Abstract
Background:
Roughly 3 million children die every year of vaccine preventable diseases and a significant number of these children live in developing countries. The present study was conducted to assess the reasons for failure of immunization among 12-23-month-old children of Lucknow city in India.
Materials and Methods:
Out of all villages in rural areas and mohallas in urban areas of Lucknow district, eight villages and eight mohallas were selected by simple random sampling. A community based cross-sectional study was done among 450 children aged 12-23 months. The immunization status of the child was assessed by vaccination card and by mother's recall. A pre-designed and pre-tested questionnaire was used to elicit information on reasons for failure of immunization. Data was analysed using statistical package for social services (SPSS) version 11.5. Chi square test was used to find out the significant association.
Results:
Overall, 62.7% children were fully immunized, 24.4% children were partially immunized, and 12.9% children were not immunized. The major reasons for failure of immunization were postponing it until another time, child being ill and hence not brought to the centre for immunization, unaware of the need of immunization, place of immunization being too far, no faith in immunization, unaware of the need to return for 2nd and 3rd dose, mother being too busy, fear of side reactions, wrong ideas about immunization, and polio was considered only vaccine, and others.
Conclusion:
More awareness should be generated among the people living in rural and urban areas to immunize their children.
Keywords: 12-23 months children, immunization status, reasons for failure
INTRODUCTION
Immunization is a significant, cost effective, and important public health intervention measure to prevent disease. Roughly 3 million children die every year of vaccine preventable diseases (VPDs) and a significant number of these children live in developing countries. Recent estimates suggest that approximately 34 million children are not completely immunized, with almost 98% of them living in developing countries. Effective immunization has reduced the morbidity and mortality of children due to VPD to a great extent worldwide. Eradication of small pox is a glaring example of the success of vaccination.
National Family Health Survey (NFHS) III cites that national full immunization coverage against the six expanded programme on immunization (EPI) vaccines in the age group of 12-23 months is only 47.3%, ranges from 13% in Nagaland to 91% in Tamil Nadu. Uttar Pradesh (U.P.), Bihar, Madhya Pradesh (M.P.), Rajasthan, and northeastern states have the majority of the non-immunized children in India. In U.P., only 23% children aged 12-23 months have undergone full immunization.
A study in different states of India showed that 63.3% children were fully immunized, 27.1% were partially immunized, and 9.6% were unimmunized.[1] Another study in urban slums of Lucknow district showed that only 44.1% children were fully immunized, while 32% were partially immunized, and 23.9% were unimmunized.[2]
Lucknow is centrally placed district of U.P., spread over an area of 2544 km2, which constitute 0.86% of the total area of the country. In 2001, the district Lucknow had a population of about 36,47,834, with 13,26,873 living in rural areas and 23,20,961 in urban areas and a female to male ration of 888:1000. Main languages spoken in the district are Hindi and Urdu. DLHS-III observed that 51.1% of children in Lucknow were fully immunized.
The present study was conducted to assess the reasons for failure of immunization among 12-23-month old children in rural and urban areas of Lucknow.
MATERIALS AND METHODS
List of all villages in rural areas and mohallas in urban areas of Lucknow district was procured. Eight villages and eight mohallas were selected by simple random sampling. A community based cross-sectional study was done among 450 children aged 12-23 months.
First, the sample size of 450 was divided equally into urban and rural areas. Then, the number of household to be taken for the survey in each village and mohallas was decided according to Probability Proportionate to Size (PPS) technique. Simple random sampling (using last digit of currency) was used to select the first household for the survey. Then, every household with a child of 12-23 months were surveyed till the desired number of children were met from that village or mohalla.
Help of Auxillary Nurse Midwife (ANM), Anganwadi Worker (AWW), and Accredited Social Health Activist (ASHA) was taken to build a rapport with local people. Mother of the child was preferred as the primary respondent. In the absence of mother, the father was taken as the respondent. In case of absence of both of them, the adult in the household who remained with the child for most of the time, was taken as respondent. Help of other available adult member of the household or nearby household was also taken.
The immunization status of the child was assessed by vaccination card and by mother's recall where vaccination card was not available.
The immunization status of the children was categorized as follows:
Fully immunized: When the child had received Bacillus Calmette–Guérin (BCG), three doses of diphtheria, pertussis (whooping cough), and tetanus (DPT), and three doses of oral polio vaccine (OPV) and measles vaccine
Partially immunized: When the child had received some but not all vaccines
Not immunized: When the child had not received any of the vaccine.
A pre-designed and pre-tested questionnaire was used to assess the reasons for non-immunization and partial immunization of the child.
