Abstract
Purpose
Previously we showed that mild thermal stress increased Natural Killer (NK) cell - mediated tumor cytotoxicity and that this could be blocked by anti-NKG2D or anti-MICA antibodies. Here, we investigated the role of the transcription factor HSF1 in thermal regulation of MICA expression in tumor cells in vitro and in vivo.
Materials and Methods
Hyperthermia experiments were conducted in vitro and in mice using a target temperature of 39.5°C. Apoptotic cells and NK cells in situ were visualized by use of the TUNEL assay or expression of NKp46 respectively. Using Colo205 cells, HSF1 message was blocked utilizing siRNA while luciferase reporter assays were used to measure the activity of the MICA promoter in vitro. Cell surface MICA was measured by flow cytometry.
Results
Following WBH, tumor tissues showed an increase in NK cells and apoptosis. Mild thermal stress resulted in a transient increase in surface MICA and enhanced NK cytotoxicity of the Colo205 colon cancer cell line. Silencing (mRNA) HSF1 expression in Colo205 cells prevented the thermal enhancement of MICA message and surface protein levels, with partial loss of thermally enhanced NK cytotoxicity. Mutations of the HSF1 binding site on the MICA promoter implicated HSF1 in the thermal enhancement of MICA. Some, but not all, patient-derived colon tumor derived xenografts also exhibited an enhanced MICA message expression after WBH.
Conclusions
Upregulation of MICA expression in Colo205 cells and enhanced sensitivity to NK cell killing following mild thermal stress is dependent upon HSF1.
Keywords: Natural Killer Cells, Fever-Range Hyperthermia, Cytotoxicity, HSF-1, NKG2D
Introduction
Natural Killer (NK) cells are immune effector cells with the innate ability to target and kill MHC Class I negative target cells [1, 2]. Therefore NK cells provide host surveillance against cells that exhibit loss or downregulation of MHC Class I such as virally infected or transformed cells, [3–5], and they are therefore recognized as having an important role in controlling tumor growth and metastasis [6, 7]. NK cells express two distinct classes of cell surface receptors, inhibitory and activating receptors, which enable target recognition and ensure the appropriate response. Inhibitory receptors, which protect target cells from cytotoxicity include Killer Inhibitory Receptor family members (KIR) that recognize HLA family members [8] and CD94/NKG2A-B heterodimeric receptors that specifically recognize HLA-E [9]. On the other hand, there are a variety of activating receptors which induce cell cytotoxicity and include Natural Cytotoxicity Receptors (NCR) (i.e. NKp30, NKp44, NKp46 and NKp80)[10], NKG2D [11], KIR2DS [12], 2B4 [13], DNAM-I [14], NTB-A [15] and CD94/NKG2C heterodimer [16]. NK cell mediated killing cannot be triggered unless there is a dominance of activating receptor signals over inhibitory receptor signals for receptor-ligand mediated recognition of target cells [17]. Therefore, identification of factors which can result in elevated levels of activating ligands on target cells may play an important role in enhancing regulating NK cell function.
A variety of hyperthermia protocols have been shown to have different effects on the cytotoxic activity of NK cells (for review see [18]) but overall these studies indicate a general increase in NK mediated cytotoxicity induced by hyperthermia in both pre-clinical and clinical studies. Our group has previously shown that the activity of NK cells against the human colon carcinoma cell line, Colo205 can be enhanced following treatment with mild (fever-range) hyperthermia. [19]. However, little is known about potential mechanism(s) by which NK cell function is regulated by temperature.
In response to several different types of stress, cells upregulate expression of MICA [20, 21], [22] [23], [24–35] a ligand for NKG2D on NK cells, and we have previously speculated that upregulation of MICA in response to thermal stress could act as an evolutionarily conserved danger signal that may play a role during febrile states. [19, 36]. The MICA core promoter contains heat shock elements that inducibly bind HSF1 [21, 32]. Many previous studies have shown that HSF1 acts as a temperature sensitive transcription factor that regulates heat shock protein expression following heat shock and other stresses. [37]. Fionda et al. [38] showed that inhibition of (mRNA) HSF1 with shRNA interference blocks MICA and MICB upregulation in human myeloma cell lines and that HSF1 is recruited to MICA/B promoters by HSP90 inhibitors. Moreover, HSF1 is upregulated in T lymphocytes following mild thermal stress temperatures of 39°C [39]. In line with these findings, heat shock treatment upregulated MICA promoter activity in quiescent HCT116 colon tumor cells [32]. However, there is little information on whether HSF1 could be a key regulator of MICA expression under physiological (fever-range) temperatures. Thus, in this study we tested whether MICA might be regulated by HSF1 following mild thermal stress which in turn, leads to enhanced recognition of target cells by NK cells.
Materials and Methods
Cell lines, NK and human colon cell isolation and in vitro heating
Colo205 and HT29 human colon adenocarcinoma cell lines, CT26 colon and B16.F10 melanoma murine cell lines (ATCC) were propagated in RPMI-1640 medium with 2mM L-glutamine and 10% FBS. For in vitro heating of cells, we incubated control cell culture plates at 37°C, and experimental cell culture plates at 39.5°C for 6 hours in a controlled humidity CO2 incubator.
Human NK cells were isolated from healthy donor peripheral blood as described before [19]. Briefly NK cells were purified by depletion of non-NK cells from PBMC with magnetic separation using an NK cell isolation kit (Miltenyi Biotech, Auburn, CA) according to the manufacturer’s protocol. Cell viability and purity were found to be over 90% with propidium iodide staining.
For isolation of human colonocytes, approximately 5 cm long (~ 10g) samples from normal regions of ascending colon were collected through Tissue Procurement from recently deceased patients at Roswell Park Cancer Institute using an approved protocol and processed within 18 hrs. Blood and luminal contents were removed by washing the section with cold tap water and then the sections were dissected longitudinally and placed in sterile ice-cold RPMI-1640 with L-glutamine, penicillin/streptomycin and Amphotericin B. Visible fat, necrotic tissue/debris and mucus were removed. The mucosal layer (top layer-which contains epithelial cells) was separated from the connective tissue and membranes (bottom layer) and strips (approx. 4–5mm) were cut and placed in Petri dishes and washed with warm HBSS with 0.15% DTT to remove residual matter. Mucosal strips were transferred to a new container with 200ml of RPMI 1640 with 1mM EDTA, 10% Fetal Bovine Serum (FBS) and antibiotic/antimycotic solution (RPMI-EDTA-FBS) with a stir bar and stirred at room temperature at 60rpm for a minimum of 4 hours to release cells from basal lamina. These isolated colon cells were cultured as previously described [40], and propagated in Epithelial Growth Media consisting of RPMI-1640 medium supplemented with 5% fibroblast conditioned media, antibiotic/antimycotic solution (penicillin, streptomycin, amphotericin B), 2mM L-glutamine, 10% FBS, insulin (5µg/ml) and transferrin (5µg/ml).
