Abstract
Objectives
To evaluate the association between caregiver burden and preventive dental care use for children with special health care needs (CSHCN) and assess if caregiver burden explains the relationship between child- and family-level characteristics and preventive dental care use.
Methods
Samples of U.S. CSHCN ages 3–17 years with a functional limitation (n=7,559) and those without (n=26,345) were derived from the 2005–2006 National Survey of CSHCN. We generated structural equation models, stratified by functional limitation, to describe the relationships between caregiver burden and preventive dental utilization. We measured caregiver burden using six items on whether the child's health condition impacted work, time spent on health management, and finances.
Results
About 80.9% of CSHCN used preventive dental care. Higher levels of caregiver burden were associated with significantly lower odds of preventive dental care use for CHSCN with a functional limitation (β=−0.06; P<0.001) and those without (β=−0.07; P<0.001). For CSHCN with a functional limitation, family poverty and being uninsured were significantly associated with greater caregiver burden and less preventive dental use. Findings were similar for CSHCN without a functional limitation, except that lower caregiver education was also associated with greater caregiver burden and less preventive dental care use.
Conclusions
Caregiver burden is potential barrier to preventive dental care use for CSHCN and explains the relationship between child- and family-level characteristics and preventive dental care use. Interventions to improve the oral health of CSHCN should include strategies to reduce caregiver burden, especially within socioeconomically vulnerable families.
Keywords: children with special health care needs, caregiver burden, preventive dental care use, oral health disparities, structural equation models
INTRODUCTION
The 2011 Institute of Medicine report “Improving Access to Oral Health Care for Vulnerable and Underserved Populations” highlights persisting disparities in access to dental care encountered by children with special health care needs (CSHCN) (1). Dental care is the most common unmet health care need among CSHCN (2). Nearly 80% of caregivers of CSHCN report that their child has unmet dental needs (3). While CSHCN may be slightly more likely to use preventive dental care than non-CSHCN (46.1% and 37.4%, respectively) (4), subgroups of CSHCN, including children with severe chronic health conditions, are significantly less likely to use preventive dental care than other CSHCN (5,6). For instance, lower proportions of CSHCN with a functional limitation used preventive dental care than CSHCN with no functional limitation (44.2% and 46.6%, respectively) (4). Potential barriers to dental care that uniquely affect CSHCN include: dentists' unwillingness to treat patients with special needs because of difficulties managing uncooperative behavior, systemic health care needs that are higher priority than dental care, transportation difficulties, and inadequate insurance. Because dental disease (e.g., tooth decay) is cumulative, poor access to preventive dental care over time may perpetuate disparities in oral health within subgroups of CSHCN. These disparities manifest as more frequent toothaches, emergency department visits to address dental problems, and hospitalizations under general anesthesia for oral rehabilitation (7–9).
Anecdotal evidence suggests that caregiver burden is a barrier to preventive dental care for CSHCN. Caregiver burden is defined as “the time and financial demands associated with caring for a child with disability that constrain the parental social role” (10). Most CSHCN are cared for by a parent who takes on the role of informal caregiver (11). Caregivers provide daily home-based care (e.g., administering medications, changing bandages and diapers, brushing the child's teeth), coordinate visits to health providers, and manage other responsibilities related to the child's health. Collectively, these responsibilities may disrupt the caregiver's professional, household, and social roles (12) and result in high levels of caregiver burden (13–15). A number of publications have documented the negative effects of caregiver burden on health outcomes for the caregiver (16–18). And while studies have examined caregiver burden and pediatric health outcomes (19–25), no study to date has assessed how caregiver burden is a potential barrier to preventive dental care for CSHCN. Furthermore, the potential mechanisms by which child- and family-level factors influence caregiver burden and dental use have not been elucidated.
To better understand the role of child- and caregiver-level factors on children's preventive health service utilization, we used a national dataset to examine the relationship between caregiver burden and preventive dental care use for CSHCN with and without functional limitations. We tested two hypotheses: 1) increased caregiver burden is associated with lower odds of preventive dental care use; and 2) caregiver burden explains the relationship between child- and family-level characteristics (e.g., race/ethnicity, insurance status, health condition severity, maternal education, family structure, family income) and preventive dental care use. This work is a first step in developing comprehensive family-centered interventions and policies that improve access to preventive dental care for CSHCN.
METHODS
Data and Study Population
We drew our study sample from the 2005–2006 U.S. National Survey of Children with Special Health Care Needs (NS-CSHCN), a random-digit dial telephone survey designed to calculate national and state-specific prevalence estimates of CSHCN and to describe characteristics of CSHCN under age 18 years (26). All responses to the survey were provided by the child's caregiver or legal guardian. The overall survey sample (n=38,866) contained approximately 750 CSHCN from each state. Blumberg and colleagues (2008) provide details on survey methods (27). In the current study, we restricted our sample to CSHCN ages 3–17 years with complete data on the covariates of interest (N=33,904), with the exception of family income where imputed income data were utilized. We excluded children under age 3 years because the determinants of dental use for young children are different (28) and our focus was on older children. This study was conducted in accordance with prevailing ethical principles and was approved for human subjects exemption by the University of Wisconsin at Madison Institutional Review Board.
