Abstract
Traditional medicine plays a vital role for primary health care in India, where it is widely practiced to treat various ailments. Among those obtained from the healers, 78 medicinal plants were scientifically evaluated for antibacterial activity. Methanol extract of plants (100 μg of residue) was tested against the multidrug resistant (MDR) Gram-negative and Gram-positive bacteria. Forty-seven plants showed strong activity against Burkholderia pseudomallei (strain TES and KHW) and Staphylococcus aureus, of which Tragia involucrata L., Citrus acida Roxb. Hook.f., and Aegle marmelos (L.) Correa ex Roxb. showed powerful inhibition of bacteria. Eighteen plants displayed only a moderate effect, while six plants failed to provide any evidence of inhibition against the tested bacteria. Purified compounds showed higher antimicrobial activity than crude extracts. The compounds showed less toxic effect to the human skin fibroblasts (HEPK) cells than their corresponding aromatic fractions. Phytochemical screening indicates that the presence of various secondary metabolites may be responsible for this activity. Most of the plant extracts contained high levels of phenolic or polyphenolic compounds and exhibited activity against MDR pathogens. In conclusion, plants are promising agents that deserve further exploration. Lead molecules available from such extracts may serve as potential antimicrobial agents for future drug development to combat diseases caused by the MDR bacterial strains as reported in this study.
1. Introduction
Treatment of infections is compromised worldwide by the emergence of bacteria that are resistant to multiple antibiotics [1]. New and emerging drug resistance bacteria strains, particularly methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant enterococci (VRE), Mycobacterium tuberculosis (MTB), and multidrug resistance (MDR) Gram-negative bacteria, are increasing worldwide and add to the gravity of the situation [2]. S. aureus cause a variety of syndromes such as food poisoning, toxic shock syndrome, skin lesions [3], hyperproliferative skin disease [4], and atopic dermatitis [5, 6]. Community-acquired pneumonia caused by Streptococcus pneumoniae, Klebsiella pneumonia, and S. aureus accounts for significant mortality in Southeast Asia [7]. Melioidosis has been recognized as an important human infection caused by Burkholderia pseudomallei in Singapore, Malaysia, Thailand, and Northern Australia [8, 9]. Cases have also been reported from some other tropical and subtropical regions like Africa and America, and a number of cases in man has recently been reported to increase in China, Taiwan, and South India [10, 11]. Infection with antibiotic resistant bacteria negatively impacts on public health, due to an increased incidence of treatment failure and severity of diseases. Development of resistant bacteria due to the chromosomal mutations is more commonly associated with the horizontal transfer of resistance determinants borne on mobile genetic elements [12]. B. pseudomallei is intrinsically resistant to many antibiotics [13, 14]. Considering the higher cost for producing synthetic drugs and the various side effects associated with their use, the need to search for alternative agents from medicinal plants and essential oils used in folklore medicine is further justified to overcome these issues. In India, there are about 550 tribal communities covered under 227 ethnic groups residing in about 5000 villages throughout different forest and vegetation regions [15]. India is one of the world's 12 megabiodiversity countries [16, 17]. Plant derived medicines have played a major role in human societies throughout the history and prehistory of mankind [18]. The traditional healers (traditional physicians) or medicinemen have a long history of their own diagnostic and treatment system, which they have acquired from their ancestors [19]. Approximately 80% of the world population still relies on traditional medicine for the treatment of common diseases [20–22]. Medicinal plants thus offer significant potential for the development of novel antibacterial therapies and adjunct treatments [23]. Plant derived drugs serve as a prototype to develop more effective and less toxic medicines. In previous studies, few attempts were made to confirm the antimicrobial activity of some indigenous medicinal plants [24, 25]. Not only extracts of various medicinal plants but also essential oils and their constituents have been investigated for their antimicrobial properties against bacteria and fungi [26–28].
The principal compounds from the leaves showed a better antibacterial activity against P. aeruginosa and B. subtilis bacteria and a significant antifungal activity on C. albicans [29]. The essential oil from R. officinalis (alpha pinene/verbenone/bornyl acetate) was found to be more sensitive to the Gram-positive bacteria (MIC 2.5–4 mg/mL) than to the Gram-negative bacteria [30]. Several essential oils kill bacteria by damaging the cell membrane structure and inhibiting their membrane function [31]. Because of the antimicrobial potency of plant extracts and oils, they become a rich source of raw materials for many biotechnological and pharmaceutical industries for the development of therapeutic drugs. The increasing trend in the use of aromatic plants and essential oils in food, cosmetic, and pharmaceutical industries suggests that a systematic study of traditional medicinal plants is very important in order to find active compounds from such sources [32–34]. The purpose of this study is to survey and investigate popular medicinal aromatic plants and their essential oils with a view to fight against multidrug resistant human pathogens. In the present study, 71 plant species were selected on the basis of the available medicinal information and screened for their in vitro antimicrobial efficacy against bacteria.
2. Materials and Methods
2.1. Ethnomedicinal Survey and Collection of Plants
Ethnomedicinal surveys were conducted during March 1998 and July 2001 from various tribal localities (Kolli hills, Kalrayan hills, Pachamalai, Javadi hills, Mundanthurai) of Eastern and Western Ghats, Tamil Nadu, India. For ethnobotanical studies, questioners were used to collect the general information on the tribes, and the key information on medicinal details was collected through interviews. The medicinal plants were identified by a taxonomist using the standard Flora of Tamil Nadu Carnatic [35], and the voucher specimens were deposited in the department's herbarium at the Entomology Research Institute, Loyola College, Chennai, India.
2.2. Preparation of Plant Extracts
Using a Soxhlet apparatus, the shade-dried and powdered plant materials (200 g of each) were extracted with 1000 mL of methanol (CH3OH) for 10 h. The collected methanol extracts were filtered (Whatman no. 1 filter paper) and evaporated with a rotary evaporator and freeze dryer (lyophilized) to obtain the crude extracts (Buchi, Labortechnik AG, Switzerland). The dried crude extracts were stored at 4°C for antimicrobial assays [34].
2.3. Culture of Microorganisms
The following Gram-negative: Burkholderia pseudomallei (TES21), Burkholderia pseudomallei (KHW22), Klebsiella pneumoniae (ATCC15380), Klebsiella pneumoniae, Pseudomonas aeruginosa (ATCC27853), Vibrio damsela, and Salmonella typhi (ATCC51812) and Gram-positive: Staphylococcus aureus (ATCC 29213), Streptococcus pyogenes, and Streptococcus pneumoniae (ATCC49619) microorganisms were used for cultures. B. pseudomallei bacterial strains such as KHW and TES were isolated from the patient samples obtained from the Department of Microbiology, NUS, Singapore. The strains were subcultured on 20 mL Tryptic Soy (TS) and Mueller Hinton (MH) agar plates (pH 7.4) and incubated overnight at 37°C before use.
2.4. Antimicrobial Activity
The standard bacterial cultures were stored at −70°C, subcultured on 20 mL MH and TS agar plates (pH 7.4), and incubated overnight at 37°C prior to use. The antimicrobial property was tested using the disc-diffusion method [36]. Five young colonies of each strain of bacteria taken from their respective cultures grown overnight on TS agar plates (Oxoid limited, Wode Road, Basingstoke, Hants, England, UK) were suspended in 5 mL of sterile saline (0.9%), and the density of the suspension was adjusted to approximately 3 × 108 colony forming unit (CFU). The swab was used to inoculate the dried surface of TS agar plate by streaking four times over the surface of the agar and rotating the plate approximately 90°C to ensure an even distribution of the inoculums. The medium was allowed to dry for about 3 min before adding a 6 millimeter in diameter (mm) sterile paper disc (Becton Dickinson, USA) on the surface. Each disc was tapped gently down onto the agar to provide a uniform contact. Lyophilized residue (100 μg/mL) of each plant extracts and purified fractions was weighed and dissolved in 1 mL of water, and 20 μL of the extracts and oils (containing 100 μg of residue) were applied on each disc (3 replicates), while the sterile blank disc served as a normal control. The antimicrobial effect of the extracts on the clinical isolates was determined in comparison with the reference antibiotics (chloramphenicol 30 μg/disc and ceftazidime 30 μg/disc), which were used as positive controls. The plates were incubated at 37°C for 24 h, and the inhibition zones were measured and calculated.
2.5. Minimum Inhibitory Concentrations (MICs) Assay
MICs were evaluated based on the in vitro screening of 16 purified fractions that were found to have potent antimicrobial activity. Broth dilution method was used for the MIC assay with some slight modifications as recommend by the NCCLS [37]. Two-fold serial dilutions of all the fractionated compounds were made with MH and TS broth in microtiter plate wells to adjust the final concentration from 7.8 to 250 μg/mL, while wells containing the broth alone without any sample served as a control. Three replicates (n = 3) were used for each dilution and culture containing approximately 1 × 105 CFU/mL. The plates were incubated at 37°C for 24 h, and the absorbance was measured at 560 nm.
2.6. Cytotoxicity Assay
The cytotoxic effects of various extracts were tested by MTT assay [38] using human skin fibroblast HEPK cells. The toxic effect of plant extracts and essential oils was assayed on human skin fibroblast (HEPK) cell proliferation in 96-well microtitre plates. Confluent cells (5 × 106 cells per well) were incubated with extracts and oils for 24 h, and the percentage inhibitory concentration (IC50) was determined.