Whole body hyperthermia (WBH)
The systemic heating of mice was carried out in an incubator (Memmert Model BE500, East Troy, WI). Sterile cages were preheated to ~38.5°C in the incubator. Sentinel mice bearing tumors and implanted with glass-encased temperature transponders (BioMedic Data Systems, Inc. Seaford, DE) at least two weeks prior to heating were included in each cage in order to allow monitoring of temperature during the incubation period. Temperature readings were performed using a hand-held, non-contact temperature measurement device. (BMDS Pocket Scanner, Model DAS-5007, BioMedic Data Systems, Inc. Seaford, DE). Baseline measurements were taken, mice were injected intraperitoneally with 1 mL sterile saline and then placed in either a cabinet at room temperature (controls) or in pre-heated cages in the incubator (WBH). Temperatures of sentinel mice were taken after 15–30 minutes and then every hour for the duration of the WBH. The temperature of the incubator was adjusted as necessary to maintain a mouse core temperature 39.5±0.5°C.
Cytotoxicity Assays
Cytotoxicity assays were performed using the CytoTox 96 non-radioactive cytotoxicity assay (Promega Corp, Madison WI) according to the manufacturer’s instructions as described before [19]. Briefly human colon tumor cells were mixed with purified human NK cells at several dilutions and after brief centrifugation to bring them in contact, incubated for six hours. The supernatant was analyzed for lactate dehydrogenase (LDH) release from dead cells and compared to maximum LDH release from detergent mediated lysis and spontaneous LDH release from untreated cells.
Monoclonal antibodies and Flow Cytometry
For flow cytometric staining, 106 cells were washed twice with PBS followed by incubation with anti-MICA monoclonal antibody (mAb) (Immatics Biotechnologies, Tubingen, Germany), anti-HLA-ABC mAb (BD Biosciences Pharmingen, San Diego CA), or isotype control antibodies for 30 min. on ice. They were then washed twice with sterile PBS, and stained with PE conjugated secondary antibody (BD Biosciences Pharmingen) for 20 min. on ice. Finally, cells were washed twice with PBS and fixed with freshly prepared 2% paraformaldehyde in PBS, and analyzed with FACScan (BD Biosciences, San Jose, CA) flow cytometer and FCS Express 3 software (De Novo Software, Los Angeles, CA).
Immunohistochemistry
Six to eight micrometer thick frozen sections of tumors isolated from mice were air-dried overnight and fixed in cold acetone for 10 minutes. Slides were washed with PBS/Tween 20 (0.5% v/v) and endogenous peroxidase and biotin was blocked with 0.3% hydrogen peroxide for avidin/biotin treatments. Sections were treated with 0.03% casein before treatment with goat anti-mouse NKp46/NCR1 antibody (Catalogue number AF2225, R&D Systems Minneapolis, MN) diluted 1:500 in DAKO antibody diluent (DAKO North America, Carpentaria, CA) for one hour. After washing with PBS/Tween three times, and with PBS once, sections were treated with secondary antibody (1:250 dilution of biotinylated horse anti-goat antibody from Vector Laboratories, Burlingame, CA). Sections were washed three times with PBS-Triton X100 (0.2% v/v) and incubated with Streptavidin-HRP followed by the ImmPACT DAB substrate (Vector Laboratories, Burlingame, CA). Sections were counter-stained with Hematoxylin, dehydrated with gradual washes of ethanol and xylene and mounted with Permount Mounting media (Fisher Scientific, Pittsburg, PA), examined and photographed with an Olympus BX40 microscope mounted with a Hitachi HV-C20 CCD camera.
RNA preparation and Quantitative Real-Time PCR procedure
(mRNA) MICA, HSF1 and HSP70 were analyzed by reverse transcription and PCR analysis as well as Quantitative Real Time PCR. RNA from tumor tissue homogenized in lysis buffer was extracted using RNeasy Mini Kit (Qiagen Inc., Valencia, CA) and quantified by measuring absorbance at 260 and 280 nm using GeneQuant RNA/DNA Calculator (Pharmacia/Pfizer, New York, NY). cDNA was prepared as described before [19]. 18S ribosomal RNA (18S) was used as an internal control in quantitative PCR experiments where, FastStart Universal SYBR Green Master mix (Roche Diagnostics GmbH, Mannheim Germany) was used. Briefly SYBR Green Master Mix containing SYBR Green dye, FastStart Taq DNA polymerase, dNTPs, passive reference (ROX) and buffer components, were mixed with MICA reverse (5’-CATGGATCTCACAGACCCTAATCT-3’) and forward (5’-GGATGACCCTGGCTCATATCA-3’), HSF1 reverse (5’-GAGATCAGGAACTGAATGAGC-3’) and forward (5’-AAGTACTTCAAGCACAACAACAT-3’), or HSP70 reverse (5’-GCGATCTCCTTCATCTTGGT-3’), forward (5’-AAGGTGGAGATCATCGCCAA-3’) primers, cDNA, and water according to the manufacturer’s protocols. Amplifications were performed in 96 well QRT-PCR plates (Axygen Scientific Inc. Union City, CA) using an ABI Prism 7900HT Sequence Detection System (Applied Biosystems, Foster City, CA). Fold change in relative signal was determined using the 2−ΔΔCt formula. When necessary, PCR products were analyzed with 1.5% agarose gel electrophoresis and ethidium bromide staining. Images of the gels were obtained with a BioDoc-It Transilluminator System (UVP Upland, CA).
TUNEL assay
Apoptosis in tumor sections was detected by staining sections of frozen tissue in Tissue-Tek O.C.T. blocks for TUNEL assay (Sakura Finetek USA, Torrance, CA) using MEBSTAIN Apoptosis Kit Direct (MBL, Japan) according to manufacturer’s instructions. Briefly, 6µm frozen sections were prepared, fixed in 4% paraformaldehyde and washed with PBS. Next, they were treated with TdT enzyme and FITC conjugated dUTP. Tissue sections were mounted on slides with Vectashield mounting media containing DAPI (Vector Laboratories, Burlingame CA). Positive control sections were treated with DNase I solution (Sigma-Aldrich, St. Louis, MO). Sections were examined with Zeiss Axioskop2 MOT fluorescent microscope mounted with SPOT camera (Diagnostic Instruments, Sterling Heights, MI).
Silencing of HSF1
HSF1 in Colo205 cells was silenced using Silencer Pre-designed siRNAs (Ambion Inc, Austin, TX). The 21-mer siRNA sequences are as follows: #115674 sense 5-GCAACAGAAAGUCGUCAACtt-3, antisense 5-GUUGACGACUUUCUGUUGCtg-3; #3134 sense 5´-AUAGUCAGAAUUGUAUUUUtt-3´, antisense 5'-AAAAUACAAUUCUGACUAUtg-3´. Five million cells were transfected with 5µg HSF1 or control siRNA using Nucleofector Kit T (Amaxa Biosystems, Gaithersburg, MD), according to the manufacturer’s instructions. The cells were harvested 72 hours after transfection for further experiments.
Cycloheximide treatment
Colo205 cells were divided into four groups: the first group was treated with DMSO for the duration of 12 hrs at 37°C; the second group was treated with DMSO for 6 hrs at 37°C and with cycloheximide (5µg/ml) for another 6 hrs at 37°C; the third group was treated with DMSO for 6 hrs at 39.5°C and then with cycloheximide (5µg/ml) for another 6 hrs at 37°C; the fourth group was treated with DMSO for 6 hrs at 39.5°C and for another 6 hrs at 37°C. Cell surface MICA was measured at 0, 6, 7, 8, 9 and 12 hrs with flow cytometry.