RESULTS
Table 1 shows that, overall, 282 (62.7%) children were fully immunized, 110 (24.4%) were partially immunized, and 58 (12.9%) were not immunized. In urban areas, 127 (56.4%) children were fully immunized, while 56 (24.9%) were partially immunized, and 42 (18.7%) were not immunized. In rural areas, 155 (68.9%) children were fully immunized, while 54 (24%) were partially immunized, and 16 (7.1%) were not immunized.
Table 1.
Immunization status of the study population
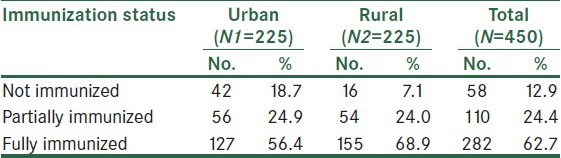
Figure 1 shows the overall vaccination coverage of each individual vaccine as well as the coverage in urban and rural areas. Overall BCG vaccination coverage was 87.60%, while, in urban and rural areas, it was 82.70% and 92.40%, respectively. OPV 3 vaccination coverage was 67.60% and 84.50% in urban and rural areas, respectively, while overall it was 76%. DPT 3 vaccination coverage was 67.10% and 84.40% in urban and rural areas, respectively, while overall it was 75.80%. Overall measles vaccination coverage was 62.20%, while, in urban and rural areas, it was 56.40% and 68%, respectively.
Figure 1.
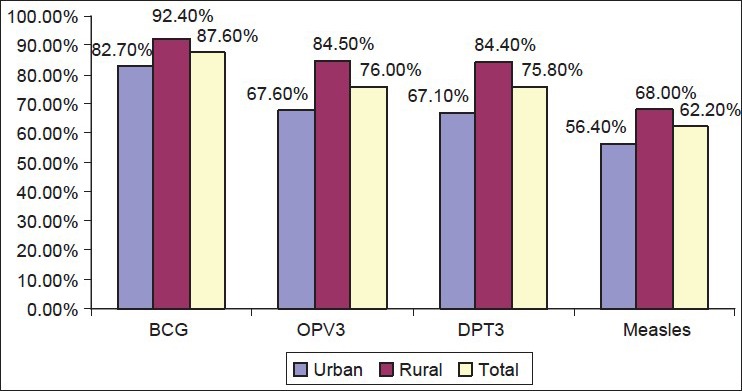
Vaccination coverage of individual vaccines
Table 2 shows the dropout rate of the vaccine. The dropout rate for BCG to measles in urban areas was 31.72%, while, it was 26.44% in rural areas, whereas the overall dropout rate was 28.93%. The dropout rate for DPT 1 to DPT 3 in urban areas was 10.65%, while it was 7.31% in rural areas, whereas the overall dropout rate was 8.82%. The dropout rate for OPV 1 to OPV3 in urban areas was 11.11%, while it was 7.31% in rural areas; the overall dropout rate for OPV 1 to OPV 3 was 8.77%. The dropout rate for DPT 3 to measles in urban areas was 15.89%, while it was 19.47% in rural areas; the overall dropout rate for DPT 3 was 17.88%.
Table 2.
Dropout rates of the vaccine
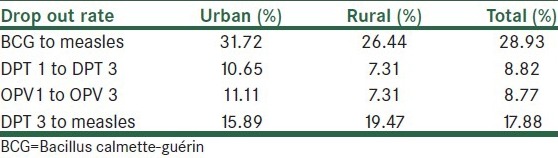
Table 3 shows that the reasons for non-immunization were unawareness of the need of immunization (32.63%), fear of side reactions (4.21%), postponing it until another time (12.63%), lack of faith in immunization (21%), place of immunization being too far (5.26%), mother being too busy (1.05%), child being ill and hence not brought for immunization (13.68%), polio was considered only vaccine (7.36%), and others (2.1%).
Table 3.
