Abstract
Purpose
Oncologists are now prescribing more oral chemotherapy than ever before, thus placing the onus for taking the right dose at the right time under the right circumstances directly on the patient. This study was undertaken to understand emerging adherence issues and to explore available adherence assessment tools.
Methods
This two-part study 1) examined N0747, a randomized, phase II trial that tested the oral agents, sunitinib and capecitabine, in patients with metastatic esophageal cancer an adherence standpoint; and 2) conducted a systematic review to compile and assess adherence tools that can be used in future clinical trials.
Results
First, in N0747, patients were assigned to sunitinib and capecitabine versus capecitabine; 53 chemotherapy cycles were prescribed to this 12-patient cohort. Nearly all patients denoted they “always or almost always” took their pills as prescribed, and 2 patients who reported lack of full adherence suffered grade 3+ adverse events. Surprisingly, however, over 14 cycles, 9 patients reported grade 3+ toxicity but checked “always or almost always” to describe adherence. No relationships were observed between adherence and cancer outcomes. Secondly, 21 articles identified adherence tools: 1) healthcare providers’ interviews; 2) patient-reported adherence with diaries/calendars; 3) patient-completed adherence scales; 4) medication event monitoring; 5) automated voice response; 6) drug/metabolite assays; and 7) prescription data bases. Of note, only the automated voice response seems capable of real time detection of over-adherence, as observed in N0747.
Conclusion
Oral chemotherapy adherence should be further studied, particularly from the standpoint of over-adherence.
Keywords: oral chemotherapy, adverse events, adherence, over adherence
The list of oral chemotherapy agents for solid tumor malignancies has lengthened over the last few years and now includes everolimus, vandetanib, vismodegib, imatinib mesylate, topotecan, axitinib, sorafenib, regorafenib, sunitinib, erlotinib, temozolomide, and capecitabine -- to name a few. In addition, a recent study found that the proportion of total pharmacy costs for oral chemotherapy more than doubled between 2002 and 2006 [1]. These two observations underscore the fact that oncologists are prescribing more oral chemotherapy today than ever before.
This long list of oral cancer drug options has created unique medication adherence concerns. With intravenous chemotherapy, healthcare providers take direct and exclusive responsibility for administering cancer drugs with accuracy. In contrast, oral chemotherapy puts the onus for taking the right dose at the right time under the right circumstances -- by definition, “adherence” to medication instructions -- directly on the patient. Patients’ adherence to an oral regimen becomes especially relevant when one considers that many oral chemotherapy agents have a narrow therapeutic window: taking a few extra pills or missing some or taking pills at the wrong time can lead to untoward adverse events or unfavorable clinical outcomes.
Are cancer patients, particularly those with metastatic disease, taking their medications correctly, and how can healthcare providers know for sure? This two-part study was formulated in an attempt to explore this two-part question. It examined a prospectively-conducted cancer clinical trial that included two different oral chemotherapy agents, sunitinib and capecitabine, and focused on trial results from the vantage point of identifying adherence issues. This study also provided a systematic review of the published literature on oral cancer chemotherapy adherence tools, which were designed to assess adherence, with the goal of better understanding the strengths and limitations of each such tool.
METHODS
Overview
The first part of this study examined N0747, a North Central Cancer Treatment Group (NCCTG) trial that was approved by each site’s institutional review board and conducted in patients with metastatic esophageal cancer. This trial tested the oral agents, sunitinib and capecitabine, as first-line chemotherapy. The original primary endpoints and eligibility criteria are outlined on www.clinicaltrials.gov (NCT00891878) [2]. Because of poor accrual, this trial was halted prematurely, hence providing the platform for the current study on adherence.
The second part of this study consisted of a systematic review of the published literature and was undertaken with the goal of identifying and better understanding the strengths and limitations of oral chemotherapy assessment tools. This effort seemed timely, given this increase in oral chemotherapy prescribing patterns and given the concerns for over adherence, as identified in N0747.
