Abstract
This study evaluated a tailored intervention to promote sun protection in parents and their children, hypothesizing that the tailored intervention would lead to improved skin cancer prevention behaviors compared to generic materials. Families were recruited through schools and community centers and were included if there was one child in Grades 1–3 at moderate to high risk for skin cancer. Participants were randomized into one of two intervention groups: a tailored intervention, in which they received personalized skin cancer education through the mail; or a control group who received generic skin cancer information materials. Both pre- and post-intervention, parents completed questionnaires about their and their children’s skin cancer risk and prevention knowledge and behaviors. Parents also completed 4-day sun exposure and protection diaries for their child and themselves. Tailored group participants demonstrated significantly greater positive changes in prevention behavior after the intervention, including children’s use of sunscreen, shirts, and hats, and parents’ use of shade, and skin examinations. Effect sizes were small and perceived benefits and social norms mediated intervention effects. Findings from this study support the efficacy of focusing tailored communications to families in order to change skin cancer prevention practices in young children.
Skin cancer is the most common cancer diagnosed in the United States (Rogers et al., 2010) and has increased in the past two decades, producing an enormous public health burden and substantial health costs (Chen et al., 2001; Housman et al., 2003). Epidemiologic research has consistently highlighted sun exposure as the principal environmental cause of cutaneous melanoma (Armstrong & Kricker, 2001). Researchers estimate that significant risk for skin cancer begins during childhood as a result of sun exposure and the resultant sunburns (Gandini et al., 2005; Truhan, 1991). By developing interventions that target children, particularly those at higher risk for developing skin cancer, substantial reductions in morbidity and mortality from all forms of skin cancer can be achieved.
Unfortunately, targeting those at high risk remains difficult because there is no standard or widely accepted definition of skin cancer risk among children. There is a growing literature on assessment of various components of skin cancer risk (Fears et al., 2006; Glanz et al., 2003) and physical assessment of risk among children (Aalborg et al., 2009; Crane et al., 2009). However, to date, no one has developed a practical tool that can readily assess children’s risk for skin cancer, nor evaluated how such a tool might effectively be used as part of a cancer prevention intervention.
Previous childhood skin cancer intervention programs have been conducted in many different environments (Hart & DeMarco, 2008; Saraiya et al., 2004) including primary schools (Eakin, Maddock, Techur-Pedro, Kaliko, & Derauf, 2004; Hunter et al., 2010), child care centers,(Aulbert et al., 2009) recreational settings (Glanz, Geller, Shigaki, Maddock, & Isnec, 2002), through health care providers (Norman et al., 2007), and through public health announcements via media outlets (Smith, Ferguson, McKenzie, Bauman, & Vita, 2002). Parental involvement has been reported to be a crucial element of behavior change programs for children.(Fielding & Teutsch, 2010)These programs use standard messages for groups of participants and have yielded mixed results. Existing skin cancer literature lacks personalization in contrast to other areas of prevention research in families and children where tailored interventions have proven effective (Noar, Benac, & Harris, 2007). A tailored intervention involving both parents and children may provide a low-cost, convenient, and efficacious opportunity to target individuals at highest risk for developing skin cancer later in life, and is the focus of the present study. The aim of the present research was to develop and evaluate a tailored intervention we hypothesized would help decrease children’s skin cancer risk by reducing sun exposure, improving sun protection behaviors, and increasing parental skin examinations for children.
Methods
Present Study
The present research was conducted as part of Project SCAPE (Skin Cancer Awareness, Prevention and Education), which consisted of two trials to evaluate the impact of a mailed, tailored intervention, relative to standard skin cancer education materials, on prevention and early detection of skin cancer in moderate to high risk individuals. The Project SCAPE adult trial findings have been reported previously (Glanz, Schoenfeld, & Steffen, 2010). This trial targeted children and their parents.
The Project SCAPE family trial was a randomized controlled trial in which the intervention group received multiple mailings with tailored skin cancer prevention materials, and the control group received a single mailing of standardized skin cancer informational materials. Skin cancer prevention behaviors were assessed at the beginning and end of the summer season, approximately 16 weeks later.
Project SCAPE was conducted in two geographical regions in the United States: Hawaii and Suffolk County, a coastal county of Long Island, New York, to include participants from various ethnic groups and climatic regions.
Sample Recruitment
Children were recruited during the Spring of 2000 and 2001 from a convenience sample of cooperating schools and recreation programs on Long Island, New York and in Hawaii (on Oahu and Maui). Inclusion criteria were: 1) child in grade 1, 2, or 3; 2) resident of Suffolk County, NY or Hawaii; and 3) at moderate or high risk for skin cancer, as determined by the children’s Brief skin cancer Risk Assessment Tool (BRAT) (described in Measures, below). Exclusion criteria included: 1) parent currently being treated for any kind of skin cancer, 2) non-English speaking, 3) plans to be away from home for more than two weeks during the summer, or 4) report of currently practicing sun precautions always when outdoors. If a family included more than one child in grades 1 to 3, only the oldest child was included in the study.
Children were given a packet from their teacher to take to their parents explaining the study and inviting them to participate. The packet included a letter to the parents, a copy of the BRAT for children and a consent/information form to be mailed in a pre-stamped envelope to the research center. The information form requested the child’s name and age, and the parent’s contact information.
Baseline Assessment and Randomization
After enrollment, each parent of an eligible child was sent a packet with two additional measures of skin cancer preventive behaviors and attitudes for their child. The Sun Habits Survey (SHS) inquired about general sun protection habits and related attitudes, and the Sun Exposure Diary (SED) was used to record specific sun protection practices on specific days (described in Measures section, below). After these were returned, families were randomized (using a computerized random number generator in Microsoft Excel) to the intervention group (tailored communications) or the control group. Randomization was stratified by study site and skin cancer risk level, so that equivalent numbers of moderate and high risk participants were included in each group.. Interviewers and data collectors were blinded to group allocation. All interventions were conducted during the summer months.