2.7. Phytochemical Analysis of Plant Extracts
The most active extracts were used for purification of antimicrobial compounds [39]. 100 g each of the plant powder was percolated with 500 mL of 4% aqueous HCl (adjusted to pH 2) and heated at 50°C for 3 h. The extract was washed with 2 × 250 mL of diethyl ether, and the organic phase evaporated to dryness using vacuum rotary evaporator. The dark brown gummy residues obtained by acid hydrolysis were chromatographed on silica gel column 60 × 3.2 cm (60–120 mesh, pH 7, Merck) by gradually eluting with n-hexane/ethyl acetate (8 : 2; 6 : 4; 3 : 7 and 1 : 1) and chloroform/methanol (3 : 2). The aliquots of each fraction were subjected to thin layer chromatography (TLC) on silica gel coated TLC plate (1 mm Merck) using the solvent system consisting of 20% (v/v) n-hexane/ethyl acetate. The chromatograms were detected using 50% H2SO4 solution as a spray reagent [34]. The individual fractions were collected and concentrated by vacuum rotary evaporator at 40°C. All the purified compounds recovered from the silica gel column were monitored by reading the absorbance at 190–350 nm (UV spectrophotometer, Hitachi, Japan). The active fractions were further purified, and the final yields of the compounds were recorded. The lyophilized pooled concentrated compounds were then assayed (100 μg/mL) against bacteria. The phytochemical screening was done on the pure compounds using the chemical method previously reported for the detection of secondary metabolites [40]. The different chemical constituents tested include alkaloids, flavonoids, glycosides, polyphenols, saponin, sterols, triterpenes, tannins, reducing sugars, gallic acid, catechol, and aglycones.
2.8. Statistical Analysis
The bacterial growth inhibitory activity (inhibition zones millimeter in diameter) was compared for significant differences within the bacterial strains. One way analysis of variance was performed (mean ± SD, n = 3 replicates) using GraphPad Prism 4, USA. *P < 0.01 was considered statistically significant (inhibition zones of extracts/fractions versus antibiotic drugs).
3. Results
3.1. Study Area for the Collection of Aromatic Medicinal Plants
The Western and Eastern Ghats were selected for the present study with the cite map showing the landmarks (Figures 1(a)-1(b)). Kalrayan hills are situated north of Attur taluk (Salem district), one of the major range of hills in the Eastern Ghats of Tamil Nadu (Figure 1(c)). Pachamalai hills are situated to the north of Thuraiyur taluk of Tiruchirappalli district. The rich biodiversity part of Eastern Ghats lies between latitudes 11°09′ 00′′ to 11° 27′ 00′′ N and longitudes 78°28′ 00′′ to 78° 49′ 00′′ E, and occupies an area of about 527.61 square km. It is located near 11° 11′N 78°21E/11.18°N 78.35°E/11.18; 78.35 (Figure 1(d)). Mundanthurai is located nearly 45 km west of Tirunelveli district, TN, between latitude 8° 25′ and 8° 53′ N and longitude 77° 10′ and 77° 35′ E. This is the only area of Western Ghats that has the longest raining period of about 8 months and forms the catchment area for 14 rivers and streams (Figure 1(e)). Kolli Malai is a small mountain range located in Namakkal district. The mountains are about 1000–1300 m in height and cover an area of approximately 280 km. The Kolli hills are part of the Eastern Ghats, which is a mountain range that runs mostly parallel to the east coast of Tamil Nadu in South India (Figure 1(f)). Javadi hills are one of the largest in the Eastern Ghats in Vellore district in the northern part of the state of Tamil Nadu. They consist of bluish gray hills, with peaks averaging 3600–3800 feet or 1100–1150 meter (Figure 1(g)). Based on the vegetation type (Figures 2(a)–2(d)), the study area consists of (i) dry, deciduous, (ii) moist deciduous, and (iii) rain forests and diverse proportion of plant parts in abundance (Figures 2(e)-2(f)). Three different types of tribes (i.e., Kani, Malayali and Paliyan tribes) inhabit in the hill ranges. The Kani tribes, located at Mundanthurai, raise different types of vegetables in their own fields, while the Malayali tribes cultivate rice. They all engage not only in the agricultural work but also are involved in silvicultural work assigned by the forest department, Government of TN, India.
Figure 1.
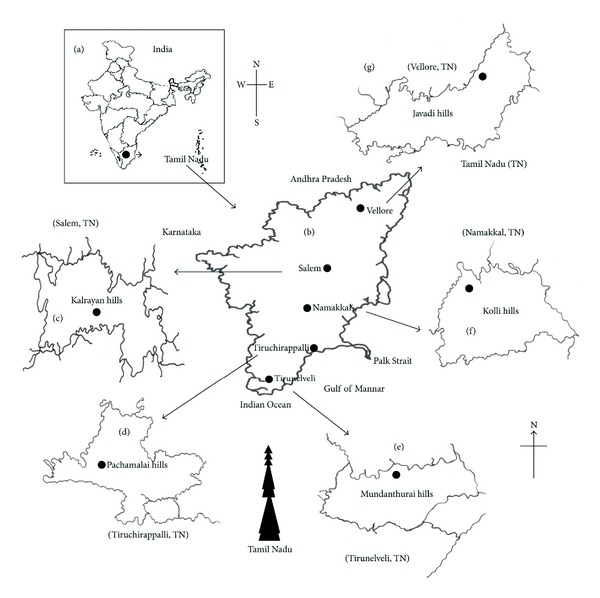
(a) The site for collection of medicinal plants in Western and Eastern Ghats of Tamil Nadu. (b) The landmark (map) of traditional medicine distribution and collection of different types of plants. (c) District map showing the collection site of plants from Kalrayan hills (Salem), (d) Pachamalai hills (Thiruchirappalli), and (e) Mundanthurai (Tirunelveli) rich biodiversity hot-spot of the Western Ghats. (f) Kolli hills (Namakkal), (g) Javadi hills (Vellore), part of the Eastern Ghats, which is a mountain range that runs mostly parallel to the east coast of South India.
Figure 2.
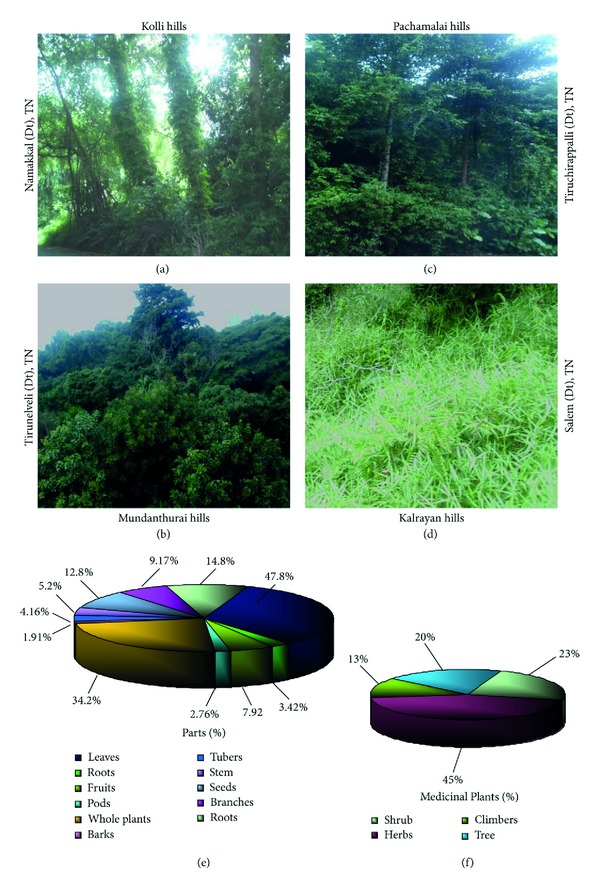
Diverse biodiversity richness of medicinal plants in Western and Eastern Ghats. (a) Topography of plant covering area in Kolli hills (Namakkal district, Tamil Nadu). (b) Aerial view of occurrence of medicinal plants in Mundanthurai hills (Tirunelveli district, TN). (c) Pachamalai hills (Trichy district) and its natural vegetation inhabitants for Malaiyali tribes. (d) Deforestation of natural herbal resources due to urbanization in Kalrayan hills (Salem district) in the Eastern Ghats of TN. (e) Medicinal plants and its various parts used by the natives (traditional healers) for the treatment of diverse human illness with a very high percentage of leaves and whole plants often used for herbal drug preparation by the local practitioners. (f) Various category of plants like shrub, herb, climbers and tree, and the parts used in medicine.
3.2. Medicinal Plants Glory
Western Ghats (Mundanthurai) and Eastern Ghats (Kolli hills, Javadi hills, Kalrayan hills, Pachamalai hills) possess a rich diversity of medicinal plants that are used as food and drug by different groups of tribal communities. Urbanization, habitat degradation, and fragmentation of these forests have resulted in the depletion of natural resources on which these tribes used to depend for their livelihoods. It has become increasingly difficult for them to live in their traditional way. In addition, the impact of modernization and urbanization has encroached in and around tribal settlements, thus changing their lifestyles.
3.3. Plants Valued as Edibles
Various types of plant parts are collected during different seasons, cooked, and eaten along with boiled rice (Table 1). For example, Solanum nigrum leaf is most commonly used in all the four regions. There are a large number of wild edible fruits, including yielding plants such as Citrus acida, Ficus benghalensis, Ficus microcarpa, Ficus racemosa, Phyllanthus emblica, Solanum trilobatum, and Syzygium cumini are popularly used by the tribes.
Table 1.
