Abstract
Female fertility declines dramatically with age, and childbearing at older maternal ages has significant medical consequences for mother and infant that are well-known to health professionals. Despite this, the average maternal age in the United States continues to rise. Many factors likely contribute to this secular trend; to date, no research has examined whether American women are aware of the complications of deferring conception and how this correlates with health literacy. The purpose of this study was to evaluate women's knowledge of the implications of delaying pregnancy. A structured, in-person interview was administered to 300 women between 20 and 50 years of age attending 1 of 2 gynecologic clinics at a single institution. Demographic information, medical history, and gynecologic history were obtained; and participants answered questions about the implications of aging for fertility and pregnancy outcome. Health literacy and numeracy were assessed. Participants demonstrated knowledge deficits about the implications of aging on fertility and pregnancy, and many were unfamiliar with success rates of infertility treatments. Several demographic factors correlated with knowledge; health literacy and numeracy were both important predictive variables. To the authors' knowledge, this is the first study of women's knowledge about fertility, aging, and their health literacy. Awareness of the importance of health literacy and numeracy should inform future educational efforts about fertility.
Fertility declines with advancing age, beginning as early as the middle of the third decade. Women who do conceive at an advanced maternal age (traditionally defined as age 35 years or older) are at greater risk of early pregnancy-related complications including miscarriage, aneuploidy, and ectopic pregnancy. Other obstetric complications linked to older age include gestational diabetes, hypertension, preeclampsia, placenta previa, placental abruption, dysfunctional labor, cesarean delivery, postpartum hemorrhage, and maternal mortality; fetal complications include congenital anomalies, prematurity, growth restriction, macrosomia, and stillbirth (American Congress of Obstetricians and Gynecologists, 2008; Nassar & Usta, 2009; Schmidt, Sobotka, Bentzen, & Anderson, 2012).
Despite these adverse consequences, population-based birth statistics demonstrate a consistent increase in the proportion of women choosing to delay childbearing until later in their reproductive years. The birth rate among American women in their 40s has increased by more than 70% since 1990, and the number of births to women age 35–39 years rose by more than 50% in this same time period (Hamilton, Hoyert, Martin, Strobino, & Guyer, 2013; Martin et al., 2011; Matthews & Hamilton, 2009). This rise in maternal age likely has many causes, including improved educational and professional opportunities for women, rising age of first marriage, and improved access to effective contraception. However, it is unknown to what degree American women are aware of the consequences of deferring pregnancy. It is also unknown whether the availability of assisted reproductive technologies (ART) influences women's deferral of childbearing and whether women have realistic information about the success of ART. Furthermore, although health literacy has been demonstrated to correlate with health knowledge in other disciplines, little is known about implications in women's health, and we are not aware of any work that has examined health literacy and fertility knowledge. The goals of this investigation were (a) to assess women's knowledge about loss of fertility over time, medical and genetic implications of later childbearing, and success of reproductive technologies for treating infertility; and (b) to examine the relationship of fertility-related health knowledge to demographic factors, historical factors, and health literacy.
Method
This was a single-institution descriptive study surveying women who sought gynecologic care at two locations: the Northwestern Medical Faculty Foundation (a faculty practice) and the Prentice Ambulatory Care Clinic (the continuity clinic for Northwestern Obstetrics and Gynecology residents in Chicago, Illinois). Of the sample, 50% was recruited from each clinic in order to create a sample with diverse socioeconomic background and payer mix. Nonpregnant women between 20 and 50 years of age who were not currently receiving evaluation or treatment for infertility were asked to participate. We recruited 150 women between 20 and 35 years of age and 150 women between 36 and 50 years of age. Half of each age cohort was recruited from each clinic to ensure that women across the reproductive age range of low- and high-income status were represented. We obtained informed consent before each interview and compensated each participant with a US$20 gift card for her time. Study procedures were approved by the Northwestern University Institutional Review Board.
A structured interview tool was developed for this study, and answers were recorded using a computer-based interview program, Snap (SnapSurveys, Bristol, United Kingdom). The survey instrument was created by the investigators with input from colleagues in psychology, sociology, and health literacy. The survey was initially piloted in four focus groups; focus groups participants were recruited from the same clinic sites and age groups as were the final study participants. Feedback from participants was used by the four investigators to clarify the questions in an iterative manner such that revised questions from one group were then piloted with the next focus group. The revised survey was then administered to 300 female patients who sought care from the Northwestern Medical Faculty Foundation and the Prentice Ambulatory Care Clinic. All participants were recruited and interviewed by two study investigators who were trained in the use of the Snap program by one of the senior investigators. The survey was administered as a computer-assisted structured interview; questions were read to the participants and their answers recorded in the Snap program by the interviewer. The refusal rate was low (4%); no information was collected about those women who declined to participate.
