Abstract
Background
Due to the inconvenience of performing oral glucose tolerance tests and day to day variability in glucose level, glycated hemoglobin (HbA1c) has been recommended by the American Diabetes Association as a method to diagnose diabetes. In addition, the Korean Diabetes Association has also recommended the use of HbA1c as a diagnostic test for diabetes. In this study, we evaluated the prevalence of diabetes according to fasting plasma glucose (FPG) level only or the combination of FPG and HbA1c tests.
Methods
Data from the 2011 Korea National Health and Nutrition Examination Survey (KNHANES) were analyzed. Among 5,811 subjects aged 30 years or older, 5,020 were selected after excluding the data of fasting time <8 hours, missing values from fasting glucose or HbA1c level, previous diagnosis of diabetes made by physicians, or current use of antidiabetic medications. Diabetes was defined as FPG ≥126 mg/dL, previous diagnosis of diabetes made by a medical doctor, current use of antidiabetic medications, and/or HbA1c ≥6.5%. Prediabetes was defined as FPG of 100 to 125 mg/dL and/or HbA1c of 5.7% to 6.4%.
Results
When we used FPG only, the prevalence of diabetes and prediabetes were 10.5% (men, 12.6%; women, 8.5%) and 19.3% (men, 23.8%; women, 14.9%), respectively. When HbA1c was included as a diagnostic test, the prevalence of diabetes and prediabetes increased to 12.4% (men, 14.5%; women, 10.4%) and 38.3% (men, 41%; women, 35.7%), respectively. Participants with HbA1c ≥6.5% and fasting glucose level <126 mg/dL were older and had lower estimated glomerular filtration rate.
Conclusion
We concluded that using fasting glucose level only may result in an underestimation of diabetes and prediabetes. HbA1c is an acceptable complementary diagnostic test for diabetes in Korean patients. However, national standardization is needed to order to use HbA1c as a diagnostic method of diabetes and prediabetes.
Keywords: Diabetes mellitus; Hemoglobin A, glycosylated; Korea National Health and Nutrition Examination Survey; Prediabetic state; Prevalence
INTRODUCTION
The prevalence of type 2 diabetes has tremendously increased worldwide and in Korea [1-3]. Type 2 diabetes was previously defined using fasting plasma glucose (FPG) and 2-hour plasma glucose (PPG) level measured during an oral glucose tolerance test (OGTT). Glycated hemoglobin (HbA1c) has been used as a glycemic marker of diabetes treatment. In June 2009, the International Expert Committee recommended the use of the HbA1c test with a threshold ≥6.5% to diagnose diabetes, which has since been adopted by the American Diabetes Association [4,5]. The Korean Diabetes Association also recommended HbA1c as a diagnostic test [6]. Using HbA1c to diagnose diabetes may identify additional subjects compared to using only fasting glucose level because the measurements of fasting glucose and HbA1c reflect different aspects of glucose metabolism [4,7-9]. After applying this new recommendation, the prevalence of undiagnosed diabetes increased [10].
Although HbA1c may be affected by red cell turnover and renal function rather than glycemia, HbA1c is still a useful diagnostic method of diabetes because of the many advantages such as reduced intraindividual variability, better stability after collection, and no need for fasting compared with measurement of fasting glucose level [4,5]. In comparison, OGTT is a more difficult and time-consuming test to perform than evaluating HbA1c level. If using FPG only for diagnosis of diabetes, individuals with FPG <126 mg/dL and PPG ≥200 mg/dL may be missed because results from FPG and PPG can show a discordance [11-14]. An advantage of using HbA1c level is that it can be determined by both FPG and PPG exposure [7-9]. If using FPG as well as HbA1c in a large-scale screening survey, subjects with FPG <126 mg/dL and PPG ≥200 mg/dL may be diagnosed with diabetes.
We evaluated the prevalence of diabetes according to FPG only and both FPG and HbA1c levels using data from the Korea National Health and Nutrition Examination Survey (KNHANES). In addition, we investigated the trend of the prevalence of diabetes according to sex and age and estimated the population of patients with diabetes or prediabetes.
METHODS
Data source and subjects
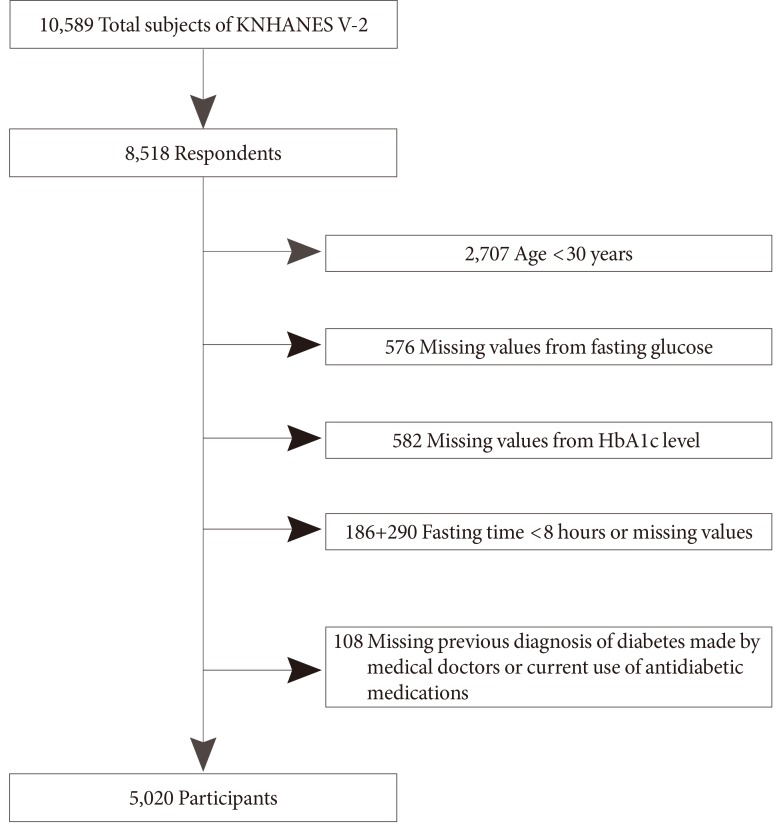