Intervention and Follow-Up Assessments
The tailored messages and materials were based on the Health Belief Model (Champion & Skinner, 2008) and Social Cognitive Theory (Bandura, 2005). Tailoring variables included risk levels and specific risk factors from the children’s BRAT; reported sun exposure, sun protection, and skin examination practices (both parent and child); readiness to change; barriers to change; and extent of sunscreen application (parent and child), from the baseline SHS. The key constructs of risk perception, barriers and benefits (from the Health Belief Model), behavioral capability (knowledge of skills), and social norms (from Social Cognitive Theory) were hypothesized mediating variables (Baron & Kenny, 1986).
Two to three weeks after randomization, participants began receiving mailings according to the group to which they were assigned. The control group received a single mailing: a standard skin cancer prevention and detection information brochure for children published by the Skin Cancer Foundation, a tip sheet on use of sunscreen, hats, shade, and shirts to protect from the sun published by the American Cancer Society, and a bookmark encouraging child skin examination. The intervention group received three packets, mailed two weeks apart, containing personalized risk feedback and recommendations based on responses to the baseline questionnaire, interactive skin cancer education materials (using pictures and graphics), a family fun guide (which included games and stories about safe sun practices that parents and children could complete together), suggestions for overcoming barriers, and reminders to engage in preventive practices. About two weeks after the second tailored-group mailing, an interviewer contacted all parents by telephone and conducted an interview, querying sun exposure and sun protection habits for the preceding weekend, and receipt of and reactions to the intervention materials.
The third and final packet of tailored intervention materials was then mailed; its contents were unaffected by the telephone interview. Twelve weeks after the baseline survey, all participants were sent a second SHS and SED to assess efficacy of the interventions. Reminders and follow-up telephone calls were made to respondents who had not returned the survey and diary after two weeks. To improve participation and retention, the families received small gift incentive items such as magnets, pens, beanbag animals (“Beanie Babies”), and movie/video rental coupons for returning surveys and diaries.
Measures
BRAT
The BRAT was originally developed to provide a short, self-administered instrument to reliably assess skin cancer risk among adults. The reliability of the adult version was established in a related study (Glanz, et al., 2003). A children’s version of the BRAT was developed for the present study using similar methodology. The questionnaire asked parents about family history of melanoma, number of large moles (≥ 1/8th inch diameter for children), freckles, sunburn history, and sun sensitivity (i.e., skin color, natural hair color, ease of sun tanning and sun burning) (MacKie, 1998; Weinstock, 1992; Westerdahl, Olsson, Masback, Ingvar, & Jonsson, 1996). The BRAT focuses primarily on malignant melanoma risk factors.
The scoring system is based on the relative risk of melanoma for each risk factor. The BRAT was pilot tested with a separate group of 90 children of similar age to the intervention study (6.7 ± 0.9 years), to whom the BRAT was administered four weeks apart. Risk categories were defined by tertile BRAT scores, as described in previous publications (Glanz et al., 2009; Glanz, et al., 2003). The children’s BRAT was found to have acceptable to good test-retest reliability, with good to excellent weighted kappas of .59 to .98 for various items. Using a dichotomous risk measure of “low risk” vs. “moderate or high risk,” over 81% of the participants would be classified in the same category at the two separate administrations. Using the three-group classification, 72.5% of children did not change their risk assessment score categories between the first and the second risk assessment. Thus, the children’s BRAT instrument was sufficiently reliable to determine eligibility for the main trial.
Sun Habits Survey (SHS)
The SHS was developed specifically for Project SCAPE. The children’s version was a modified version of the adult Project SCAPE survey, reported in a previous article (Glanz, Schoenfeld, et al., 2010). In the children’s version, sun exposure was measured by parent-reported average number of hours their child spent outside between 10 a.m. and 4 p.m., weekdays and weekends. Sun protection practices of children were assessed by measuring five protective behaviors (wearing shirt, sunglasses, and hat; staying in the shade; using sunscreen) and six parent behaviors (same five plus limiting time in midday sun) on 4-point ordinal scales. Sunscreen application of both parent and child was also assessed. The parent’s perception of general risks and benefits, social norms, knowledge about sun protection, and parent intent to increase their own sun protection were also assessed as potential mediators of sun protection behavior. The follow-up SHS asked the same questions, excluding demographic characteristics.
Internal consistency was assessed using baseline data from the full study: Cronbach alpha’s for subscale scores ranged from .45 to .85. Alpha coefficients for parent sun protection habit scores were higher (.61) than for child sun protection habit scores (.46). Test-retest reliability of the SHS variables was assessed in a preliminary study of 52 parents and children with repeated administrations of the SHS, about four weeks apart. Overall, test-retest reliability for both parent and child measures was good at .87 using the ICC (intraclass correlation coefficient).
Sun Exposure Diary (SED)
The SED is a four-day record of sun exposure and protective behaviors developed for Project SCAPE. The children’s version is a modified version of the adult SED (Glanz, Schoenfeld, et al., 2010). Parents completed the diary on behalf of their child for two weekdays and two weekend days for the hours 10 a.m. and 4 p.m., sufficient for estimating weekly behavior (Glanz, Silverio, & Farmer, 1997). The category of the child’s outdoor activities was recorded (e.g., transport, recreation/sport). Time indoors was also recorded. Sun protection habits assessed for each recorded hour were: using sunscreen, wearing a hat, staying in the shade, and covering up. The level of the child’s sun protection was calculated by dividing the amount of time the parent reported them using each type of sun protection by the amount of time spent outside for that day, resulting in a range from 0 to 100 percent. The main outcomes for the diary were calculated by averaging across all four days of measurement. Outcomes included measures of “usual sun protection” for each of the four habits (averaged across 4 diary days), an “average percent of all methods” across the four habits (i.e., composite Sun Protection Habits Index), and an indicator of “any sun protection,” the use of any of the four sun protection behaviors. Test-retest reliability of the SED measure of average percent overall child Sun Protection, assessed with the same 52 families described above for the SHS, was .69, and for percentage of any sun protection method used, .73, using the average ICC method.