Luciferase reporter assays of MICA promoter
Luciferase reporter activity under the MICA promoter was determined following transfection into Colo205 cells using Nucleofector Kit T (Amaxa Biosystems, Gaithersburg, MD), according to the manufacturer’s instructions. One million cells were transfected with 1µg luciferase reporter plasmid and 0.1µg of pRL-CMV Renilla vector, for standardization of transfection efficiency. The cells were harvested 72 hours after transfection. Luciferase assays were performed using Dual Luciferase Reporter Assay System (Promega Corp, Madison WI) according to the manufacturer’s protocol. Transcriptional activity was measured in a Fluoroskan Ascent FL Luminometer (Thermo Electron Corporation, Vantaa, Finland).
MICA promoter plasmids were constructed by cloning the minimal MICA promoter into pGL3.basic vector (Promega Corp, Madison WI), named pGL3.MICA. HSF1 binding site mutations were performed on the pGL3.MICA plasmid using QuikChange Site-Directed Mutagenesis Kit (Stratagene, La Jolla, CA), as detailed in Fig. 2a. Mutations were confirmed by standard sequencing protocols. The mutated plasmid was designated pGL3.HSRE. A reporter plasmid carrying the Simian virus 40 (SV40) promoter and enhancer was used as positive control (pGL3.SV40).
Figure 2. Silencing of (mRNA) HSF1 in tumor cells results in decreased MICA expression and impaired thermally-enhanced cytotoxicity by human NK cells.
Colo205 cells were transfected with two different siRNA constructs against HSF1 (#3134 and #115674) at two different concentrations 3pg/cell (■) and 5pg/cell (□), or with control siRNA at 5pg/cell ( ). Cells were either treated with hyperthermia (39.5°C) for 6 hours, heat-shock (42°C) for one hour or kept at normothermic temperatures. (a) The (mRNA) HSF1 message level was detected with quantitative real-time PCR, 48 hours after transfection. The results were normalized to 18S rRNA expression. (b) The MICA expression on the surface of transfected cells was analyzed by flow cytometry. Dotted line indicates control levels of (mRNA) HSF1 message or MICA surface levels at normothermic temperatures. (c) Thermally enhanced cytotoxicity of human NK cell was reduced when (mRNA) HSF1-silenced Colo205 cells were used as targets in vitro. Target cells were treated with control siRNA (■ and □) or (mRNA) HSF1 siRNA (
). Cells were either treated with hyperthermia (39.5°C) for 6 hours, heat-shock (42°C) for one hour or kept at normothermic temperatures. (a) The (mRNA) HSF1 message level was detected with quantitative real-time PCR, 48 hours after transfection. The results were normalized to 18S rRNA expression. (b) The MICA expression on the surface of transfected cells was analyzed by flow cytometry. Dotted line indicates control levels of (mRNA) HSF1 message or MICA surface levels at normothermic temperatures. (c) Thermally enhanced cytotoxicity of human NK cell was reduced when (mRNA) HSF1-silenced Colo205 cells were used as targets in vitro. Target cells were treated with control siRNA (■ and □) or (mRNA) HSF1 siRNA ( and
and  ) at hyperthermic (39.5°C, 6hrs) (□ and
) at hyperthermic (39.5°C, 6hrs) (□ and  ), or normothermic control temperatures (37°C) (■ and
), or normothermic control temperatures (37°C) (■ and  ). The data were representative of three donors for cytotoxicity assays (n=3). *, p≤0.05 compared to the corresponding normothermic group. †,p≤0.05 compared to the corresponding control siRNA using unpaired t-test with Welch's correction.
). The data were representative of three donors for cytotoxicity assays (n=3). *, p≤0.05 compared to the corresponding normothermic group. †,p≤0.05 compared to the corresponding control siRNA using unpaired t-test with Welch's correction.
Statistics
All data were analyzed using the GraphPad Prism 5.0 (GraphPad Software Inc. San Diego, CA) statistical analysis software. ANOVA analysis was used in tests involving more than two variables. T-test with Welch`s correction was used for the analysis of significance between two unmatched experimental groups. Significance was accepted over 95% confidence.
Results
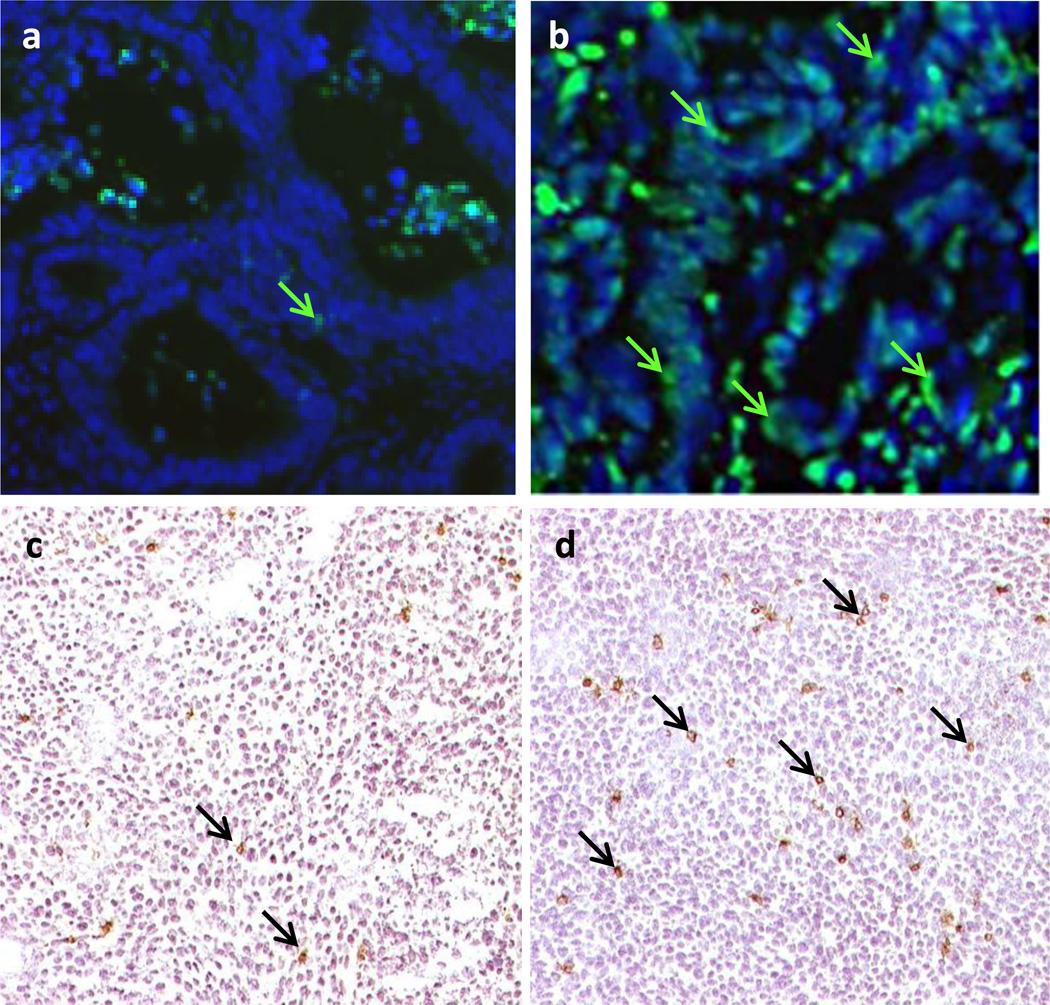
Tumor cell apoptosis and the presence of NK cells in the tumor microenvironment is increased after mild systemic thermal stress
Previous studies from our group demonstrated increased numbers of leukocytes, including NK cells, in the tumor microenvironment of tumor bearing SCID mice treated with fever-range whole body hyperthermia (WBH) [41]; moreover, in that study, we also observed evidence of increased apoptosis which we hypothesized was due to the increased presence of NK cells in the tumor microenvironment. We have confirmed this information using other model systems here: Using a patient-derived colon tumor xenograft we again looked for changes in apoptosis following mild WBH. Tumors from unheated mice showed a low level of apoptosis, (determined using the TUNEL assay [42]) with only a few apoptotic cells visible at normothermic conditions (Fig 1a). However, within a day after WBH, we observed evidence of increased TUNEL positive cells in tumor sections (Fig 1b). In another experiment, using CT26 cells grown as a tumor in BALB/c mice, we found that WBH resulted in an increase in the number of cells bearing a marker for NK cells, NKp46 [10]. Representative photomicrographs from normothermic and hyperthermic BALB/c mice carrying CT26 tumors are shown in Figures 1c and 1d, respectively
Figure 1. Whole body hyperthermia (WBH) increases the numbers of NK cells and apoptotic cells in colon tumors.