Some of the important traditional medicinal plant species, families, voucher specimens, parts used, yield of extracts, phytochemical screening, and toxicity on human macrophage cells.
| Scientific name | Family | Voucher specimen | Plant parts | Yield (gm) | Phytochemical analysis |
|---|---|---|---|---|---|
| Adhatoda vasica Nees | Acanthaceae | D2020 | Leaf | 6.4 | Vasicine |
| Aegle marmelos (L.) Correa ex Roxb. | Rutaceae | D2018 | Root-bark | 5.8 | Alkaloids |
| Alangium salvifolium (L.) f. Wangerin. | Alangiaceae | 0140 | Leaf | 6.3 | Phenolic |
| Andrographis paniculata Wallich ex Nees | Acanthaceae | 0061 | Leaf | 6.8 | Andrographolide |
| Andrographis echioides Nees | Acanthaceae | 0116 | Leaf | 7.0 | Terpenoids, |
| Acalypha indica L. | Euphorbiaceae | 29644 | Leaf | 6.1 | Acalyphe |
| Acalypha lanceolata L. | Euphorbiaceae | 15791 | Leaf | 7.1 | Alkaloids |
| Achyranthes aspera L. | Amaranthaceae | 2666 | Leaf | 2.7 | Betaine |
| Ageratum conyzoides L. | Asteraceae | 4812 | Leaf | 3.7 | Essential oils |
| Asteracantha longifolia L. | Acanthaceae | 0234 | Stem | 7.4 | Glycosides |
| Azadirachta indica A. Juss. | Meliaceae | D0204 | Leaf, bark | 6.7 | Tannins |
| Borassus flabellifer L. | Arecaceae | D0202 | Root | 0.8 | Flavonoids, phenolics |
| Boerhavia erecta L. | Nyctaginaceae | 10897 | Whole plant | 2.8 | Phenolics |
| Calotropis procera (Ait.) Ait. f. | Asclepiadaceae | D073 | Root-bark | 1.3 | Terpenoids |
| Calotropis gigantea (L.) R.Br.ex Ait | Asclepiadaceae | D070 | Milky latex | 4.8 | Alkaloids |
| Cassia auriculata L. | Caesalpiniaceae | 0141 | Leaf | 4.9 | Saponins |
| Cassia occidentalis L. | Caesalpiniaceae | 0111 | Root | 9.5 | Flavonoids, saponins |
| Cassia tora L. | Caesalpiniaceae | 0100 | Stem, bark | 6.9 | Saponins |
| Cassia fistula L. | Caesalpiniaceae | 037 | Whole plant | 7.9 | Saponins |
| Cardiospermum halicacabum L. | Sapindaceae | 0125 | Whole plant | 5.8 | Flavonoids |
| Catharanthus roseus (L.) G.Don. | Apocynaceae | 0029 | Leaf, root |
1.4 0.7 |
Alkaloids |
| Cinnamomum zeylanicum Garcin ex Blume | Lauraceae | 00209 | Bark | 3.1 | Essential oil, Tannin |
| Cinnamomum iners Reinw. ex Blume | Lauraceae | 043-c | Leaf, bark | Alkaloids | |
| Cissus quadrangularis Roxb. | Vitaceae | D02023 | Leaf | 6.8 | Glycosides |
| Citrus acida Roxb. Hook.f. | Rutaceae | 0213 | Leaf | 5.2 | Saponins, Terpenoids |
| Centella asiatica (L.) | Umbelliferae | 0138 | Whole plant | 8.9 | Flavonoids, Alkaloids |
| Clerodendrum inerme (L.) Gaertn. | Verbenaceae | D02043 | Stem | 7.8 | Sterols, diterpenes |
| Clitoria ternatea L. | Papilionaceae | D02026 | Seed | 9.8 | Protein |
| Cleistanthus collinus (Roxb.) Benth. and Hook.f. | Euphorbiaceae | 0011 | Whole plant | 0.03 | Cleistanthin, collinusin |
| Cleome gynandropsis L. | Capparidaceae | 12247 | Leaf | 6.2 | Glycosides |
| Cleome viscose L. | Capparidaceae | 29999 | Leaf | 2.7 | Phenolics |
| Coccinia grandis W & A | Cucurbitaceae | D02030 | Leaf, root | 0.9 | Glycosides |
| Cymbopogon citratus (DC.) | Gramineae | D012 | Root | 0.25 | Essential oil |
| Datura metel L. | Solanaceae | D02038 | Leaf, stem | 3.9 | Steroids |
| Eucalyptus globulus Labill. | Myrtaceae | D0220 | Leaf | 1.2 | Terpenoids |
| Eclipta alba (L.) Hassk | Asteraceae | D028 | Whole plant | 0.7 | Phenolic |
| Euphorbia hirta Linn | Euphorbiaceae | 0018-c | Whole plant | 0.12 | — |
| Eclipta prostrata (L.) | Asteraceae | D210 | Leaf | 1.10 | Triterpenoid, saponin |
| Eugenia caryophyllus (Sprengel) Bullock & Harrison | Myrtaceae | 0025 | Flower buds | 1.16 | Essential oils |
| Elettaria cardamomum White et Mason | Zingiberaceae | 0009 | Fruit pods | 3.17 | Essential oils |
| Gloriosa superba L. | Liliaceae | 020-S | Tuber | 1.08 | Alkaloids, phenol |
| Jatropha curcas L. | Euphorbiaceae | 015 | Whole plant | 5.3 | Alkaloids, flavonoids |
| Hyptis suaveolens (L.) Poit. | Lamiaceae | 24688 | Leaf | 6.3 | Essential oil |
| Hemidesmus indicus L. | Asclepiadaceae | D-009 | Roots | Coumarins | |
| Ichnocarpus frutescens (L.) R.Br. | Apocynaceae | 0110 | Root, flower | 7.3 | Terpenoids |
| Leucas aspera (Willd.) Link | Labiatae | 0114 | Leaf | 8.3 | Triterpenes |
| Lawsonia inermis L. | Lythraceae | T261 | Leaf | 0.9 | Glycosides, phenolic |
| Madhuca longifolia (L.) JF Macbr | Sapotaceae | D01415 | Nut | 9.3 | Sitosterol |
| Merremia hastate L. (Desr.) Hallier.f. | Convolvulaceae | 10894 | Whole plant | 4.0 | Alkaloids |
| Mentha piperita L. | Lamiaceae | 0217-c | Whole plant | 0.7 | Essential oils |
| Morinda tinctoria Roxb | Rubiaceae | 0122 | Leaf | 1.4 | Glycosides |
| Mimosa pudica L. | Mimosaceae | 0071 | Whole plant | 0.6 | — |
| Oldenlandia umbellata L. | Rubiaceae | D02047 | Leaf | 4.4 | Alkaloids |
| Ocimum sanctum L. | Lamiaceae | 0016 | Whole plant | 3.0 | Alkaloids |
| Piper attenuatum Buch. Hamex Miq. | Piperaceae | 007 | Flower | 4.6 | Alkaloids |
| Plumbago zeylanica (L.) Cav | Plumbaginaceae | 0121 | Root | 4.8 | Plumbagin |
| Plectranthus amboinicus (L.) Spreng. | Lamiaceae | 0410 | Whole plant | 1.2 | Essential oils, terpenoids |
| Phyllanthus debilis L. (Klein ex Willd) | Euphorbiaceae | 0120 | Whole plant | 4.9 | Polyphenol |
| Phyllanthus madraspatensis L. | Euphorbiaceae | 0117 | Whole plant | 5.0 | Polyphenol |
| Premna tomentosa Willd. | Verbenaceae | 0129 | Leaf | 5.3 | Diterpenes |
| Rosmarinus officinalis L. | Lamiaceae | 0017 | Root | 0.23 | Essential oils |
| Rauwolfia serpentine L. | Apocynaceae | 020-S | Root | 1.15 | Alkaloid |
| Sebastiania chamaelea (L.) Muell Arg. | Euphorbiaceae | 0034 | Leaf | 1.1 | Polyphenol |
| Solanum trilobatum L. | Solanaceae | D02054 | Leaf, flower | 4.0 | Tannins |
| Sphaeranthus indicus L. | Asteraceae | D02060 | Whole plant | 1.0 | Essential oil |
| Swertia chirata (L.) Ham. | Gentianaceae | D0540 | Whole plant | 1.6 | Glycodises |
| Strychnos nux-vomica L. | Loganiaceae | S-22 | Nuts | 0.36 | Alkaloids |
| Tragia involucrata L. | Euphorbiaceae | D068 | Leaves | 1.6 | Shellsol |
| Tinospora cordifolia (Willd.) Miers ex Hoof.f & Thoms | Menispermaceae | 0118 | Leaf, root, stem |
5.0 | Glycosides, tannins |
| Tridax procumbens L. | Compositae | 10649 | Leaf | 1.8 | Flavonoids |
| Terminalia arjuna (DC) W & A | Combretaceae | 033-c | Bark | 8.0 | Phenolics |
| Tephrosia purpurea (L.) Pers | Fabaceae | S-43 | Whole plant | 0.8 | Isoflavone |
| Vitex negundo L. | Verbenaceae | 0031 | Leaf | 2.4 | Terpineol |
| Vetiveria zizanioides L. | Gramineae | 0051 | Root | 1.03 | Essential oil |
| Withania somnifera (L.) Dunal | Solanaceae | D02063 | Root | 2.1 | Alkaloids |
| Wedelia calendulacea Less | Asteraceae | S-24 | Leaves | Flavonoids | |
| Zingiber officinale Rosc. | Zingiberaceae | 0327 | Rhizome | 2.3 | Tannins |
| Zanthoxylum limonella (Dennst.) Alston | Rutaceae | 009 | Bark | 1.9 | Alkaloids, essential oil |
Class of chemical compounds: A: alkaloids, S: saponins, T: tannins, St: steroids, G: glycosides, T: terpenoids, P: polyphenol, P: phenolics, Sh: shellsol, H: hydrocarbon esters.
3.4. Plants Used for Snakebite Treatment
Thirty-four plants used for snakebite treatment are documented (Table 1). Snakebite is a major health hazard that leads to high mortality in tribal settlements. The majority of the antidotes are prepared freshly from plant materials frequently collected from the leaves of A. paniculata, A. echioides, Aristolochia indica, E. alba, E. prostrata, M. pudica, O. sanctum, T. involucrata, and Cleistanthus collinus (Oduvanthalai); the whole plants of Achyranthes aspera and Wedelia calendulacea; the stem-barks and nuts of Strychnos nux-vomica; the roots of Hemidesmus indicus, Tephrosia purpurea, Rauwolfia serpentina, C. roseus, and so forth, and the tubers of Gloriosa superba. The tuber paste is usually applied externally on the site of snakebite, and decoction is given orally for treatment by indigenous people. Besides, these tribes rely on the medicinal plants as ingredients for fabricating a kind of medicated stone for health management. “Vishakallu” (poison stone) is used by the indigenous groups called Kani in Kerala, India, to treat a snakebite. When the stone is placed directly on the bitten area, it sticks to the body to absorb the poison and then become detached when absorption seems to be complete. The ingredients of Vishakallu stones are made with leaves of Ocimum sanctum, Anisomeles malabarica, Leucas aspera, Piper betle, Santalum album, and the pebbles collected from the river bank.