Reactions to interventions
Questions about parents’ reactions to the mailed materials were included in the follow-up SHS. Parents were asked to rate the materials they received on a scale of 1 to 5 (1= did not like at all to 5=liked very much) for six features: easy to understand, informative, interesting, personally relevant, attractive, and confusing.
Statistical Methods
Sample size calculations assumed a baseline score of 20% on the composite Sun Protection Habits Index (range: 0–100%) from the SED and an intervention effect of four point improvement in the tailored intervention group, resulting in a required sample size of 400 per group, or 800 total. Participants who completed the SHS at baseline and follow-up were considered to have completed the study and were included in the analysis (517 in the tailored intervention group and 530 in the control group). Bivariate analyses (e.g., χ2 test, t-test) were conducted to examine possible characteristics associated with attrition and incomplete data.
The multivariate analyses of intervention effects were analyzed (in SAS 9.2, SAS Institute Inc, Cary, NC) using three approaches. For interval scale survey outcomes, a mixed model approach (i.e., PROC MIXED) was used with a data set containing two records per person and a time variable indicating baseline and follow-up administrations. This approach allows for the test of the (fixed) intervention-by-time interaction effect while accounting for the random effects associated with correlated repeated measurements (Littell, Pendergast, & Natarajan, 2000). For the binomial variables, generalized linear models (PROC GENMOD) were used modeling a binomial distribution and generalized estimating equations accounted for the covariance structure of the repeated measurements. The diary variables required a different analytic approach due to their more extreme non-normal distributions. Using a simple change score (i.e., follow-up score – baseline score), diary change variables had distributions that were appropriate for multiple regression. Skin cancer risk level (medium or high) and location (Hawaii or Suffolk County, NY) were tested as moderators of intervention effect, and when not significant, were included as covariates throughout main effect multivariate analyses.
Reactions to the tailored and standard materials were compared for the two groups using Wilcoxon rank sums test. Mediator analyses were conducted using autoregressive mediation path models for individual mediators using Mplus, version 6.12 (Muthén & Muthén, Los Angeles, CA). (MacKinnon, 2008). Results are provided for the Comparative Fit Index (CFI), Root Mean Square Error of Approximation (RMSEA), and the Tucker-Lewis Index (TLI), three standard measures of model fit.
Descriptive statistics are reported as mean ± standard deviation (SD) for continuous variables and counts or percentages for categorical ones.
Results
Sample Characteristics
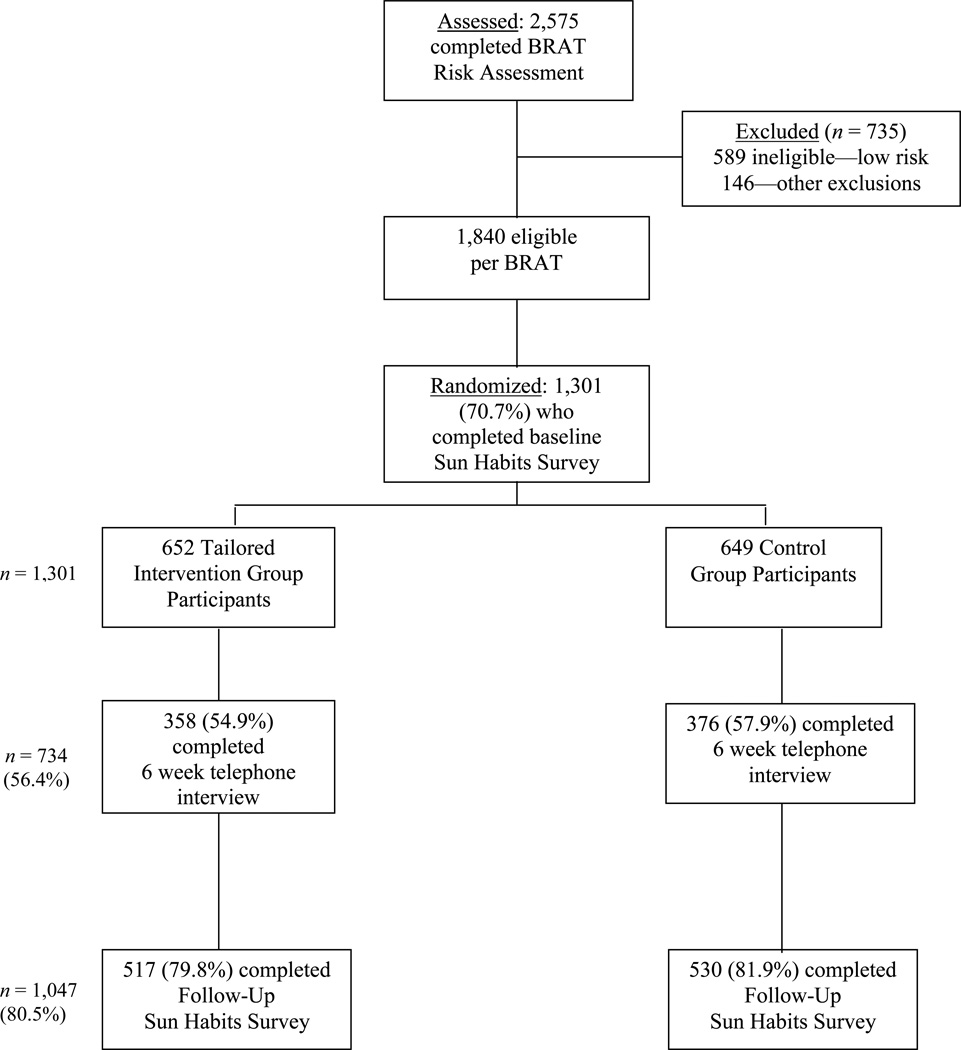
Figure 1 details the participation rates at each phase of data collection. The initial response rates to the take-home packet ranged from 20% to 50% from the various sites. Among families screened and found eligible, the response rate to the baseline mailed packet was 71%. During this two year study, 1,301 participants (610 from Hawaii and 691 from Suffolk County, NY) from separate families completed the baseline SHS and were randomized into the two intervention groups that resulted in groups with no significant differences in their baseline characteristics (see Table 1). The child participants were approximately two-thirds Caucasian, half male, and with an average age of 7.1 years. About 38% were categorized as high risk (the rest were moderate risk) and 40% had two or more sunburns the previous summer. Sun protection habit scores averaged 2.19, between “sometimes” and “usually” on the 4 point scale. Over 90% of the responding parents were mothers, almost 90% were married, and 40% were college graduates.