(a, b) Localization of apoptotic cells by TUNEL assay in a patient tumor xenograft from control (a) or WBH treated (b) SCID mice (arrows, original mag. 40×). (c, d) Immunohistochemical localization of NKp46+ cells in CT26 tumors from control (c) and WBH treated (d) mice at 24 hrs post-WBH (arrows, original mag-10×).
Since NK cells are the primary cytolytic effector cells in the SCID mouse model, these anatomical and immunohistochemistry data support our hypothesis that mild heating may, in some way, stimulate increased NK cell mediated anti-tumor activity. Additionally, we and others have also shown previously that in vitro heat treatments can enhance NK cell cytotoxicity [18, 19] and that this effect coincides with increased surface expression of MICA on the human colon adenocarcinoma cell line Colo205 [19]. Collectively, these observations support the hypothesis that NK cells are sensitive to thermal stress and that by better understanding the mechanisms underlying this sensitivity, we may better target these cells for clinical hyperthermia applications. Thus, next we examined in greater molecular detail the mechanism by which MICA expression could be regulated by mild thermal stress and focused largely on the role of HSF1.
Thermal enhancement of NK cytotoxicity against colon carcinoma cells is dependent upon HSF1 dependent induction of MICA
We have previously shown that mild heating in vitro results in a significant increase in surface expression of MICA on cells from the human Colo205 cell line [19]. To determine if the increase in MICA following thermal stress was due to HSF1, Colo205 cells were transfected with two constructs of (mRNA) HSF1 siRNA to silence the transcription factor. Control transfectants included negative control siRNA at the highest concentration used for (mRNA) HSF1 silencing. HSF1 is endogenously present in Colo205 cells, and was suppressed to a quarter of the levels in controls by siRNA mediated silencing as determined by western blotting (data not shown). Transfected Colo205 cells were exposed to mild (fever-range) thermal stress (39.5°C) for 6 hours or kept at normothermic (37°C) temperature in vitro. Analysis for (mRNA) HSF1 carried out with quantitative RT-PCR at 48 hours showed that silencing with (mRNA) HSF1 siRNA resulted in a five-fold decrease in thermal stress inducible HSF1 message (Fig 2a) correlating with the reduced protein expression.
The effect of HSF1 reduction on surface MICA expression by Colo205 cells was examined with flow cytometry (Fig 2b). Colo205 cells were treated with thermal stress (39.5°C) for 6 hours and then analyzed for MICA expression. We observed an overall reduction of thermally enhanced surface MICA expression on Colo205 cells after transfection with both (mRNA) HSF1 siRNA constructs at all concentrations.
We next asked whether silencing of HSF1 message would affect susceptibility of the Colo205 cells to NK cell killing. NK cells were isolated from three healthy human donors. Colo205 cells transfected with (mRNA) HSF1 siRNA were used as target cells in NK cell cytotoxicity assays. Transfected cells were either held at (37°C) or treated with mild thermal stress (39.5°C) for 6 hours in vitro as above. Cytotoxicity assays showed that (mRNA) HSF1 silencing resulted in a significant decrease in NK cell mediated cytotoxicity at higher NK cell to target ratios (Fig 2c). These findings confirm our earlier report that thermal stress enhances NK activity and up regulates MICA expression on tumor cells and further suggest that HSF1 plays a critical role in the induction of MICA on Colo205 cells.
Mutation of the HSF1 binding site results in the loss of thermally enhanced activity of the MICA promoter
To further test the role of HSF1 in thermal induction of MICA, the minimal MICA promoter described in [32] was cloned into the pGL3 luciferase reporter construct. HSF1 binding sites in the promoter were mutated by site directed mutagenesis (Fig 3a). Promoter constructs were transfected into Colo205 cells; the cells were then subjected to thermal stress (Fig 3b). Mild thermal stress induced a significant increase in MICA promoter activity as measured by increased luciferase activity and this was abrogated when the HSF1 binding site was mutated. Thermal stress had no effect on luciferase activity in cells transfected with either a promoter-less construct (pGL3) or when luciferase expression was driven by SV40 (pGL3.SV40).
Figure 3. Mutation of HSF1 binding site results in the loss of thermally enhanced activity of MICA promoter.
(a) Schematic representation of plasmid constructs containing luciferase reporter gene driven by MICA promoter. Basic pGL3 construct (pGL3), pGL3 construct carrying the MICA promoter (pGL3.MICA), point mutations in heat shock response element (HSRE) in MICA promoter (pGL3.HSRE), and positive control construct carrying an SV40 promoter and enhancer (pGL3.SV40). (b) Colo205 cells were transfected with the reporter constructs described in (a) and treated at normothermic (■) or hyperthermic (□) temperatures for 6 hours. Relative luciferase activity was detected by dual luciferase reporter assay and normalized to Renilla luciferase activity as transfection control. *, p≤0.05 compared to the corresponding normothermic group.
MICA stability on tumor cell surface after thermal stress depends on thermally enhanced MICA synthesis
Previously we observed an increase in MICA message within three hours after thermal stress in vitro, followed by an observed increase in MICA surface expression at 6 hours [19]. Cycloheximide, as an inhibitor of eukaryotic protein signaling, can block translational elongation; therefore, we used it to determine the extent of de novo translation-independent surface MICA upregulation after mild thermal stress. This experiment tests whether thermal stress-induced cell surface MICA upregulation is due to elevated transcription/translation, or is perhaps due to other events, such as cell membrane changes as we previously observed [19]. Since treatment with cycloheximide following thermal stress leads to a faster loss of MICA surface expression than seen using DMSO alone following thermal stress, the prolonged upregulated MICA surface expression following thermal stress likely requires continual protein synthesis.