Measures
Conceptual Model
We used the Behavioral Model for Vulnerable Populations (BMVP) proposed by Gelberg and colleagues (2000) to generate a model and select relevant covariates (29). The BMVP extends Andersen's original Behavioral Model developed in the 1960s by including measures that uniquely affect vulnerable populations. For instance, having a special health care need and functional limitations are examples of measures under the Need Vulnerable Domain. Cargiver burden is an example of a measure under the Enabling Vulnerable Domain. The BMVP is based on the premise that factors contributing to vulnerability are also likely to influence health behaviors.
Main predictor variable
We measured caregiver burden related to the child's health condition using six questions from the NS-CSHCN: 1) whether the parent stopped work (no/yes); 2) whether the parent reduced work hours (no/yes); 3) hours/week the parent spent providing health care to the child (0, <1, 1–5, 6–10, ≥11); 4) hours/week the parent spent coordinating the child's health care (<1, 1–5, 6–10, ≥11); 5) whether out-of-pocket expenses were ≥$1,000 in the past 12 months (no/yes); and 6) whether the family experienced financial problems because of the child's health care needs (no/yes).
Outcome measure
The outcome measure was parent-reported preventive dental care use by the child during the last 12 months (no/yes).
Model covariates
There were three child-level predisposing variables: age, gender, and race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, other). Child-level enabling factors measured two dimensions of the child's access to medical care services. The first was constancy of health insurance, a parent-reported measured indicating whether the child experienced any insurance lapse in the last year (no/yes). The second measure was whether the child had a medical home (no/yes). Specifically, children who met the following criteria were classified as having a medical home: 1) had a personal doctor or nurse; 2) had a usual source of care for well and sick care; 3) received family-centered compassionate, culturally effective care from all providers; 4) had no problem getting referrals; and 5) had effective care coordination. Our operationalization of medical home is consistent with the Maternal and Child Health Bureau's definition of medical home (30). Finally, we included two child-level need factors, severity of the child's health condition, which was measured by parent report of how often the child's condition affected function (never; very little; some; a great deal), as well as whether the child had a functional limitation (no/yes).
There were three maternal and family enabling characteristics: maternal education (did not complete high school, completed high school, completed more than high school); family structure (single parent, two-parent family); and family income (<100% Federal Poverty Level [FPL], 100% to <185% FPL, ≥185% FPL). We imputed missing income data using relevant files from the National Center for Health Statistics and methods described by Pedlow and colleagues (31).
Data Analyses
To test our study hypotheses, we used structural equation models (SEM), which allow us to partition out random measurement error (32). We used six indicators to measure the latent variable, caregiver burden. The SEM consists of a measurement model and a structural model. The measurement model indicates how well the six indicators of caregiver burden measure caregiver burden. Loadings indicate the magnitude of the relationship between item responses and caregiver burden levels. Thresholds describe the relative importance of each of the six indicators. The structural model describes the relationships between caregiver burden and other covariates in the model. We simultaneously estimated the association between: 1) each child and family characteristic and caregiver burden; and 2) caregiver burden and preventive dental care utilization controlling for child and family characteristics. In structural models, one interprets pathway coefficients similarly to regression coefficients. To evaluate model fit, we utilized the comparative fit index (CFI) and root mean square error of approximation (RMSEA). Consistent with guidelines from previous studies, we considered a CFI>0.95 or RMSEA<0.06 as indicating acceptable fit (33). We first tested the fit for just the measurement model and subsequently tested the fit of a model that included both the measurement and structural models (32).
After fitting the SEM, we tested for indirect effects for covariates for which there was a strong and statistically significant association with both caregiver burden and preventive dental care utilization using the delta method (34). Direct effects estimate the association between a covariate (e.g., family income) and the outcome variable (preventive dental care use). Indirect effects estimate the sum of the pathways between a covariate (e.g., family income) and caregiver burden, and between caregiver burden and the outcome variable (i.e., preventive dental care use). We estimated all models separately for CSHCN with and without a functional limitation since previous work suggests that caregiver burden varies depending on a child's functional limitations (35).
RESULTS
Descriptive Statistics
The study included 33,904 CSHCN, 22.3% of whom had a functional limitation (Table 1). Children were predominantly non-Hispanic White (70.6%), 58.9% were male, and 8.2% were uninsured at any point in the previous year. Most children had a mother who completed more than high school (71.4%) and were from families with incomes ≥185% FPL (62.9%).
Table 1.