The survey was divided into three sections. The first section collected demographic information as well as medical, surgical, and gynecologic histories of participants. The second section assessed whether the participant had completed her family, was actively trying to get pregnant, or wanted to have children in the future. Women also identified factors they felt were necessary before attempting pregnancy (e.g. marriage, career success, financial stability) and ideal number of years between pregnancies. The third section ascertained women's factual knowledge about the consequences of age or ART on reproductive outcomes. Women were given a series of 13 statements about possible consequences of aging and ART, and they were asked if they “strongly agree,” “agree,” “disagree,” or “strongly disagree” with each statement (see Table 2). Participants' answers were then dichotomized into correct or incorrect responses on the basis of whether the statement was true or false. If a participant “agreed” or “strongly agree” with a true statement, this was considered correct, and vice versa. A total knowledge score (TKS) was then calculated with a possible range of 0–13 points, with higher scores indicating more accurate knowledge about fertility, aging, and ART outcomes. Subscales were calculated assessing women's knowledge of the implications of advanced maternal age (AMA) for pregnancy and fertility (referred to as the AMA knowledge score, range = 0–7) and the implications of ART for pregnancy and fertility outcomes (ART knowledge score, range = 0–6). Women were then asked to estimate what percentage of women would able to get pregnant, both naturally and then with the aid of fertility therapy, at age 25, 30, 35, 40, and 45 years using a visual analog scale.
Table 2.
Knowledge questions, correct answer, and percentage of participants answering correctly
| Question | True or false | Percentage correct |
|---|---|---|
| After age 35, miscarriage is less common. | False | 88.6 |
| After age 35, women are healthier during pregnancy because they are more mature. | False | 85.6 |
| After age 35, it is harder to get pregnant. | True | 78.5 |
| After age 35, cesarean section is more common. | True | 63.9 |
| After age 35, stillbirths / fetal deaths are less common. | False | 89.3 |
| After age 35, the risk of genetic problems in the baby is higher. | True | 87.0 |
| After age 35, women have more medical problems during pregnancy. | True | 84.2 |
| After infertility treatment, miscarriage rates are higher. | True | 65.6 |
| After infertility treatment, women have fewer problems like diabetes and high blood pressure. | False | 87.2 |
| After infertility treatment, cesarean section is more common. | True | 63.4 |
| After infertility treatment, stillbirths/fetal deaths are more common. | True | 45.6 |
| After infertility treatment, there are more twins and triplets. | True | 93.4 |
| After infertility treatment, the risk of genetic problems in the baby is higher. | True | 54.8 |
We measured health literacy using the Rapid Estimate of Adult Literacy in Medicine (REALM; Davis et al., 2011). The REALM is a literacy tool that requires participants to read and correctly pronounce 66 words. Each word pronounced incorrectly or not attempted is marked as incorrect; the REALM score is the total number of correct words. Numeracy was assessed by a seven-question instrument adapted from Lipkus, Samsa, and Rimer (2001) and scored as the total number of correct questions. This instrument asks subjects to estimate probabilities and risk (e.g., “If the chance of getting a disease is 10%, how many people would be expected to get the disease out of 100?”)
Statistical analyses were performed with PAWS/SPSS Statistics 18.0 (Chicago, Illinois). We estimated the correlation between demographic variables, medical history, health literacy, and numeracy with participants total knowledge scores. Categorical variables were analyzed with an analysis of variance and continuous variables with linear regression. A multivariable linear regression model was then created with those variables demonstrating a significant association with knowledge scores. A p value of .05 or less was considered significant.
Results
A total of 300 women completed the final survey—150 from the faculty practice and 150 from the resident clinic, stratified by age to create four cohorts. Demographic data and health literacy data are presented in Table 1. The mean age of women included in the study was 34.8 years (SD = 7.9 years). The majority of women were African American (47.7%), heterosexual (97.0%), married or living with their significant other (54.6%), identified themselves with a particular religion (80.3%), had access to the Internet (94.3%), and had been pregnant before (70%). In addition, 46% had completed a 4-year college, and 65% worked outside the home for pay. Regarding insurance, 49% of patients had state-funded medical insurance. Participants' annual household income ranged from less than $10,000 to more than $200,000; 52% had a household income of less than $50,000 per year.