3.5. Survey of Medicinal Plants and Their Health Care Values
The present study is an attempt to provide scientific basis and obtain justification for the traditional beliefs of reliance on a rich diversity of ethnomedicinal plants, along with the rich heritage of traditional medicine practices related to health care system made available by the primitive tribal communities located at different settlements. The native traditional practitioners called “vaidyars” have a good knowledge about the traditional plants locally available for treatment of various diseases (Figures 3(a)–3(p)). Such traditional medical knowledge is used for preparing home remedies, ill health prevention, and routine health maintenance. This knowledge is also applicable to cover other sectors of social life. During the ethnobotanical survey, the wealth of 78 medicinal plant species used by the indigenous tribal community for various types of health treatment was documented. The botanical names, family names, parts used, chemical constituents, and their application are provided (Table 1).
Figure 3.

Medicinal aromatic herbs, spices, and toxic plants were collected from the tribal areas of the Western and Eastern Ghats region in Tamil Nadu, India. (a) A. vasica Nees (leaf), (b) Eclipta alba (L.) Hassk. (whole plant), (c) Mimosa pudica L. (whole plant), (d) P. amboinicus (L.) Spreng. (whole plant), (e) T. procumbens (L.) (whole plant), (f) Euphorbia hirta Linn (whole plant), (g) A. paniculata Wallich ex Nees, (H) C. roseus (L.) G.Don. (whole plant) used for therapy. (i) Cinnamomum iners Reinw. ex Blume (leaf) (j) E. globulus Labill. (leaf and bark), (k) Z. officinale Rosc. (Rhizome), (l) E. caryophyllus (Sprengel) Bullock and Harrison (flower buds), (m) M. piperita L. (whole plant), (n) C. citratus (DC.) Clitoria ternatea L. (whole plant), (o) C. zeylanicum Garcin ex Blume (bark), (p) Elettaria cardamomum White et Mason (fruit pod) used for medicine and food preparation.
3.6. Antimicrobial Activity of Crude Extracts
In this study, we reported the antimicrobial screening of methanolic crude extracts of 78 medicinal plants (Table 2). Results revealed that 68 plant extracts displayed potent activities against one or more Gram-positive and -negative bacteria. Of which, Tragia involucrata, Citrus acida, Aegle marmelos, Adhatoda vasica, Calotropis procera, Andrographis paniculata and Mentha piperita, Azadirachta indica, Sphaeranthus indicus, and Elettaria cardamomum showed the highest antibacterial activity against the multidrug resistant B. pseudomallei (KHW and TES) and S. aureus at 100 μg/mL concentration. The extracts showed pronounced antibacterial activity with their inhibitory zones ranging from 20 to 31 mm in diameter as compared to the standard drugs chloramphenicol and ceftazidime (29–33 mm). The majority of the plants demonstrated a powerful antimicrobial potency against the multidrug resistant strains of B. pseudomallei (KHW and TES), K. pneumonia, and S. aureus. Approximately, twenty-one plant extracts exerted only a weak or moderate effect against the tested bacteria, while the crude extract of 13 plants failed to show any effect at all. Except for the plant extracts of T. involucrata, A. lanceolata, A. vasica, and S. indicus extracts, the majority of the plant extracts were ineffective against the V. damsela infection, fascinatingly, only 11 plants exhibited activity against P. aeruginosa, of which S. indicus, M. piperita, and C. procera were found to have very strong inhibition of bacteria at the tested concentrations. Interestingly, sixteen plants such as Andrographis echioides, C. auriculata, C. viscose, C. gigantea, T. arjuna, Oldenlandia umbellata, Boerhavia erecta, and E. hirta exerted a strong activity against the Gram-positive S. aureus bacteria.
Table 2.
Antimicrobial activity of methanol extract of aromatic medicinal plants and essential oils evaluated against multidrug resistant (MDR) human pathogens at 100 µg/mL concentration.
| Scientific name | Microorganisms; growth inhibition zones (6 millimeter in diameters) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| KHW | TES | K.p | K.pr | P.a | S.a | St.p | S.p | V.d | V.d | |
| Adhatoda vasica Nees | 28 | 19 | 22 | 18 | 12 | — | 10 | 17 | 16 | — |
| Aegle marmelos (L.) Correa ex Roxb. | 29 | 17 | 9 | 10 | — | 15 | — | — | — | — |
| Alangium salvifolium (L.) f. Wangerin. | 15 | 10 | 8 | 8 | — | 12 | 9 | 10 | — | — |
| Andrographis echioides L. | 12 | 9 | — | — | — | 17 | 8 | 9 | — | — |
| Andrographis paniculata Wallich ex Nees | 26 | 21 | 19 | 13 | — | 25 | 8 | 16 | 12 | — |
| Acalypha indica L. | — | — | — | — | — | 18 | — | — | — | — |
| Acalypha lanceolata L. | — | — | 12 | 13 | — | 10 | — | — | 21 | — |
| Achyranthes aspera L. | — | — | 7 | 14 | — | 15 | 12 | 11 | — | — |
| Ageratum conyzoides L. | 10 | 8 | — | — | — | — | — | — | — | — |
| Asteracantha longifolia L. | 16 | 12 | — | — | — | 15 | — | — | — | — |
| Azadirachta indica A. Juss. | 15 | 17 | 21 | 16 | 14 | 23 | 12 | 14 | — | — |
| Borassus flabellifer L. | 9 | 10 | 17 | 8 | — | — | 9 | 10 | — | — |
| Boerhavia erecta L. | — | — | 8 | 9 | 7 | 16 | — | — | — | — |
| Calotropis procera (L.) | — | — | 15 | — | 18 | 28 | 9 | — | — | — |
| Calotropis gigantea (L.) R.Br.ex Ait | 11 | 9 | — | — | — | 20 | — | — | 9 | 8 |
| Cardiospermum halicacabum L. | 23 | — | — | 14 | — | 9 | 19 | — | — | — |
| Catharanthus roseus (L.) G.Don. | 13 | 7 | 12 | 9 | — | 15 | 11 | 8 | — | — |
| Cassia auriculata L. | 17 | 13 | 12 | — | — | 19 | 13 | — | — | — |
| Cassia occidentalis L. | 18 | — | — | — | — | — | — | — | — | — |
| Cassia tora L. | — | — | — | — | — | — | — | — | — | — |
| Cassia fistula L. | — | — | — | — | — | — | — | — | — | — |
| Citrus acida Roxb. Hook.f. | 26 | 22 | — | 12 | 29 | 9 | 13 | 8 | — | |
| Cissus quadrangularis L. | — | — | — | — | — | — | — | — | — | — |
| Cinnamomum zeylanicum Garcin ex Blume | 14 | 16 | 7 | 20 | — | 22 | 19 | 7 | — | — |
| Cinnamomum iners Reinw. ex Blume | 20 | 16 | — | 15 | — | 16 | 12 | — | — | — |
| Rosmarinus officinalis L. | — | 9 | — | 10 | — | 7 | — | 8 | — | — |
| Centella asiatica (L.) | 9 | 8 | — | — | — | 11 | — | — | — | — |
| Clerodendrum inerme (L.) Gaertn. | 13 | 7 | 12 | — | — | 15 | 11 | 8 | — | — |
| Clitoria ternatea L. | — | — | — | — | — | — | — | — | — | — |
| Clitoria ternatea L. | 16 | 12 | — | 13 | — | 8 | 10 | — | — | — |
| Cleome gynandropsis L. | — | — | 12 | 19 | 11 | — | 9 | 15 | 12 | — |
| Cleome viscose L. | — | — | 8 | 10 | 14 | 20 | — | — | — | — |
| Coccinia grandis W & A | 9 | 10 | 17 | 8 | — | — | 9 | 10 | — | — |
| Cymbopogon citratus (DC.) | 16 | 18 | — | 17 | — | 14 | — | — | — | — |
| Datura metel L. | — | — | — | — | — | — | — | — | — | — |
| Eclipta alba (L.) Hassk | 20 | — | — | 9 | — | — | 10 | — | — | — |
| Euphorbia hirta Linn | 11 | — | — | — | — | 16 | — | — | — | — |
| Eucalyptus globulus Labill. | — | — | — | 7 | — | — | — | 7 | — | — |
| Eugenia caryophyllus Bullock & Harrison | — | 7 | — | 11 | — | 9 | — | 8 | — | — |
| Elettaria cardamomum White et Mason | 21 | 20 | 7 | 14 | — | 22 | 12 | 17 | — | — |
| Hyptis suaveolens (L.) Poit. | 8 | 10 | 8 | 7 | — | — | — | — | — | — |
| Ichnocarpus frutescens (L.) W.J. Aiton | — | — | — | — | — | — | — | — | — | — |
| Jatropha curcas L. | — | — | — | 8 | — | 11 | — | 12 | — | 7 |
| Leucas aspera (Willd.) Link | 9 | 10 | 17 | 8 | — | 12 | 9 | 10 | — | — |
| Lawsonia inermis L. | — | — | — | — | — | — | — | — | — | — |
| Madhuca longifolia (L.) JF Macbr | 18 | 16 | 14 | 19 | 12 | — | 8 | 7 | 9 | — |
| Merremia hastate L. (Desr.) Hallier.f. | — | — | — | — | — | — | — | — | — | — |
| Morinda tinctoria Roxb | — | — | — | — | — | — | — | — | — | — |
| Mentha piperita L. | 23 | 17 | 26 | 12 | 20 | 25 | 19 | — | — | — |
| Ocimum sanctum L. | 12 | 9 | 11 | 7 | — | 15 | 7 | 8 | — | — |
| Oldenlandia umbellata L. | — | — | — | — | — | 17 | — | — | — | — |
| Piper attenuatum Buch. Hamex Miq. | 13 | 7 | 12 | 21 | — | 17 | 11 | 8 | — | — |
| Plumbago zeylanica (L.) Cav | 9 | 10 | 17 | 8 | — | 12 | 9 | 10 | — | — |
| Plectranthus amboinicus (L.) Spreng. | — | — | — | 8 | 11 | 15 | — | — | — | — |
| Phyllanthus debilis L. (Klein ex Willd) | 7 | 8 | — | 9 | — | 9 | 18 | 7 | — | — |
| Phyllanthus maderaspatensis L. | 17 | — | — | — | — | — | — | — | — | — |
| Premna tomentosa Willd. | 13 | 10 | — | 15 | — | 9 | 10 | — | — | — |
| Gloriosa superba L. | 17 | 16 | 7 | 8 | — | 15 | — | — | — | 8 |
| Sebastiania chamaelea (L.) Muell Arg. | 19 | 12 | — | 17 | — | 13 | 19 | 8 | — | — |
| Solanum trilobatum L. | — | — | 13 | 9 | — | 8 | — | — | — | — |
| Sphaeranthus indicus L. | 20 | 18 | 21 | 7 | 22 | — | 11 | 9 | — | 16 |
| Swertia chirata (L.) Ham. | — | — | — | — | — | — | — | — | — | — |
| Terminalia arjuna (W. & A) | — | — | — | — | — | 16 | — | — | — | — |
| Tinospora cordifolia (Willd.) Miers ex Hoof.f & Thoms | — | — | 23 | 16 | — | 12 | 15 | — | — | — |
| Tridax procumbens L. | 9 | 8 | 7 | — | — | 14 | — | — | — | — |
| Tragia involucrata L. | 25 | 23 | 20 | — | — | 31 | 28 | 22 | 19 | — |
| Vitex negundo L. | — | — | — | — | — | 14 | — | — | — | — |
| Vetiveria zizanioides (L.) | 11 | 9 | 7 | 7 | — | 16 | — | — | 8 | |
| Withania somnifera (L.) Dunal | 12 | 20 | — | — | — | 15 | 12 | — | — | — |
| Zingiber officinale Rosc. | 14 | 11 | 7 | 15 | — | 7 | 12 | 7 | — | — |
| Zanthoxylum limonella (Dennst.) Alston | 13 | 7 | 12 | 9 | — | — | 11 | 8 | — | — |
| Chloramphenicol (30 µg/disc) | 21 | 12 | 15 | 17 | 29 | 16 | 15 | 18 | 13 | 11 |
| Ceftazidime (30 µg/disc) | 33 | 16 | 22 | 19 | 16 | 25 | 21 | 20 | 12 | 15 |
*Bacteria (+/−). Results obtained in the disc diffusion assay; antibacterial activity is expressed as the mean ± SD (n = 3), of the inhibition by the extract and its diameter around the discs. One way analysis of variance was performed (mean ± SD, n = 3 replicates). Size of inhibition zones were including the sterile blank discs 6 millimeter (mm) in diameters. Absence of bacterial inhibition indicates (—), antibiotic disc (30 µg/disc).