Characteristics of study population of children with special health care needs (CSHCN) ages 3–17 (N=33,904) and CSHCN with a functional limitation (n=7,559) and CSHCN without a functional limitation (n=26,345)
| Characteristic | Weighted % | ||
|---|---|---|---|
|
| |||
| Whole sample (N=33,904) | CSHCN with a functional limitation (n=7,559) | CSHCN without a functional limitation (n=26,345) | |
|
| |||
| Main predictor variable: caregiver burden | |||
|
| |||
| Stopped work due to child's health condition | 11.4 | 27.8 | 6.7 |
|
| |||
| Reduced work hours due to child's health condition | 14.7 | 29.1 | 10.4 |
|
| |||
| Hours/week spent providing child's health care | |||
| 0 | 55.9 | 46.9 | 58.4 |
| <1 | 18.0 | 11.5 | 19.8 |
| 1–5 | 16.8 | 18.8 | 16.2 |
| 6–10 | 3.6 | 6.8 | 2.7 |
| ≥11 | 5.7 | 16.0 | 2.8 |
|
| |||
| Hours/week spent coordinating child's health care | |||
| <1 | 56.0 | 34.9 | 62.2 |
| 1–5 | 36.3 | 47.5 | 33.1 |
| 6–10 | 4.8 | 10.5 | 3.1 |
| ≥11 | 2.9 | 7.1 | 1.7 |
|
| |||
| Out of pocket expenses ≥$ 1,000 related to child's condition | 60.2 | 68.6 | 57.2 |
|
| |||
| Experienced financial problems due to child's health care needs | 17.5 | 34.2 | 12.6 |
|
| |||
| Main outcome variable: dental utilization | |||
|
| |||
| Used preventive dental care in last 12 months | 80.9 | 75.2 | 82.5 |
|
| |||
| Child characteristics | |||
|
| |||
| Age, weighted mean (SE mean) in years | 10.6 (0.03) | 10.6 (0.05) | 10.6 (0.03) |
|
| |||
| Gender | |||
| Male | 58.9 | 62.0 | 58.1 |
|
| |||
| Race/ethnicity | |||
| White, non-Hispanic | 70.6 | 66.5 | 71.8 |
| Black, non-Hispanic | 13.6 | 15.7 | 12.9 |
| Hispanic | 4.6 | 5.0 | 4.5 |
| Other | 11.2 | 12.7 | 10.8 |
|
| |||
| Uninsured at any point during the previous year | 8.2 | 10.4 | 7.6 |
|
| |||
| Has a medical home | 15.2 | 17.6 | 14.5 |
|
| |||
| Severity of health condition | |||
| None | 38.2 | 3.4 | 48.4 |
| Mild | 23.1 | 13.1 | 26.1 |
| Moderate | 27.4 | 49.0 | 21.2 |
| Severe | 11.2 | 34.6 | 4.4 |
|
| |||
| Has a functional limitation | 22.5 | 0.0 | 100.0 |
|
| |||
| Maternal and family characteristics | |||
|
| |||
| Maternal education | |||
| Less than high school | 5.8 | 8.2 | 5.1 |
| High school or equivalent | 22.8 | 27.0 | 21.6 |
| More than high school | 71.4 | 64.9 | 73.3 |
|
| |||
| Family structure | |||
| Lives in a single-parent household | 16.2 | 18.8 | 15.5 |
|
| |||
| Family income | |||
| <100% FPL | 18.4 | 25.6 | 16.3 |
| ≥100% and <185% FPL | 18.7 | 22.9 | 17.4 |
| ≥185% FPL | 62.9 | 51.5 | 66.2 |
About 11.4% of caregivers stopped work and 14.7% reduced work hours because of the child's health condition. The majority of caregivers (55.9%) spent zero hours providing health care to the child whereas 5.7% spent ≥11 hours/week. Most caregivers (56%) spent less than one hour/week coordinating health care for their child and 2.9% spent ≥11 hours/week. Over 60% had out-of-pocket health care expenses ≥$1,000 related to their child's condition and one-in-five caregivers experienced financial problems because of the child's condition.
Compared to caregivers of CSHCN with no functional limitation, larger proportions of caregivers of CSHCN with a functional limitation stopped working, reduced work hours, spent ≥11 hours/week providing or coordinating care, and experienced financial problems related to their child's condition.
Overall, 80.9% of CSHCN used preventive dental care in the previous 12 months. The frequency of preventive dental care was higher among CSHCN without a functional limitation compared to those with a functional limitation (82.5% and 75.2%, respectively).
Measurement Model
The measurement model fit acceptably (CFI=0.938; RMSEA=0.035) and we did not modify it (Table 2). The factor loadings for caregiver burden ranged from 0.34 to 0.75. The item with the highest factor loading was stopped work because of the child's health condition. The thresholds ranged from −0.18 to 2.16. The item with the highest threshold was spending ≥11 hours/week providing their child's care, indicating that this item was associated with relatively high levels of caregiver burden.
Table 2.