Reasons for partial and non-immunization of the children
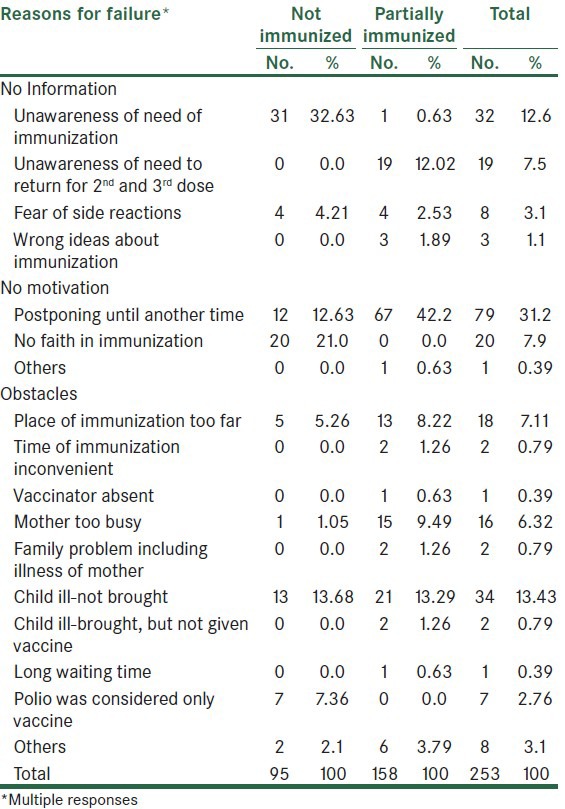
Reasons for partial immunization were unawareness of the need of immunization (0.63%), unawareness of the need to return for 2nd and 3rd dose (12.02%), fear of side reactions (2.53%), wrong ideas about immunization (1.89%), postponing it until another time (42.2%), place of immunization being too far (8.22%), time of immunization being inconvenient (1.26%), vaccinator being absent (0.63%), mother being too busy (9.49%), family problem including illness of mother (1.26%), child being ill and hence not brought (13.29%), child being ill and brought but not vaccinated (1.26%), long waiting time (0.63%), and others (4.42%).
Overall, reasons for failure of immunization were unawareness of the need of immunization (12.6%), unawareness of the need to return for 2nd and 3rd dose (7.5%), fear of side reactions (3.1%), wrong ideas about immunization (1.1%), postponing it until another time (31.2%), lack of faith in immunization (7.9%), place of immunization being too far (7.11%), time of immunization being inconvenient (0.79%), vaccinator being absent (0.39%), mother being too busy (6.32%), family problem including illness of mother (0.79%), child being ill and hence not brought (13.43%), child being ill and brought but not vaccinated (0.79%), long waiting time (0.39%), polio was considered only vaccine (2.76%), and others (3.49%).
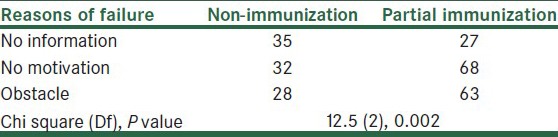
No motivation and obstacle were significant reasons for partial immunization of the child and lack of information was the major reason for non-immunization of the child [Table 4].
Table 4.
Association between immunization status with the reasons of failure of immunization
DISCUSSION
In the present study, overall, 62.7% children were fully immunized, 24.4% were partially immunized, and 12.9% were not immunized. Similar results were shown by Singh et al. in a study in different states of India, where 63.3% children were fully immunized, 27.1% were partially immunized, and 9.6% were unimmunized.[1] DLHS-III observed that 51.1% of children in Lucknow were fully immunized. Bholanath et al.[2] in a study in urban slums of Lucknow district showed that only 44.1% children were fully immunized, while 32% were partially immunized, and 23.9% were unimmunized.[2]
The overall dropout rate for BCG to measles in the present study was 28.93%. Similar study by Bholanath et al. in urban slums of Lucknow showed the overall dropout rate of 33.24%.[2] Sharma et al. in their study showed that the dropout rate for BCG to measles was 60.2% in the slums of Surat.[3] In the present study, the overall dropout rate for DPT 1 to DPT 3 was 8.82%. Sharma et al.[3] in the slums of Surat, Bholanath et al. in urban slums of Lucknow, and Yadav et al. in urban slums of Jamnagar showed that the dropout rate for DPT 1 to DPT 3 was 31.9%, 23.16%, and 10.4%, respectively.[4] In the present study, the overall the dropout rate for OPV 1 to OPV 3 was 8.77%. Similar studies by Sharma et al.[3] in the slums of Surat, by Bholanath et al. in the slums of Lucknow, and by Yadav et al.[4] in the urban slums of Jamnagar showed that the OPV 1 to OPV3 dropout rate was 31.5%, 23.16%, and 10.1%, respectively. In the present study, the overall dropout rate for DPT 3 to measles was 17.88%. Similar study by Bholanath et al. in urban slums of Lucknow showed that the dropout rate for DPT 3 to measles was found to be 13.12%.[2]
In the present study, major reasons for non-immunization were unawareness of the need of immunization (32.63%), lack of faith in immunization (21%), child being ill and hence not brought (13.68%), postponing until another time (12.63%), polio was considered only vaccine (7.36%), place of immunization being too far (5.26%), fear of side reactions (4.21%), and others (2.1%). Similar study conducted by Bholanath et al. in urban slums of Lucknow showed that lack of faith, lack of knowledge, and considering polio as the only vaccine were significant independent reasons for non-immunization of the child. Saxena et al. in a study in the urban slums of Agra district showed that lack of awareness and side effects of vaccination were the main reasons for non-immunization of children.[5] Punith et al. in a study in Bangalore showed that major reasons for non acceptance/discontinuation of immunization were unawareness of the need of immunization, unawareness of the need to return for 2nd or 3rd dose, lack of information about the place of immunization, fear of side reaction, and postponing until another time.[6]
Lack of knowledge and lack of faith came out to be the main reasons for non-immunization of the children in the present study.