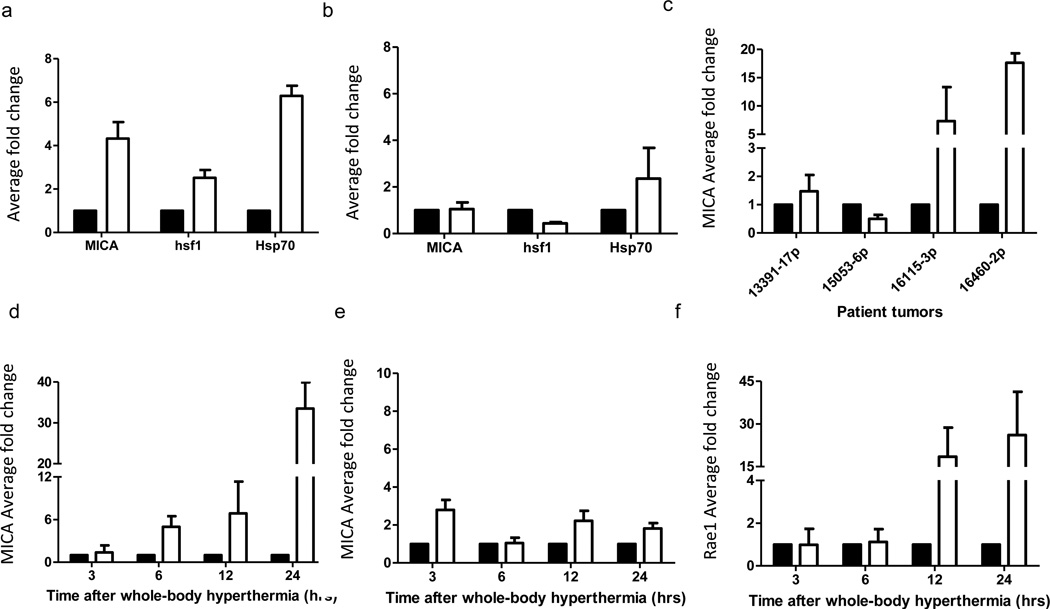
Whole body hyperthermia results in increased MICA in tumor cells in vivo
Our previous results demonstrated that in vitro thermal stress results in upregulation of MICA levels on tumor cells, which correlates with enhanced NK cell cytotoxicity [19]. To ask whether similar results would occur in vivo, i.e., in tumor cells in mice treated with WBH, SCID mice bearing Colo205 (Fig 5a), HT29 (Fig 5b) and 4 different patient-derived colon tumor xenografts (Fig 5c) were treated with WBH. Colo205 derived tumors were found to have upregulated message levels for MICA, HSF1 and HSP70 after whole body hyperthermia (Fig 5a), while HT29 derived tumors only showed an increase in HSP70 (Fig 5b). Of the four patient xenografts, MICA was upregulated in two of the earlier passage tumors 16115 (2nd passage) and 16460 (3rd passage), but not in two late passage tumors 13391 (17th passage) and 15053 (6th passage).
Figure 5. Response of colon cell lines and patient tumor xenografts to mild thermal stress.
Colo205 (a), or HT29 (b) tumor bearing SCID mice were treated with whole body hyperthermia (WBH) at 39.5°C for 6 hours in vivo. Fold change of MICA, HSF1 and HSP70 mRNA in the tumors compared to 18S RNA or levels in tumors from control mice was measured by quantitative RT-PCR and calculated against 18S RNA, using triplicate wells. The data shown represent the mean ± SD (n≥3) of three experiments. (c) Colon tumors from four patients were implanted into SCID mice and treated with WBH. MICA mRNA expression was detected by qPCR and fold change determined compared to untreated controls (d–e) Kinetics of MICA mRNA levels in Colo205 and HT29 xenografts respectively at 3, 6, 12 and 24 hrs after WBH. (f) Kinetics of the murine MICA orthologue, Rae1 mRNA expression in CT26 tumors in BALB/c mice □ hyperthermic, ■ normothermic.
Previous kinetic studies of MICA upregulation with thermal stress showed that transcriptional regulation of MICA message starts as early as three hours in vitro [19]. Therefore we investigated the kinetics of MICA message in Colo205 and HT29 tumors within 24 hours after whole body hyperthermia. (mRNA) MICA levels steadily increased in the Colo205 tumors up to 24h after WBH (Fig 5d). On the other hand, MICA message levels did not increase over the course of 24 hours in HT29 tumors (Fig 5e), in agreement with the lack of increase in MICA message expression at 6 hrs in (Fig 5b). Mouse MICA orthologue, Rae1, mRNA expression in CT26 tumors occurred at 12 hrs post-WBH (Fig 5f) which is slightly slower than the analogous response in Colo205.
Normal human colonocytes do not upregulate MICA after thermal stress
We examined whether mild thermal stress also enhanced surface expression of MICA by normal human colonocytes. Colonocytes isolated from colon samples were treated with mild thermal stress at 39.5°C for 6 hours in vitro, labeled for surface MICA protein expression and pan-HLA (since thermally mediated NK cell cytotoxicity against these cells could potentially change if surface MHC Class I expression is altered) and then compared to Colo205 cells treated under the same conditions. Although MICA and HLA are expressed on normal colonocytes, we observed no change in the expression of either following mild thermal stress (Fig 6a). This compliments our previous studies which showed that there was no change in HLA expression on tumor cells following thermal stress [19].
Figure 6. Expression levels of MICA and MHC Class I are not altered with thermal stress in non-malignant, normal human colon epithelial cells.
Normal colon epithelial cells isolated from donors and Colo205 cells were treated with mild thermal stress at 39.5°C for 6 hours in vitro and cell surface levels of MICA and HLA-A, B, C were quantified by flow cytometry. The results are plotted showing means and standard deviations of six samples.
*, p=0.0002 compared to the corresponding normothermic group using unpaired t test with Welch's correction
Discussion
The initial data presented here (Fig. 1) provides some additional descriptive evidence that following systemic heating in vivo, tumor cell apoptosis increases (Fig. 1a and Fig. 1b) and, in a different tumor model, that there is an increase in the presence of NK cells, as detected by the marker NKp46+ cells within the tumor microenvironment. (Fig 1c and Fig 1d). NKp46 has recently been validated as a human NK cell marker in the gut associated tissues, including its association with Innate Lymphoid Cells (ILC) in mice [43]. These observations, combined with our previous studies demonstrating that NK cell cytotoxicity is enhanced by mild heating, provided an impetus to learn more about how mild heating affects tumor cell sensitivity to NK cells. Thus, the major goal of this study was to study effects of mild heating on tumor cell expression of the non-classical MHC-like molecule, MICA, which is a major ligand for NKG2D on NK cells, and more specifically, to whether any increased expression of MICA on the surface of tumor cells following mild heat exposure might be regulated by HSF1.
We demonstrated that downregulation of (mRNA) HSF1 by use of two different siRNAs resulted in decreased HSF1 message, accompanied by downregulation of thermally enhanced, but not endogenous, MICA levels. This confirms that the effect of thermal stress on MICA expression is at the transcriptional level through the activity of HSF1 (Fig 2). Consistent results using two different siRNA constructs support that HSF1 silencing mediated (mRNA) MICA downregulation is not a non-specific, off-target effect (Fig 2a,b). Importantly MICA message downregulation resulted in decreased NK activity against Colo205 tumor cells in vitro (Fig 2c). The observed decrease in NK mediated cytotoxicity with (mRNA) HSF1 siRNA at normothermic conditions suggests a role for HSF1 in NK cell function under normothermic conditions..While a role for other activating ligands that might be present on Colo205 cell surface was not suspected since NKG2D/MICA blocking antibodies were previously shown to block endogenous and thermally enhanced cytotoxicity in this model [19], our data does not exclude a role possible other surface molecules that might be altered with thermal stress.