This study was based on data from 2011, the second year of the 5th KNHANES V-2 [15]. The KNHANES is a nationally representative, cross-sectional survey designed to estimate the health and nutritional status of the Korean population as determined by the Division of Health and Nutrition Survey under the Korea Centers for Disease Control and Prevention. This survey used a rolling sampling design with stratified multistage cluster probability sampling. The KNHANES consisted of a health interview survey, health examination survey, and nutrition survey. A stratified, multistage probability sampling was used for the selection of 192 primary sampling units (survey districts), and 3,840 households were extracted and surveyed. A total of 10,589 individuals were sampled for the KNHANES V-2, and 8,518 participated in the survey, for a response rate of 80.4%. Of the 8,518 participants in the health survey, we excluded 2,707 subjects aged <30 years, 1,158 subjects with missing glucose or HbA1c, 476 subjects who fasted for less than 8 hours, and 108 subjects who had not been previously diagnosed by a medical doctor or based on current use of antidiabetic medications. The number of excluded subjects among adults aged ≥30 years was 791. These subjects were more likely to be older, male, and have higher FPG than individuals included in the analysis. Therefore, the prevalence of diabetes may be slightly underestimated because excluded subjects might have a higher risk of diabetes. Finally, 5,020 subjects were included in this analysis (Fig. 1). The total number of adults aged ≥30 years in Korea was estimated to be 31,623,912 (15,442,222 men and 16,181,690 women).
Fig. 1.
Study population framework. KNHANES, Korea National Health and Nutrition Examination Survey; HbA1c, glycated hemoglobin.
Subjects with a previous diagnosis of diabetes made by a physician or those taking insulin or oral hypoglycemic agents were classified as known diabetes. Newly diagnosed diabetes was defined as individuals with FPG ≥126 mg/dL and/or HbA1c ≥6.5% in the absence of known diabetes. Prediabetes was classified as FPG between 100 and 125 mg/dL and/or HbA1c between 5.7% and 6.4% [5].
All individuals in the survey participated voluntarily, and informed consent was obtained from all participants. The survey protocol was approved by the institutional review board of the Korean Centers for Disease Control and Prevention.
Biochemical measurements
Blood was collected from the antecubital vein of each participant after overnight fasting. The samples were properly processed, refrigerated at 2℃ to 8℃, and transported to the Central Testing Institute in Seoul, Korea. Blood samples were analyzed within 24 hours of transportation. Analysis of fasting glucose was performed using a Hitachi Automatic Analyzer 7600 (Hitachi, Tokyo, Japan). HbA1c level was measured with high performance liquid chromatography-723G7 (Tosoh, Tokyo, Japan). Estimated glomerular filtration rates (eGFRs) were calculated with the Cockcroft-Gault formula [16].
Statistical analysis
The data were analyzed with complex-samples analysis procedures in SPSS version 19.0 (IBM Co., Armonk, NY, USA). We used the KNHANES sampling weight variables with stratification and clustering variables to incorporate sample weights and adjust the analysis for the complex sample design of the survey. Nominal variables were presented as the number of cases and percentage and continuous variables as mean±standard error. In order to compare characteristics of four mutually exclusive groups by FPG and HbA1c, general linear regressions were used for continuous variables. A 2-sided P<0.05 was considered to be statistically significant.
RESULTS
We compared characteristics of the four groups by the presence or absence of FPG ≥126 mg/dL and HbA1c ≥6.5% after excluding cases of known diabetes (Table 1). Most participants were classified into the same group by both FPG and HbA1c; 94.9% of participants were classified as nondiabetic and 1.9% as diabetic. However, discordant classifications occurred for 2.1% of subjects with a HbA1c ≥6.5% and FPG <126 mg/dL and for 1.1% with a HbA1c <6.5% and FPG ≥126 mg/dL. Among the study population, 82.6% of individuals with a HbA1c ≥6.5% and FPG <126 mg/dL had impaired fasting glucose (100 to 125 mg/dL) and 82.9% with a HbA1c <6.5% and FPG ≥126 mg/dL had an HbA1c value between 5.7% to 6.4%. Subjects with HbA1c ≥6.5% and FPG <126 mg/dL were older and had a lower eGFR (P<0.05).
Table 1.