N0747
The primary goal of the first part of this study was to explore whether patients’ completion of a single-item patient-reported adherence tool was associated with any objective clinical parameters, such as adverse events or tumor response. Immediately after completion of each chemotherapy cycle, patients were asked to complete the adherence tool (Figure 1).
Figure 1.
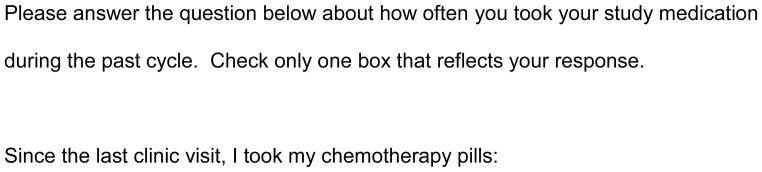

Part 1 of this study included a single-item patient-reported adherence tool, as shown in figure 1.
This randomized phase II trial examined single agent capecitabine 1000 mg/m2/dose orally twice per day for two weeks as part of a 21-day chemotherapy cycle versus capecitabine at this same dose plus sunitinib 37.5 mg orally once a day for 21 days as part of a 21-day cycle. The study provided sunitinib to patients. Dose adjustments were outlined in the protocol, based on type and severity of adverse events, and called for cutting back on the capecitabine dose to as low as 500 mg/m2/dose with some possibility of dose escalation to 1250 mg/m2/dose in the event a patient were to tolerate the drug extremely well. Similarly, sunitinib could be cut to as low as 12.5 mg orally per day for toxicity but with no possibility of a dose escalation. Crossover from capecitabine alone to the 2-drug arm was allowed in the event of cancer progression.
Patients were monitored for cancer progression-free survival, the primary endpoint for the original trial, with every 6-week radiographic imaging, as per the RECIST criteria [3]. Patients were also monitored for adverse events, as per the Common Terminology Criteria for Adverse Events, version 3. Chi square tests were used to assess the relationship between categorical variables, and Kaplan Meier methodology and the log rank test were used to analyze overall survival and progression free survival. Relationships between these clinical outcomes and patients’ responses to the single-item patient-reported adherence tool are presented descriptively.
Systematic Review
For the second part of this study, a research librarian (AF) used the Ovid interface to search MEDLINE (from January 1946 through January 2013) and Embase (from January 1988 through January 2013). Medical subject headings and keywords were combined to yield greater relevance. Such key words consisted of numerous descriptors for adherence (for example, compliance, persistence, over-adherence, over-compliant), for oral chemotherapy (for example, tablet, capsule, pill), for neoplasms (for example, tumor, malignancy, carcinoma), and for self-reporting (for example, tool, assess, evaluation, measure, electronic monitoring, questionnaire). The search was restricted to only articles relevant to adult patients. The full search strategy appears in Figure 2.
Figure 2.
The search strategy for this systematic review of the literature is attached.
Prospectively-conducted interventional and quantitative studies were sought. Only those in English were reviewed. Based on abstract review, articles were preliminarily deemed eligible for inclusion if they appeared to meet the following criteria: 1) the article focused on solid tumor malignancies; 2) oral chemotherapy was prescribed; 3) the main focus of the article was adherence to oral chemotherapy; and 4) the article sought to acquire primary data as opposed to providing a topic review. Articles that focused on chemoprevention (as opposed to cancer treatment) or patients with hematologic malignancies (where the goals of therapy are sometimes more oriented toward cure) were excluded because it was thought that adherence issues under these circumstances or in these groups would be different from those in solid tumor cancer patients receiving oral chemotherapy. After this first-pass review of abstracts, all full articles were reviewed in detail to determine whether they truly met all the eligibility criteria described above, and further articles were retrieved and examined from references in the first set. Review of abstracts and full articles was undertaken by two investigators (KP and AJ) with differences in opinions adjudicated with a face-to-face discussion.
