Abstract
Problem gambling is an addictive behavior with high comorbidity with alcohol problems and smoking. A common feature shared by these conditions is impulsivity. Past research shows that individuals with any of these addictions discount delayed money at higher rates than those without, and that the presence of gambling and substance use lead to additive effects on discounting. To date, however, no study examined the impact of smoking on these associations. The goals of this study were to compare the discounting rates of gamblers with and without histories of alcohol problems and smoking, and assess the associations these addictions might have on discounting. We analyzed the discounting rates of treatment-seeking gamblers categorized into four groups based on their histories of alcohol and smoking. Results revealed effects of history of alcohol problems, and an interaction between smoking and alcohol problems, on discounting. Never smokers with histories of alcohol problems discounted money less steeply than the other groups of gamblers. These results suggest that smoking does not produce additional increases on discounting rates in individuals with other addiction problems and the small subpopulation of gamblers with alcohol problems who never smoked is less impulsive and may have unique risk and/or protective behaviors.
Keywords: Delay discounting, impulsivity, gambling, alcohol use problems, and smoking
Problem gambling is an addictive behavior affecting up to 5% of the United State’s population (Kessler et al. 2008; Shaffer, Holt & Bilt 1999), and it has high rates of comorbidity with alcohol use and smoking. Lifetime rates of alcohol use disorders and nicotine dependence among pathological gamblers are 73% and 60%, respectively (Petry, Stinson & Grant 2005; see also Kessler et al. 2008).
Alcohol use and smoking are also closely linked with one another. For example, epidemiological data indicate that 30% of the general population has a problem with alcohol over their lifetimes (Hasin et al. 2007), and 50% of the population smokes over their lifetimes (Dawson 2000). Among individuals with lifetime alcohol problems, even those without diagnosed conditions, the rates of lifetime smoking are extraordinarily high, and between 62% and 88% of heavy drinkers smoke (Substance Abuse and Mental Health Services Administration 2004; Stuyt 1997; Hurt et al. 1996; Batel et al. 1995; DiFranza & Guerrera 1990).
Problem gamblers (i.e., individuals with subthreshold diagnostic criteria and those with a diagnosis of pathological gambling) have high rates of both alcohol use and smoking when each substance use problem is assessed individually (Kessler et al. 2008; Petry, Stinson & Grant 2005). However, the combined prevalence rate of both drinking and smoking, and the prevalence of one substance use problem without the other, has not been examined explicitly in problem gamblers to date. Further, the mechanisms underlying the high rates of comorbidy across addictive disorders are not fully understood (see Funk, Marinelli & Lê 2006; Little 2000 for reviews).
A common feature shared by all three of these conditions that might help explain high rates of comorbidity is impulsivity. Impulsivity can be operationally defined in terms of preference for the smaller more immediate reward over the larger more delayed reward (Logue 1988), and it can be measured via delay discounting (Green & Myerson 2004). The term delay discounting is used to refer to the decline in the subjective value of a reward as a function of the delay to its occurrence. Discounting data are well described by hyperbolic functions (Green & Myerson 2004; Mazur 2001; Kirby 1997), such as the following model proposed by Mazur (1984)
| (1) |
where V is current value of a future reward, D is the delay to reward delivery, A is the undiscounted value of a reward, and k is a free parameter that determines how steep the value of a reward decreases with the passage of time. The higher the discounting rate is, the faster the subjective value of an outcome decays with the passage of time, and thus the more likely the individual will choose the smaller more immediate outcome.
The discounting rate (k in the equation) reflects how decision making is impacted by immediacy, and this parameter is viewed as an impulsivity index. It has been extensively studied within the context of addictive disorders and is conceptually similar across types of addictions. Alcohol dependent individuals, for example, repeatedly select the relatively immediate and short-term effects produced by alcohol intoxication, such as euphoria, or removal of withdrawal symptoms, over the more important delayed consequences produced by sobriety, such as better health, jobs, and social relationships. A similar analogy can be made for smoking, in which the short-term positive effects, including social benefits for those initiating smoking and relief from withdrawal for those physiological dependent on nicotine, are chosen over the long-term health benefits of not smoking. Likewise, individuals with gambling problems wager for the relatively brief positive potential outcomes associated with gambling (e.g., rush, chances of winning), over long-term consequences of not gambling (e.g., having more money and better relationships).
Robust evidence shows that cigarette smokers (e.g., Sweitzer et al. 2008; Reynolds et al. 2004; Bickel, Odum & Madden 1999) as well as individuals with alcohol use disorders (Dom et al. 2006; Mitchell et al. 2005; Bjork et al. 2004; Petry 2001), discount at higher rates than nonsubstance using controls. Even in less severe populations such as college social drinkers, higher discounting rates have been observed in individuals who drink heavily relative to light drinkers (Vuchnich & Simpson 1998). Problem and pathological gamblers also discount delayed rewards at higher rates than non-problem gambling controls (Ledgerwood et al. 2009; Alessi & Petry 2003; Dixon, Marley & Jacobs 2003; Petry 2001; Petry & Casarella 1999).