3.7. Phytochemical Screening of Plants
The results obtained from the phytochemical screening as shown in Table 1 indicate the presence of various types of secondary metabolites such as polyphenols, tannins, saponins, alkaloids, and glycosides/polysaccharides. Most of the plant extracts relatively rich in alkaloids, phenols, flavonoids, polyphenols, tannins, sterols, and terpenoids were found to inhibit the growth of organisms.
3.8. Antimicrobial Activity of Fractioned Compounds
Active components were purified from the most active extracts for further testing. The compound shellsol of T. involucrata and C. acida exhibited the most potent action against the antibiotic resistant strains of B. pseudomallei (KHW), S. aureus, B. pseudomallei (TES), and K. pneumoniae. A. marmelos was also found to inhibit the growth of B. pseudomallei (KHW) more effectively than other tested bacteria. A. vasica showed the broad spectrum growth inhibitory activity on B. pseudomallei (KHW), K. pneumoniae, K. pneumoniae, resistant B. pseudomallei (TES), S. pyogenes, and V. damsela. However, E. cardamomum displayed antimicrobial activity on some of the B. pseudomallei (KHW), S. pyogenes, B. pseudomallei (TES), and S. typhi strains. Similarly, A. indica exerted the growth inhibition on K. pneumoniae and S. aureus. Remarkably, Sebastiania chamaelea was more active against K. pneumoniae, K. pneumoniae, and S. pyogenes. The compound from S. indicus inhibited the growth of K. pneumoniae, K. pneumoniae, B. pseudomallei (KHW and TES), and S. typhi strains, as compared to the activity shown by the crude extracts (Figure 4). The antimicrobial efficacy of fractions collected from the oil yielding plants was also compared with that of the tested compounds. C. zeylanicum and R. officinalis were the most sensitive in controlling the growth of B. pseudomallei (KHW), S. aureus, K. pneumonia, and S. pneumoniae. Fascinatingly, all the compounds obtained from aromatic plants, except those from E. globules, were found to be very effective against the multidrug resistant human pathogen B. pseudomallei (KHW) that causes melioidosis. On the other hand, compounds from C citrates, O. sanctum, E. caryophyllus, and Z. zizanioide, showed some promising effect only against S. aureus (Figure 5). The activity of the compounds were pronounced more than that of the oil yielding plant fractions.
Figure 4.
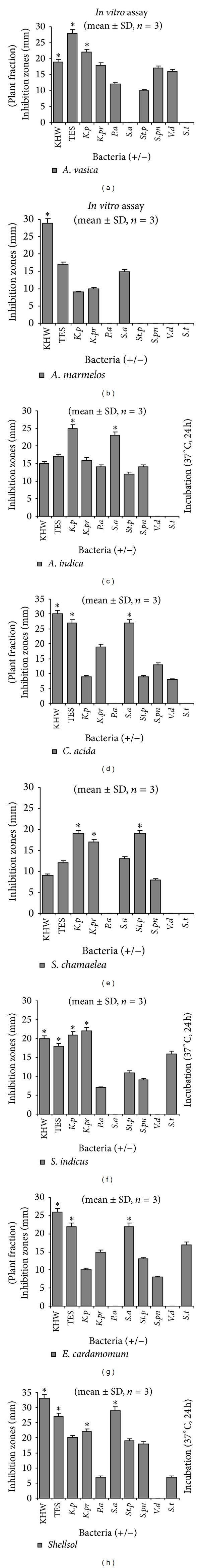
In vitro antimicrobial activity of purified fractions from the most active plant extracts tested against bacteria. Growth inhibition zones were measured and analyzed with mean ± standard deviation (SD), (n = 3) using one way analysis of variance. Level of significance at (*P > 0.01). Most of the fractions exerted a potent inhibitory effect against multidrug resistant Gram-negative bacteria (B. pseudomallei strains KHW and TES), K. pneumonia, and Gram-positive bacteria S. aureus.
Figure 5.
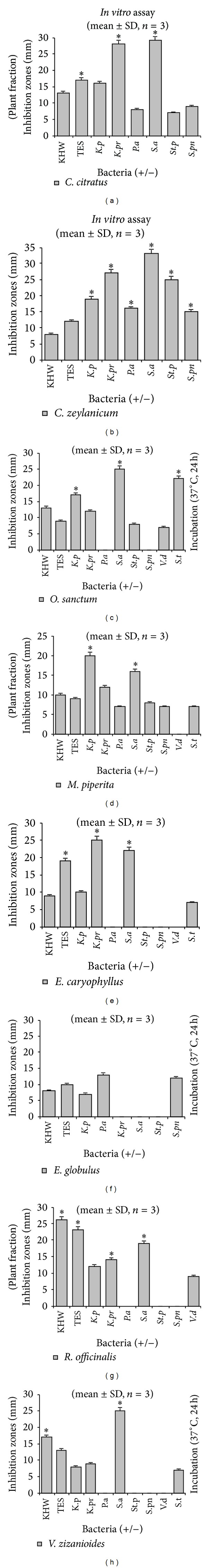
Comparison of antimicrobial effect of plant compounds obtained from the most popularly used sources of essential oils as assayed by the disc-diffusion method in vitro. It displayed a powerful activity against B. pseudomallei and S. aureus than the other bacteria strains. Other compounds showed only a moderate or weak action against the tested bacteria. Values for zone of bacterial growth inhibition were presented as mean ± SD, (n = 3) with level of significance at (*P > 0.01).
3.9. Minimum Inhibitory Concentrations (MICs)
The antibiotic potential of the purified fractions was obtained from the MIC determination. The hydrocarbon ester shellsol (T. involucrata) and C. acida showed an interesting inhibitory potential against S. aureus (MIC of 7.8 μg/mL) and B. pseudomallei strain of KHW (MIC of 15.6 μg/mL). A. vasica showed an MIC of 15.6 μg/mL against B. pseudomallei (KHW) and an MIC of 31.25 μg/mL against K. pneumoniae, K. pneumoniae, S. pyogenes, and V. damsela strains. Fractions from A. marmelos and terpenoid from A. indica exerted bacteriostatic effect with MIC values of 31.25 μg/mL on some selected bacteria including B. pseudomallei of KHW, S. aureus, and B. pseudomallei of TES. The MIC of 31.25 μg/mL was found for E. cardamomum against S. aureus, K. pneumonia, and S. pyogenes. S. indicus displayed a very strong inhibition against MDR K. pneumoniae (MIC of 15.6 μg/mL), and against B. pseudomallei (KHW and TES) at MIC of 31.25 μg/mL. When the antimicrobial efficacies of purified fractions from aromatic plants were compared, the C. zeylanicum fraction displayed an important antimicrobial effect against S. aureus (MIC of 7.8 μg/mL), MDR B. pseudomallei of KHW (MIC of 15.6 μg/mL), and S. pneumoniae (MIC of 31.25 μg/mL). The essential oil from M. piperatea showed MIC value of 31.25 μg/mL against K. pneumoniae, S. aureus, and B. pseudomallei (KHW), respectively. O. sanctum and C. citratus fractions also showed antimicrobial activity (MICs of 31.25–125 μg/mL) only at higher concentrations against the tested bacteria. In addition to that, higher concentrations (>250 μg/mL) (of Vetiveria fractions) were required to inhibit Vibro species, and others (including E. globulus fractions) failed to show any effect at tested concentrations (7.8–125 μg/mL). However, the purified fractions (from most active medicinal plants) showed strong bacteriostatic inhibition against the tested organisms (Table 3).