Results of the age-adjusted measurement model of caregiver burden for CSHCN with a functional limitation (n=7,559) and CSHCN without a functional limitation (n=26,345)
| CSHCN with a functional limitation (n=7,559) | CSHCN without a functional limitation (n=26,345) | |||
|---|---|---|---|---|
|
| ||||
| Factor Loading | Thresholds | Factor Loading | Thresholds | |
|
| ||||
| Caregiver burden | ||||
|
| ||||
| Stopped work due to child's health condition | 0.75 | 1.49 | 0.75 | 1.49 |
|
| ||||
| Reduced work hours due to child's health condition | 0.64 | 1.27 | 0.64 | 1.28 |
|
| ||||
| Hours per week spent providing child's health care | 0.45 | 0.45 | ||
| 0 | - | - | ||
| <1 | 0.26 | 0.26 | ||
| 1–5 | 0.78 | 0.78 | ||
| 6–10 | 1.52 | 1.52 | ||
| ≥11 | 1.83 | 1.83 | ||
|
| ||||
| Hours per week spent coordinating child's health care | 0.60 | 0.60 | ||
| <1 | - | - | ||
| 1–5 | 0.30 | 0.30 | ||
| 6–10 | 1.64 | 1.64 | ||
| ≥11 | 2.16 | 2.16 | ||
|
| ||||
| Out of pocket expenses ≥$ 1,000 related to child's condition | 0.34 | −0.18 | 0.34 | −0.18 |
|
| ||||
| Experienced financial problems due to child's health care needs | 0.67 | 0.43 | 0.67 | 0.43 |
Model fit: CFI=0.938; RMSEA =0.035
Structural Model
The results of the structural model for CSHCN with a functional limitation suggest that higher levels of caregiver burden were associated with lower odds of preventive dental care use (β=−0.059; P<0.001) (Figure 1). Having a more severe health condition (β=0.72; P<0.001), being uninsured at any point in the past year (β=0.21; P<0.001), and family income <100% FPL (β=0.33; P<0.001) were all associated with higher levels of caregiver burden. Being uninsured (β=−0.63; P<0.001), family income <100% FPL (β=−0.40; P<0.001), and maternal education of high school or less (β=−0.25; P<0.001) were all associated with significantly lower odds of preventive dental care use. Similar patterns emerged for CSHCN without a functional limitation (Figure 2).
Figure 1.
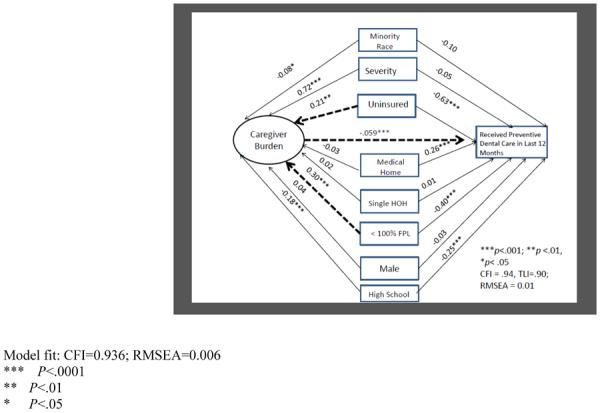
Results of the age-adjusted structural model of caregiver burden and preventive dental care use for CSHCN ages 3 to 17 with a functional limitation (n=7,559). Dashed arrows indicate statistically significant indirect effects.
Figure 2.
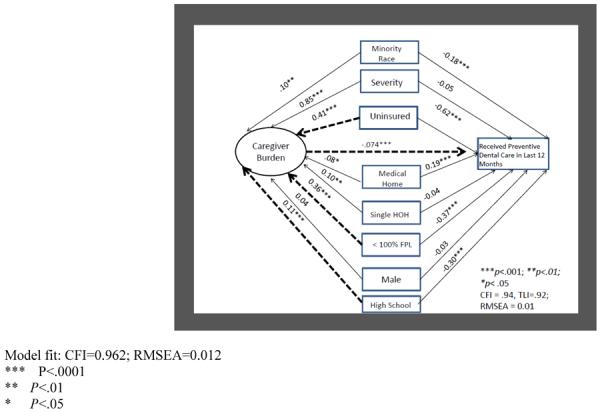
Results of the age-adjusted structural model of caregiver burden and preventive dental care use for CSHCN ages 3 to 17 without a functional limitation (n=26,345). Dashed arrows indicate statistically significant indirect effects.
Direct and Indirect Effects
For CSHCN with a functional limitation (Figure 1), two covariates were associated with caregiver burden and preventive dental care use – being uninsured and family income <100% FPL (Figure 1). The indirect effects analysis revealed that caregiver burden had a small, but significant explanatory effect on the association between preventive dental care use and family income <100% FPL (β=−0.03; P<0.001) and being uninsured (β=−0.02; P<0.001) (Table 3). For CSHCN without a functional limitation (Figure 2) three covariates were significantly associated with caregiver burden and the outcome – maternal education of high school or less, child being uninsured at any point during the last 12 months, and family income <100% FPL. Regarding indirect effects for CSHCN without a functional limitation, caregiver burden had a small, but significant explanatory effect on the association between preventive dental care utilization and family income <100% FPL (β=−0.03; P<0.001), maternal education of high school or less (β=−0.01; P<0.001), and being uninsured (β=−0.03; P<0.001).
Table 3.