FIGURE 1.
Participant Flow through the Family SCAPE Study
Table 1.
Tailored Intervention Study: Baseline Characteristics of Participants, by Study Groupa
| Enrolled | Completed | |||||
|---|---|---|---|---|---|---|
| Characteristic | Total Enrolledbc |
Intervention | Control | Intervention | Control | p-value (completers) |
| (N = 1301), % or Mean (SD) |
(n = 652) , % or Mean (SD) |
(n = 649) , % or Mean (SD) |
(n = 517) , % or Mean (SD) |
(n = 530) , % or Mean (SD) |
||
| Children | ||||||
| Ethnicity (% Caucasian) | 65.6 | 65.3 | 65.8 | 65.6 | 65.1 | .82 |
| Gender (% female) | 49.0 | 50.5 | 47.5 | 50.5 | 48.4 | .5 |
| Age (M+SD; range 4–10) | 7.1 (1.1) | 7.1 (1.1) | 7.1 (1.1) | 7.1 (1.1) | 7.0 (1.1) | .51 |
| Risk level (% high risk) | 38.3 | 38.5 | 38.1 | 36.4 | 38.3 | .52 |
| Sunburns (% having two or more last summer) | 40.4 | 40.8 | 40.0 | 41.3 | 40.9 | .91 |
| Skin examination by parent (% in last 3 mos.) | 57.7 | 58.3 | 57.0 | 59.4 | 56.2 | .3 |
| Sun Protection Habits Index (range 1–4) | 2.19 (0.47) | 2.19 (0.47) | 2.18 (0.46) | 2.19 (0.47) | 2.19 (0.46) | .98 |
| Parent risk perception for child (range 1–5) | 2.99 (0.90) | 2.97 (0.90) | 3.02 (0.90) | 3.22 (0.87) | 3.23 (0.85) | .95 |
| Parent-rated health of child (range 1–5) | 4.27 (0.33) | 4.27 (0.34) | 4.27 (0.33) | 4.27 (0.33) | 4.28 (0.33) | .87 |
| Parents | ||||||
| Ethnicity (% Caucasian) | 68.2 | 67.6 | 68.7 | 67.7 | 67.9 | .62 |
| Marital Status (% married or living together) | 88.7 | 89.2 | 88.2 | 89.3 | 89 | .86 |
| Education (% college graduates) | 40.2 | 41.6 | 38.8 | 42.3 | 39.7 | .45 |
| Employment (% full-time) | 42.7 | 44.8 | 40.6 | 44.9 | 41.1 | .38 |
| Household income (% $40K or higher) | 73.0 | 72.9 | 73.2 | 74.6 | 75.7 | .38 |
| Household size (M+SD; range 2–16) | 4.4 (1.1) | 4.3 (1.0) | 4.4 (1.2) | 4.3 (1.0) | 4.4 (1.2) | .35 |
No statistically significant differences were found between completers and non-completers.
Sample sizes smaller for some items due to missing data
Chi-square tests were used to assess relationships for categorical variables and t-tests for continous variables; no significant differences were found.
Approximately 80% of those enrolled were retained through the end. Attrition was significantly greater among participants who had income <$40,000, or had “other mixed” race children and spouse (those who do not fit into four categories of white, Asian, Pacific Islander, or Hawaiian). Attrition did not differ by intervention group, and neither race nor income interacted with treatment to predict dropouts. Among those completing baseline and follow-up surveys, 22% did not complete both baseline and follow-up diaries. Participants with missing diary data more often resided in Suffolk County, NY, and the parents had lower baseline (and follow-up) Sun Protection Habits and knowledge scores. Asian, Pacific Islander, and Hawaiian participants were more likely to have completed diaries compared to Caucasians and “other mixed” race, as were college graduates.
Between Hawaii and New York, some differences were noted. Participants from Hawaii had proportionally more non-whites, males, more persons with lower income (<$40,000 per year), more likely to be a college graduate, work full-time, not married or living with a partner, and live in three person or less households. They reported proportionally fewer child skin exams within the past three months at baseline and their children’s mean age was slightly higher. There were more children considered high risk for skin cancer in Hawaii, while baseline child sun protection habits were lower. No other differences between locations were found.
Intervention Effects
Survey data
Table 2 presents the adjusted means for sun protection, sun exposure, sunburn, and skin examination outcomes. There was a statistically significant time-by-intervention interaction effect favoring the intervention group for total children’s Sun Protection Habits [effect size (ES)=0.16], use of sunscreen (ES=0.13), wearing shirts and hats (ES=0.12, 0.11), and sunglasses (ES= 0.07), but not for staying in the shade. There was a trend toward increased practice of skin examination of the children which was moderated by location with an effect in Suffolk County, NY (ES=0.22) but not in Hawaii (ES=−0.02).