Characteristics of Korea National Health and Nutrition Examination Survey participants without known diabetes using glycated hemoglobin and fasting plasma glucose
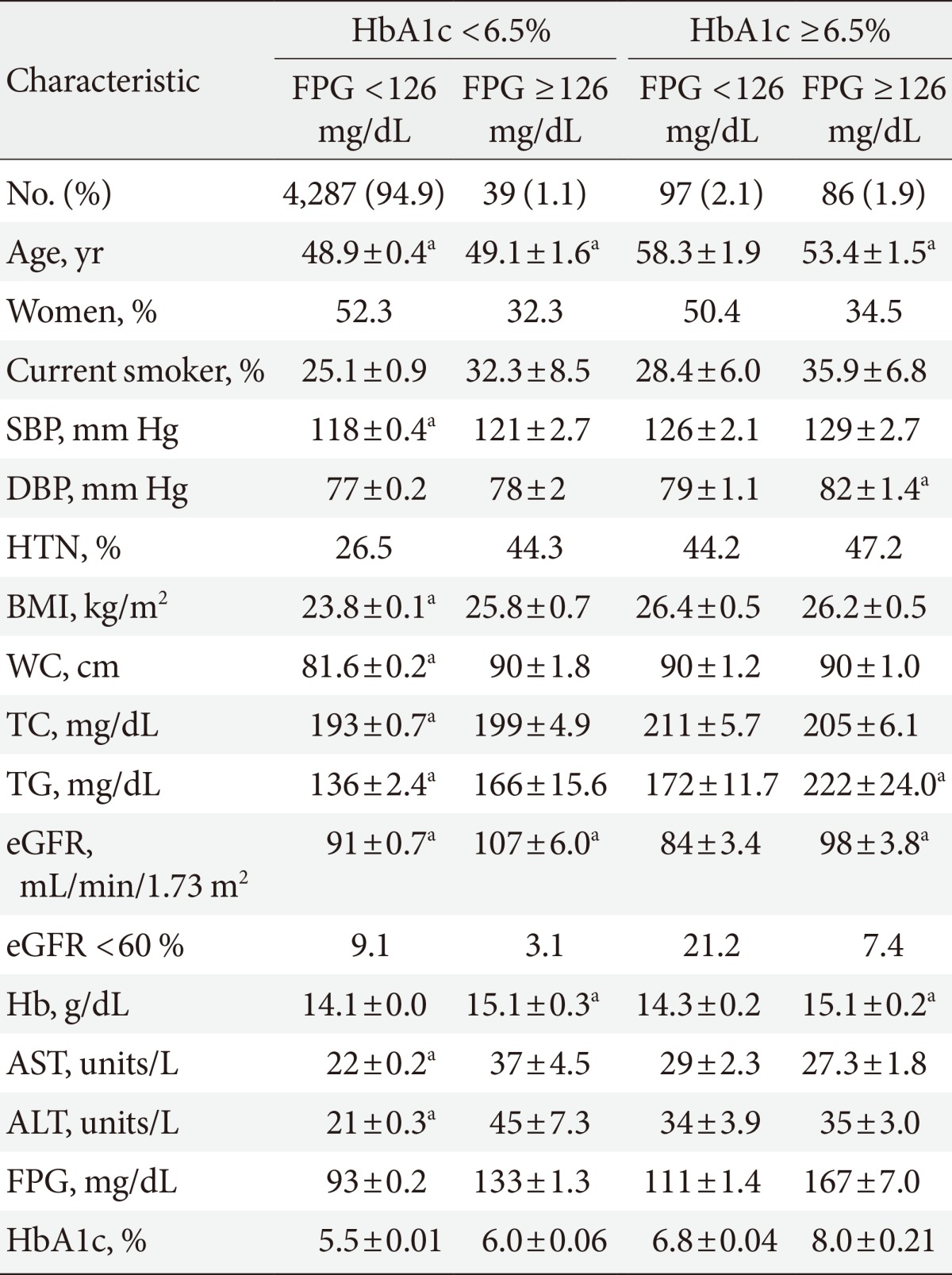
Values are presented as mean±standard deviation. Data were analyzed excluding 46 participants with missing variables.
HbA1c, glycated hemoglobin; FPG, fasting plasma glucose; SBP, systolic blood pressure; DBP, diastolic blood pressure; HTN, hypertension; BMI, body mass index; WC, waist circumference; TC, total cholesterol; TG, triglyceride; eGFR, estimated glomerular filtration rate were calculated using the Cockcroft-Gault formula; Hb, hemoglobin; AST, aspartate aminotransferase; ALT, alanine aminotransferase.
aP<0.05 compared with the group with HbA1c ≥6.5% and FPG <126 mg/dL.
The prevalence of newly diagnosed diabetes was 2.7% using FPG values only (Table 2). If HbA1c was added to the diagnostic measurement, the prevalence of newly diagnosed diabetes increased to 4.7%. The prevalence of diabetes was 10.5% based on FPG only (estimated to be 3.38 million people) and 12.4% based on both FPG and HbA1c (estimated to be 4.01 million people) (Tables 2 and 3). The prevalence of diabetes in male patients increased from 12.6% to 14.5%, and the prevalence of diabetes in female patients increased from 8.5% to 10.4% when including both tests. The percentage of individuals with prediabetes was 19.3% using FPG only (estimated to be 6.1 million people), and that number doubled if HbA1c level was added to FPG value (estimated to be 12.2 million people) (Tables 3 and 4).
Table 2.