Promoter reporter assays revealed an upregulation of MICA promoter activity with thermal stress which is dependent on presence of intact HSF1 binding site in the promoter (Fig 3). These results are in agreement with previous studies demonstrating the role of HSF1 binding site in MICA promoter in quiescent HCT116 colon tumor cells with heat shock [32]. However, a correlation between HSF1 mediated transcriptional regulation of the MICA gene at mild thermal stress temperatures has not been previously described. The observed increase in luciferase activity at control temperatures when the HSF1 binding site is mutated, suggests that MICA expression might be suppressed by HSF1 under normothermic conditions. However, these arguments would have been greatly supported by the use of a chromatin immunoprecipitation (ChIP) assay showing direct HSF1 binding to the MICA promoter.
We have previously observed a transient increase in mild thermal stress enhanced NK cell cytotoxicity of Colo205 cells, which regresses to non-significant levels of cytotoxicity compared to control temperatures within 24 hours in vitro (unpublished results). Here we show that thermally enhanced surface MICA expression on cell surface is dependent on sustained MICA synthesis, where disruption leads to faster levels of decay from the cell surface (Fig 4). Our results indicate that MICA cell surface kinetics follow “one-phase exponential decay”, with significantly enhanced MICA levels on the cell surface without cycloheximide. While thermal stress clearly helps to regulate the transcription of MICA, the precise mechanisms by which MICA trafficking to the cell surface might be affected requires further research.. In addition, it is important to remember that shedding of MICA molecules from the tumor cell surface occurs through metalloproteinase activity [44, 45]; however we have not yet addressed this issue under thermal stress conditions.
Figure 4. Cycloheximide inhibits induction of MICA by thermal stress in Colo205 cells.
Colo205 cells were treated with mild thermal stress at 39.5°C (▲, ▼) or at 37°C (◆, ●) with DMSO for 6 hours in vitro, followed by cycloheximide (5µg/ml in the culture medium) (▼, ●) or DMSO, the solvent used for cycloheximide (▲, ◆) at normothermic temperatures. Cell surface MICA expression was detected with flow cytometry.
We also tested whether systemic heating in vivo could up regulate (mRNA) MICA expression, i.e., in Colo205 and HT29 tumor cells growing in mice (Fig 5). We consistently observed an upregulation of MICA message in Colo205 tumors following WBH, averaging a 4.2 fold change compared to tumors in mice maintained at normothermia. While Colo205 tumors in SCID mice show a consistent increase of MICA message levels up to 24 hours following WBH, HT29 cells do not (see also ref. [19]). However, HSP70 upregulation with thermal stress is still intact in HT29 cells, albeit less than Colo205 cells. The role of HSF1 in in regulation of HSP70 and MICA message may vary between different tumor cells and the basis for these differences should be investigated.
Several studies have shown that classical MHC Class I molecule expression on cell surface is the major signal for “self” recognition by the immune system, and is also a major deterrent for NK cell mediated cytotoxicity [46, 47]. Previous reports for endogenous expression of MICA on human colonocytes [11, 48], combined with the importance of HLA expression for limiting NK cell mediated killing, led us to investigate the expression of HLA and MICA levels on colonocytes isolated from human donors and then treated in vitro with hyperthermia. Although we have observed relatively low expression of MICA message in normal colonocytes, our study suggests that mild heat stress does not lead to significant changes in MICA or HLA (A,B,C) levels (Fig 6). This evidence for some specificity of heat stress on MICA expression on tumor cells versus normal cells requires further analysis to test whether there are changes in the transcriptional control of MICA expression during colon cancer progression..
This report has highlighted HSF1 mediated MICA expression on tumor cells as a potential molecular mechanism to explain the enhancement of NK cell cytotoxicity against tumors following mild thermal stress. However there are other studies suggesting alternative regulation pathways for MICA regulation in the literature, mainly through other transcription factors. For example, a recent study shows that NF-κB may also be a transcription factor that controls MICA expression. Lin et al. [49] demonstrated that the TNF-α mediated MICA upregulation on human umbilical vein endothelial cells (HUVECs) is through NF-κB. In this model NF-κB acts on the −130bp of MICA transcription start site, overlapping with HSRE. We also investigated this region, in our study. They found that TNF-α mediated MICA upregulation is inhibited with an inactive form of HSF1 (lacking a transactivation domain). These results further supports our observations. Lin et al. further suggested a competition between NF-κB and HSF1 for the MICA promoter binding site, which is found to be responsive to heat shock (42°C 1hr). However Andresen et al. [50] reported that histone deactylase inhibitors cause an increase in surface MICA/B expression in Jurkat T cells, which is completely abrogated by intracellular calcium depletion, independent of NF-κB but dependent on transcription factor Sp1. They identified −115 to −84 of MICA promoter as the strong regulatory region in Jurkat T cells. In our colon tumor models, we have not determined whether the effect of HSF1 on MICA expression is independent of NF-κB or TNF-α. Luo et al. [51] stated that hypoxia inducible factor (HIF-1) regulates MICA expression in human renal proximal tubular epithelial cells HK-2. This observation of MICA upregulation under hypoxic stress provides further support to our earlier observation [19] of its upregulation under thermal stress. Another transcription factor identified in MICA transcriptional regulation is STAT3 [52]. Studies suggest that STAT3 negatively regulates MICA after it was observed that there was increased expression of MICA following STAT3 inhibition and direct binding of STAT3 on MICA promoter. MICA induction in mesenchymal stem cells after heat shock (45°C, 1 hr) is also prevented with constitutive activation of STAT3, suggesting that STAT3 might also play a role in thermal regulation of MICA upregulation. Clearly, the role of other transcription factors in thermal modulation of NK cell activity requires further investigation.
Overall, the data shown here provides additional support for the notion that mild thermal stress can enhance the activity of immune cells such as NK cells. However, at the present time, there are no clinical studies which have correlated MICA expression on tumor cells with patient survival following hyperthermia treatment and this is clearly an important gap in the field. The studies reported here predict that some patients may benefit from mild hyperthermia treatment through thermally enhanced tumor cell expression of MICA and increased anti-tumor NK cell cytolytic function. However, our data also reveals significant variation among tumor cells in terms of MICA expression following heating, suggesting that not all patients may benefit. Clearly new biomarkers or correlative studies which can link heat-induced changes in NK cell activity, and/or tumor cell sensitivity, could be very helpful in predicting which patients may benefit most by receiving clinical hyperthermia.
Acknowledgements
We are grateful to Dr. Bonnie Hylander for expert advice on immunohistochemical staining and for the critical review of the manuscript, Dr. Hima Bansal for her help on reporter assays, Rose Pitoniak for help and advice on animal studies, Earl Timm for advice on flow cytometry analyses and Katie Kokulos for her help with the manuscript.
This study was supported by Komen Foundation DISS0402487 and Fulbright Scholarships to BED and also NIH P01 CA94045, R01 CA71599, R21 CA098852, Roswell Park Cancer Institute Core grant CA16056.