Table 2.
Effects of Tailored Messages on Children’s Sun Protection and Skin-Examination: Survey Results
| Intervention (n=517)b | Control (n=530)b | ||||
|---|---|---|---|---|---|
| Variable: Adjusted Mean (SE)a | Baseline | Follow-up | Baseline | Follow-up | p-value |
| Sun Protection Habits Indexc | 2.19 (0.02) | 2.48 (0.02) | 2.19 (0.02) | 2.34 (0.02) | <.0001 |
| Use Sunscreen | 3.06 (0.03) | 3.33 (.03) | 3.16 (0.03) | 3.24 (0.03) | <.0001 |
| Wear a Shirt | 2.33 (0.04) | 2.60 (0.04) | 2.28 (0.04) | 2.33 (0.04) | <.001 |
| Wear a Hat | 1.92 (0.04) | 2.25 (0.04) | 1.97 (0.04) | 2.13 (0.04) | <.001 |
| Stay in Shade | 1.98 (0.03) | 2.33 (0.03) | 1.91 (0.03) | 2.24 (0.03) | .53 |
| Wear Sunglasses | 1.66 (0.03) | 1.88 (0.03) | 1.64 (0.03) | 1.76 (0.03) | .03 |
| Sun Exposure Between 10 and 4d | 3.41 (0.05) | 2.98 (0.05) | 3.45 (0.05) | 3.08 (0.05) | .24 |
| Weekday Sun Exposure | 3.11 (0.05) | 2.71 (0.05) | 3.21 (0.05) | 2.80 (0.05) | .81 |
| Weekend Sun Exposure | 3.71 (0.06) | 3.26 (0.06) | 3.70 (0.05) | 3.35 (0.05) | .12 |
| Sunburnse | 1.61 (0.04) | 1.27 (0.04) | 1.68 (0.04) | 1.37 (0.04) | .67 |
| Skin-Examination (by parent)f | 0.60 (0.14) | 0.87 (0.06) | 0.57 (0.18) | 0.81 (0.06) | .06 |
Means calculated with adjustment for covariates: location and risk group. Mixed models were used unless otherwise stated with p-value indicating the significance of the time × intervention term.
n’s for separate analyses lower due to some missing data
Range of values: 1=rarely to 4=always
Range of values: 1=1 or less to 6=6 hours per day
Range of values: 1=one to 5=5 or more sunburns
Proportion adjusted for covariates. Model was a generalized linear model with binomial distribution using GEE.
Table 3 shows the effects of the intervention on the parents’ sun self-care. As with the children, there was also a statistically significant time-by-intervention interaction effects favoring the intervention group for total Sun Protection Habits (ES=0.07), sunscreen use (ES=0.06), staying in the shade (ES=0.08), limiting exposure during peak hours (ES=0.07), weekday sun exposure (ES=0.08) and skin self-examination (ES=0.14). Hat use among parents showed an effect moderated by risk level: moderate risk control group and high risk intervention group participants showed larger gains than those at moderate risk (ES=0.08).
Table 3.
Effects of Tailored Messages on Parent Sun Protection Habits and Skin Self-Examination: Survey Results
| Intervention (n=517)b | Control (n=530)b | ||||
|---|---|---|---|---|---|
| Variable: Adjusted Mean (SE)a | Baseline | Follow-up | Baseline | Follow-up | p-value |
| Sun Protection Habits Indexc | 2.43 (0.02) | 2.62 (0.02) | 2.39 (0.02) | 2.53 (0.02) | .02 |
| Use Sunscreen | 2.83 (0.04) | 3.06 (0.04) | 2.81 (0.04) | 2.94 (0.04) | .04 |
| Wear a Shirt | 2.32 (0.04) | 2.38 (0.04) | 2.17 (0.04) | 2.22 (0.04) | .86 |
| Wear a Hat | 1.69 (0.04) | 1.82 (0.04) | 1.66 (0.04) | 1.82 (0.04) | .52 |
| Stay in Shade | 2.33 (0.03) | 2.61 (0.03) | 2.34 (0.03) | 2.50 (0.03) | .01 |
| Wear Sunglasses | 2.98 (0.05) | 3.13 (0.05) | 2.90 (0.04) | 3.03 (0.04) | .52 |
| Limit Exposure in Peak Hours | 2.44 (0.04) | 2.74 (0.04) | 2.47 (0.04) | 2.66 (0.04) | .02 |
| Sunscreen Application Indexd | 5.92 (0.12) | 6.12 (0.12) | 5.82 (0.12) | 6.01 (0.12) | .95 |
| Sun Exposure Between 10 and 4e | 2.80 (0.05) | 2.46 (0.05) | 2.83 (0.05) | 2.43 (0.05) | .29 |
| Weekday Sun Exposure | 2.31 (0.06) | 2.10 (0.06) | 2.44 (0.05) | 2.03 (0.05) | .01 |
| Weekend Sun Exposure | 3.27 (0.06) | 2.83 (0.06) | 3.22 (0.06) | 2.83 (0.06) | .54 |
| Sunburnsf | 1.46 (0.04) | 1.00 (0.04) | 1.49 (0.04) | 1.03 (0.04) | .97 |
| Skin Self-Examinationg | 0.54 (0.33) | 0.79 (0.07) | 0.52 (0.60) | 0.71 (0.08) | .03 |
Means calculated with adjustment for covariates: location and risk group. Mixed models were used unless otherwise stated with p-value indicating the significance of the time × intervention term.
n’s for separate analyses lower due to some missing data
Range of values: 1=rarely to 4=always
Range of values: 0=none to 9=all exposed body parts
Range of values: 1=1 or less to 6=6 hours per day
Range of values: 0=none to 3=3 or more sunburns
Proportion adjusted for covariates. Model was a generalized linear model with binomial distribution using GEE.