Prevalence of diabetes and prediabetes by fasting plasma glucose and/or glycated hemoglobin
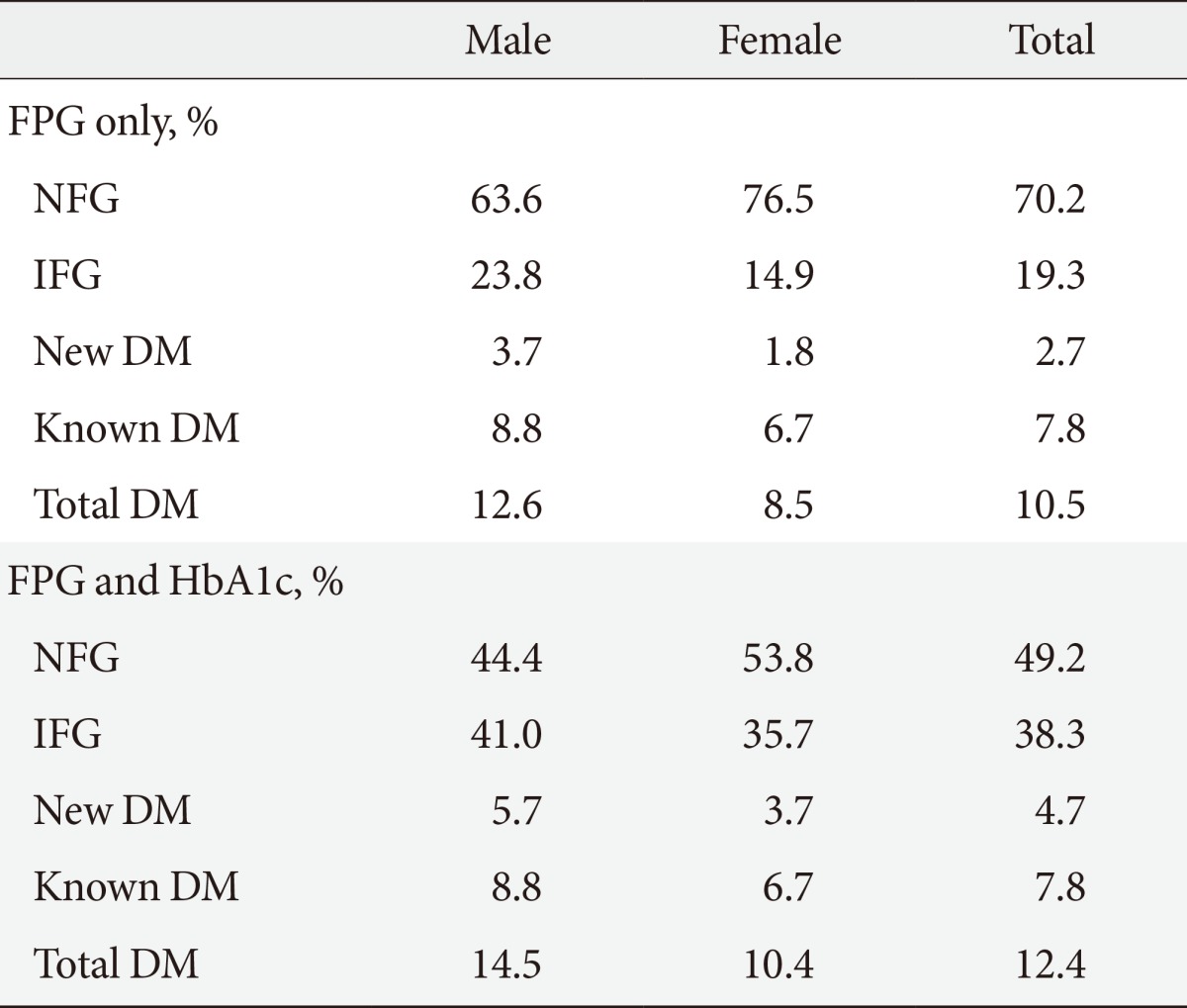
NFG refers to FPG <100 mg/dL and/or HbA1c <5.7%. IFG refers to FPG of 100 to 125 mg/dL and/or HbA1c of 5.7% to 6.4%.
FPG, fasting plasma glucose; NFG, normal fasting glucose; IFG, impaired fasting glucose; DM, diabetes mellitus; HbA1c, glycated hemoglobin.
Table 3.
Prevalence of diabetes according to sex and age
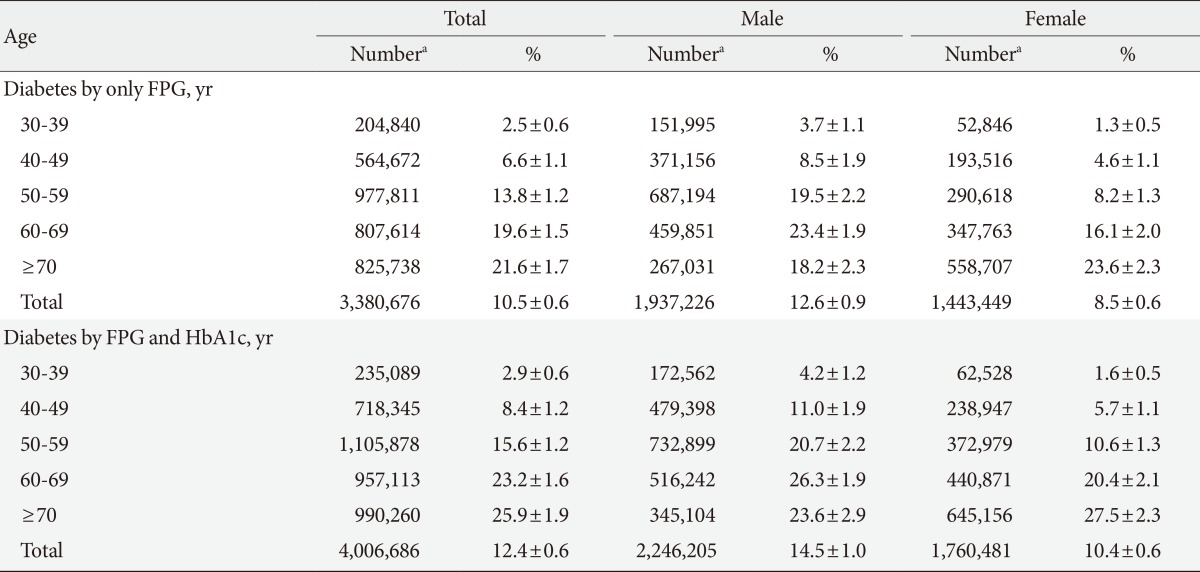
Values are presented as mean±standard deviation.
FPG, fasting plasma glucose; HbA1c, glycated hemoglobin.
aThe prevalence of diabetes is based on a 2011 population estimate.
Table 4.