Table 3.
Minimum inhibitory concentrations (MICs) of purified plant fractions and essential oils against antibiotic resistant bacteria.
| Botanical name | Family | Parts used | Gram-positive and -negative bacteria (MICs µg/mL) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| KHW | TES | K.p | K.Pr | S.a | St.p | S.p | V.d | S.t | |||
| A. indica Juss. | Meliaceae | Seed (fraction) | 31.25 | 62.5 | 125 | <250 | 31.25 | — | — | — | — |
| A. marmelos (L.) | Rutaceae | Root-bark (F) | 31.25 | 31.25 | — | — | 31.25 | 62.5 | 125 | 250 | — |
| A. paniculata Nees | Acanthaceae | Leaf (fraction) | 250 | — | 125 | — | 62.5 | — | — | 125 | — |
| A. vasica Nees | Acanthaceae | Fraction (Stem) | 15.6 | 31.25 | 31.25 | 62.5 | — | <250 | 31.25 | 31.25 | — |
| C. acida Roxb. | Rutaceae | Leaf (fraction) | 15.6 | 62.5 | — | — | 7.8 | — | 31.25 | — | — |
| E. cardamomum White et Mason | Acanthaceae | Fraction (WP) | 62.5 | — | 31.25 | — | 31.25 | 250 | 62.5 | — | — |
| S. indicus (L.) | Euphorbiaceae | Whole plant (F) | 31.25 | 125 | 15.6 | — | 62.5 | — | — | <250 | — |
| T. involucrata (L.) | Euphorbiaceae | Shellosol (leaf) | 15.6 | 31.25 | — | — | 7.8 | 62.5 | — | — | — |
| Cinnamomum zeylanicum (L.) | Lauraceae | Bark (fraction) | 15.6 | 62.5 | — | — | 7.8 | 31.25 | — | — | 125 |
| Cymbopogon citratus (L.) | Graminae | Leaf (fraction) | 250 | <250 | 62.5 | — | 62.5 | 125 | — | — | — |
| Eugenia caryophyllus (L.) | Myrtaceae | Flower buds (F) | 62.5 | 125 | — | — | 62.5 | — | — | — | — |
| Eucalyptus globulus (L.) | Myrtaceae | Fraction (leaf) | — | — | — | — | — | — | <250 | — | <250 |
| Mentha piperita (L.) | Labiatae | Fraction (WP) | — | 62.5 | 31.25 | — | 31.25 | — | <250 | — | — |
| Ocimum sanctum (L.) | Labiatae | Leaf (fraction) | 62.5 | 125 | — | 31.25 | 62.5 | — | 125 | <250 | — |
| Rosmarinus officinalis (L.) | Labiatae | Rosemary oil | 31.25 | — | — | — | 31.25 | — | — | — | — |
| Vetiveria zizanioides (L.) | Graminae | Root (fraction) | — | 125 | 125 | — | — | — | >250 | >250 | |
The bacterial growth inhibitory activity was compared for significant differences within the bacterial strains by broth-dilution method at 250, 125, 62.5, 31.25, 15.6, and 7.8 µg/mL. F: fractions.
3.10. Cytotoxic Effects of Plants
When the components were assayed for cytotoxicity against the normal human skin fibroblasts (HEPK) cells, the compounds obtained from E. cardamomum, T. involucrata, S. indicus, C. acida, A. vasica, A. marmelos, A. indica, and A. paniculata did not show toxicity up to 1000 μg/mL (see Figures S1 and S2 in Supplementary Material available online at http://dx.doi.org/10.1155/2013/525613). A slight reduction of cell proliferation was noted only at higher doses (2000 μg/mL). In contrast, cell proliferation was markedly reduced after exposure of HEPK cells to O. sanctum, E. globulus, V. zizanioides, C. citratus, and E. globulus compounds. There was no gradual reduction in skin cell proliferation seen after exposure to C. zeylanicum, R. officinalis, and M. piperita (see Figures S3 and S4) compounds. The toxicity was found to be concentration-dependent when the skin fibroblasts (HEPK) cells were exposed to various compounds. The cell proliferation was increased by the influence of the plant components at the lower concentrations. Whereas the oil yielding plant compounds showed inhibition of cell proliferation and toxicity at higher doses 250–1000 μg/mL.
4. Discussion
The Western Ghats is considered as one of the richest biodiversity hotspots in the world [41]. In this survey, we collected nearly 78 medicinal plants from Western and Eastern Ghats that are edible and popularly used for curing various ailments including snakebite. Traditional remedies have a long-standing history in many tribal settlements in TN, India, and they continue to provide useful and applicable tools for treating ailments [42]. The ingredients that make up the “Vishakallu” stone, which is used as an antidote for snakebite, are different herbs and pebbles available from the river banks. Likewise, aqueous paste and decoction obtained from the leaves of A. paniculata are widely used for snakebite treatment by indigenous people [43]. Previous studies have reported that ethnomedicine plays major roles in conserving the disappearing knowledge of tribal communities [44–47]. The traditional beliefs of reliance on a rich diversity of ethnomedicinal plants located at different settlements have also been confirmed in another study [48, 49]. Herein, we explored the various types of traditional practices reported by the primitive tribal communities with a view to gain further knowledge from such studies.
In the present investigation, potentially rich sources of tribal medicine (71 plants) were scientifically evaluated for their antibacterial activity against the MDR bacteria, and the accumulated data was disseminated for the first time to the scientific community. Out of the 71 medicinal plants screened for the antibacterial activity, 10 of them (T. involucrata, C. acida, A. marmelos, A. vasica, C. procera, A. paniculata and M. piperita, A. indica, S. indicus, and E. cardamomum) displayed the highest antibacterial activity against the multidrug resistant B. pseudomallei (KHW and TES) and S. aureus strains. The antibacterial activity of those crude plant extracts was as equally effective as that of the standard drugs. Our findings corroborated with the previous reports made on the antistaphylococcal activity of tribal medicinal plants [34, 50, 51]. On the other hand, isolated components from the most active extracts of T. involucrata, shellsol, and C. acida exhibited the most potent action against the antibiotic resistant B. pseudomallei (KHW), K. pneumoniae, and S. aureus strains. These results further confirmed our previous findings on the leaves of T. involucrata and its compounds hydrocarbon ester-like shellsol, which displayed a high antibacterial effect against the different bacterial strains, especially that of S. aureus [34]. Eugenol and caryophyllene are the active agents contained in the M. piperita [52] and O. sanctum plants, which are believed to be mainly responsible for the antimicrobial properties of these plants [53]. Interestingly, the compounds obtained from the aromatic plants such as C. zeylanicum and R. officinalis were also found to be very effective against the multidrug resistant human pathogen K. pneumoniae, S. aureus, S. typhi, and B. pseudomallei (KHW) that causes melioidosis.
The inhibitory potential determined for the shellsol (T. involucrata), vaseline (A. vasica), C. acida, and C. zeylanicum indicates that the MIC of 7.8–31.25 μg/mL found against the B. pseudomallei of KHW, K. pneumoniae, K. pneumoniae, S. pyogenes, and V. damsel, and S. pneumoniae was quite low. Similarly, lower MIC values were found for M. piperita (MIC of 1.13–2.25 mg/mL) against the above bacterial strains [52]. MIC was found for the most active alcohol extracts of A. salvifolium (MIC 0.034–0.263 mg/mL) on S. aureus [54], and the MIC for S. trilobatum aqueous extracts determined against the tested organisms ranged from 0.06 to 0.5 mg/mL [55]. C. zeylanicum was found to have an effective antibacterial activity (MIC 64 μg/mL) against P. aeruginosa, E. coli, B. subtilis, and S. aureus [56]. Previously, several investigators have demonstrated that active agents exert interesting activity against bacteria even at lower concentrations tested [57, 58]. The bacteriostatic mechanism involves damage to the cell walls of bacteria, followed by inhibition of protein synthesis that ultimately leads to bacterial death [59]. The most active plants are widely used by various tribes as traditional treatment (i.e., cut wounds, skin infection, and scabies), thus indicating the potential for further development into promising drugs. In order to ascertain the safety and efficacy of the most active compounds, their effect on human skin fibroblast cells was evaluated. Chemical constituents of E. cardamomum, T. involucrata, S. indicus, C. acida, A. vasica, A. marmelos, A. indica, and A. paniculata plants failed to produce any noticeable toxicity up to 1000 μg/mL. Although some of the tested compounds exhibited a slight reduction of cell proliferation and some minor morphological changes, such changes were insignificant at lower doses and became evident only at higher doses. However, certain aromatic compounds of O. sanctum, E. globulus, V. zizanioides, C. citratus, and E. globulus plants showed reduction of cell proliferation against HEPK cells.