Diary data
Analysis of the SED data showed that the intervention group had significant improvement on the Sun Protection Habits index (ES=0.35) as well as for use of any sun protection method, and wearing a shirt and/or hat as compared to the control group (Table 4).
Table 4.
Effects of Tailored Messages on Children’s Sun Protection: Sun Exposure Diary Results
| Intervention | Control | ||
|---|---|---|---|
| Variable: Adjusted Mean (SE) of change scorea,b | (n=417)c | (n=434)c | p-valued |
| Average Sun Protection Habits | 6.12 (0.72) | 0.80 (0.71) | <.0001 |
| Any Sun Protection | 9.51 (1.78) | 0.79 (1.74) | <.001 |
| Use Sunscreen | 1.58 (1.85) | −0.15 (1.82) | .51 |
| Wear a Shirt | 13.93 (1.85) | 2.21 (1.81) | <.0001 |
| Wear a Hat | 2.95 (1.16) | −1.96 (1.14) | <.005 |
| Stay in Shade | 6.01 (1.53) | 3.11 (1.50) | .18 |
| Sun Exposure Totale | −0.46 (0.07) | −0.36 (0.07) | .31 |
| Sun Exposure Weekdayse | −0.47 (0.10) | −0.32 (0.10) | .27 |
| Sun Exposure Weekendse | −0.44 (0.10) | −0.36 (0.10) | .59 |
Means calculated with adjustment for covariates: risk group and location.
Range of values: −100 to 100 change scores, i.e., % used at follow-up - % used at baseline
n’s for some analyses are lower because scores were not calculated when respondent stayed indoors
F test result for intervention effect from GLM model
Range of values: −7 to 7 hours, i.e., follow-up hours - baseline hours
Mediators analysis
Among the a priori mediators tested (perceived risks (parent and child), benefits, barriers, social norms, knowledge, and parent intent to increase sun protection), intervention condition was related to follow-up levels of Perceived Benefits and Social Norms, controlling for baseline levels, which were, in turn, related to follow-up child sun habits, controlling for baseline level of each mediator and the outcome. All seven models showed adequate fit (RMSEA range .00-.06, CFI range .98–1.0, TLI range .96–1.01). Perceived Benefits mediated 4.2% of the total intervention effect, and Social Norms mediated 9.7% of the total intervention effect, as tested in separate models.
Reactions to interventions
Both study groups had positive reactions to the mailings; most scores exceeded 4 on a 5-point scale. The intervention participants rated their materials significantly higher than the control group in terms of ease of understanding, interest, relevance, attractiveness and information (all ps<.001).
Discussion
Findings from this study support the effectiveness of focusing tailored communications on a family unit to change skin cancer prevention practices in young children. The intervention proved successful in changing sun protective habits for both children and parents, with statistically significant improvements in overall sun protective habits and the use of sunscreen compared to the control group. Children in the intervention group had greater increases in their use of hats and shirts, and parents increased their use of shade. Children’s sun exposure did not decrease after the intervention and parents’ weekday sun exposure decreased significantly. Skin self-examinations increased among adults in the intervention group and for children, skin self-examinations increased among Suffolk County, NY participants. Outcomes assessed by children’s sun exposure diaries were similar and showed a larger effect size for overall Sun Protection Habits than did survey results (ES=0.35 for diary, ES = 0.16 for survey).
A 2005 national survey of US adults found that younger, more educated, Caucasian participants adhered more to sun protection practices, consistent with the differences observed by race and education in the present trial, and suggesting that it may be beneficial to select a target audience where an impact can be made both in the parent and child (Hay, Coups, Ford, & DiBonaventura, 2009). Skin cancer prevention in the home may also be useful, as school policies and practices may be insufficient in terms of promoting more covering-up practices (Eakin, et al., 2004; Hunter, et al., 2010; Saraiya, et al., 2004). Day camps, summer camps, and outdoor recreation settings such as swimming pools may also support sun habits improvements (Glanz, et al., 2002; Glanz, Lew, Song, & Murakami-Akatsuka, 2000).
Sun protection research in schools and childcare centers have generally found such interventions to increase knowledge and use of sun protection methods; (Aulbert, et al., 2009; Hunter, et al., 2010). Limitations of past research include a lack of generalization to home use (Hunter, et al., 2010) and the need for parents to be present to reinforce the childrens’ behavior (Aulbert, et al., 2009; Fielding & Teutsch, 2010; Hunter, et al., 2010).
The Sun Sense Study conducted in Los Angeles pediatric medical practices showed improvements in sunscreen and hat use among their pediatric population but, similar to other reported studies and to the findings of the present study, did not impact the duration of children’s sun exposure (Glasser, Shaheen, Glenn, & Bastani, 2010). The fact that these prior intervention studies with children were not successful in decreasing sun exposure or increasing shade use may reflect the limited amount of shade areas available for children during outside play. We note that, in contrast, the present study had a positive impact on shade seeking behavior and reduced weekday sun exposure in the parents, while the Project SCAPE adult trial (Glanz, Schoenfeld, et al., 2010) did not find greater shade use or limiting sun exposure in the intervention group. It is possible that focusing on the children was an effective indirect method to influence parents’ behavior in this Family Study.
Strengths of this study include the inclusion of two geographically distinct regions, the multiethnic sample, a high participant retention rate through the trial, and an intervention that included tailored materials directed to the child with activities for the parent and child do together. Limitations include the short duration of follow-up through a single summer season, small to medium effect sizes, differences between intervention and control groups in number of mailings received, and the reliance on parent reports of children’s behavior when they may not have been supervised continuously. The small to medium effect sizes for some behaviors may not be considered clinically significant, but they might be considered cost-effective given the low cost of the tailored interventions. Because this was a first efficacy trial, future effectiveness studies should be conducted, perhaps with modifications or enhancements to the tailored materials.
