is any lack of rotation from fibrosis. Manual stretches are performed in flexion/extension, lateral bending, as well as in rotation. Sets of 15 stretches, holding the stretch for 1 secs, with a 10 secs rest in between is done 3 times/week. During the manual stretching, a snapping sensation may be heard and felt.[14] This sensation is caused by tearing of the SCM and may be associated with bruising. Despite the muscle trauma, patients still do remarkably well. Cervical collars could be necessary adjuncts used to restrain the neck in its normal position. Active physiotherapy regimen as described above was given for our patient preoperatively. However, the deformity did not improve and was persistent, prompting us to plan for surgical release of the SCM muscle.
Various surgical procedures reported for management of CMT includes, unipolar SCM muscle lengthening, bipolar SCM muscle lengthening, Z lengthening or radical resection of the SCM.[9] The choice of procedure is determined by the surgeon's preferences as well as to a lesser degree by the amount of SCM tightness. Bipolar release of SCM was planned for our case looking at the resistant nature of the deformity after physiotherapy and age of the patient. Postoperatively, the patient was put on torticollis braces and active physiotherapy regimen to prevent relapse and maintain the normal range of neck movement. At 12 months review, the patient showed complete range of the head and neck movements with no head tilt and neck stiffness.
Besides physiotherapy and surgery or combination of both, other treatment modalities have also been reported. Joyce and de Chalain[15] have published their intermediate follow-up of treatment of recalcitrant CMT by botulinum toxin (Botox). Botox could enhance the effectiveness of stretching of SCM on the side of contracture and allow strengthening of the overstretched and weakened muscle on the opposite side of the neck. Although Botox has promising potential, it carries the risk of systemic diffusion, hematoma formation, as well as neck pain.
In CMT, early diagnosis and physical therapy result in the best outcome. However, for resistant cases or in those treated after the age of one, surgical lengthening or release of SCM Muscle is necessary.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Tubby AH. 2nd ed. Vol. 1. London, England: MacMillan; 1912. Deformities and Diseases of Bones and Joints; p. 56. [Google Scholar]
- 2.Wei JL, Schwartz KM, Weaver AL, Orvidas LJ. Pseudotumor of infancy and congenital muscular torticollis: 170 cases. Laryngoscope. 2001;111:688–95. doi: 10.1097/00005537-200104000-00023. [DOI] [PubMed] [Google Scholar]
- 3.Davids JR, Wenger DR, Mubarak SJ. Congenital muscular torticollis: Sequela of intrauterine or perinatal compartment syndrome. J Pediatr Orthop. 1993;13:141–7. [PubMed] [Google Scholar]
- 4.Tang S, Liu Z, Quan X, Qin J, Zhang D. Sternocleidomastoid pseudotumor of infants and congenital muscular torticollis: Fine-structure research. J Pediatr Orthop. 1998;18:214–8. [PubMed] [Google Scholar]
- 5.Hollier L, Kim J, Grayson BH, McCarthy JG. Congenital muscular torticollis and the associated craniofacial changes. Plast Reconstr Surg. 2000;105:827–35. doi: 10.1097/00006534-200003000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Cheng JC, Au AW. Infantile torticollis: A review of 624 cases. J Pediatr Orthop. 1994;14:802–8. [PubMed] [Google Scholar]
- 7.Colonna P. Congenital torticollis. Va Med Mon (1918) 1927;53:794–6. [Google Scholar]
- 8.Coventry MB, Harris LE. Congenital muscular torticollis in infancy; some observations regarding treatment. J Bone Joint Surg Am. 1959;41-A:815–22. [PubMed] [Google Scholar]
- 9.Do TT. Congenital muscular torticollis: Current concepts and review of treatment. Curr Opin Pediatr. 2006;18:26–9. doi: 10.1097/01.mop.0000192520.48411.fa. [DOI] [PubMed] [Google Scholar]
- 10.Ballock RT, Song KM. The prevalence of nonmuscular causes of torticollis in children. J Pediatr Orthop. 1996;16:500–4. doi: 10.1097/00004694-199607000-00016. [DOI] [PubMed] [Google Scholar]
- 11.Loder RT. Congenital abnormalities of the cervical spine. In: Frymoyer JW, Wiesel SW, editors. The Adult and Pediatric Spine. 3rd ed. Philadelphia: Lippincott Williams and Wilkins; 2004. pp. 605–17. [Google Scholar]
- 12.Porter SB, Blount BW. Pseudotumor of infancy and congenital muscular torticollis. Am Fam Physician. 1995;52:1731–6. [PubMed] [Google Scholar]
- 13.Berlin H. The differential diagnosis and management of torticollis in children. Phys Med Rehabil Clin N Am. 2000;14:197–206. [Google Scholar]
- 14.Cheng JC, Chen TM, Tang SP, Shum SL, Wong MW, Metreweli C. Snapping during manual stretching in congenital muscular torticollis. Clin Orthop Relat Res. 2001;384:237–44. doi: 10.1097/00003086-200103000-00028. [DOI] [PubMed] [Google Scholar]
- 15.Joyce MB, de Chalain TM. Treatment of recalcitrant idiopathic muscular torticollis in infants with botulinum toxin type A. J Craniofac Surg. 2005;16:321–7. doi: 10.1097/00001665-200503000-00023. [DOI] [PubMed] [Google Scholar]