RESULTS
N0747
Demographics
This trial recruited 12 patients with an equal distribution of patient numbers and gender to each study arm. The median ages in the 2-drug and 1-drug arm were 73 and 75 years, respectively. No statistically significant difference in performance score was observed across arms at study entry; two patients in the 2-drug arm had a performance score of 2, as did one in the 1-drug arm. Two patients crossed over to the 2-drug arm.
The Adherence Statement Response Item and Adverse Events
All patients completed the single-item patient-reported adherence tool over all 53 cycles of chemotherapy prior to the possibility of crossover, except for one who did not complete this item after his one and only cycle of chemotherapy (see below and Table 1).
Table 1.
| Patient # | Drug(s) | Total # of Cycles | Adherence Statement Response | Adverse Events* | Best Tumor Response |
|---|---|---|---|---|---|
| 1 | capecitabine | 2 | “always or almost always” | Cycle 2: thrombosis (grade 4); anorexia, dehydration, nausea, vomiting, diarrhea, muscle weakness (grade 3) | stable |
| 2 | capecitabine (crossed over to both drugs after cycle 9 for 3 cycles) | 9 | Cycle 1: “usually” Cycles 2–9: “always or almost always” | none | stable |
| 3 | capecitabine (crossed over to both drugs after cycle 1 for 1 cycle) | 1 | “always or almost always” | none | progression |
| 4 | capecitabine | 2 | “always or almost always” | Cycles 1 and 2: diarrhea (grade 3) | progression |
| 5 | capecitabine | 2 | “always or almost always” | Cycle 2: fatigue (grade 3) | stable |
| 6 | capecitabine | 12 | “always or almost always” | Cycle 2 and 6: hand/foot syndrome (grade 3); Cycle 10: diarrhea (grade 3); Cycle 12: thrombosis (grade 3) | stable |
| 7 | capecitabine sunitinib | 1 | not available | Cycle 1: mucositis (grade 3); neutropenia (grade 4); febrile neutropenia (grade 3) | not available |
| 8 | capecitabine sunitinib | 10 | “always or almost always” | Cycle 1: gastrointestinal bleeding and anemia on warfarin (grade 3) Cycle 10: neutropenia and anemia (grade 3) |
partial response |
| 9 | capecitabine sunitinib | 1 | “always or almost always” | Cycle 1: vomiting (grade 3); esophageal pain (grade 4) | progression |
| 10 | capecitabine sunitinib | 2 | Cycle 1: “rarely” Cycle 2: “always or almost always” | Cycle 1: anorexia, dehydration, gastritis, gastrointestinal anastomotic leak, muscle weakness (all grade 3) Cycle 2: fatigue, anorexia, gastritis (all grade 3) |
progression |
| 11 | capecitabine sunitinib | 3 | “always or almost always” | Cycle 1: hand foot syndrome, rash, mucositis (all grade 3) | stable |
| 12 | capecitabine sunitinib | 8 | “always or almost always” | Cycle 5: pneumonitis (grade 3) | partial response |
Only grade 3 or worse adverse were reported in this trial.
Patients almost uniformly checked “always or almost always” after the chemotherapy cycle to describe their adherence to oral chemotherapy. Surprisingly, over the course of 14 cycles, 9 different patients reported grade 3 or worse toxicity but nonetheless checked “always or almost always” on the single-item patient-reported adherence tool.
Within the whole cohort, in only 3 instances, patients checked another adherence category. One patient on the 1-drug arm checked, “usually,” after one cycle. A second patient in the 2-drug arm checked, “rarely” after the first cycle and also suffered grade 3 anorexia, dehydration, gastritis, anastomotic leak, and muscle weakness during that first cycle. This patient had to hold the oral chemotherapy because of this toxicity. As alluded to above, a third patient in the 2-drug arm did not complete the single-item patient-reported adherence tool at all after his first and only cycle and suffered grade 3 mucositis and grade 3 febrile neutropenia with grade 4 neutropenia during that cycle.