Some data suggest that the presence of more than one addictive problem is associated with increased delay discounting rates relative to having only one addiction. To date, these data are derived from individuals with gambling and substance use problems (Andrade & Petry 2012; Petry 2001; Petry & Casarella 1999). For example, Petry (2001) evaluated the delay discounting rates of pathological gamblers with and without substance use problems and non-problem gambling, non-substance using controls. Pathological gamblers with substance use problems discounted at higher rates than pathological gamblers without substance use problems, who in turn discounted at higher rates than controls. Conversely, in a sample of controls and substance abusers who were divided into those with and without gambling problems, those with the dual problems had the highest discounting rates, those with only substance use problems had intermediary discounting rates, and those with neither gambling nor substance use problems had the lowest discounting rates (Petry & Cassarela 1999).
Although k values seem to increase with the number of addictive disorders experienced, no known studies have examined the impact of smoking on these associations. The additive effect of substance use and gambling problems may relate to their co-morbidity with smoking status, which was not evaluated in the above studies. Because smoking is related to high rates of discounting (Sweitzer et al. 2008; Reynolds et al. 2004; Bickel, Odum & Madden 1999), it may have independent or additive effects on discounting in problem gamblers with and without alcohol problems.
The purpose of this study was to examine the main and interactive effects of alcohol problem and smoking status on delay discounting in problem gamblers. In this group of problem gamblers, high prevalence rates of both smoking and alcohol problems were anticipated. We hypothesized that alcohol and smoking status may have an additive effect on discounting rates. Given that so few problem drinkers have no histories of smoking, we also anticipated that this group, while expected to be small, may have protective mechanisms related to discounting.
Method
Participants
Participants (n = 323) were drawn from randomized clinical trials of brief interventions for problem and pathological gamblers (Petry et al. 2008; Petry, unpublished data). Recruitment occurred between 1999 and 2005 at substance abuse treatment and medical clinics, and through advertisements. A screening questionnaire containing the South Oaks Gambling Screen (SOGS; Lesieur & Blume 1987), along with items about recent gambling activities and demographic information, was administered. Individuals were invited to participate in the study if they (1) were 18 years of age or older; (2) gambled at least four times and spent a minimum of $100 gambling in the last two months; and (3) scored at least 3 on the SOGS. Participants were ineligible to participate if they (1) had past-month psychotic symptoms or suicidal intention; (2) had reading-level skills below fifth grade; or (3) expressed interest in more intense gambling treatment than the one offered in the clinical trial. Prior to the initiation of the study, individuals who met inclusion criteria provided written informed consent approved by the University of Connecticut Health Center Institutional Review Board.
Assessments
After providing informed consent, patients completed a series of questionnaires in which information about demographics, gambling severity, smoking status, and substance use histories and treatment were collected. Additionally, delay discounting questionnaires were administered.
The Addiction Severity Index (ASI, McLellan et al. 1985), containing an additional section on gambling (ASI-G), assessed severity of problems across eight domains: medical, employment, gambling, alcohol, drug use, legal, social, and psychiatric. A composite score ranging from 0 to 1, with higher values indicating greater problem severity, was derived for each domain. Both the ASI and ASI-G subsection have satisfactory reliability and validity (Petry 2007, 2003; Leonhard et al. 2000; Lesieur & Blume 1992, 1991; McLellan et al. 1985).
The SOGS evaluated severity of problems associated with gambling. The SOGS is a 20-item assessment with well established psychometric properties (Stinchfield 2002; Lesieur & Blume 1987). Scores range from 0 to 20, with scores of 5 or higher reflecting probable pathological gambling, and scores of 3–4 indicating problem gambling (e.g., Bondolfi et al. 2008; Wiebe & Cox 2005; Stinchfield 2002; Volberg & Steadman 1988; Lesieur & Blume 1987).
Delay Discounting Questionnaire
Kirby and colleagues (Kirby, Petry & Bickel 1999; Kirby & Marakovic 1996) developed a questionnaire comprised of 27 questions, each involving a choice between a smaller monetary amount delivered now versus a larger monetary amount delivered at a later point in time. Reward amounts and delays ranged from $11 to $85, and from 7 days to 186 days, respectively. A small ($25–$35), a medium ($50–$60), and a large ($75–$85) magnitude range of monetary values, containing nine questions each, were used for the larger more delayed alternative. Refer to Kirby, Petry, & Bickel (1999) for complete listing of the questions and a more thorough description of the method used to estimate discounting rates, which is briefly outlined below.
Delay discounting estimation procedure
Equation 1 estimated the discounting rates (k) based on the indifference points—that is, the point in which the subjective value of the smaller sooner alternative is assumed to be equal to the larger more delayed alternative. After solving for k in the equation, the delay and magnitude values associated with each pair of choice alternatives lead to nine indifference k values: 0.00016, 0.00040, 0.0010, 0.0025, 0.0060, 0.016, 0.041, 0.1, and 0.25. Each of these nine indifference k values were associated with small, medium, and large monetary values used for the larger delayed alternative (described above), and defined the ranges of values from which participants’ responses were analyzed.