Table 1.
Demographic characteristics of the study sample
| Characteristic | n (%) |
|---|---|
| Race | |
| African American | 143 (47.7) |
| Caucasian | 101 (33.7) |
| Hispanic | 32 (10.7) |
| Asian | 14 (4.7) |
| Other | 10 (3.3) |
| Relationship status | |
| Married/life partner | 112 (37.3) |
| Living with significant other | 52 (17.3) |
| In a relationship, not living together | 59 (19.7) |
| Single | 77 (25.7) |
| Prior history of medical problems | |
| None | 171 (57.0) |
| One or more | 129 (43.0) |
| History of gynecologic problems | 56 (18.7) |
| Education completed | |
| Grades 1–11 | 15 (5.0) |
| Grade 12 or general equivalency diploma | 46 (12.0) |
| College 1–3 years | 111 (37.0) |
| College graduate | 138 (46.0) |
| Primary source of fertility and pregnancy information | |
| Internet | 77 (25.7) |
| Television | 39 (13.0) |
| Magazines | 22 (7.3) |
| Newspaper | 9 (3.0) |
| My doctor | 96 (32.0) |
| Family or friends | 57 (19.0) |
| REALM score | |
| Mean | 33.3 ± 3.9 |
| Range | 35–66 |
REALM = Rapid Estimate of Adult Literacy in Medicine.
Literacy skills were measured by the REALM; 296 of 300 participants completed the assessment. The range of participant scores was 35–66 of a possible 66, with a mean score of 63.3 (SD = 3.9, range = 35–66). Only 2 women (0.7%) had limited health literacy according to the REALM (score less than 44); 39 (13.1%) had marginal health literacy (scores between 45 and 60), and the majority (255, 86.1%) had adequate health literacy. For the purpose of statistical analysis, the limited and marginal groups were combined. Numeracy was assessed by a seven-question instrument adapted from Lipkus and colleagues (2001) and scored as the total number of correct questions. Mean numeracy score was 4.5 of a possible 7 (range = 0–7, SD = 1.5).
Participants' knowledge of the reproductive consequences of aging and ART are shown in Table 2. In general, participants were more aware of the implications of later childbearing than of ART. For each of the seven statements about advanced maternal age, 63 to 89% of women knew the correct answer. For each of the six statements about ART, 43 to 93% of women knew the correct answer. Most women knew that ART is associated with multiple gestations (93%); other complications were less well known. TKS ranged from 5 to 13 of a possible 13, with a mean of 9.9 (SD = 2.1). AMA knowledge scores ranged from 2 to 7 of a possible 7, with a mean of 5.8 (SD = 1.3) and ART knowledge scores ranged from 1 to 6, with a mean of 4.1 (SD = 1.3). Distributions of scores are represented in Figure 1. In total, 39.9% of women correctly answered all seven AMA questions. In contrast, only 16.6% of women correctly answered all six of the ART questions. Only 10.8% of women correctly answered 13 questions.
Figure 1.
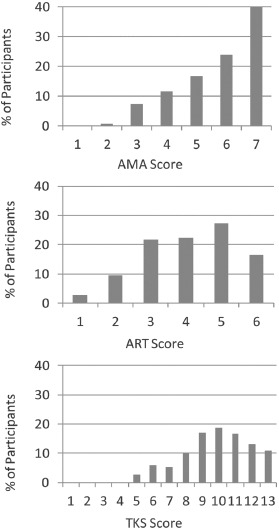
Distribution of scores for advanced maternal age (AMA), assisted reproductive technologies (ART), and total knowledge score (TKS).
Women then estimated the probability of pregnancy at each of five ages (25, 30, 35, 40, 45 years) first for spontaneous conception and then with ART. The mean estimates are displayed in Figure 2 (spontaneous pregnancy) and Figure 3 (pregnancy after ART). Estimates of the true rates of natural fertility are plotted on the same graph for reference (Practice Committee, 2007). Estimates of the success of ART are plotted in Figure 3; these were generated on the basis of published data (Malizia, Hacker, & Penzias, 2009).
Figure 2.