Prevalence of prediabetes according to sex and age
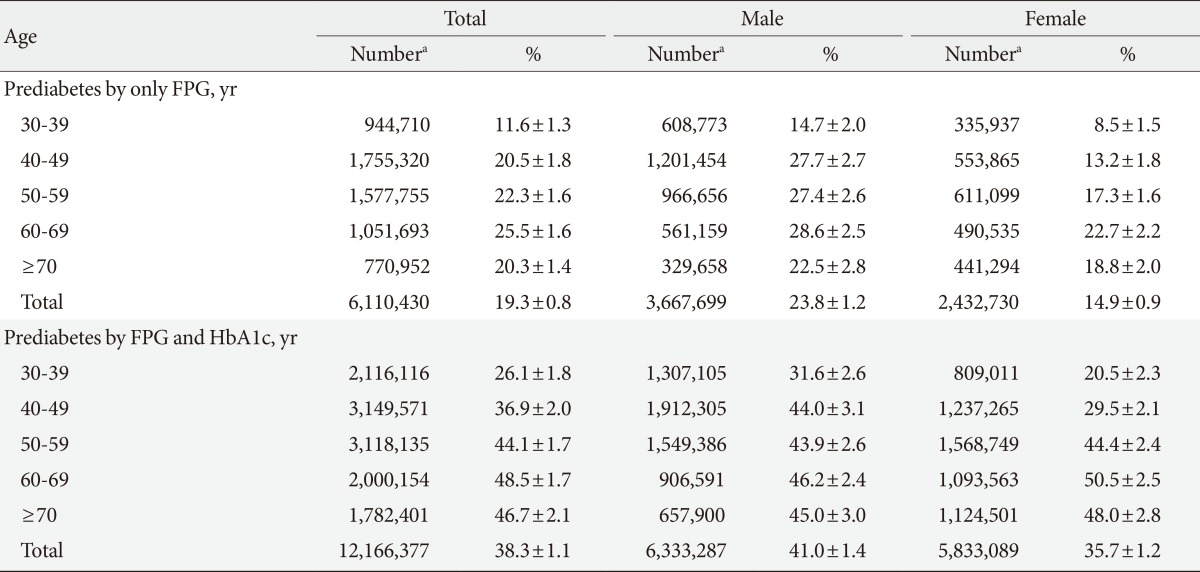
Values are presented as mean±standard deviation.
FPG, fasting plasma glucose; HbA1c, glycated hemoglobin.
aThe prevalence of diabetes is based on a 2011 population estimate.
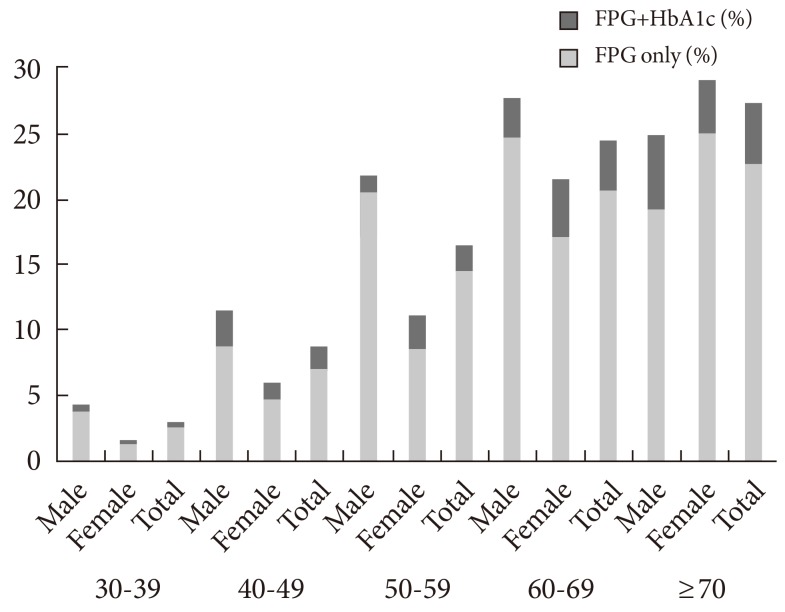
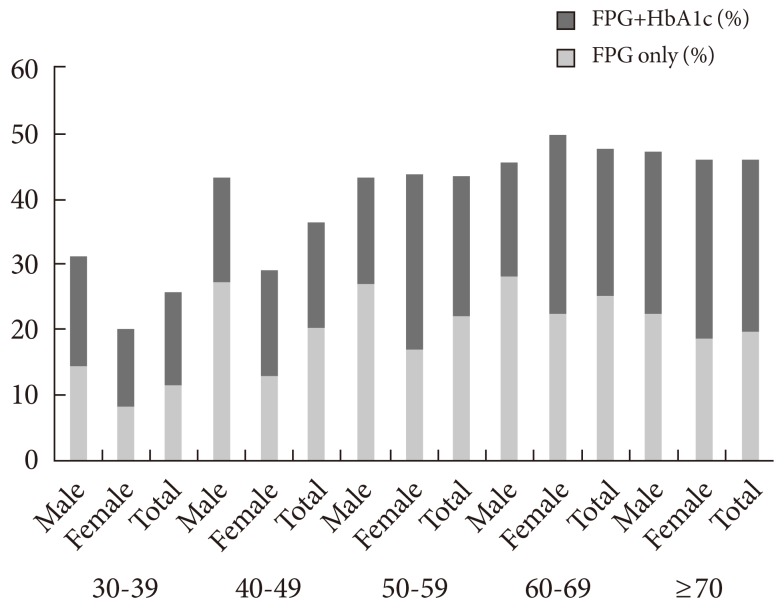
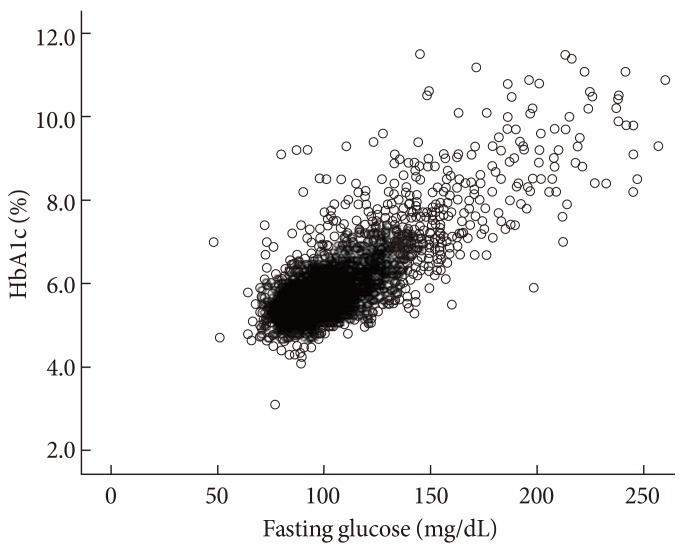
The prevalence of diabetes increased with age (Table 3, Fig. 2). Participants aged ≥70 years had diabetes rates of greater than 20%. When HbA1c was used as an additional diagnostic tool of diabetes, the rate of increasing prevalence according to increasing age was high and around by 5% in the group aged ≥70 years. The prevalence of diabetes in males according to age was stable after the age of 50, but the prevalence of diabetes in females was found to continuously increase with age. The prevalence of prediabetes increased even more than the prevalence of diabetes when both FPG and HbA1c tests were used (Table 4, Fig. 3). Prediabetes was largely increased and was found in approximately 50% of subjects aged ≥60 years. HbA1c and FPG levels were highly correlated each other (r=0.820) (Fig. 4).