Participants’ delay discounting rates were inferred to be larger or smaller than the indifference k value associated with a given pair of choice alternatives, based on the choices for the smaller sooner or larger later alternative, respectively. Two questions were extracted from the questionnaire to serve as examples: (1) “Would you prefer $40 today, or $55 in 62 days?” (2) “Would you prefer $34 today, or $50 in 30 days?” The indifference k value associated with questions (1) and (2) is 0.060 and 0.16, respectively. Therefore, if a participant selected the smaller sooner alternative in (1) and the larger more delayed alternative in (2), it is inferred that participant’s k was > 0.060 and < 0.16, and the geometric mean of these values was used as the discounting rate. We analyzed participant’s choice pattern and assigned the k value that was most consistent across the 27 questions. Consistency was defined as proportion of choices compatible with each possible k value. In cases in which participants’ response pattern was compatible with more than one k value, we used the arithmetic mean; when participants exclusively selected the smaller or larger alternative, we assigned the lowest or highest k endpoint values, respectively (i.e., 0.00016 or 0.25).
Categorization of alcohol problem history and smoking status
Because the primary studies (Petry et al. 2008; unpublished data) did not diagnose nicotine dependence or alcohol use disorders, we categorized participants into those with and without a lifetime history of alcohol problems and smoking. Specifically, participants were asked if they ever received inpatient or outpatient treatment for alcohol use, and if they ever had a “significant problem” with alcohol. Those who endorsed either question affirmatively were classified as having an alcohol problem. In total, 149 (46.13%) individuals were categorized as having a history of alcohol problems; of these, 86 (57.7%) reported receiving treatment for alcohol, whereas the remaining 63 (42.3%) did not. These rates of alcohol problems are consistent with the prevalence rates of alcohol use diagnoses reported in other samples of problem gamblers (Kessler et al. 2008; Ibáñez et al. 2001; Bondolfi, Osiek & Ferrero 2000; Cunningham-William et al. 1998; Ramirez et al. 1983). Moreover, epidemiological data indicate that over half of individuals with alcohol use disorders never seek treatment for alcohol (Substance Abuse and Mental Health Services Administration 2009; Hasin et al. 2007; Dawson et al. 2006; Regier et al. 1993), consistent with rates of non-treatment seeking for alcohol use problems in our sample.
Participants were also asked if they ever smoked cigarettes daily. A total of 275 participants reported a lifetime history of daily smoking. In total, four groups were created: never smokers with no history of alcohol problems (n=35), ever smokers with no history of alcohol problems (n=139), never smokers with a history of alcohol problems (n=13), and ever smokers with a history of alcohol problems (n= 136).
Data Analytic Procedure
Baseline characteristics among these four groups were evaluated using analyses of variance (ANOVA) for continuous variables and chi-square tests for categorical data. When ANOVAs revealed significant differences among groups, post-hoc t-tests (Least significant difference, LSD) were used to compare differences between each group in relation to the others. Years of education, income, ASI subscale scores, and delay discounting rates were not normally distributed. Because parametric statistics require normality, these variables were log-transformed before the statistical tests were conducted.
General Linear Model Univariate Analysis of Variance (UNIANOVA) evaluated the relationship between smoking and alcohol use problem status, and their interaction, on delay discounting rates. Delay discounting rates (log transformed) were included as the dependent variable, and history of alcohol and smoking problems were included as independent variables in the model (i.e., a two-way factorial design). Other non-overlapping variables that differed across the alcohol and smoking status groups were also included in the model: race, gender, log-transformed years of education, and log-transformed ASI gambling, drug and psychiatric scores. SOGS scores were not included as a covariate in the model because they were highly correlated with ASI gambling scores (p <.001), and other variables were also excluded due to high correlations with other covariates (e.g., education, income and ASI employment scores were all highly correlated, ps < .001). All analyses were conducted on SPSS for Windows (v. 15).
Results
Table 1 depicts baseline and demographic characteristics of problem gamblers by history of alcohol problems and smoking. The groups differed with respect to race, and post-hoc tests found that never smokers (regardless of alcohol problem status) were more likely to be Caucasian and less likely to be African American and Hispanic than ever smokers. Never smokers also scored lower on the SOGS, and they had more years of education and higher salary than ever smokers. In regards to ASI scores, differences among the groups were noted on most domains. Ever smokers (regardless of alcohol status) scored higher than never smokers on the employment and drug use scales. Never smokers with no history of alcohol problems scored lower than smokers on the gambling scale; ever smokers who also endorsed alcohol problems scored higher than participants who did not endorse alcohol problems on the medical subscale of the ASI. In addition, ever smokers with histories of alcohol problems scored higher than the other groups on the psychiatric section, whereas ever smokers without histories of alcohol problems scored lower on the alcohol section. Those with histories of both alcohol problems and smoking had also been treated for substance use problems more often than those with no histories of alcohol problems.
Table 1.