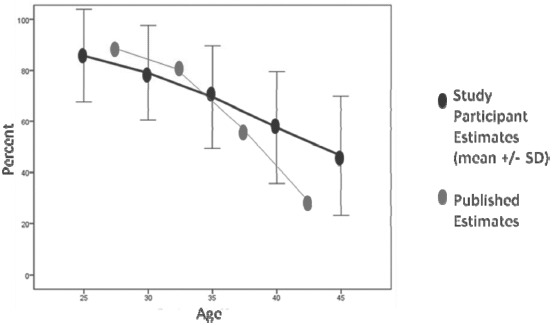
Participants' estimates of probability of spontaneous pregnancy at different ages (M ± 1 SD). (Color figure available online.)
Figure 3.
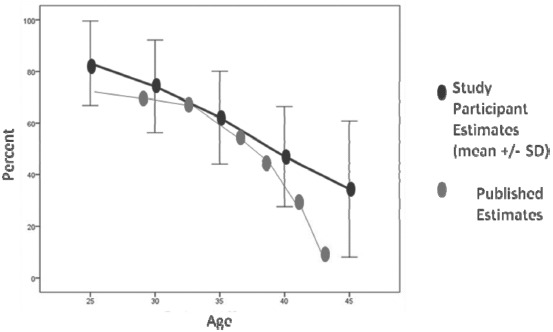
Participants' estimates of probability of pregnancy after ART at different ages (M ± 1 SD). ART = assisted reproductive technologies. (Color figure available online.)
We examined the relationship between demographic factors, medical or gynecologic history, pregnancy, infertility experience, health literacy, numeracy, and participants' knowledge scores. Demographic and historical factors associated with TKS in univariate analysis are shown in Table 3. Specifically, age, race, education, employment status, Internet access, religion, pregnancy, infertility treatment, and publicly funded insurance were all significantly correlated with TKS. Other variables analyzed that did not correlate with TKS included household income, religiosity, sexual orientation, relationship status, clinic site, or reported history of medical or gynecologic problems.
Table 3.
Factors associated with TKS in univariate analyses (analysis of variance or linear regression)
| TKS (M ± SD) | p | |
|---|---|---|
| Race | <.001 | |
| Caucasian | 10.3 (1.9) | |
| African American | 9.4 (2.1) | |
| Latino | 9.8 (2.0) | |
| Asian | 11.4 (1.4) | |
| Other/declined | 10.0 (2.4) | |
| Years of education completed | <.001 | |
| Grades 1–8 | 8.0 (2.8) | |
| Grades 9–11 | 7.6 (2.1) | |
| Grade 12/general equivalency diploma | 9.4 (2.3) | |
| Some college | 9.7 (2.0) | |
| College graduate | 10.4 (1.8) | |
| Regular Internet access | .001 | |
| No | 8.3 (1.8) | |
| Yes | 10.0 (2.1) | |
| Work outside the home for pay | .001 | |
| No | 9.3 (2.0) | |
| Yes | 10.2 (2.1) | |
| Public insurance | .003 | |
| No | 10.3 (2.0) | |
| Yes | 9.5 (2.1) | |
| Religion | .008 | |
| Catholicism | 10.3 (1.9) | |
| Other Christian religion | 9.5 (2.0) | |
| Judaism | 11.0 (0.8) | |
| Islam | 11.6 (1.6) | |
| Hinduism | 13.0 (n/c, n = 1) | |
| Other | 9.5 (2.7) | |
| None | 10.1 (2.2) | |
| Previous pregnancy | <.001 | |
| No | 10.7 (1.8) | |
| Yes | 9.3 (2.1) | |
| Prior treatment for infertility | .03 | |
| No | 8.9 (1.8) | |
| Yes | 11.4 (2.3) | |
| REALM health literacy score | <.001 | |
| 0–60 (limited and marginal) | 8.8 (2.3) | |
| 61–66 (adequate) | 10.1 (2.0) | |
| Numeracy score | r2 = 0.1 | <.001 |
| Age | r2 = .02 | .03 |
Note. Factors that remain significant in multivariate regression model are in bold. REALM = Rapid Estimate of Adult Literacy in Medicine; TKS = total knowledge score.
The REALM score and numeracy score were significantly associated with TKS. The REALM score was analyzed as a categorical variable (marginal or limited vs. adequate); women with lower literacy had an average TKS of 8.8, compared with 10.1 among women with adequate health literacy (p < .001). When the REALM score was treated as a continuous variable, the relationship was again demonstrated; regression analysis revealed a small but statistically significant effect (r = .27, p < .001). The correlation between numeracy scores and the TKS was estimated using linear regression, and a correlation of similar magnitude was identified (r = .32, p < .001).