Abbreviations
- MICA
MHC class I related chain A
- WBH
whole body hyperthermia
- HBSS
Hanks Balanced Salt Solution
- HSF1
heat shock factor 1
- MHC
Major Histocompatibility Complex
- KIR
Killer Inhibitory receptors
- HLA
Human Leukocyte Antigen
- PBMC
Peripheral Blood Mononuclear Cells
Footnotes
Declaration of Interest: The authors report no further declarations of interest.
References
- 1.Herberman RB, et al. Natural cytotoxic reactivity of mouse lymphoid cells against syngeneic and allogeneic tumors. II. Characterization of effector cells. Int J Cancer. 1975;16(2):230–239. doi: 10.1002/ijc.2910160205. [DOI] [PubMed] [Google Scholar]
- 2.Kiessling R, et al. "Natural" killer cells in the mouse. I. Cytotoxic cells with specificity for mouse Moloney leukemia cells. Specificity and distribution according to genotype. Eur J Immunol. 1975;5(2):112–117. doi: 10.1002/eji.1830050208. [DOI] [PubMed] [Google Scholar]
- 3.Glimcher L, et al. Identification of a cell-surface antigen selectively expressed on the natural killer cell. J Exp Med. 1977;145(1):1–9. doi: 10.1084/jem.145.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gryllis C, et al. Increased LAK activity against HIV-infected cell lines in HIV-1+ individuals. Clin Exp Immunol. 1992;89(3):356–361. doi: 10.1111/j.1365-2249.1992.tb06962.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smyth MJ, et al. Tumor necrosis factor-related apoptosis-inducing ligand (TRAIL) contributes to interferon gamma-dependent natural killer cell protection from tumor metastasis. J Exp Med. 2001;193(6):661–670. doi: 10.1084/jem.193.6.661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Garner WL, et al. Human breast cancer and impaired NK cell function. J Surg Oncol. 1983;24(1):64–66. doi: 10.1002/jso.2930240115. [DOI] [PubMed] [Google Scholar]
- 7.Kobayashi H, et al. Role of trans-cellular IL-15 presentation in the activation of NK cell-mediated killing, which leads to enhanced tumor immunosurveillance. Blood. 2005;105(2):721–727. doi: 10.1182/blood-2003-12-4187. [DOI] [PubMed] [Google Scholar]
- 8.Moretta A, et al. P58 molecules as putative receptors for major histocompatibility complex (MHC) class I molecules in human natural killer (NK) cells. Anti-p58 antibodies reconstitute lysis of MHC class I-protected cells in NK clones displaying different specificities. J Exp Med. 1993;178(2):597–604. doi: 10.1084/jem.178.2.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Braud VM, et al. HLA-E binds to natural killer cell receptors CD94/NKG2A, B and C. Nature. 1998;391(6669):795–799. doi: 10.1038/35869. [DOI] [PubMed] [Google Scholar]
- 10.Moretta A, et al. Activating receptors and coreceptors involved in human natural killer cell-mediated cytolysis. Annu Rev Immunol. 2001;19:197–223. doi: 10.1146/annurev.immunol.19.1.197. [DOI] [PubMed] [Google Scholar]
- 11.Bauer S, et al. Activation of NK cells and T cells by NKG2D, a receptor for stress-inducible MICA. Science. 1999;285(5428):727–729. doi: 10.1126/science.285.5428.727. [DOI] [PubMed] [Google Scholar]
- 12.Winter CC, et al. Direct binding and functional transfer of NK cell inhibitory receptors reveal novel patterns of HLA-C allotype recognition. J Immunol. 1998;161(2):571–577. [PubMed] [Google Scholar]
- 13.Garni-Wagner BA, et al. A novel function-associated molecule related to non-MHC-restricted cytotoxicity mediated by activated natural killer cells and T cells. J Immunol. 1993;151(1):60–70. [PubMed] [Google Scholar]
- 14.Shibuya A, et al. DNAM-1, a novel adhesion molecule involved in the cytolytic function of T lymphocytes. Immunity. 1996;4(6):573–581. doi: 10.1016/s1074-7613(00)70060-4. [DOI] [PubMed] [Google Scholar]
- 15.Bottino C, et al. NTB-A [correction of GNTB-A], a novel SH2D1A-associated surface molecule contributing to the inability of natural killer cells to kill Epstein-Barr virus-infected B cells in X-linked lymphoproliferative disease. J Exp Med. 2001;194(3):235–246. doi: 10.1084/jem.194.3.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lopez-Botet M, et al. The CD94/NKG2C-type lectin receptor complex in recognition of HLA class I molecules. Res Immunol. 1997;148(3):155–159. doi: 10.1016/s0923-2494(97)84217-4. [DOI] [PubMed] [Google Scholar]
- 17.Long EO, et al. Killer cell inhibitory receptors: diversity, specificity, and function. Immunol Rev. 1997;155:135–144. doi: 10.1111/j.1600-065x.1997.tb00946.x. [DOI] [PubMed] [Google Scholar]
- 18.Dayanc BE, et al. Dissecting the role of hyperthermia in natural killer cell mediated anti-tumor responses. Int J Hyperthermia. 2008;24(1):41–56. doi: 10.1080/02656730701858297. [DOI] [PubMed] [Google Scholar]
- 19.Ostberg JR, et al. Enhancement of natural killer (NK) cell cytotoxicity by fever-range thermal stress is dependent on NKG2D function and is associated with plasma membrane NKG2D clustering and increased expression of MICA on target cells. J Leukoc Biol. 2007;82(5):1322–1331. doi: 10.1189/jlb.1106699. [DOI] [PubMed] [Google Scholar]
- 20.Bahram S, et al. MIC and other NKG2D ligands: from none to too many. Curr Opin Immunol. 2005;17(5):505–509. doi: 10.1016/j.coi.2005.07.016. [DOI] [PubMed] [Google Scholar]
- 21.Groh V, et al. Cell stress-regulated human major histocompatibility complex class I gene expressed in gastrointestinal epithelium. Proc Natl Acad Sci U S A. 1996;93(22):12445–12450. doi: 10.1073/pnas.93.22.12445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Borchers MT, et al. NKG2D ligands are expressed on stressed human airway epithelial cells. Am J Physiol Lung Cell Mol Physiol. 2006;291(2):L222–L231. doi: 10.1152/ajplung.00327.2005. [DOI] [PubMed] [Google Scholar]
- 23.Gannage M, et al. Induction of NKG2D ligands by gamma radiation and tumor necrosis factor-alpha may participate in the tissue damage during acute graft-versus-host disease. Transplantation. 2008;85(6):911–915. doi: 10.1097/TP.0b013e31816691ef. [DOI] [PubMed] [Google Scholar]
- 24.Armeanu S, et al. Natural killer cell-mediated lysis of hepatoma cells via specific induction of NKG2D ligands by the histone deacetylase inhibitor sodium valproate. Cancer Res. 2005;65(14):6321–6329. doi: 10.1158/0008-5472.CAN-04-4252. [DOI] [PubMed] [Google Scholar]