Reasons for partial immunization in the present study were postponing until another time (42.2%), child being ill and hence not brought to the centre (13.29%), unawareness of the need to return for 2nd and 3rd dose (12.02%), place of immunization being too far (8.22%), mother being too busy (9.49%), fear of side reactions (2.53%), family problem including illness of mother (1.26%), child being ill and brought but not vaccinated (1.26%), wrong ideas about immunization (1.89%), time of immunization being inconvenient (1.26%), vaccinator being absent (0.63%), unawareness of the need of immunization (0.63%), long waiting time (0.63%), and others (4.42%).
Similar study conducted by Bholanath et al. in the urban slums of Lucknow showed that common reasons for partial immunization of the children are were both parents being busy (17.2%), parents gone to village/native place/migrated to other place (14.7%), child/sibling became ill as a result of previous vaccination (11.7%), carelessness (11.7%), no knowledge of vaccine and/or place (10.4%), no reason (10.4%), child being ill and not brought (8.6%), mother being ill (8.0%), mother being too busy (7.4%), child was brought but because of illness not vaccinated (6.1%), opposition from family members (4.3%), no one came at home (3.7%), financial constraints (1.8%), fear of side reaction (1.8%), no faith (1.8%), father too busy (1.2%), husband not willing (1.2%), polio was considered as the only vaccine to be given (0.6%), and others (4.9%).[2]
In the present study, lack of motivation among parents and illness of the child were the main reasons for partial immunization of the child.
Recommendations
It is of little value to assess the immunization coverage if the assessment is not followed by policy action to improve the immunization coverage and health of the children. The following are the suggestions for improving the immunization coverage in the area:
More awareness should be generated among the people living in rural and urban areas to immunize their children and to prevent the morbidity and mortality from six lethal VPDs
Parents education and poverty have a great impact on immunization coverage. In order to improve the vaccination coverage, investments in basic services, such as primary education, particularly for girls, is essential as increased education can influence a mother's understanding of the importance of immunization in her child's health Educated mothers also have opportunity of being employed in better paying jobs and thus can help in raising the socio economic status of the family.
Information, education, and communication (IEC) services should be directed towards improving the immunization status of the children in the community
Reasons for poor utilization of health care services should be inquired and should be dealt with
The importance of primary immunization under UIP is overshadowed by repeated Pulse Polio Immunization (PPI) rounds. Many people failed to immunize their children as they considered polio as the only vaccine. More awareness should be generated among people that there are five other vaccines to be given to their children other than polio vaccine.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Singh P, Yadav RJ. Immunization status of children in India. Indian Pediatr. 2000;37:1194–9. [PubMed] [Google Scholar]
- 2.Nath B, Singh JV, Awasthi S, Bhushan V, Kumar V, Singh SK. A study on determinants of immunization coverage among 12-23 months old children in urban slums of Lucknow district, India. Indian J Med Sci. 2007;61:598–606. [PubMed] [Google Scholar]
- 3.Sharma R, Desai VK, Kavishvar A. Assessment of immunization status in the slums of Surat by 15 clusters multi indicators cluster survey technique. Indian J Community Med. 2009;34:152–5. doi: 10.4103/0970-0218.51222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yadav S, Mangal S, Padhiyar N, Mehta JP, Yadav BS. Evaluation of immunization coverage in urban slums of Jamnagar city. Indian J Community Med. 2006;31:10–12. [Google Scholar]
- 5.Saxena P, Prakash D, Saxena V, Kansal S. Assessment of routine immunization in urban slums of Agra district. Indian J Prev Soc Med. 2008;39:60–2. [Google Scholar]
- 6.Punith K, Lalitha K, Suman G, Pradeep BS, Kumar KJ. Evaluation of primary immunization coverage of infants under universal immunization programme in an urban areas of Bangalore city using cluster sampling and lot quality assurance sampling technique. Indian J Community Med. 2008;33:151–5. doi: 10.4103/0970-0218.42049. [DOI] [PMC free article] [PubMed] [Google Scholar]