Clinical Outcomes
The median cancer progression-free survival was 2.4 months (95% confidence interval: 0.6 to 8.4) in the 2-drug arm and 6.1 months (0.6 to 9.2) in the 1-drug arm (p=0.43). The median overall survival was 5.9 months (95% confidence interval: 0.9 to 29.8) in the 2-drug arm and 6.2 months (1.5 to 18.8) in the 1-drug arm.
Although no statistical analyses were undertaken, no relationships seemed apparent between the above outcomes and responses to the single-item patient-reported adherence tool.
Systematic Review
In view of the increasing use of oral chemotherapy and the identification of this issue of over-adherence in N0747, it seemed timely to undertake a systematic review of the published literature on adherence tools and to comment upon their strengths and limitations. The methods outlined above resulted in a total of 1346 abstracts, which yielded 21 full and unique articles that met the study’s eligibility criteria. All these articles were published in the last 20 years with more articles becoming available more recently.
These articles identified seven different tools relevant to adherence assessment: 1) healthcare providers’ interviews of patients about adherence; 2) patient-reported adherence with diaries or calendars; 3) patient-completed adherence scales; 4) a medication event monitoring system (MEMS); 5) an automated voice response system; 6) drug or metabolite assays; and 7) use of prescription data bases (Table 2). Of note, only one tool, the automated voice response system, appeared capable of responding to over-adherence in a real time manner. Moreover, only 5 of 21 studies specified a focus on patients with metastatic cancer, a setting in which our preliminary data from N0747 raised concerns for over-adherence.
Table 2.
| ADHERENCE ASSESSMENT METHOD | EXPLANATION OF METHOD | ADVANTAGES AND DISADVANTAGES | REFERENCE |
|---|---|---|---|
| Healthcare provider interviews | consists of healthcare providers’ asking patients in a face-to-face manner or by telephone whether they had taken their oral chemotherapy | Advantages: less expensive; integrated into patient care; allows for more detailed understanding of adherence issues Disadvantages: accuracy of information less clear (patients embarrassed and will not confess to poor adherence); healthcare provider may forget to ask |
5, 6, 7, 8, 9 |
| Patient-reported adherence with diaries or calendars | patients report their pill taking after each dose or at some other frequency | Advantages: low cost; accuracy of information might vary based on patients’ understanding of who would get the report (healthcare provider or personnel within a large data base) Disadvantages: patients may forget to complete or may do so less frequently with gaps in accuracy; diaries/calenders can get lost leaving large gaps in data |
7, 8, 9, 10, 11, 12, 13, 14 |
| Patient-completion of adherence scales | patients complete a questionnaire that estimates their understanding of adherence and frequency of medication adherence | Advantages: low cost; less effort intensive for the patient than diaries; sometimes allows for better understanding of why adherence might be poor(drug side effects, drug expense, etc) Disadvantages: accuracy of data may be an issue (patients embarrassed about poor adherence); patients may lose questionnaire prior to submission or may not complete; requires higher degree of patient literacy than a diary or calender |
15, 16 |
| Medication Event Monitoring System(MEMS) | an electronic cap that covers the medication bottle activates every time the bottle is opened and counts and records patients’ opening the cap as taking their medication | Advantages: relieves burden from patients of recording adherence Disadvantages: more expensive than other methods; patients might find it intrusive; risk of malfunction; may suggest over-adherence, as any time the bottle is opened, it counts as a pill ingestion |
12, 13, 14, 17, 18, 19, 20 |
| Automated Voice Response System | patients are called at the times of their choice, respond to questions with their telephone touch pad, and an automated phone response system provides information specific to each patients’ tailored informational needs relevant to drug adherence | Advantages:provides tailored information on adherence; more accessible to patients as a result of wide-spread cell phone use; high patient acceptance; capable of real time detection of over-adherence. Disadvantages: more expensive; may not be able to be tailored to address every single patients’ needs |
21 |
| Drug and Drug Metabolite Assays | patients submit their urine, blood, or hair for drug level assessment | Advantages: provides objective information Disadvantages: expensive; may miss sporadic skipping of medication or timing of medication administration; may not be able to detect small changes in adherence; patients might find it intrusive or painful (blood draw); does not take into account pharmacogenomics differences from patient-to-patient in drug bioavailability or metabolism; not amenable to monitoring all oral agents |
9, 22, 23 |
| Databases that Capture Prescriptions | Either hospital-based pharmacy or other such databases are used to examine drug adherence based on the number of prescriptions filled. | Advantages: little/no effort on the part of the patient; might lessen Hawthorne effect; might be lower cost (depending on infrastructure in place) Disadvantages: patients may fill prescriptions elsewhere and therefore good adherence may not be registered; might be a great delay between knowing about adherence and assessing other outcomes, depending on the organization of the data base |
2, 11, 16 |
Otherwise, with the exception of prescription data base reviews and the MEMS, most of these tools puts the burden of reporting on the patient; and no tool appears foolproof in guarding against a patient’s forgetting to report or being too embarrassed to report poor adherence.