The use of parental report of children’s behaviors and nevus counts, and of their own behavior, are limitations common to skin cancer prevention trials, although our recent validation study shows reasonable concordance between self-report and objective measures of sunscreen use (Smith, et al., 2002), covering-up (O’Riordan et al., 2009), and UVR exposure (Glanz et al., 2010).
The findings from this study advance current knowledge regarding tailoring behavioral interventions for skin cancer prevention among families with children at increased risk for skin cancer. They have the potential to focus prevention efforts on those who can most benefit from them during childhood, a time when both the biological and social foundations of skin cancer are established. Continued research into tailored interventions appears warranted, to further explore the most effective interventions for preventing damaging skin exposure at an early age for those at risk.
Acknowledgments
This work was supported by a grant from the National Cancer Institute [Grant number CA 76419]. Dr. Karen Glanz’s effort was supported in part by a Distinguished Scholar Award from the Georgia Cancer Coalition.
The authors wish to acknowledge the contributions of Martin Weinstock, Gabriela Layi, Jeanne Kidd, and Jennifer Chee in the development and conduct of this trial.
Contributor Information
Karen Glanz, University of Pennsylvania School of Medicine, Philadelphia, Pennsylvania, USA.
Alana D. Steffen, Cancer Research Center of Hawai’i, University of Hawai’i
Elinor Schoenfeld, School of Medicine, Stony Brook University.
Karyn A. Tappe, University of Pennsylvania School of Medicine, Philadelphia, Pennsylvania, USA
References
- Aalborg J, Morelli JG, Mokrohisky ST, Asdigian NL, Byers TE, Dellavalle RP, Crane LA. Tanning and Increased Nevus Development in Very-Light-Skinned Children Without Red Hair. Archives of Dermatology. 2009;145(9):989–996. doi: 10.1001/archdermatol.2009.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong BK, Kricker A. The epidemiology of UV induced skin cancer. Journal of Photochemistry and Photobiology B: Biology. 2001;63(1–3):8–18. doi: 10.1016/s1011-1344(01)00198-1. [DOI] [PubMed] [Google Scholar]
- Aulbert W, Parpart C, Schulz-Hornbostel R, Hinrichs B, Kruger-Corcoran D, Stockfleth E. Certification of sun protection practices in a German child day-care centre improves children’s sun protection--the ‘SunPass’ pilot study. British Journal of Dermatology. 2009;161(Suppl 3):5–12. doi: 10.1111/j.1365-2133.2009.09443.x. [DOI] [PubMed] [Google Scholar]
- Bandura A. The Evolution of Social Cognitive Theory. In: Smith KG, Hitt MA, editors. Great Minds in Management: The Process of Theory Development. 1st ed. Oxford: Oxford University Press; 2005. pp. 9–35. [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Champion VL, Skinner CS. The Health Belief Model. In: Glanz K, Rimer B, Viswanath K, editors. Health Behavior and Health Education. 4th ed. San Francisco: Jossey-Bass; 2008. pp. 45–65. [Google Scholar]
- Chen JGABF, Jr., Smith ED, Kancler C, Goldman ND, Williford PM, Feldman SR. Cost of Nonmelanoma Skin Cancer Treatment in the United States. Dermatologic Surgery. 2001;27(12):1035–1038. doi: 10.1046/j.1524-4725.2001.01004.x. [DOI] [PubMed] [Google Scholar]
- Crane LA, Mokrohisky ST, Dellavalle RP, Asdigian NL, Aalborg J, Byers TE, Morelli JG. Melanocytic Nevus Development in Colorado Children Born in 1998: A Longitudinal Study. Archives of Dermatology. 2009;145(2):148–156. doi: 10.1001/archdermatol.2008.571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eakin P, Maddock J, Techur-Pedro A, Kaliko R, Derauf DC. Sun Protection Policy in Elementary Schools in Hawaii. Preventing Chronic Disease. 2004;1(3):1–10. [PMC free article] [PubMed] [Google Scholar]
- Fears TR, Guerry D, IV, Pfeiffer RM, Sagebiel RW, Elder DE, Halpern A, Tucker MA. Identifying Individuals at High Risk of Melanoma: A Practical Predictor of Absolute Risk. Journal of Clinical Oncology. 2006;24(22):3590–3596. doi: 10.1200/JCO.2005.04.1277. [DOI] [PubMed] [Google Scholar]
- Fielding JE, Teutsch SM. Skin cancer prevention: sunnyside up or scrambled? Journal of the National Cancer Institute. 2010;102(7):445–447. doi: 10.1093/jnci/djq056. [DOI] [PubMed] [Google Scholar]
- Gandini S, Sera F, Cattaruzza MS, Pasquini P, Picconi O, Boyle P, Melchi CF. Meta-analysis of risk factors for cutaneous melanoma: II. Sun exposure. European Journal of Cancer. 2005;41(1):45–60. doi: 10.1016/j.ejca.2004.10.016. [DOI] [PubMed] [Google Scholar]
- Glanz K, Geller AC, Shigaki D, Maddock JE, Isnec MR. A randomized trial of skin cancer prevention in aquatics settings: the Pool Cool program. Health Psychology. 2002;21(6):579–587. [PubMed] [Google Scholar]
- Glanz K, Gies P, O’Riordan DL, Elliott T, Nehl E, McCarty F, Davis E. Validity of self-reported solar UVR exposure compared with objectively measured UVR exposure. Cancer Epidemiol Biomarkers Prev. 2010;19(12):3005–3012. doi: 10.1158/1055-9965.EPI-10-0709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glanz K, Lew RA, Song V, Murakami-Akatsuka L. Skin cancer prevention in outdoor recreation settings: effects of the Hawaii SunSmart Program. Effective Clinical Practice. 2000;3(2):53–61. [PubMed] [Google Scholar]