Age-adjusted total, direct, and indirect effects in the structural model for CHSCHN with a functional limitation (n=7,559)and CSHCN without a functional limitation (n=26,345)
| Characteristic | % | Total | Indirect | Direct |
|---|---|---|---|---|
| CSHCN with a functional limitation | ||||
| Family income <100% FPL | 48.5 | −0.36*** | −0.03*** | −0 34*** |
| Child uninsured at any point during the previous year | 10.4 | −0.66*** | −0.02*** | −0.64*** |
| CHSCN without a functional limitation | ||||
| Family income <100% FPL | 33.8 | −0.40*** | −0.03*** | −0.37*** |
| Maternal education high school or less | 35.2 | −0.31*** | −0.01*** | −0.30*** |
| Child uninsured at any point during the previous year | 7.6 | −0.65*** | −0.03*** | −0.62*** |
P<.001;
P<.01;
P<.05
DISCUSSION
This is the first study to examine the relationship between caregiver burden and preventive dental care use for CSHCN. There were two main findings.
The first main finding is that, consistent with our hypothesis, we found a negative association between caregiver burden and preventive dental care use for CSHCN with and without a functional limitation. Previous research has not sufficiently explained why subgroups of CSHCN do not use preventive dental care services as recommended by the American Academy of Pediatric Dentistry (36). Our results are consistent with previous research on children with behavioral health difficulties suggesting that caregiver strain was related to decreased likelihood of subsequent outpatient visits (25) and increased non-specialty outpatient services (e.g., visits to the pediatrician, family physician, emergency department) (23) and other mental health services (19–21). This suggests that caregiver burden is associated with less primary prevention (e.g., well baby visits, dental checkups) and greater utilization of secondary and tertiary prevention services. In the context of our findings among CSHCN with varying diagnoses and needs, high caregiver burden may prompt parents to postpone or cancel preventive dental care for their child, which could eventually lead to increased use of the emergency department for treatment of dental problems. Recent recommendations from the American Academy of Pediatrics underscore the importance of family function to children's overall health and health service utilization (37). Pediatricians and other health professionals play an integral role in screening for caregiver burden and checking if a child is utilizing preventive dental care. For children who are not utilizing preventive care, a referral could be made to a local dentist. which is likely to improve child health outcomes and lower health care costs by reducing the need for emergency dental care. When caregiver burden is noted, dental referrals could include this information so that the dental staff has increased awareness of the child's family circumstances and can work with caregivers to develop tailored oral health strategies.
The second major finding of the paper is that caregiver burden explains the relationship between child- and family-level enabling characteristics and preventive dental care use. For CSHCN with a functional limitation, caregiver burden had indirect effects on the relationship between two enabling factors (any insurance lapse in the last year and household Federal Poverty Level) and preventive dental care use. For CSHCN without a functional limitation, caregiver burden had indirect effects on the relationship between an additional enabling factor (maternal education) and preventive dental care use. In other words, enabling factors are related to caregiver burden, which in turn, influences preventive dental care use for CSHCN. There are few studies to which we can compare these findings. In our models, caregiver burden explained the relationship between three measures of social disadvantage (child being uninsured in the previous 12 months, low family income, and low maternal education) and preventive dental care use. Previous research indicates the benefit of consistent health insurance and socioeconomic resources on both reducing caregiver burden (10,36) and promoting access to preventive dental care (38). However, ours is the first known study to simultaneously examine the roles of social disadvantage, caregiver burden, and preventive dental care utilization. Our models suggest that caregiver burden is an important construct to explain why CSHCN from families with fewer economic resources and inconsistent health insurance coverage are less likely to have preventive dental visits.
While caregiver burden did not mediate race and preventive dental care use in our models, a previous study found that caregiver stress mediated the relationship between African American race and mental health service use for children ages 8–20 (24). A possible explanation is dissimilar study populations, whereby a larger proportion of subjects in our study were White (70.6%) whereas in the other study 43% were non-Hispanic White and 57% were African American or Hispanic. Another study reported that mental health condition severity was a reliable predictor of caregiver strain (39), which is consistent with our models. However, in our study, the indirect effects of caregiver burden on condition severity and dental utilization were not significant. Additional work is needed to further clarify the mediating role of caregiver burden, particular between social and behavioral factors and preventive dental care use for CSHCN.
Our results also have clinical and policy relevance. For example, the measurement model indicates that parents with out-of-pocket expenses ≥$1,000 had relatively lower levels of caregiver burden while parents who spent ≥11 hours/week coordinating their child's care had higher levels of caregiver burden. This finding reinforces previous work that interventions and policies should focus on providing meaningful care coordination and respite services for caregivers of CSHCN (15) rather than direct financial remuneration for health care services. Care coordination and respite services could allow parents of CSHCN to better balance family and work responsibilities and further reduce caregiver burden.
In developing future interventions and policies, one might argue that reducing caregiver burden is not a feasible way to improve use of preventive dental care services for CSHCN because of high costs. However, based on a common risk factors approach (40,41), it is likely that reducing caregiver burden will lead to other health benefits for the child, caregiver, and family. For instance, reducing caregiver burden could help to improve use of other types of preventive health care services such as visits to the pediatrician for well child care (23). Targeting caregiver burden could also help parents to manage stress and regulate mood, which could lead to both short- and long-term health benefits for caregivers (42). Future efforts aimed at improving preventive dental care use for CSHCN should be incorporated into comprehensive efforts to improve access to primary health care services (43,44) and reduce the need for costly emergency department care. Furthermore, because caregiver burden appears to mediate the relationship between measures of social disadvantage and preventive dental care use, these interventions and policies should be tailored to socioeconomically vulnerable families to optimize health outcomes for CSHCN at greatest risk for health disparities.