Our phytochemical screening also provides evidence of the presence of several types of compounds that are mainly responsible for the remarkable antibacterial effect of these plants. The differences noted for the bactericidal activity of various plant extracts in this study appears to be directly related to the diversity of compounds (shown in parentheses) that are accumulated in the following plants (e.g., A. marmelos and O. umbellate) [60–62]. Compounds like tannins, phenol, and polyphenols can bind the Gram-negative bacteria to form a heavy soluble complex on the cell surface, which subsequently disturbs the availability of receptor on cells and kills the bacteria [63]. Several species having wide spectra of antimicrobial activity mainly due to the active constituents such as essential oil, phenolic compounds like thymol, carvacrol in oregano and thyme, eugenol in clove, and cinnamon were also identified previously [64, 65]. Essential oils degrade the cell wall, interact with the cell components, and then disrupt the cytoplasmic membrane [66]. The antimicrobial effect of phenolic compounds may involve multiple modes of action, including damage to the membrane protein, interference with membrane integrated enzymes [67], causing leakage of cellular components, coagulation of cytoplasm, depletion of the proton motive force, alteration of fatty acid and phospholipid constituents, impairment of enzymatic mechanisms for production and metabolism, alteration of nutrient uptake and electron transport [68], influencing the synthesis of DNA and RNA, and destroying protein translation and the function of the mitochondrion in eukaryotes [69]. The mode of action of antimicrobial agents depends on the type of microorganism and is mainly related to their cell wall structure and the outer membrane arrangement. Most of the plant spices and herbs contain complex phenolics (i.e., phenolic acids, flavonoids, tannins, lignans, coumarins, quinines). In addition, the mechanisms of action of each phenolic compound against various bacteria are also very complicated [26, 70]. Further investigation is therefore required to understand the relationship between the antimicrobial action and the chemical structure of every phenolic compound in the tested extracts. The information available from previous pharmacological sources combined with the findings herein reported on the medicinal plant extracts may serve as essential data for future drug development to combat diseases caused by the MDR bacterial strains.
Supplementary Material
Evaluating herbal drugs in vitro could be a valuable tool for screening antibiotic potential of plants. To develop new strategy for improvement for the assessment of their pharmacological, toxicological profile, scientific evidence based approaches are being employed to appropriately evaluate composition, quality, potential medicinal activity and safety of these natural products.
Acknowledgments
The authors are thankful to the ERI, Loyola College, Chennai, India, for his support during the survey. The authors also thank the Department of Microbiology, NUHS, NUS for the bacterial cultures used in this investigation. The authors are thankful to the tribal people for sharing their healing knowledge on medicinal aromatic plants.
Abbreviations
- MDR:
Multidrug resistant bacteria
- TES:
Strain of Burkholderia pseudomallei
- MRSA:
Methicillin-resistant Staphylococcus aureus
- VRE:
Vancomycin-resistant enterococci
- MTB:
Mycobacterium tuberculosis
- CH3OH:
Methanol
- CFU:
Colony forming unit
- HCl:
Hydrochloric acid
- TLC:
Thin layer chromatography
- H2SO4:
Sulphuric acids
- UV:
Ultraviolet spectrophotometer
- HEPK:
Human skin fibroblasts.
References
- 1.Alekshun MN, Levy SB. Molecular mechanisms of antibacterial multidrug resistance. Cell. 2007;128(6):1037–1050. doi: 10.1016/j.cell.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 2.Russell AD. Antibiotic and biocide resistance in bacteria: introduction. Symposium Series Society for Applied Microbiology. 2002;31(92):1S–3S. [PubMed] [Google Scholar]
- 3.Guay DR. Treatment of bacterial skin and skin structure infections. Expert Opinion on Pharmacotherapy. 2003;4(8):1259–1275. doi: 10.1517/14656566.4.8.1259. [DOI] [PubMed] [Google Scholar]
- 4.Brosnahan AJ, Schlievert PM. Gram-positive bacterial superantigen outside-in signaling causes toxic shock syndrome. FEBS Journal. 2011;278(23):4649–4667. doi: 10.1111/j.1742-4658.2011.08151.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fellermann K, Wehkamp J, Herrlinger KR, Stange EF. Crohn’s disease: a defensin deficiency syndrome? European Journal of Gastroenterology and Hepatology. 2003;15(6):627–634. doi: 10.1097/00042737-200306000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Chen L, Lin S, Agha-Majzoub R, Overbergh L, Mathieu C, Chan LS. CCL27 is a critical factor for the development of atopic dermatitis in the keratin-14 IL-4 transgenic mouse model. International Immunology. 2006;18(8):1233–1242. doi: 10.1093/intimm/dxl054. [DOI] [PubMed] [Google Scholar]
- 7.Song JH, Thamlikitkul V, Hsueh PR. Clinical and economic burden of community-acquired pneumonia amongst adults in the Asia-Pacific region. International Journal of Antimicrobial Agents. 2011;38(2):108–117. doi: 10.1016/j.ijantimicag.2011.02.017. [DOI] [PubMed] [Google Scholar]
- 8.Dance DAB. Melioidosis. Current Opinion in Infectious Diseases. 2002;15(2):127–132. doi: 10.1097/00001432-200204000-00005. [DOI] [PubMed] [Google Scholar]
- 9.White NJ. Melioidosis. The Lancet. 2003;361(9370):1715–1722. doi: 10.1016/s0140-6736(03)13374-0. [DOI] [PubMed] [Google Scholar]
- 10.Yang S. Melioidosis research in China. Acta Tropica. 2000;77(2):157–165. doi: 10.1016/s0001-706x(00)00139-x. [DOI] [PubMed] [Google Scholar]
- 11.Hsueh PR, Teng LJ, Lee LN, et al. Melioidosis: an emerging infection in Taiwan? Emerging Infectious Diseases. 2001;7(3):428–433. doi: 10.3201/eid0703.010310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Walsh C, Fanning S. Antimicrobial resistance in food-borne pathogens—a cause for concern? Current Drug Targets. 2008;9(9):808–815. doi: 10.2174/138945008785747761. [DOI] [PubMed] [Google Scholar]
- 13.Vorachit M, Chongtrakool P, Arkomsean S, Boonsong S. Antimicrobial resistance in Burkholderia pseudomallei . Acta Tropica. 2000;74(2-3):139–144. doi: 10.1016/s0001-706x(99)00063-7. [DOI] [PubMed] [Google Scholar]
- 14.Thibault FM, Hernandez E, Vidal DR, Girardet M, Cavallo JD. Antibiotic susceptibility of 65 isolates of Burkholderia pseudomallei and Burkholderia mallei to 35 antimicrobial agents. Journal of Antimicrobial Chemotherapy. 2004;54(6):1134–1138. doi: 10.1093/jac/dkh471. [DOI] [PubMed] [Google Scholar]
- 15.Sikarwar RLS. Ethnogynaecological uses of plants new to India. Ethnobotany. 2002;12(1-2):112–115. [Google Scholar]
- 16.Siva R. Status of natural dyes and dye-yielding plants in India. Current Science. 2007;92(7):916–925. [Google Scholar]
- 17.Kumar Singh P, Kumar V, Tiwari RK, Sharma A, Rao ChV, Singh RH. Medico-ethnobotany of ‘chatara’ block of district sonebhadra, Uttar Pradesh, India. Advances in Biological Research. 2010;4(1):65–80. [Google Scholar]
- 18.Lewis WH, Elwin-Lewis MP. Medical Botany: Plants Affecting Human Health. New York, NY, USA: John Wiley & Sons; 2003. [Google Scholar]
- 19.Perumal Samy R, Pushparaj PN, Gopalakrishnakone P. A compilation of bioactive compounds from Ayurveda. Bioinformation. 2008;3(3):100–110. doi: 10.6026/97320630003100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.World Health Organization (WHO) Traditional Medicine Strategy 2002–2005. Geneva, Switzerland: Genera: World Health Organization; 2002. [Google Scholar]
- 21.Haddad PS, Azar GA, Groom S, Boivin M. Natural health products, modulation of immune function and prevention of chronic diseases. Evidence Based Complementary and Alternative Medicine. 2005;2(4):513–520. doi: 10.1093/ecam/neh125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Poonam K, Singh GS. Ethnobotanical study of medicinal plants used by the Taungya community in Terai Arc Landscape, India. Journal of Ethnopharmacology. 2009;123(1):167–176. doi: 10.1016/j.jep.2009.02.037. [DOI] [PubMed] [Google Scholar]
- 23.Mahady GB. Medicinal plants for the prevention and treatment of bacterial infections. Current Pharmaceutical Design. 2005;11(19):2405–2427. doi: 10.2174/1381612054367481. [DOI] [PubMed] [Google Scholar]
- 24.Kumar VP, Chauhan NS, Padh H, Rajani M. Search for antibacterial and antifungal agents from selected Indian medicinal plants. Journal of Ethnopharmacology. 2006;107(2):182–188. doi: 10.1016/j.jep.2006.03.013. [DOI] [PubMed] [Google Scholar]
- 25.Nair R, Kalariya T, Chanda S. Antibacterial activity of some plant extracts used in folk medicine. Journal of Herbal Pharmacotherapy. 2007;7(3-4):191–201. doi: 10.1080/15228940802152836. [DOI] [PubMed] [Google Scholar]
- 26.Kalemba D, Kunicka A. Antibacterial and antifungal properties of essential oils. Current Medicinal Chemistry. 2003;10(10):813–829. doi: 10.2174/0929867033457719. [DOI] [PubMed] [Google Scholar]
- 27.Ashour AH. Antibacterial, antifungal, and anticancer activities of volatile oils and extracts from stems, leaves, and flowers of Eucalyptus sideroxylon and Eucalyptus torquata . Cancer Biology and Therapy. 2008;7(3):399–403. doi: 10.4161/cbt.7.3.5367. [DOI] [PubMed] [Google Scholar]