Fig. 2.
Prevalence of diabetes according to sex and age. FPG, fasting plasma glucose; HbA1c, glycated hemoglobin.
Fig. 3.
Prevalence of prediabetes according to sex and age. FPG, fasting plasma glucose; HbA1c, glycated hemoglobin.
Fig. 4.
The association of fasting plasma glucose and glycated hemoglobin (HbA1c).
DISCUSSION
This study showed that an additional 2.1% of participants were diagnosed with diabetes when using HbA1c criteria. This percentage was higher than the 1.2% of participants with HbA1c <6.5% and fasting glucose ≥126 mg/dL among subjects with undiagnosed diabetes. This group may have been living with undiagnosed diabetes for a significant period of time. Therefore, it is thought that chronic hyperglycemia and delays in diagnosis might contribute to reduction of renal function.
As expected, the prevalence of diabetes and prediabetes increased with increasing age. Using HbA1c as a diagnostic tool, elderly patients were more likely to be diagnosed with diabetes and prediabetes. The prevalence of diabetes in elderly patients was higher after including HbA1c level, which partly reflects postprandial hyperglycemia, one of the earliest presentations of diabetes [9,10,17]. Using HbA1c levels ranging from 5.7% to 6.4%, the prevalence of prediabetes was 38.3% of the population, twice as high as the prevalence of prediabetes using FPG criteria alone over all age groups. High levels of HbA1c indicated high risk of subsequent diabetes. It is necessary to determine the optimal cut-off values of HbA1c for prediabetes that may require further intervention and management. This was a tradeoff in that a higher cutoff value would be better for patients at higher risk for the disease but was ultimately not costly. First, the relationship between HbA1c level and increased incidence of diabetes should be clarified with prospective studies in Korea. Next, prediabetic cutoff points of HbA1c must be identified and selected according to capacity for management, budget, and effectiveness of the intervention such as lifestyle modifications [18].
Racial and ethnic differences in HbA1c have been reported [19-22]. In contrast to data of the United States National Health and Nutrition Examination Survey, our data showed that the proportion of participants with HbA1c ≥6.5% and FPG <126 mg/dl was larger than that of participants with HbA1c <6.5% and FPG ≥126 mg/dL among subjects with undiagnosed diabetes [10]. Asians had higher HbA1c levels than whites after adjusting for factors that affected glycemia such as fasting and postload glucose level [19]. Hemoglobin glycation rate, red cell turnover, and other unknown factors may contribute to racial and ethnic differences in HbA1c level [20,23,24]. It is not known, however, if these racial and ethnic differences in HbA1c are related to the risk of microvascular or macrovascular complications. Therefore, an HbA1c threshold of 6.5% should be validated to detect diabetic complications in Korea. For example, the association between hyperglycemia and diabetic retinopathy was the basis for the diagnosis of diabetes [25], and in a cross-sectional cohort study, an HbA1c threshold of 6.5% was appropriate to detect diabetic retinopathy in Korean patients [26]. Further studies are necessary to define the relationship between HbA1c and risk for diabetic complications.
Because of methodological differences among laboratories, the HbA1c assay has been standardized through national programs in the USA, Japan, and Sweden [27-29]. Furthermore, for global standardization of HbA1c measurements, the International Federation of Clinical Chemistry and Laboratory Medicine (IFCC) introduced a new reference method to allow for the conversion of values obtained by previous measurements in different countries [30]. This national and global standardization should be required to adopt HbA1c in the clinical setting and to compare data obtained from many countries. The International HbA1c Consensus Committee recommended that HbA1c results be reported in IFCC units (mmol/mol), derived National Glycohemoglobin Standardization Program units (%), and estimated average glucose level [31].
The strength of our study was that these data were based on a nationwide population that was representative of Korean patients. To our knowledge, this was the first study to investigate the prevalence of diabetes and the characteristics in newly diagnosed diabetes using newly revised recommendation guidelines. This study had some limitations. We raised the issue that prediabetes was largely increased and had a prevalence of almost 40% in the Korean population aged ≥30 years using new diagnostic criteria of diabetes. In a prospective cohort study, the 4-year risk of diabetes in subjects with HbA1c of 5.5% to 6.4% was 2.66 times greater compared to patients with HbA1c level <5.5% [32]. In another prospective, community-based cohort study, an HbA1c cutoff of 5.6% was appropriate for the identification of patients at risk of developing diabetes [33]. Another 4-year longitudinal study showed that an HbA1c cut point of 5.7% was suitable for predicting future cases of diabetes [34]. However, we could not determine an optimal cut point of HbA1c for classifying cases of prediabetes that required further intervention. Finally, OGTTs were not performed in the KNHANES and therefore could be not compared to data collected in this study for the diagnosis of diabetes.