- Glanz K, McCarty F, Nehl EJ, O’Riordan DL, Gies P, Bundy L, Hall DM. Validity of Self-Reported Sunscreen Use by Parents, Children, and Lifeguards. American Journal of Preventive Medicine. 2009;36(1):63–69. doi: 10.1016/j.amepre.2008.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glanz K, Schoenfeld E, Steffen A. A Randomized Trial of Tailored Skin Cancer Prevention Messages for Adults: Project SCAPE. American Journal of Public Health. 2010;100(4):735–741. doi: 10.2105/AJPH.2008.155705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glanz K, Schoenfeld E, Weinstock MA, Layi G, Kidd J, Shigaki DM. Development and reliability of a brief skin cancer risk assessment tool. Cancer Detection and Prevention. 2003;27(4):311–315. doi: 10.1016/s0361-090x(03)00094-1. [DOI] [PubMed] [Google Scholar]
- Glanz K, Silverio R, Farmer A. Daily Diary reveals sun protective practices. Primary Care and Cancer. 1997;17(5):21–23. [Google Scholar]
- Glasser A, Shaheen M, Glenn BA, Bastani R. The sun sense study: an intervention to improve sun protection in children. American Journal of Health Behaviors. 2010;34(4):500–510. doi: 10.5993/ajhb.34.4.11. [DOI] [PubMed] [Google Scholar]
- Hart KM, DeMarco RF. Primary Prevention of Skin Cancer in Children and Adolescents: A Review of the Literature. Journal of Pediatric Oncology Nursing. 2008;25(2):67–78. doi: 10.1177/1043454208314499. [DOI] [PubMed] [Google Scholar]
- Hay J, Coups EJ, Ford J, DiBonaventura M. Exposure to mass media health information, skin cancer beliefs, and sun protection behaviors in a United States probability sample. Journal of the American Academy of Dermatology. 2009;61(5):783–792. doi: 10.1016/j.jaad.2009.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Housman TS, Williford PM, Feldman SR, Teuschler HVABF, Jr., Goldman ND, Chen GJ. Nonmelanoma Skin Cancer: An Episode of Care Management Approach. Dermatologic Surgery. 2003;29(7):700–711. doi: 10.1046/j.1524-4725.2003.29185.x. [DOI] [PubMed] [Google Scholar]
- Hunter S, Love-Jackson K, Abdulla R, Zhu W, Lee J-H, Wells KJ, Roetzheim R. Sun Protection at Elementary Schools: A Cluster Randomized Trial. Journal of the National Cancer Institute. 2010;102(7):484–492. doi: 10.1093/jnci/djq010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Littell RC, Pendergast J, Natarajan R. Modelling covariance structure in the analysis of repeated measures data. Statistics in Medicine. 2000;19(13):1793–1819. doi: 10.1002/1097-0258(20000715)19:13<1793::aid-sim482>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- MacKie RM. Incidence, risk factors and prevention of melanoma. European Journal of Cancer. 1998;34(Supplement 3):3–6. doi: 10.1016/s0959-8049(98)00003-3. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP. Indroduction to Statistical Mediation Analysis. New York: Lawrence Erlbaum Associations; 2008. [Google Scholar]
- Noar SM, Benac CN, Harris MS. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychological Bulletin. 2007;133(4):673–693. doi: 10.1037/0033-2909.133.4.673. [DOI] [PubMed] [Google Scholar]
- Norman GJ, Adams MA, Calfas KJ, Covin J, Sallis JF, Rossi JS, Patrick K. A Randomized Trial of a Multicomponent Intervention for Adolescent Sun Protection Behaviors. Archives of Pediatric & Adolescent Medicine. 2007;161(2):146–152. doi: 10.1001/archpedi.161.2.146. [DOI] [PubMed] [Google Scholar]
- O’Riordan DL, Nehl E, Gies P, Bundy L, Burgess K, Davis E, Glanz K. Validity of covering-up sun-protection habits: Association of observations and self-report. Journal of the American Academy of Dermatology. 2009;60(5):739–744. doi: 10.1016/j.jaad.2008.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers HW, Weinstock MA, Harris AR, Hinckley MR, Feldman SR, Fleischer AB, Coldiron BM. Incidence Estimate of Nonmelanoma Skin Cancer in the United States, 2006. Archives of Dermatology. 2010;146(3):283–287. doi: 10.1001/archdermatol.2010.19. [DOI] [PubMed] [Google Scholar]
- Saraiya M, Glanz K, Briss PA, Nichols P, White C, Das D, Rochester P. Interventions to prevent skin cancer by reducing exposure to ultraviolet radiation: A systematic review. American Journal of Preventive Medicine. 2004;27(5):422–466. doi: 10.1016/j.amepre.2004.08.009. [DOI] [PubMed] [Google Scholar]
- Smith BJ, Ferguson C, McKenzie J, Bauman A, Vita P. Impacts from repeated mass media campaigns to promote sun protection in Australia. Health Promotion International. 2002;17(1):51–60. doi: 10.1093/heapro/17.1.51. [DOI] [PubMed] [Google Scholar]
- Truhan AP. Sun Protection in Childhood. Clinical Pediatrics. 1991;30(12):676–681. doi: 10.1177/000992289103001205. [DOI] [PubMed] [Google Scholar]
- Weinstock MA. Assessment of sun sensitivity by questionnaire: validity of items and formulation of a prediction rule. Journal of Clinical Epidemiology. 1992;45(5):547–552. doi: 10.1016/0895-4356(92)90104-u. [DOI] [PubMed] [Google Scholar]
- Westerdahl J, Olsson H, Masback A, Ingvar C, Jonsson N. Risk of malignant melanoma in relation to drug intake, alcohol, smoking and hormonal factors. British Journal of Cancer. 1996;73(9):1126–1131. doi: 10.1038/bjc.1996.216. [DOI] [PMC free article] [PubMed] [Google Scholar]