Baseline demographics and characteristics of problem gamblers by alcohol problem and smoking status.
| Variable | No history of alcohol problems | History of alcohol problems | Statistic (df) | p | ||
|---|---|---|---|---|---|---|
|
| ||||||
| Never Smoker (n=35) | Ever Smoker (n=139) | Never Smoker (n=13) | Ever Smoker (n=136) | |||
| Men, % (n) | 57.1 (20) | 54.0 (75) | 92.3 (12) | 58.8 (80) | χ2(3) = 7.26 | .064 |
| Race, % (n) | χ2(9) = 32.22 | <.001 | ||||
| Caucasian | 62.9 (22) | 29.9 (41) | 92.3 (12) | 45.9 (61) | ||
| African American | 17.1 (6) | 45.3 (62) | 7.7 (1) | 34.6 (46) | ||
| Hispanic | 17.1 (6) | 21.9 (30) | 0.0 (0) | 5.3 (7) | ||
| Other | 2.9 (1) | 2.9 (4) | 0.0 (0) | 5.3 (7) | ||
| Age | 39.89 ± 13.29 | 41.17 ± 11.24 | 41.15 ± 9.99 | 42.49 ± 9.01 | F(3, 319) = .72 | .54 |
| Years of educationa | 14.51± 3.08 | 12.31 ± 2.15 | 14.15 ± 1.77 | 12.10 ± 1.9 | F(3, 319) = 11.49 | <.001 |
| Annual incomea | $36,499 ± 37,541 | $18,141 ± 28,535 | $33,300 ± 28,725 | $16,682 ± 22,485 | F(3, 316) = 5.31 | .001 |
| Married, % (n) | 20.0 (7) | 13.7 (19) | 15.4 (2) | 10.3 (14) | χ2(3) = 2.52 | .47 |
| ASI a | ||||||
| Medical | .30 ± .36 | .26 ± .29 | .40±.44 | .47 ± .35 | F(3, 319) = 9.56 | <.001 |
| Employment | .32 ± .37 | .64 ± .35 | .37±.31 | .70 ± .31 | F(3, 319) = 16.80 | <.001 |
| Gambling | .39 ± .20 | .49 ± .21 | .39±.16 | .48 ± .23 | F(3, 319) = 2.89 | .03 |
| Alcohol | .09 ± .10 | .04 ± .07 | .13±.14 | .13 ± .16 | F(3, 319) = 12.67 | <.001 |
| Drug | .01 ± .04 | .08 ± .09 | .02±.03 | .09 ± .10 | F(3, 319) = 9.34 | <.001 |
| Legal | .06 ± .14 | .12 ± .20 | .08±.12 | .11 ± .19 | F(3, 319) = 1.13 | .34 |
| Family/social | .22 ± .24 | .20 ± .20 | .20±.20 | .22 ± .19 | F(3, 319) = .25 | .86 |
| Psychiatric | .18 ± .23 | .16 ± .20 | .13±.19 | .26 ± .22 | F(3, 318) = 5.29 | .001 |
| SOGS scores | 7.60 ± 3.40 | 10.70 ± 4.11 | 7.92 ± 3.62 | 11.58 ± 4.43 | F(3, 318) = 10.37 | <.001 |
Values were log transformed prior to the statistic analysis. To facilitate interpretation, the values are shown in their natural form.
ASI = Addiction Severity Index
SOGS = South Oaks Gambling Screen
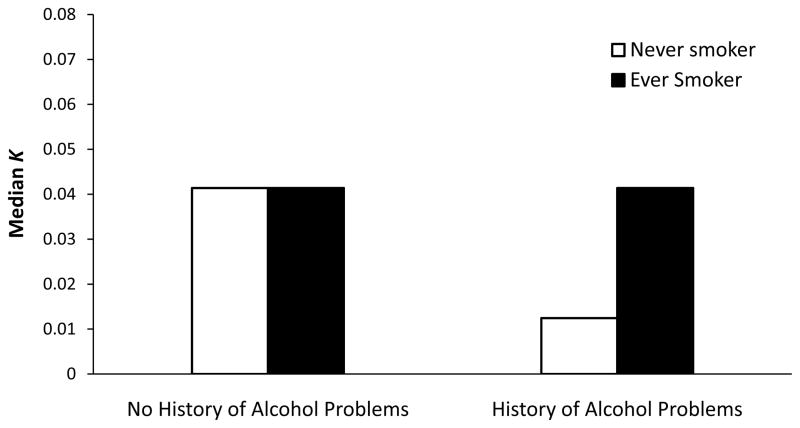
After including race, gender, years of education, and ASI gambling, drug, and psychiatric scores in the model (with the continuous variables log transformed), UNIANOVA revealed significant effects of history of alcohol problems status on logged discounting rates, F (1, 305) = 4.20, p = .04, and a significant interaction between smoking and alcohol problem status, F (1, 305) = 6.21, p =.01. No significant main effect of smoking status on discounting rates were observed, F (1, 305) = 1.03, p = .31. The analysis was also run excluding the covariates. The effects of history of alcohol problems and the interaction between smoking and alcohol problems on logged delay discounting remained significant (ps < .05, data not shown).
Figure 1 depicts the median discounting rates across groups. The median (interquartile (IQ)) discounting rate of ever smokers with and without histories of alcohol problems were 0.04 (0.13) and 0.04 (0.11), respectively. The median (IQ) discounting rates of never smokers with and without histories of alcohol problems were 0.01 (0.02) and 0.04 (0.11), respectively.
Figure 1.
Delay (k value) discounting parameters. Median values obtained by ever smokers (filled bar) and never smokers (unfilled bar) with and without history alcohol problems. To enhance interpretability of the results, values are shown in their natural form.