DISCUSSION
This two-part study provides three important observations on oral chemotherapy adherence in cancer patients. First, despite its small sample size, N0747 raises the concern that patients, particularly those with metastatic cancer, may be more likely to become over-adherent to oral chemotherapy. In N0747, we observed that, in 14 instances, patients checked the single-item patient-reported adherence tool at the end of their chemotherapy cycle to indicate that they “always or almost always” were taking their chemotherapy pills -- even in the setting of grade 3 or worse adverse events. Although we cannot know for sure that these patients actually took all their pills, the fact that they suffered severe adverse events suggests they were. These findings, in contrast to the adjuvant breast cancer setting, where adherence rates have sometimes been as low as 16%, suggest that more research is needed on cancer chemotherapy adherence, particularly in the setting of metastatic disease [4]. Indeed, our systematic review of the literature suggests that this topic of over-adherence in patients with metastatic cancer has not been fully addressed; only 5 studies specify whether patients had metastatic cancer or not, and only one tool, the automated voice response system, appears capable of detecting and responding to over-adherence in a real time manner. Future research should perhaps focus on whether patients with metastatic cancer and limited therapeutic options have different incentives, different adherence rates, and, consequently, different needs in terms of monitoring adherence and specifically in terms of monitoring over-adherence.
Second, our systematic review demonstrates that, with only 21 articles gleaned from our review, the published literature -- as of now and as defined by our review criteria -- is sparse on the topic of oral chemotherapy adherence. Nonetheless, it appears this landscape is changing to coincide with the growing availability of oral cancer chemotherapy agents. All 21 articles in this review were published in just the past 20 years, and the overall pattern of publication seems to suggest a slight crescendo in more recent years. Clearly, more adherence research is needed, and, likely, more will be forthcoming.
Third and importantly, no fool-proof method -- short of the draconian approach of constantly watching a cancer patient ingest each of his/her pills without vomiting or spitting them out and without taking extra pills – yet exists to ascertain whether or not patients are taking their oral cancer therapy as prescribed. The single-item patient-reported adherence tool tested in N0747 makes it impossible to detect episodic omissions in pill ingestion. Similarly, all the published adherence methods in our systematic review also reveal loopholes and are unable to discern definitively whether patients had forgotten to take some of their medication or whether they might have been too embarrassed to recount omissions. In essence, all the adherence methods used or reviewed rely on patients’ willingness to report candidly their own drug self-administration patterns or their willingness to be carefully monitored. Thus, we cannot be totally assured of the true accuracy of the information that these tools yield.
Finally, this study has limitations, particularly with respect to N0747. Although other studies on adherence sometimes included small sample sizes, it remains important to recognize his limitation here and to point out that this small sample size enables us to draw only preliminary observations [5–7, 10, 17, 20, 21, 23]. In addition, the fact that this study was slow to accrue suggests that the patients enrolled in this trial might not be representative of a more general group of patients with metastatic cancer. Despite these limitations, the possibility of over-adherence in patients with metastatic disease, as raised in N0747, remains a major source of concern and an area that merits further investigation. Our systematic review of adherence tools also identified an unmet need to design more tools that are capable of specifically detecting over adherence and specifically in patients with metastatic cancer.