This study had several strengths including the use of a multi-item caregiver burden measure with acceptable psychometric properties, the use of a latent variable approach on a nationally representative population of CSHCN, and analyses that accounted for functional limitation status as well as complex survey sampling methods. However, as with all studies, there are limitations. The first is that the data were cross-sectional, which precludes definitive conclusions regarding causality. Future work should examine the relationship between caregiver burden and preventive dental care use longitudinally. The second is that we did not include social and behavioral confounders (e.g., social connectedness, family function, self-efficacy, perceived susceptibility to disease) in our models because they were not part of the survey. In the future, researchers should collect relevant behavioral and social measures that are likely to part of a comprehensive explanatory model of preventive dental care use for CSHCN. Finally, we measured the primary outcome of interest (preventive dental use) by parent-report using one survey question. Future work could incorporate methods to validate self reports by linking survey and administrative claims data.
One-in-five CHSCN in our study did not utilize preventive dental care in the previous year, which is a missed opportunity to ensure that medically vulnerable children are able to benefit fully from dental care that prevents oral diseases. Oral health is inextricably linked to general health outcomes and health-related quality of life. Ensuring optimal oral health in medically vulnerable children is particularly important because dental disease can exacerate underlying systemic health conditions and may require families to devote limited resources to seeking invasive, costly restorative care for theis children. Our findings underscore the importance of ensuring that all barriers to preventive dental care for CSHCN are identified and eliminated. We also recognize that preventive dental care is not a panacea for dental diseae in CSHCN. There is a need to develop family-tailored strategies that help caregivers enforce consistent behaviors at home. Such behavioral strategies should include regular supervised toothbrushing with fluoridated toothpaste and enforcement of healthy diets (e.g., ensuring well-defined mealtimes, eliminating sugar sweetened beverages, reducing frequency of carbohydrate intake). Collectively, these efforts are likely to help CSHCN maintain optimal oral health and lead healthier lives.
CONCLUSION
Our study findings reveal that higher levels of caregiver burden are associated with significantly lower odds of preventive dental care use for CSHCN regardless of whether the child has a functional limitation. Interventions aimed at improving the oral and systemic health of CSHCN should include strategies to reduce caregiver burden, especially within socioeconomically vulnerable families.
ACKNOWLEDGMENTS
All phases of this study were supported by NIH/NIDCR Grant Number K08DE020856.
REFERENCES
- 1.Institute of Medicine (IOM) and National Research Council (NRC) Improving access to oral health care for vulnerable and underserved populations. The National Academies Press; Washington, DC: 2011. [Google Scholar]
- 2.Newacheck PW, Kim SE. A national profile of health care utilization and expenditures for children with special health care needs. Arch Pediatr Adolesc Med. 2005 Jan;159(1):10–7. doi: 10.1001/archpedi.159.1.10. [DOI] [PubMed] [Google Scholar]
- 3.Lewis C, Robertson AS, Phelps S. Unmet dental care needs among children with special health care needs: implications for the medical home. Pediatrics. 2005 Sep;116(3):e426–31. doi: 10.1542/peds.2005-0390. [DOI] [PubMed] [Google Scholar]
- 4.Iida H, Lewis C, Zhou C, Novak L, Grembowski D. Dental care needs, use and expenditures among U.S. children with and without special health care needs. J Am Dent Assoc. 2010 Jan;141(1):79–88. doi: 10.14219/jada.archive.2010.0025. [DOI] [PubMed] [Google Scholar]
- 5.Chi DL, Momany ET, Neff J, Jones MP, Warren JJ, Slayton RL, Weber-Gasparoni K, Damiano PC. Impact of chronic condition status and severity on dental utilization for Iowa Medicaid-enrolled children. Med Care. 2011 Feb;49(2):180–92. doi: 10.1097/MLR.0b013e3181f81c16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lewis CW. Dental care and children with special health care needs: a population-based perspective. Acad Pediatr. 2009 Nov-Dec;9(6):420–6. doi: 10.1016/j.acap.2009.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lewis C, Stout J. Toothache in US children. Arch Pediatr Adolesc Med. 2010 Nov;164(11):1059–63. doi: 10.1001/archpediatrics.2010.206. [DOI] [PubMed] [Google Scholar]