Discussion
The purposes of this study were to assess discounting rates of problem gamblers with and without histories of alcohol problems and smoking and to examine possible interactive effects that these addictions may have on delay discounting rates. Analyses revealed effects of history of alcohol problems, and an interaction between smoking and alcohol problem status, on delay discounting in problem gamblers. Never smokers with a history of alcohol problems discounted the value of money more slowly than ever smokers with, and both ever and never smokers without, histories of alcohol problems. The lower rates of discounting in never smokers with a history of alcohol problems suggest that these individuals are less impulsive—at least on this index—than the other groups of problem gamblers.
In this sample, almost half of the treatment-seeking gamblers reported having alcohol problems at some point in their lives. Of these, the overwhelming majority (91%) also reported having a history of smoking. Such rates are in line with previous epidemiological studies showing strong association between alcohol and nicotine use (e.g., Hasin et al. 2007; Falk, Yi & Hiller-Sturmhöfel 2006; Dawson 2000), as well studies showing the association of these substance use problems with gambling problems (Kessler et al. 2008; Petry, Stinson & Grant 2005).
Very few individuals who had developed gambling and alcohol problems in this sample never smoked. Lower discounting rates in this group may imply that these individuals were protected, in the sense of being less susceptible to developing comorbid smoking problems. Evidence stemming mainly from nonhuman experiments supports the view of discounting as a marker for developing substance use problems, and suggests that higher discounting precedes drug acquisition. For instance, rats categorized as highly impulsive for food in a delay discounting procedure later self-administered greater amounts of cocaine and alcohol than their less impulsive counterparts (Perry, Nelson & Carroll 2008; Perry et al. 2005; Poulos, Le & Parker 1995). Prospective studies are needed to verify the external validity of these findings and the relation to the development of various addictive problems in humans.
Because earlier studies conducted in problem gamblers and substance abusers have shown that k values increase with the number of addictive disorders (Andrade & Petry 2012; Petry 2001; Petry & Casarella 1999), we anticipated that gamblers with neither alcohol nor smoking problems would exhibit the lowest rates of discounting among all the four groups. Although this effect was not observed, significant interactive effects of smoking and alcohol status were noted. Given the high prevalence rates of smoking and alcohol use problems in gamblers observed here and elsewhere (Kessler et al. 2008; Petry, Stinson & Grant 2005), our results suggest that the small minority of problem gamblers with alcohol use problems who do not smoke may be unique and may have different pathways toward developing addictions, in which delay discounting impulsivity may be less prognostic.
Numerous studies show that smokers discount at higher rates than non-smokers (e.g., Sweitzer et al. 2008; Reynolds et al. 2004; Bickel, Odum & Madden 1999; see Reynolds 2006 for a review), and many studies have demonstrated that substance abusers discount at higher rates than non-substance users (see Yi, Mitchell & Bickel 2010; Reynolds 2006; and Bickel & Marsch 2001, for reviews). However, no known studies have evaluated the additive impact of smoking status on discounting rates in individuals with other addiction problems. Because so many individuals with substance use problems also have smoking histories, evaluation of the impact of smoking status on discounting rates is important. The lack of a main effect of smoking status on delay discounting rates in the current study suggests that smoking status is not associated with further increases in discounting rates among those with other addiction problems.
There are some limitations in the current study that must be considered in interpreting the findings. First, the experimental design does not allow one to assess the direction of the association between discounting rates and substance use, or if this association is a function of other variables that may be confounded with histories of alcohol problems and smoking status. Secondly, alcohol use disorders and smoking dependence were not diagnosed in this study, and different results may have arisen if formal diagnostic criteria were employed. Thirdly, the subgroups of never smokers, especially never smokers with histories of alcohol problems, were small. Distinctions between current and former smokers, and between current and former alcohol problems, were not made because such subgroups would be even smaller. Finally, the lack of a control group without gambling problems might have truncated the range of discounting overall, making the detection of group differences based on histories of alcohol and smoking status less discernable.
Strengths of this study include the large overall sample size and broad inclusion criteria, designed to increase the generalization of the findings. This is the first study to evaluate the additive effect of smoking status on the delay discounting rates of individuals with one or more addiction problems. The results of this study shed some light on the main and interactive effects of alcohol problems and smoking status on discounting rates in individuals with gambling problems. First, smoking status did not lead to additive effects on discounting in individuals with one or more other addiction problems. Second, never smokers with a history of alcohol problems discounted delayed money more slowly than the other groups of problem gamblers. Although the sample size of this group was small, these intriguing results suggest that more research should be directed toward understanding the role of discounting in unique subpopulations of individuals with addictive disorders who managed to refrain from using the most commonly abused substance—nicotine.
Acknowledgments
This research and preparation of this report were supported in part by grants: R01-MH60417, R01-DA021567, P30-DA023918, T32-AA07290, R01-DA027615, R01-DA022739, RO1-DA13444, R01-DA018883, R01-DA016855, R01-DA14618, P50-DA09241, P60-AA03510, R01-DA024667, R21-DA021836, and DF07-028.
Contributor Information
Leonardo F. Andrade, University of Connecticut School of Medicine.
Sheila M. Alessi, University of Connecticut School of Medicine.
Nancy M. Petry, Email: petry@uchc.edu, Calhoun Cardiology Center, MC-3944, University of Connecticut School of Medicine, 263 Farmington Avenue, Farmington, CT 06030-3944. Telephone: 860-679-2593, Fax: 860-679-1312.