- 28.Abad MJ, Bedoya LM, Apaza L, Bermejo P. The Artemisia L. genus: a review of bioactive essential oils. Molecules. 2012;17(3):2542–2566. doi: 10.3390/molecules17032542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Marzoug HN, Romdhane M, Lebrihi A, et al. Eucalyptus oleosa essential oils: chemical composition and antimicrobial and antioxidant activities of the oils from different plant parts (stems, leaves, flowers and fruits) Molecules. 2011;16(2):1695–1709. doi: 10.3390/molecules16021695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Proestos C, Sereli D, Komaitis M. Determination of phenolic compounds in aromatic plants by RP-HPLC and GC-MS. Food Chemistry. 2006;95(1):44–52. [Google Scholar]
- 31.Chao S, Young G, Oberg C, Nakaoka K. Inhibition of methicillin-resistant Staphylococcus aureus (MRSA) by essential oils. Flavour and Fragrance Journal. 2008;23(6):444–449. [Google Scholar]
- 32.Akin M, Oguz D, Saracoglu HT. Antibacterial effects of some plant extracts from Labiatae (Lamiaceae) growing naturally around Sirnak-Silopi, Turkey. International Journal of Pharmaceutical and Applied Sciences. 2010;1(1):4–47. [Google Scholar]
- 33.Bayoub K, Baibai T, Mountassif D, Retmane A, Soukri A. Antibacterial activities of the crude ethanol extracts of medicinal plants against Listeria monocytogenes and some other pathogenic strains. African Journal of Biotechnology. 2010;9(27):4251–4258. [Google Scholar]
- 34.Samy RP, Gopalakrishnakone P, Sarumathi M, Houghton P, Ignacimuthu S. Purification of antibacterial agents from Tragia involucrata—a popular tribal medicine for wound healing. Journal of Ethnopharmacology. 2006;107(1):99–106. doi: 10.1016/j.jep.2006.02.020. [DOI] [PubMed] [Google Scholar]
- 35.Matthew KM. The Flora of Tamil Nadu Carnatic. Madras, India: Part I–III printed at the Diocesan Press; 1981–1983. [Google Scholar]
- 36.Bauer AW, Kirby WM, Sherris JC, Turck M. Antibiotic susceptibility testing by a standardized single disk method. American Journal of Clinical Pathology. 1966;45(4):493–496. [PubMed] [Google Scholar]
- 37.National Committee for Clinical Laboratory Standards. Performance Standards For Antimicrobial Susceptibility Testing, 12th Informational Supplement. Wayne, Pa, USA: National Committee for Clinical Laboratory Standards; 2002. (Approved standard M100-S12). [Google Scholar]
- 38.Elsinghorst EA. Measurement of invasion by gentamicin resistance. Methods in Enzymology. 1994;236:405–420. doi: 10.1016/0076-6879(94)36030-8. [DOI] [PubMed] [Google Scholar]
- 39.Harborne JB. Phytochemical Methods. New York, NY, USA: Chapman and Hall; 1976. [Google Scholar]
- 40.Wagner H, Bladt S, Zgairski EM. Plant Drug Analysis. New York, NY, USA: Springer; 1984. [Google Scholar]
- 41.Myers N, Mittermeler RA, Mittermeler CG, da Fonseca GAB, Kent J. Biodiversity hotspots for conservation priorities. Nature. 2000;403(6772):853–858. doi: 10.1038/35002501. [DOI] [PubMed] [Google Scholar]
- 42.Perumal Samy R, Ignacimuthu S. Antibacterial activity of some folklore medicinal plants used by tribals in Western Ghats of India. Journal of Ethnopharmacology. 2000;69(1):63–71. doi: 10.1016/s0378-8741(98)00156-1. [DOI] [PubMed] [Google Scholar]
- 43.Nampoothiri K, Chrispal A, Begum A, Jasmine S, Gopinath KG, Zachariah A. A clinical study of renal tubular dysfunction in Cleistanthus collinus (Oduvanthalai) poisoning. Clinical Toxicology. 2010;48(3):193–197. doi: 10.3109/15563651003641786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Strathern M. Useful Knowledge. Brunswick, UK: The Isiah Berlin Lecture. University of Manchester; [Google Scholar]
- 45.Sunil CN, Pradeep AK. (2001) Another new species of Tripogon (Poaceae) from India. Sida. 2005;19:803–806. [Google Scholar]
- 46.Biber-Klemm S, Cottier T. Right To Plant Genetic Resources and Traditional Knowledge: Basic Issues and Prospective. Nosworthy Way, UK: Oxfordshire; 2006. [Google Scholar]
- 47.Ramachandran VS, Shijo Joseph S, Aruna R. Ethnobotanical studies from amaravathy range of Indira Gandhi Wildlife Sanctuary, Western Ghats, Coimbatore District, Southern India. Ethnobotanical Leaflets. 2009;13:1069–1087. [Google Scholar]
- 48.Rajasab AH, Mohamad I. Documentation of folk knowledge on edible wild plants of North Karnataka. Indian Journal of Traditional Knowledge. 2004;3(4):419–429. [Google Scholar]
- 49.Rajadurai M, Vidhya VG, Ramya M, Bhaskar A. Ethno-medicinal plants used by the traditional healers of pachamalai hills, Tamilnadu, India. Studies on Ethno-Medicine. 2009;3(1):39–41. [Google Scholar]
- 50.Adesina SK, Idowu O, Ogundaini AO, et al. Antimicrobial constituents of the leaves of Acalypha wilkesiana and Acalypha hispida . Phytotherapy Research. 2000;14(5):371–374. doi: 10.1002/1099-1573(200008)14:5<371::aid-ptr625>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 51.Gutierrez-Lugo MT, Singh MP, Maiese WM, Timmermann BN. New antimicrobial cycloartane triterpenes from Acalypha communis . Journal of Natural Products. 2002;65(6):872–875. doi: 10.1021/np020044g. [DOI] [PubMed] [Google Scholar]
- 52.Tyagi AK, Malik A. Antimicrobial potential and chemical composition of Mentha piperita oil in liquid and vapour phase against food spoiling microorganisms. Food Control. 2011;22(11):1707–1714. [Google Scholar]
- 53.Devendran G, Balasubramanian U. Qualitative phytochemical screening and GC-MS analysis of Ocimum sanctum L. leaves. Asian Journal of Plant Science and Research. 2011;1(4):44–48. [Google Scholar]
- 54.Jain VC, Patel NM, Shah DP, Patel PK, Joshi BH. Antioxidant and antimicrobial activities of Alangium salvifolium (L.f.) Wang root. Global Journal of Pharmacology. 2010;4(1):13–18. [Google Scholar]
- 55.Swapna Latha P, Kannabiran K. Antimicrobial activity and phytochemicals of Solanum trilobatum Linn. African Journal of Biotechnology. 2006;5(23):2402–2404. [Google Scholar]
- 56.Usha1 M, Ragini S, Naqvi SMA. Antibacterial activity of acetone and ethanol extracts of Cinnamon (Cinnamomum zeylanicum) and Ajowan (Trachyspermum ammi) on four food spoilage bacteria. International Research Journal of Biological Sciences. 2012;1(4):7–11. [Google Scholar]
- 57.Prabuseenivasan S, Jayakumar M, Ignacimuthu S. In vitro antibacterial activity of some plant essential oils. BMC Complementary and Alternative Medicine. 2006;6, article 39:1–8. doi: 10.1186/1472-6882-6-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ayoola GA, Lawore FM, Adelowotan T, et al. Chemical analysis and antimicrobial activity of the essential oil of Syzigium aromaticum (clove) African Journal of Biotechnology. 2008;7(13):2227–2231. [Google Scholar]
- 59.Fu YJ, Chen L, Zu Y, et al. The antibacterial activity of clove essential oil against Propionibacterium acnes and its mechanism of action. Archives of Dermatology. 2009;145(1):86–88. doi: 10.1001/archdermatol.2008.549. [DOI] [PubMed] [Google Scholar]
- 60.Venkatesan D, Karrunakarn CM, Selva Kumar S, Palani Swamy PT. Identification of phytochemical constituents of Aegle marmelos responsible for antimicrobial activity against selected pathogenic organisms. Ethnobotanical Leaflets. 2009;13:1362–1372. [Google Scholar]
- 61.Arun P, Purushotham KG, Johnsy jayarani J, Kumari V. In vitro Antibacterial Activity of Oldenlandia umbellata an Indian medicinal Plant. Journal of Pharmaceutical Science and Technology. 2010;2(4):198–201. [Google Scholar]
- 62.Manjamalai A, Sardar Sathyajith Singh R, Guruvayoorappan C, Berlin Grace VM. Analysis of phytochemical constituents and antimicrobial activity of some medicinal plants in Taminadu, India. Global Journal of Biotechnology and Biochemistry. 2010;5(2):120–128. [Google Scholar]
- 63.Haslam E. Natural polyphenols (vegetable tannins) as drugs: Possible modes of action. Journal of Natural Products. 1996;59(2):205–215. doi: 10.1021/np960040+. [DOI] [PubMed] [Google Scholar]
- 64.Cai Y, Luo Q, Sun M, Corke H. Antioxidant activity and phenolic compounds of 112 traditional Chinese medicinal plants associated with anticancer. Life Sciences. 2004;74(17):2157–2184. doi: 10.1016/j.lfs.2003.09.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Shan B, Cai YZ, Sun M, Corke H. Antioxidant capacity of 26 spice extracts and characterization of their phenolic constituents. Journal of Agricultural and Food Chemistry. 2005;53(20):7749–7759. doi: 10.1021/jf051513y. [DOI] [PubMed] [Google Scholar]
- 66.Lambert RJW, Skandamis PN, Coote PJ, Nychas G-JE. A study of the minimum inhibitory concentration and mode of action of oregano essential oil, thymol and carvacrol. Journal of Applied Microbiology. 2001;91(3):453–462. doi: 10.1046/j.1365-2672.2001.01428.x. [DOI] [PubMed] [Google Scholar]
- 67.Raccach M. The antimicrobial activity of phenolic antioxidants in food: a review. Journal of Food Safety. 1984;6(3):141–170. [Google Scholar]
- 68.Taniguchi M, Yano Y, Tada E, et al. Mode of action of polygodial, an antifungal sesquiterpene dialdehyde. Agricultural and Biological Chemistry. 1988;52(6):1409–1414. [Google Scholar]
- 69.Nychas GJE. Natural antimicrobials from plants. In: Gould GW, editor. New Methods of Food Preservation. London, UK: Blackie Academic; 1995. pp. 58–89. [Google Scholar]
- 70.Burt S. Essential oils: their antibacterial properties and potential applications in foods—a review. International Journal of Food Microbiology. 2004;94(3):223–253. doi: 10.1016/j.ijfoodmicro.2004.03.022. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Evaluating herbal drugs in vitro could be a valuable tool for screening antibiotic potential of plants. To develop new strategy for improvement for the assessment of their pharmacological, toxicological profile, scientific evidence based approaches are being employed to appropriately evaluate composition, quality, potential medicinal activity and safety of these natural products.