In conclusion, diabetes and prediabetes are largely increased when HbA1c is added as a diagnostic test. Using FPG only can underestimate detection of diabetes and prediabetes. We expect new recommendations to be helpful for detection of subjects with early diabetes at risk for complications. Therefore, we conclude that HbA1c is an appropriate complementary diagnostic diagnostic test for diabetes in Korean patients.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Kim DJ. The epidemiology of diabetes in Korea. Diabetes Metab J. 2011;35:303–308. doi: 10.4093/dmj.2011.35.4.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27:1047–1053. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 3.Danaei G, Finucane MM, Lu Y, Singh GM, Cowan MJ, Paciorek CJ, Lin JK, Farzadfar F, Khang YH, Stevens GA, Rao M, Ali MK, Riley LM, Robinson CA, Ezzati M Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Blood Glucose) National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet. 2011;378:31–40. doi: 10.1016/S0140-6736(11)60679-X. [DOI] [PubMed] [Google Scholar]
- 4.International Expert Committee. International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care. 2009;32:1327–1334. doi: 10.2337/dc09-9033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(Suppl 1):S62–S69. doi: 10.2337/dc10-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ko SH, Kim SR, Kim DJ, Oh SJ, Lee HJ, Shim KH, Woo MH, Kim JY, Kim NH, Kim JT, Kim CH, Kim HJ, Jeong IK, Hong EK, Cho JH, Mok JO, Yoon KH Committee of Clinical Practice Guidelines, Korean Diabetes Association. 2011 clinical practice guidelines for type 2 diabetes in Korea. Diabetes Metab J. 2011;35:431–436. doi: 10.4093/dmj.2011.35.5.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Monnier L, Lapinski H, Colette C. Contributions of fasting and postprandial plasma glucose increments to the overall diurnal hyperglycemia of type 2 diabetic patients: variations with increasing levels of HbA(1c) Diabetes Care. 2003;26:881–885. doi: 10.2337/diacare.26.3.881. [DOI] [PubMed] [Google Scholar]
- 8.American Diabetes Association. Postprandial blood glucose. Diabetes Care. 2001;24:775–778. doi: 10.2337/diacare.24.4.775. [DOI] [PubMed] [Google Scholar]
- 9.Bonora E, Calcaterra F, Lombardi S, Bonfante N, Formentini G, Bonadonna RC, Muggeo M. Plasma glucose levels throughout the day and HbA(1c) interrelationships in type 2 diabetes: implications for treatment and monitoring of metabolic control. Diabetes Care. 2001;24:2023–2029. doi: 10.2337/diacare.24.12.2023. [DOI] [PubMed] [Google Scholar]
- 10.Carson AP, Reynolds K, Fonseca VA, Muntner P. Comparison of A1C and fasting glucose criteria to diagnose diabetes among U.S. adults. Diabetes Care. 2010;33:95–97. doi: 10.2337/dc09-1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oh JY, Lim S, Kim DJ, Kim NH, Kim DJ, Moon SD, Jang HC, Cho YM, Song KH, Ahn CW, Sung YA, Park JY, Shin C, Lee HK, Park KS Committee of the Korean Diabetes Association on the Diagnosis and Classification of Diabetes Mellitus. A report on the diagnosis of intermediate hyperglycemia in Korea: a pooled analysis of four community-based cohort studies. Diabetes Res Clin Pract. 2008;80:463–468. doi: 10.1016/j.diabres.2008.01.022. [DOI] [PubMed] [Google Scholar]
- 12.Lee ET, Howard BV, Go O, Savage PJ, Fabsitz RR, Robbins DC, Welty TK. Prevalence of undiagnosed diabetes in three American Indian populations. A comparison of the 1997 American Diabetes Association diagnostic criteria and the 1985 World Health Organization diagnostic criteria: the Strong Heart Study. Diabetes Care. 2000;23:181–186. doi: 10.2337/diacare.23.2.181. [DOI] [PubMed] [Google Scholar]
- 13.Rodriguez BL, Abbott RD, Fujimoto W, Waitzfelder B, Chen R, Masaki K, Schatz I, Petrovitch H, Ross W, Yano K, Blanchette PL, Curb JD American Diabetes Association; World Health Organization. The American Diabetes Association and World Health Organization classifications for diabetes: their impact on diabetes prevalence and total and cardiovascular disease mortality in elderly Japanese-American men. Diabetes Care. 2002;25:951–955. doi: 10.2337/diacare.25.6.951. [DOI] [PubMed] [Google Scholar]
- 14.Wahl PW, Savage PJ, Psaty BM, Orchard TJ, Robbins JA, Tracy RP. Diabetes in older adults: comparison of 1997 American Diabetes Association classification of diabetes mellitus with 1985 WHO classification. Lancet. 1998;352:1012–1015. doi: 10.1016/S0140-6736(98)04055-0. [DOI] [PubMed] [Google Scholar]
- 15.Ministry for Health Welfare and Family Affairs. The second year of the fifth Korea National Health and Nutrition Examination Survey (KNHANES V-2) [updated 2013 Jul 18]. Available from: http://knhanes.cdc.go.kr.