References
- Alessi SM, Petry NM. Pathological gambling severity is associated with impulsivity in a delay discounting procedure. Behavioural Processes. 2003;64 (3):345–354. doi: 10.1016/s0376-6357(03)00150-5. [DOI] [PubMed] [Google Scholar]
- Andrade LF, Petry NM. Delay and probability discounting in pathological gamblers with and without a history of substance use problems. Psychopharmacology. 2012;219 (2):491–499. doi: 10.1007/s00213-011-2508-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batel P, Pessione F, Maître C, Rueff B. Relationship between alcohol and tobacco dependencies among alcoholics who smoke. Addiction. 1995;9 (7):977–980. doi: 10.1046/j.1360-0443.1995.90797711.x. [DOI] [PubMed] [Google Scholar]
- Bickel WK, Marsch LA. Toward a behavioral economic understanding of drug dependence: delay discounting processes. Addiction. 2001;96 (1):73–86. doi: 10.1046/j.1360-0443.2001.961736.x. [DOI] [PubMed] [Google Scholar]
- Bickel WK, Odum AL, Madden GJ. Impulsivity and cigarette smoking: Delay discounting in current, never, and ex-smokers. Psychopharmacology. 1999;146 (4):447–454. doi: 10.1007/pl00005490. [DOI] [PubMed] [Google Scholar]
- Bjork JM, Hommer DW, Grant SJ, Danube C. Impulsivity in abstinent alcohol-dependent patients: relation to control subjects and type 1-/type 2-like traits. Alcohol. 2004;34 (2–3):133–150. doi: 10.1016/j.alcohol.2004.06.012. [DOI] [PubMed] [Google Scholar]
- Bondolfi G, Jermann F, Ferrero F, Zullino D, Osiek CH. Prevalence of pathological gambling in Switzerland after the opening of casinos and and the introduction of new preventive legislation. Acta Psychiatrica Scandinavica. 2008;117 (3):236–239. doi: 10.1111/j.1600-0447.2007.01149.x. [DOI] [PubMed] [Google Scholar]
- Bondolfi G, Osiek C, Ferrero F. Prevalence estimates of pathological gambling in Switzerland. Acta Psychiatrica Scandinavica. 2000;101 (6):473–5. doi: 10.1034/j.1600-0447.2000.101006473.x. [DOI] [PubMed] [Google Scholar]
- Cunningham-Williams RM, Cottler LB, Compton W, Spitznagel EL. Taking chances: problem gamblers and mental health disorders – results from the St. Louis Epidemiologic Catchment Area Study. American Journal of Public Health. 1998;88 (7):1093–1096. doi: 10.2105/ajph.88.7.1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DA. Drinking as a risk factor for sustained smoking. Drug and Alcohol Dependence. 2000;59 (3):235–249. doi: 10.1016/s0376-8716(99)00130-1. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Chou PS. Estimating the effect of help-seeking on achieving recovery from alcohol dependence. Addiction. 2006;101 (6):824–834. doi: 10.1111/j.1360-0443.2006.01433.x. [DOI] [PubMed] [Google Scholar]
- DiFranza JR, Guerrera MP. Alcoholism and smoking. Journal of Studies on Alcohol. 1990;51 (2):130–135. doi: 10.15288/jsa.1990.51.130. [DOI] [PubMed] [Google Scholar]
- Dixon MR, Marley J, Jacobs EA. Delay discounting by pathological gamblers. Journal of Applied Behavior Analysis. 2003;36 (4):449–458. doi: 10.1901/jaba.2003.36-449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dom G, D’haene P, Hulstijn W, Sabbe B. Impulsivity in abstinent early- and late-onset alcoholics: Differences in self-report measures and a discounting task. Addiction. 2006;101 (1):50–59. doi: 10.1111/j.1360-0443.2005.01270.x. [DOI] [PubMed] [Google Scholar]
- Falk D, Yi H, Hiller-Sturmhöfel S. An epidemiologic analysis of co-occuring alcohol and tobacco use and disorders: Findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Alcohol Research & Health. 2006;29 (3):162–171. [PMC free article] [PubMed] [Google Scholar]
- Funk D, Marinelli P, Lê A. Biological processes underlying co-use of alcohol and nicotine: Neuronal mechanisms, cross-tolerance, and genetic factors. Alcohol Research & Health. 2006;29 (3):186–192. [PMC free article] [PubMed] [Google Scholar]
- Green L, Myerson J. A discounting framework for choice with delayed and probabilistic rewards. Psychologial Bulletin. 2004;130 (5):769–792. doi: 10.1037/0033-2909.130.5.769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: Results from the national epidemiologic survey on alcohol and related conditions. Archives of General Psychiatry. 2007;64 (7):830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- Hurt RD, Offord KP, Croghan IT, Gomez-Dahl L, Kottke TE, Morse RM, Melton L. Mortality following inpatient addictions treatment: Role of tobacco use in a community-based cohort. Journal of The American Medical Association. 1996;275 (14):1097–1103. doi: 10.1001/jama.275.14.1097. [DOI] [PubMed] [Google Scholar]