Acknowledgments
This study was conducted as a collaborative trial of the North Central Cancer Treatment Group and Mayo Clinic and was supported in part by Public Health Service grants CA-25224, CA-37404, CA-35448, CA-35113, CA-35267, CA-35103, and CA-35119 from the National Cancer Institute, Department of Health and Human Services. The content is solely the responsibility of the authors and does not necessarily represent the views of the National Cancer Institute or the National Institute of Health. This study was also supported by 5K24CA131099.
References
- 1. [last accessed March 20, 2013]; http://chemoth.com/economics.
- 2. [last accessed March 20 2013]; http://clinicaltrials.gov/ct2/show/NCT00891878?term=N0747+AND+jatoi&rank=1.
- 3.Therasse P, Arbuck SG, Eisenhauer EA, et al. New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst. 2000;92:205–16. doi: 10.1093/jnci/92.3.205. [DOI] [PubMed] [Google Scholar]
- 4.Ruddy K, Mayer E, Partridge A. Patient adherence and persistence with oral anticancer treatment. CA Cancer J Clin. 2009;59:56–66. doi: 10.3322/caac.20004. [DOI] [PubMed] [Google Scholar]
- 5.Sommers RM, Miller K, Berry DL. Feasibility pilot on medication adherence and knowledge in ambulatory patients with gastrointestinal cancer. Oncology Nursing Forum. 2012;39:373–379. doi: 10.1188/12.ONF.E373-E379. [DOI] [PubMed] [Google Scholar]
- 6.Bhattacharya D, Easthall C, Willoughby KA, Small M, Watson S. Capecitabine non-adherence: Exploration of magnitude, nature and contributing factors. Journal of Oncology Pharmacy Practice. 2012;18(3):333–342. doi: 10.1177/1078155211436022. [DOI] [PubMed] [Google Scholar]
- 7.Bordonaro S, Raiti F, Di Mari A, et al. Active home-based cancer treatment. Journal of multidisciplinary healthcare. 2012;5:137–143. doi: 10.2147/JMDH.S31494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Font R, Espinas JA, Gil-Gil M, et al. Prescription refill, patient self-report and physician report in assessing adherence to oral endocrine therapy in early breast cancer patients: a retrospective cohort study in Catalonia, Spain. British Journal of Cancer. 2012;107(8):1249–1256. doi: 10.1038/bjc.2012.389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sadahiro S, Ohki S, Yamaguchi S, et al. Feasibility of a novel weekday-on/weekend-off oral UFT schedule as postoperative adjuvant chemotherapy for colorectal cancer. UFT Compliance Study Group, Kanagawa, Japan. Cancer Chemotherapy & Pharmacology. 2000;46(3):180–184. doi: 10.1007/s002800000146. [DOI] [PubMed] [Google Scholar]
- 10.Winterhalder R, Hoesli P, Delmore G, et al. Self-reported compliance with capecitabine: findings from a prospective cohort analysis. Oncology. 2011;80(1–2):29–33. doi: 10.1159/000328317. [DOI] [PubMed] [Google Scholar]
- 11.Ziller V, Kalder M, Albert US, et al. Adherence to adjuvant endocrine therapy in postmenopausal women with breast cancer. Annals of Oncology. 2009;20(3):431–436. doi: 10.1093/annonc/mdn646. [DOI] [PubMed] [Google Scholar]
- 12.Lee CR, Nicholson PW, Ledermann JA, Rustin GJS. Patient compliance with prolonged oral altretamine treatment in relapsed ovarian cancer. European Journal of Gynaecological Oncology. 1996;17(2):99–103. [PubMed] [Google Scholar]
- 13.Waterhouse DM, Calzone KA, Mele C, Brenner DE. Adherence to oral tamoxifen: a comparison of patient self-report, pill counts, and microelectronic monitoring. Journal of Clinical Oncology. 1993;11(6):1189–1197. doi: 10.1200/JCO.1993.11.6.1189. [DOI] [PubMed] [Google Scholar]