The variables found to be statistically significant in the aforementioned univariate analyses were then added in stepwise fashion to a linear regression model, and all of these are listed in Table 3. Variables that contributed to the performance of the regression model were age, education, public insurance, infertility treatment, and REALM score (treated as a categorical variable). The final model with these variables was able to predict the TKS with fair accuracy: r = 0.78, r2 = 0.61, df (5, 24), p < .001. Health literacy (REALM score) had a substantial effect on the accuracy of the model; when removed, the correlation declined to r = .69 (r2 = .47). In contrast, numeracy did not contribute to the performance of the model and was removed.
Discussion
Several studies have attempted to characterize what women know about fertility, pregnancy outcomes, ART, and aging, but to our knowledge this is the first such investigation in a diverse American population incorporating measures of health literacy and numeracy. Daniluk, Koert, and Cheung (2012) conducted an online survey of more than 3,000 childless Canadian women between 20 and 50 years of age to ascertain their knowledge of various risk factors for infertility, including age. They found “substantial knowledge gaps,” in particular with regard to the relationship between age and infertility and the success rates with ART. However, their population was 82% Caucasian, and 80% had a college degree or greater. Bretherick, Fairbrother, Avila, Harbord, and Robinson conducted a smaller study of 360 Canadian college students. They found that their subjects were aware that fertility declines with age but overestimated the likelihood of spontaneous pregnancy at all ages. Women were generally unaware of the association between advancing age and miscarriage, and overestimated the probability of successful in vitro fertilization at older ages. Tough and colleagues (2007) conducted phone interviews with more than 1,000 postpartum women and found that although most women were aware that fertility declined after 35 years of age, the majority were unaware of other complications of advancing age including cesarean delivery, low birth weight, and preterm birth. Suguira-Ogasawara, Ozaki, Kaneko, Kataori, and Kumagai (2010) surveyed 249 Japanese women at two universities and a women's health fair. Only 45% of women correctly estimated rates of infertility, and only 10.7% answered all questions about reproductive health correctly. More than 36% of participants “estimated their own age limit for natural pregnancy to be between 45 and 60 years.”
Our investigation builds on these past studies by using a diverse sample of American women; our recruitment strategy ensured oversampling of minority and low-income women, as evidenced by the demographic data. Furthermore, we believe the addition of health literacy and numeracy scales adds important nuance to the study. Our population had a broader range of educational and health care experiences than the studies noted earlier, so it was particularly important to estimate health literacy and numeracy in this population.
Strengths of this study included a racially and demographically diverse population; a very high response rate; and the ascertainment of multiple sociodemographic, medical, and gynecologic characteristics. The use of validated tools for assessment of health literacy and numeracy is another important strength of the study. Limitations of the study include a relatively small sample size—only 300 participants. In addition, because we recruited women from two gynecology clinics, it is uncertain whether their results can be extrapolated to the general population of American women. Our participants had relatively high health literacy scores; we hypothesize that the effect of health literacy might have been even greater if we had more diversity of health literacy skills. Last, our study included women who were not planning to try to conceive, for whom the risks of deferred childbearing may be less immediately relevant. It would be useful to replicate this study among a group of women who have articulated a decision to defer childbearing, and see if the results are similar.
Overall, we found that women were fairly familiar with the risks of advanced maternal age on infertility and complications of pregnancy. However, women were less well versed about the complications of assisted reproductive technologies. Similar to participants in Sugiura and colleagues' (2010) work, our participants were aware of declining fertility with age but overestimated the chance of spontaneous pregnancy at older ages. They also overestimated success rates with ART at all ages, with particular discrepancies between their estimates and published data for older women.
It is likely that women postpone childbearing for multiple reasons, including attainment of educational and professional goals, improved access to effective contraception and rising age of marriage (Mills, Rindfuss, McDonald, & te Velde, 2011). However, it may also be the case that the public attention to the successes of assisted reproduction leads women to overestimate the duration of their own fertility and the probability that ART can assist them if they do have infertility. Our data would suggest that many women have inaccurate information about the duration of natural fertility and in particular about the success of ART, which may give a false sense of security and contribute to decisions to delay childbearing. Furthermore, our study is the first to demonstrate that health literacy is an important determinant of fertility-related knowledge. The field of health literacy can provide clinicians and educators evidence-based guidance on how to design materials and interventions to clearly and effectively provide this much-needed education.