- Ibáñez A, Blanco C, Donahue E, Lesieur H, Pérez de Castro I, Fernández-Piqueras J, Sáiz-Ruiz J. Psychiatric comorbidity in pathological gamblers seeking treatment. The American Journal of Psychiatry. 2001;158 (10):1733–1735. doi: 10.1176/ajp.158.10.1733. [DOI] [PubMed] [Google Scholar]
- Kessler R, Hwang I, LaBrie R, Petukhova M, Sampson N, Winters K, Schaffer H. DSM-IV pathological gambling in the National Comorbidity Survey Replication. Psychological Medicine: A Journal of Research in Psychiatry and The Allied Sciences. 2008;38 (9):1351–1360. doi: 10.1017/S0033291708002900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirby KN. Bidding on the future: Evidence against normative discounting of delayed rewards. Journal of Experimental Psychology: General. 1997;126(1):54–70. [Google Scholar]
- Kirby KN, Marakovic NN. Delay-discounting probabilistic rewards: rates decrease as amounts increase. Psychonomic Bulletin & Review. 1996;3 (1):100–104. doi: 10.3758/BF03210748. [DOI] [PubMed] [Google Scholar]
- Kirby KN, Petry NM, Bickel WK. Heroin addicts have higher discount rates for delayed rewards than non-drug-using controls. Journal of Experimental Psychology: General. 1999;128 (1):78–87. doi: 10.1037//0096-3445.128.1.78. [DOI] [PubMed] [Google Scholar]
- Ledgerwood DM, Alessi SM, Phoenix N, Petry NM. Behavioral assessment of impulsivity in pathological gamblers with and without substance use disorder histories versus healthy controls. Drug and Alcohol Dependence. 2009;105 (1–2):89–96. doi: 10.1016/j.drugalcdep.2009.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonhard C, Mulvey K, Gastfriend D, Shwartz M. The Addiction Severity Index: a field study of internal consistency and validity. Journal of Substance Abuse Treatment. 2000;18 (2):129–135. doi: 10.1016/s0740-5472(99)00025-2. [DOI] [PubMed] [Google Scholar]
- Lesieur HR, Blume SB. Modifying the Addiction Severity Index for use with pathological gamblers. American Journal on Addictions. 1992;1 (3):240–247. [Google Scholar]
- Lesieur HR, Blume SB. Evaluation of patients treated for pathological gambling in a combined alcohol, substance abuse and pathological gambling treatment unit using the Addiction Severity Index. British Journal of Addiction. 1991;86 (8):1017–1028. doi: 10.1111/j.1360-0443.1991.tb01863.x. [DOI] [PubMed] [Google Scholar]
- Lesieur HR, Blume SB. The South Oaks Gambling Screen (SOGS): a new instrument for the identification of pathological gamblers. American Journal of Psychiatry. 1987;144 (9):1184–1188. doi: 10.1176/ajp.144.9.1184. [DOI] [PubMed] [Google Scholar]
- Little H. Behavioral mechanisms underlying the link between smoking and drinking. Alcohol Research & Health. 2000;24 (4):215–224. [PMC free article] [PubMed] [Google Scholar]
- Logue AW. Research on self-control: an integrating framework. Behavioral and Brain Sciences. 1988;11 (4):665–679. [Google Scholar]
- Mazur JE. Hyperbolic value addition and general models of animal choice. Psychological Review. 2001;108 (1):96–112. doi: 10.1037/0033-295x.108.1.96. [DOI] [PubMed] [Google Scholar]
- Mazur JE. Tests of an equivalence rule for fixed and variable reinforcer delays. Journal of Experimental Psychology: Animal Behavior Processes. 1984;10 (4):426–436. [PubMed] [Google Scholar]
- McLellan AT, Luborsky L, Cacciola J, Griffith JE, Evans F, Barr HL, O’Brien CP. New data from the Addiction Severity Index. Reliability and validity in three centers. The Journal of Nervous and Mental Disease. 1985;173 (7):412–423. doi: 10.1097/00005053-198507000-00005. [DOI] [PubMed] [Google Scholar]
- Mitchell JM, Fields HL, D’Esposito M, Boettiger CA. Impulsive responding in alcoholics. Alcoholism: Clinical and Experimental Research. 2005;29 (12):2158–2169. doi: 10.1097/01.alc.0000191755.63639.4a. [DOI] [PubMed] [Google Scholar]
- Perry JL, Larson EB, German JP, Madden GJ, Carroll ME. Impulsivity (delay discounting) as a predictor of acquisition of IV cocaine self-administration in female rats. Psychopharmacology. 2005;178 (2–3):193–201. doi: 10.1007/s00213-004-1994-4. [DOI] [PubMed] [Google Scholar]
- Perry JL, Nelson SE, Carroll ME. Impulsive choice as a predictor of acquisition of IV cocaine self-administration and reinstatement of cocaine-seeking behavior in male and female rats. Experimental and Clinical Psychopharmacology. 2008;16 (2):165–177. doi: 10.1037/1064-1297.16.2.165. [DOI] [PubMed] [Google Scholar]
- Petry NM. Gambling and substance use disorders: current status and future directions. American Journal on Addictions. 2007;16 (1):1–9. doi: 10.1080/10550490601077668. [DOI] [PubMed] [Google Scholar]
- Petry NM. Validity of a gambling scale for the Addiction Severity Index. The Journal of Nervous and Mental Disease. The Journal of Nervous and Mental Disease. 2003;191(6):399–407. doi: 10.1097/01.NMD.0000071589.20829.DB. [DOI] [PubMed] [Google Scholar]