- 14.Ruddy KJ, Pitcher BN, Archer LE, et al. Persistence, adherence, and toxicity with oral CMF in older women with early-stage breast cancer (Adherence Companion Study 60104 for CALGB 49907) Annals of Oncology. 2012;23(12):3075–3081. doi: 10.1093/annonc/mds133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Saratsiotou I, Kordoni M, Bakogiannis C, et al. Treatment adherence of cancer patients to orally administered chemotherapy: insights from a Greek study using a self-reported questionnaire. Journal of Oncology Pharmacy Practice. 2011;17(4):304–311. doi: 10.1177/1078155210380292. [DOI] [PubMed] [Google Scholar]
- 16.Clarke Hillyer G, Neugut AI, Crew KD, et al. Use of a urine anastrozole assay to determine treatment discontinuation among women with hormone-sensitive breast cancer: a pilot study. Journal of Oncology Practice. 2012;8(5):e100–104. doi: 10.1200/JOP.2011.000487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Simons S, Ringsdorf S, Braun M, et al. Enhancing adherence to capecitabine chemotherapy by means of multidisciplinary pharmaceutical care. Supportive Care in Cancer. 2011;19(7):1009–1018. doi: 10.1007/s00520-010-0927-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Partridge AH, Archer L, Kornblith AB, et al. Adherence and persistence with oral adjuvant chemotherapy in older women with early-stage breast cancer in CALGB 49907: adherence companion study 60104. Journal of Clinical Oncology. 2010;28(14):2418–2422. doi: 10.1200/JCO.2009.26.4671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee CR, Nicholson PW, Souhami ME, et al. Patient compliance with prolonged low-dose oral etoposide for small cell lung cancer. British Journal of Cancer. 1993;67(3):630–634. doi: 10.1038/bjc.1993.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thivat E, Van Praagh I, Belliere A, et al. Adherence with oral oncologic treatment in cancer patients: interest of an adherence score of all dosing errors. Oncology. 2013;84(2):67–74. doi: 10.1159/000342087. [DOI] [PubMed] [Google Scholar]
- 21.Spoelstra SL, Given BA, Given CW, et al. An intervention to improve adherence and management of symptoms for patients prescribed oral chemotherapy agents: an exploratory study. Cancer Nursing. 2013;36(1):18–28. doi: 10.1097/NCC.0b013e3182551587. [DOI] [PubMed] [Google Scholar]
- 22.Cartei G, Cartei F, Interlandi G, et al. Oral 5-fluorouracil in squamous cell carcinoma of the skin in the aged. American Journal of Clinical Oncology. 2000;23(2):181–184. doi: 10.1097/00000421-200004000-00015. [DOI] [PubMed] [Google Scholar]
- 23.Uematsu T, Nakashima M, Fujii M, et al. Measurement of 5-fluorouracil in scalp hair: a possible index of patient compliance with oral adjuvant chemotherapy. European Journal of Clinical Pharmacology. 1996;50(1–2):109–113. doi: 10.1007/s002280050077. [DOI] [PubMed] [Google Scholar]
- 24.Partridge AH, LaFountain A, Mayer E, et al. Adherence to initial adjuvant anastrozole therapy among women with early-stage breast cancer. Journal of Clinical Oncology. 2008;26(4):556–562. doi: 10.1200/JCO.2007.11.5451. [DOI] [PubMed] [Google Scholar]
- 25.Partridge AH, Wang PS, Winer EP, Avorn J. Nonadherence to adjuvant tamoxifen therapy in women with primary breast cancer. Journal of Clinical Oncology. 2003;21(4):602–606. doi: 10.1200/JCO.2003.07.071. [DOI] [PubMed] [Google Scholar]