- 16.Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16:31–41. doi: 10.1159/000180580. [DOI] [PubMed] [Google Scholar]
- 17.Bennett CM, Guo M, Dharmage SC. HbA(1c) as a screening tool for detection of Type 2 diabetes: a systematic review. Diabet Med. 2007;24:333–343. doi: 10.1111/j.1464-5491.2007.02106.x. [DOI] [PubMed] [Google Scholar]
- 18.Gregg EW, Geiss L, Zhang P, Zhuo X, Williamson DF, Albright AL. Implications of risk stratification for diabetes prevention: the case of hemoglobin A1c. Am J Prev Med. 2013;44(4 Suppl 4):S375–S380. doi: 10.1016/j.amepre.2012.12.012. [DOI] [PubMed] [Google Scholar]
- 19.Herman WH, Ma Y, Uwaifo G, Haffner S, Kahn SE, Horton ES, Lachin JM, Montez MG, Brenneman T, Barrett-Connor E Diabetes Prevention Program Research Group. Differences in A1C by race and ethnicity among patients with impaired gluglucose tolerance in the Diabetes Prevention Program. Diabetes Care. 2007;30:2453–2457. doi: 10.2337/dc06-2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ziemer DC, Kolm P, Weintraub WS, Vaccarino V, Rhee MK, Twombly JG, Narayan KM, Koch DD, Phillips LS. Glucose-independent, black-white differences in hemoglobin A1c levels: a cross-sectional analysis of 2 studies. Ann Intern Med. 2010;152:770–777. doi: 10.7326/0003-4819-152-12-201006150-00004. [DOI] [PubMed] [Google Scholar]
- 21.Brown AF, Gregg EW, Stevens MR, Karter AJ, Weinberger M, Safford MM, Gary TL, Caputo DA, Waitzfelder B, Kim C, Beckles GL. Race, ethnicity, socioeconomic position, and quality of care for adults with diabetes enrolled in managed care: the Translating Research Into Action for Diabetes (TRIAD) study. Diabetes Care. 2005;28:2864–2870. doi: 10.2337/diacare.28.12.2864. [DOI] [PubMed] [Google Scholar]
- 22.Anand SS, Razak F, Vuksan V, Gerstein HC, Malmberg K, Yi Q, Teo KK, Yusuf S. Diagnostic strategies to detect glucose intolerance in a multiethnic population. Diabetes Care. 2003;26:290–296. doi: 10.2337/diacare.26.2.290. [DOI] [PubMed] [Google Scholar]
- 23.Bunn HF, Haney DN, Kamin S, Gabbay KH, Gallop PM. The biosynthesis of human hemoglobin A1c. Slow glycosylation of hemoglobin in vivo. J Clin Invest. 1976;57:1652–1659. doi: 10.1172/JCI108436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cohen RM, LeCaire TJ, Lindsell CJ, Smith EP, D'Alessio DJ. Relationship of prospective GHb to glycated serum proteins in incident diabetic retinopathy: implications of the glycation gap for mechanism of risk prediction. Diabetes Care. 2008;31:151–153. doi: 10.2337/dc07-1465. [DOI] [PubMed] [Google Scholar]
- 25.UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) Lancet. 1998;352:837–853. [PubMed] [Google Scholar]
- 26.Cho NH, Kim TH, Woo SJ, Park KH, Lim S, Cho YM, Park KS, Jang HC, Choi SH. Optimal HbA1c cutoff for detecting diabetic retinopathy. Acta Diabetol. doi: 10.1007/s00592-013-0452-3. Epub 2013 Jan 25. DOI: http://dx.doi.org/10.1007/s00592-013-0452-3. [DOI] [PubMed] [Google Scholar]
- 27.Little RR, Rohlfing CL, Wiedmeyer HM, Myers GL, Sacks DB, Goldstein DE NGSP Steering Committee. The national glycohemoglobin standardization program: a five-year progress report. Clin Chem. 2001;47:1985–1992. [PubMed] [Google Scholar]
- 28.Shima K, Endo J, Oimomi M, Oshima I, Omori Y, Katayama Y, Kanazawa Y, Kawai T, Kawamori R, Kanno T, Kiyose H, Nakashima K, Nagamine Y, Baba S, Hoshino T, Amino N. Interlaboratory difference in HbA1c measurement in Japan: a report of the committee on an interlaboratory standardization of HbA1c determination, the Japan Diabetes Society. J Jpn Diabetes Soc. 1994;37:855–864. [Google Scholar]
- 29.Arnqvist H, Wallensteen M, Jeppson JO. Standards for long-term measures of blood sugar are established. Lakartidningen. 1997;94:4789–4790. [PubMed] [Google Scholar]
- 30.Manley S, John WG, Marshall S. Introduction of IFCC reference method for calibration of HbA: implications for clinical care. Diabet Med. 2004;21:673–676. doi: 10.1111/j.1464-5491.2004.01311.x. [DOI] [PubMed] [Google Scholar]
- 31.Hanas R, John WG International HbA1c Consensus Committee. 2013 update on the worldwide standardization of the HbA1c measurement. Diabet Med. 2013;30:885–886. doi: 10.1111/dme.12204. [DOI] [PubMed] [Google Scholar]
- 32.Lim NK, Park SH, Choi SJ, Lee KS, Park HY. A risk score for predicting the incidence of type 2 diabetes in a middle-aged Korean cohort: the Korean genome and epidemiology study. Circ J. 2012;76:1904–1910. doi: 10.1253/circj.cj-11-1236. [DOI] [PubMed] [Google Scholar]
- 33.Choi SH, Kim TH, Lim S, Park KS, Jang HC, Cho NH. Hemoglobin A1c as a diagnostic tool for diabetes screening and new-onset diabetes prediction: a 6-year community-based prospective study. Diabetes Care. 2011;34:944–949. doi: 10.2337/dc10-0644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bae JC, Rhee EJ, Lee WY, Park SE, Park CY, Oh KW, Park SW, Kim SW. Optimal range of HbA1c for the prediction of future diabetes: a 4-year longitudinal study. Diabetes Res Clin Pract. 2011;93:255–259. doi: 10.1016/j.diabres.2011.05.028. [DOI] [PubMed] [Google Scholar]