- Petry NM. Delay discounting of money and alcohol in actively using alcoholics, currently abstinent alcoholics, and controls. Psychopharmacology. 2001;154 (3):243–250. doi: 10.1007/s002130000638. [DOI] [PubMed] [Google Scholar]
- Petry NM. Unpublished data [Google Scholar]
- Petry NM, Casarella T. Excessive discounting of delayed rewards in substance abusers with gambling problems. Drug and Alcohol Dependence. 1999;56 (1):25–32. doi: 10.1016/s0376-8716(99)00010-1. [DOI] [PubMed] [Google Scholar]
- Petry NM, Stinson FS, Grant BF. Comorbidity of DSM-IV pathological gambling and other psychiatric disorders: results from the national epidemiologic survey on alcohol and related conditions. Journal of Clinical Psychiatry. 2005;66 (5):564–574. doi: 10.4088/jcp.v66n0504. [DOI] [PubMed] [Google Scholar]
- Petry NM, Wienstock J, Ledgerwood D, Morasco B. A randomized trial of brief interventions for problem and pathological gamblers. Journal of Consulting and Clinical Psychology. 2008;76 (2):318–328. doi: 10.1037/0022-006X.76.2.318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poulos CX, Le AD, Parker JL. Impulsivity predicts individual susceptibility to high levels of alcohol self-administration. Behavioural Pharmacology. 1995;6 (8):810–814. [PubMed] [Google Scholar]
- Ramirez LF, McCormick RA, Russo AM, Taber JI. Patterns of substance abuse in pathological gamblers undergoing treatment. Addictive Behaviors. 1983;8(4):425–428. doi: 10.1016/0306-4603(83)90044-8. [DOI] [PubMed] [Google Scholar]
- Regier DA, Narrow WE, Rae DS, Manderscheid RW, Locke BZ, Goodwin FK. The de facto US mental and addictive disorders service system: Epidemiologic Catchment Area prospective 1-year prevalence rates of disorders and services. Archives of General Psychiatry. 1993;50 (2):85–94. doi: 10.1001/archpsyc.1993.01820140007001. [DOI] [PubMed] [Google Scholar]
- Reynolds B. A review of delay-discounting research with humans: relations to drug use and gambling. Behavioural Pharmacology. 2006;17 (8):651–67. doi: 10.1097/FBP.0b013e3280115f99. [DOI] [PubMed] [Google Scholar]
- Reynolds B, Richards JB, Horn K, Karraker K. Delay discounting and probability discounting as related to cigarette smoking status in adults. Behavioural Processes. 2004;65 (1):35–42. doi: 10.1016/s0376-6357(03)00109-8. [DOI] [PubMed] [Google Scholar]
- Shaffer HJ, Hall MN, Vander Bilt JV. Estimating the prevalence of disordered gambling behavior in the United States and Canada: A research synthesis. American Journal of Public Health. 1999;89 (9):1369–1376. doi: 10.2105/ajph.89.9.1369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stinchfield R. Reliability, validity, and classification accuracy of the South Oaks Gambling Screen (SOGS) Addictive Behaviors. 2002;27 (1):1–19. doi: 10.1016/s0306-4603(00)00158-1. [DOI] [PubMed] [Google Scholar]
- Stuyt EB. Recovery rates after treatment for alcohol/drug dependence: Tobacco users vs. non-tobacco users. American Journal on Addictions. 1997;6 (2):159–167. [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. The NSDUH Report -Alcohol Treatment: Need, Utilization, and Barriers (Office of Applied Studies) Rockville, MD: 2009. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. NSDUH Series H–25, DHHS Publication No SMA 04–3964. Office of Applied Studies; Rockville, MD: 2004. Results from the 2003 National Survey on Drug Use and Health: National Findings. [Google Scholar]
- Sweitzer MM, Donny EC, Dierker LC, Flory JD, Manuck SB. Delay discounting and smoking: association with the Fagerstrom test for nicotine dependence but not cigarettes smoked per day. Nicotine & Tobacco Research. 2008;10 (10):1571–1575. doi: 10.1080/14622200802323274. [DOI] [PubMed] [Google Scholar]
- Volberg RA, Steadman HJ. Refining prevalence estimates of pathological gambling. The American Journal of Psychiatry. 1988;145 (4):502–505. doi: 10.1176/ajp.145.4.502. [DOI] [PubMed] [Google Scholar]
- Vuchinich RE, Simpson CA. Hyperbolic temporal discounting in social drinkers and problem drinkers. Experimental and Clinical Psychopharmacology. 1998;6 (3):292–305. doi: 10.1037//1064-1297.6.3.292. [DOI] [PubMed] [Google Scholar]
- Wiebe JD, Cox BJ. Problem and probable pathological gambling among older adults assessed by the SOGS-R. Journal of Gambling Studies. 2005;21 (2):205–221. doi: 10.1007/s10899-005-3032-9. [DOI] [PubMed] [Google Scholar]
- Yi R, Mitchell SH, Bickel WK. Delay discounting and substance abuse-dependence. In: Madden GJ, Bickel WK, editors. Impulsivity: the behavioral and neurological science of discounting. American Psychological Association; Washington, DC: 2010. [Google Scholar]