- 8.Lewis C, Lynch H, Johnston B. Dental complaints in emergency departments: a national perspective. Ann Emerg Med. 2003 Jul;42(1):93–9. doi: 10.1067/mem.2003.234. [DOI] [PubMed] [Google Scholar]
- 9.Chi DL, Momany ET, Neff J, Jones MP, Warren JJ, Slayton RL, Weber-Gasparoni K, Damiano PC. Impact of chronic condition status and severity on dental treatment under general anesthesia for Medicaid-enrolled children in Iowa state. Pediatr Anesth. 2010 Sep;20(9):856–65. doi: 10.1111/j.1460-9592.2010.03371.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McManus BM, Carle A, Acevedo-Garcia D, Ganz M, Hauser-Cram P, McCormick M. Modeling the social determinants of caregiver burden among families of children with developmental disabilities. Am J Intellect Dev Disabil. 2011 May;116(3):246–60. doi: 10.1352/1944-7558-116.3.246. [DOI] [PubMed] [Google Scholar]
- 11.Perrin JM. Health services research for children with disabilities. Milbank Q. 2002;80:303–324. doi: 10.1111/1468-0009.t01-1-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Green SE. “We're tired, not sad”: Benefits and burdens of mothering a child with a disability. Soc Sci Med. 2007;64:150–163. doi: 10.1016/j.socscimed.2006.08.025. [DOI] [PubMed] [Google Scholar]
- 13.Canning RD, Harris ES, Kelleher KJ. Factors predicting distress among caregivers to children with chronic medical conditions. J Pediatr Psychol. 1996;21:735–749. doi: 10.1093/jpepsy/21.5.735. [DOI] [PubMed] [Google Scholar]
- 14.Murphy NA, Christian B, Caplin DA, Young PC. The health of caregivers for children with disabilities: Caregiver perspectives. Child Care Health Dev. 2006;33:180–187. doi: 10.1111/j.1365-2214.2006.00644.x. [DOI] [PubMed] [Google Scholar]
- 15.Kuo DZ, Cohen E, Agrawal R, Berry JG, Casey PH. A national profile of caregiver challenges among more medically complex children with special health care needs. Arch Pediatr Adolesc Med. 2011 Nov;165(11):1020–6. doi: 10.1001/archpediatrics.2011.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Raina P, O'Donnell M, Schwellnus H, Rosenbaum P, King G, Brehaut J, Russell D, Swinton M, King S, Wong M, Walter SD, Wood E. Caregiving process and caregiver burden: conceptual models to guide research and practice. BMC Pediatr. 2004 Jan 14;4:1. doi: 10.1186/1471-2431-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Allik H, Larsson J, Smedje H. Health-related quality of life in parents of school-age children with Asperger syndrome or high-functioning autism. Health Qual Life Outcomes. 2006;4:1–8. doi: 10.1186/1477-7525-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kuhlthau K, Kahn R, Hill KS, Gnanasekaran S, Ettner SL. The well-being of parental caregivers of children with activity limitations. Matern Child Health J. 2010;14:155–163. doi: 10.1007/s10995-008-0434-1. [DOI] [PubMed] [Google Scholar]
- 19.Bussing R, Zima BT, Gary FA, Mason DM, Leon CE, Sinha K, Garvan CW. Social networks, caregiver strain, and utilization of mental health services among elementary school students at high risk for ADHD. J Am Acad Child Adolesc Psychiatry. 2003 Jul;42(7):842–50. doi: 10.1097/01.CHI.0000046876.27264.BF. [DOI] [PubMed] [Google Scholar]
- 20.Garland AF, Aarons GA, Brown SA, Wood PA, Hough RL. Diagnostic profiles associated with use of mental health and substance abuse services among high-risk youths. Psychiatr Serv. 2003 Apr;54(4):562–4. doi: 10.1176/appi.ps.54.4.562. [DOI] [PubMed] [Google Scholar]
- 21.Garland AF, Lau AS, Yeh M, McCabe KM, Hough RL, Landsverk JA. Racial and ethnic differences in utilization of mental health services among high-risk youths. Am J Psychiatry. 2005 Jul;162(7):1336–43. doi: 10.1176/appi.ajp.162.7.1336. [DOI] [PubMed] [Google Scholar]
- 22.María Brannan A, Heflinger CA. Child behavioral health service use and caregiver strain: comparison of managed care and fee-for-service Medicaid systems. Ment Health Serv Res. 2005 Dec;7(4):197–211. doi: 10.1007/s11020-005-7452-z. [DOI] [PubMed] [Google Scholar]
- 23.Chavira DA, Garland A, Yeh M, McCabe K, Hough RL. Child anxiety disorders in public systems of care: comorbidity and service utilization. J Behav Health Serv Res. 2009 Oct;36(4):492–504. doi: 10.1007/s11414-008-9139-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shin SH, Brown TA. Racial and ethnic disparities in caregiver strain and the use of child mental health services: a structural equation model. Psychiatr Serv. 2009 Aug;60(8):1039–45. doi: 10.1176/ps.2009.60.8.1039. [DOI] [PubMed] [Google Scholar]
- 25.Larson JJ, Yoon Y, Stewart M, dosReis S. Influence of caregivers' experiences on service use among children with attention-deficit hyperactivity disorder. Psychiatr Serv. 2011 Jul;62(7):734–9. doi: 10.1176/ps.62.7.pss6207_0734. [DOI] [PubMed] [Google Scholar]
- 26. [Accessed on April 9, 2012];Data Resource Center for Child and Adolescent Health Website. Available at: http://www.childhealthdata.org/.