References
- American Congress of Obstetricians and Gynecologists. Committee opinion no. 413: Age-related fertility decline. Obstetrics and Gynecology. 2008;112:409–411. doi: 10.1097/AOG.0b013e318183fbe6. [DOI] [PubMed] [Google Scholar]
- Bretherick K. L., Fairbrother N., Avila L., Harbord S. H. A., Robinson W. P. Fertility and aging: Do Canadian women know what they need to know? Fertility and Sterility. 2010;93:2162–2168. doi: 10.1016/j.fertnstert.2009.01.064. [DOI] [PubMed] [Google Scholar]
- Daniluk J. C., Koert E., Cheung A. Childless women's knowledge of fertility and assisted human reproduction: Identifying the gaps. Fertility and Sterility. 2012;97:420–426. doi: 10.1016/j.fertnstert.2011.11.046. [DOI] [PubMed] [Google Scholar]
- Davis T. C., Long S. W., Jackson R. H., Mayeaux E. J., George R. B., Murphy P. W., Crouch M. A. Rapid Estimate of Adult Literacy in Medicine: A shortened screening instrument. Family Medicine. 2011;25:391–395. [PubMed] [Google Scholar]
- Hamilton B. E., Hoyert D. L., Martin J. A., Strobino D. M., Guyer B. Annual summary of vital statistics: 2010–2011. Pediatrics. 2013;131:548–558. doi: 10.1542/peds.2012-3769. doi: 10.1542/peds.2012-3769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipkus I. M., Samsa G., Rimer B. K. General performance on a numeracy scale among highly educated samples. Medical Decision Making. 2001;21:37–44. doi: 10.1177/0272989X0102100105. [DOI] [PubMed] [Google Scholar]
- Malizia B. A., Hacker M. R., Penzias A. S. Cumulative live-birth rates after in vitro fertilization. New England Journal of Medicine. 2009;360:236–243. doi: 10.1056/NEJMoa0803072. [DOI] [PubMed] [Google Scholar]
- Martin J. A., Hamilton B. E., Ventura S. J., Osterman M. J., Kirmeyer S., Mathews T. J., Wilson E. C. Births: Final data for 2009. National vital statistics reports; vol 60 no 1. Hyattsville, MD: National Center for Health Statistics; 2011. [PubMed] [Google Scholar]
- Matthews T. J., Hamilton B. E. Delayed childbearing: More women are having their first child later in life. NCHS Data Brief. 2009;21:1–8. [PubMed] [Google Scholar]
- Mills M., Rindfuss R. R., McDonald P., te Velde E. Why do people postpone parenthood? Reasons and social policy incentives. Human Reproduction Update. 2011;17:848–860. doi: 10.1093/humupd/dmr026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nassar A. H., Usta I. M. Advanced maternal age. Part II: Long-term consequences. American Journal of Perinatology. 2009;26:107–112. doi: 10.1055/s-0028-1090593. [DOI] [PubMed] [Google Scholar]
- Practice Committee of the Society for Assisted Reproductive Technology and Practice Committee of the American Society for Reproductive Medicine. Essential elements of informed consent for elective oocyte cryopreservation: A practice committee opinion. Fertility aad Sterility. 2007;88:1495–1496. doi: 10.1016/j.fertnstert.2007.10.009. [DOI] [PubMed] [Google Scholar]
- Schmidt L., Sobotka T., Bentzen J. G., Anderson A. N. Demographic and medical consequences of the postponement of parenthood. Human Reproduction Update. 2012;18:29–43. doi: 10.1093/humupd/dmr040. [DOI] [PubMed] [Google Scholar]
- Suguira-Ogasawara M., Ozaki Y., Kaneko S., Kataori T., Kumagai K. Japanese single women have limited knowledge of age-related reproductive time limits. International Journal of Gynecology & Obstetetrics. 2010;109:75–76. doi: 10.1016/j.ijgo.2009.10.020. [DOI] [PubMed] [Google Scholar]
- Tough S., Benzies K., Newburn-Cook C., Tofflemire K., Fraser-Lee N., Faber A., Sauve R. What do women know about the risks of delayed childbearing? Canadian Journal of Public Health. 2007;97:330–334. doi: 10.1007/BF03405615. [DOI] [PMC free article] [PubMed] [Google Scholar]