- 27.Blumberg SJ, Welch EM, Chowdhury SR, Upchurch HL, Parker EK, Skalland BJ. Design and operation of the National Survey of Children with Special Health Care Needs, 2005–2006. National Center for Health Statistics. Vital Health Stat. 2008;45:11188. [PubMed] [Google Scholar]
- 28.Kanellis MJ, Damiano PC, Momany ET. Utilization of dental services by Iowa Medicaid-enrolled children younger than 6 years old. Pediatr Dent. 1997;19:310–314. [PubMed] [Google Scholar]
- 29.Gelberg L, Andersen RM, Leake BD. The Behavioral Model for Vulnerable Populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000 Feb;34(6):1273–302. [PMC free article] [PubMed] [Google Scholar]
- 30.The Child and Adolescent Health Measurement Initiative. Measuring Medical Home for Children and Youth; A Resource Manual for Child Health Program Leaders, Researchers, and Analysts; Data Resource Center on Child and Adolescent Health; Portland, OR: 2009. [Google Scholar]
- 31.Pedlow S, Luke J, Blumberg S. Multiple imputation values for National Survey of Children With Special Health Care Needs, 2001, and National Survey of Children's Health, 2003. U.S. Centers for Disease Control and Prevention; Division of Health Interview Statistics, Survey Planning and Special Surveys Branch; 2007. [Accessed on April 9, 2012]. Available at: http://www.cdc.gov/nchs/data/slaits/mimp01_03.pdf. [Google Scholar]
- 32.Bollen KA. Structural Equations with Latent Variables. Wiley Series in Probability and Mathematical Statistics. Wiley; New York: 1989. [Google Scholar]
- 33.Hu L, Bentler PM. Evaluating Model Fit. In: Hoyle RH, editor. Structural equation modeling: concepts, issues, and applications. Sage; Thousand Oaks: CA: 1995. [Google Scholar]
- 34.MacKinnon DP. Introduction to Statistical Mediation Analysis. Erlbaum; New York, NY: 2008. [Google Scholar]
- 35.Canning RD, Harris ES, Kelleher KJ. Factors predicting distress among caregivers to children with chronic medical conditions. J Pediatr Psychol. 1996 Oct;21(5):735–49. doi: 10.1093/jpepsy/21.5.735. [DOI] [PubMed] [Google Scholar]
- 36.American Academy of Pediatric Dentistry (AAPD) Guideline on caries-risk assessment and management for infants, children, and adolescents. Pediatr Dent. 2011;33(special issue):110–117. [PubMed] [Google Scholar]
- 37.Wertlieb D. Converging trends in family research and pediatrics: Recent findings for the American academy of pediatrics task force on the family. Pediatrics. 2003;111:1572, 1587. [PubMed] [Google Scholar]
- 38.Liu J, Probst JC, Martin AB, Wang JY, Salinas CF. Disparities in dental insurance coverage and dental care among US children: the National Survey of Children's Health. Pediatrics. 2007 Feb;119(Suppl 1):S12–21. doi: 10.1542/peds.2006-2089D. [DOI] [PubMed] [Google Scholar]
- 39.Brannan AM, Heflinger CA. Caregiver, child, family, and service system contributors to caregiver strain in two child mental health service systems. J Behav Health Serv Res. 2006 Oct;33(4):408–22. doi: 10.1007/s11414-006-9035-1. [DOI] [PubMed] [Google Scholar]
- 40.Sheiham A, Watt RG. The common risk factor approach: a rational basis for promoting oral health. Community Dent Oral Epidemiol. 2000 Dec;28(6):399–406. doi: 10.1034/j.1600-0528.2000.028006399.x. [DOI] [PubMed] [Google Scholar]
- 41.Watt RG, Sheiham A. Integrating the common risk factor approach into a social determinants framework. Community Dent Oral Epidemiol. 2012 Aug;40(4):289–96. doi: 10.1111/j.1600-0528.2012.00680.x. [DOI] [PubMed] [Google Scholar]
- 42.Perlick DA, Miklowitz DJ, Lopez N, Chou J, Kalvin C, Adzhiashvili V, Aronson A. Family-focused treatment for caregivers of patients with bipolar disorder. Bipolar Disord. 2010 Sep;12(6):627–37. doi: 10.1111/j.1399-5618.2010.00852.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Farmer JE, Clark MJ, Sherman A, Marien WE, Selva TJ. Comprehensive primary care for children with special health care needs in rural areas. Pediatrics. 2005 Sep;116(3):649–56. doi: 10.1542/peds.2004-0647. [DOI] [PubMed] [Google Scholar]
- 44.Cook JR, Kilmer RP. The importance of context in fostering responsive community systems: supports for families in systems of care. Am J Orthopsychiatry. 2010 Jan;80(1):115–23. doi: 10.1111/j.1939-0025.2010.01014.x. [DOI] [PubMed] [Google Scholar]