- 25.Boissel N, et al. BCR/ABL oncogene directly controls MHC class I chain-related molecule A expression in chronic myelogenous leukemia. J Immunol. 2006;176(8):5108–5116. doi: 10.4049/jimmunol.176.8.5108. [DOI] [PubMed] [Google Scholar]
- 26.Cerboni C, et al. Antigen-activated human T lymphocytes express cell-surface NKG2D ligands via an ATM/ATR-dependent mechanism and become susceptible to autologous NK-cell lysis. Blood. 2007;110(2):606–615. doi: 10.1182/blood-2006-10-052720. [DOI] [PubMed] [Google Scholar]
- 27.Eagle RA, et al. Regulation of NKG2D ligand gene expression. Hum Immunol. 2006;67(3):159–169. doi: 10.1016/j.humimm.2006.02.015. [DOI] [PubMed] [Google Scholar]
- 28.Kato N, et al. Regulation of the expression of MHC class I-related chain A, B (MICA, MICB) via chromatin remodeling and its impact on the susceptibility of leukemic cells to the cytotoxicity of NKG2D-expressing cells. Leukemia. 2007;21(10):2103–2108. doi: 10.1038/sj.leu.2404862. [DOI] [PubMed] [Google Scholar]
- 29.Molinero LL, et al. NF-kappa B regulates expression of the MHC class I-related chain A gene in activated T lymphocytes. J Immunol. 2004;173(9):5583–5590. doi: 10.4049/jimmunol.173.9.5583. [DOI] [PubMed] [Google Scholar]
- 30.Rodriguez-Rodero S, et al. Transcriptional regulation of MICA and MICB: a novel polymorphism in MICB promoter alters transcriptional regulation by Sp1. Eur J Immunol. 2007;37(7):1938–1953. doi: 10.1002/eji.200737031. [DOI] [PubMed] [Google Scholar]
- 31.Skov S, et al. Cancer cells become susceptible to natural killer cell killing after exposure to histone deacetylase inhibitors due to glycogen synthase kinase-3-dependent expression of MHC class I-related chain A and B. Cancer Res. 2005;65(23):11136–11145. doi: 10.1158/0008-5472.CAN-05-0599. [DOI] [PubMed] [Google Scholar]
- 32.Venkataraman GM, et al. Promoter region architecture and transcriptional regulation of the genes for the MHC class I-related chain A and B ligands of NKG2D. J Immunol. 2007;178(2):961–969. doi: 10.4049/jimmunol.178.2.961. [DOI] [PubMed] [Google Scholar]
- 33.Schreiner B, et al. Expression of toll-like receptors by human muscle cells in vitro and in vivo: TLR3 is highly expressed in inflammatory and HIV myopathies, mediates IL-8 release and up-regulation of NKG2D-ligands. Faseb J. 2006;20(1):118–120. doi: 10.1096/fj.05-4342fje. [DOI] [PubMed] [Google Scholar]
- 34.Jinushi M, et al. Expression and role of MICA and MICB in human hepatocellular carcinomas and their regulation by retinoic acid. Int J Cancer. 2003;104(3):354–361. doi: 10.1002/ijc.10966. [DOI] [PubMed] [Google Scholar]
- 35.Jinushi M, et al. Autocrine/paracrine IL-15 that is required for type I IFN-mediated dendritic cell expression of MHC class I-related chain A and B is impaired in hepatitis C virus infection. J Immunol. 2003;171(10):5423–5429. doi: 10.4049/jimmunol.171.10.5423. [DOI] [PubMed] [Google Scholar]
- 36.Pritchard MT, et al. Protocols for simulating the thermal component of fever: preclinical and clinical experience. Methods. 2004;32(1):54–62. doi: 10.1016/s1046-2023(03)00187-7. [DOI] [PubMed] [Google Scholar]
- 37.Sistonen L, et al. Human heat shock factors 1 and 2 are differentially activated and can synergistically induce hsp70 gene transcription. Mol Cell Biol. 1994;14(3):2087–2099. doi: 10.1128/mcb.14.3.2087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fionda C, et al. Heat shock protein-90 inhibitors increase MHC class I-related chain A and B ligand expression on multiple myeloma cells and their ability to trigger NK cell degranulation. J Immunol. 2009;183(7):4385–4394. doi: 10.4049/jimmunol.0901797. [DOI] [PubMed] [Google Scholar]
- 39.Murapa P, et al. Physiological fever temperature induces a protective stress response in T lymphocytes mediated by heat shock factor-1 (HSF1) J Immunol. 2007;179(12):8305–8312. doi: 10.4049/jimmunol.179.12.8305. [DOI] [PubMed] [Google Scholar]
- 40.Mohammadpour HA. Isolation and culture of human colon epithelial cells using a modified explant technique employing a noninjurious approach. Methods Mol Med. 2005;107:237–247. doi: 10.1385/1-59259-861-7:237. [DOI] [PubMed] [Google Scholar]
- 41.Burd R, et al. Tumor cell apoptosis, lymphocyte recruitment and tumor vascular changes are induced by low temperature, long duration (fever-like) whole body hyperthermia. J Cell Physiol. 1998;177(1):137–147. doi: 10.1002/(SICI)1097-4652(199810)177:1<137::AID-JCP15>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]
- 42.Loo DT, et al. Measurement of cell death. Methods Cell Biol. 1998;57:251–264. doi: 10.1016/s0091-679x(08)61583-6. [DOI] [PubMed] [Google Scholar]
- 43.Tomasello E, et al. Mapping of NKp46(+) Cells in Healthy Human Lymphoid and Non-Lymphoid Tissues. Front Immunol. 3:344. doi: 10.3389/fimmu.2012.00344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kaiser BK, et al. Disulphide-isomerase-enabled shedding of tumour-associated NKG2D ligands. Nature. 2007;447(7143):482–486. doi: 10.1038/nature05768. [DOI] [PubMed] [Google Scholar]
- 45.Salih HR, et al. Cutting edge: down-regulation of MICA on human tumors by proteolytic shedding. J Immunol. 2002;169(8):4098–4102. doi: 10.4049/jimmunol.169.8.4098. [DOI] [PubMed] [Google Scholar]
- 46.Ljunggren HG, et al. In search of the 'missing self': MHC molecules and NK cell recognition. Immunol Today. 1990;11(7):237–244. doi: 10.1016/0167-5699(90)90097-s. [DOI] [PubMed] [Google Scholar]
- 47.Gorelik E, et al. H-2 antigen expression and sensitivity of BL6 melanoma cells to natural killer cell cytotoxicity. J Immunol. 1988;140(6):2096–2102. [PubMed] [Google Scholar]
- 48.Perera L, et al. Expression of nonclassical class I molecules by intestinal epithelial cells. Inflamm Bowel Dis. 2007;13(3):298–307. doi: 10.1002/ibd.20026. [DOI] [PubMed] [Google Scholar]
- 49.Lin D, et al. NF-kappaB regulates MICA gene transcription in endothelial cell through a genetically inhibitable control site. J Biol Chem. 2012;287(6):4299–4310. doi: 10.1074/jbc.M111.282152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Andresen L, et al. Molecular regulation of MHC class I chain-related protein A expression after HDAC-inhibitor treatment of Jurkat T cells. J Immunol. 2007;179(12):8235–8242. doi: 10.4049/jimmunol.179.12.8235. [DOI] [PubMed] [Google Scholar]
- 51.Luo L, et al. The role of HIF-1 in up-regulating MICA expression on human renal proximal tubular epithelial cells during hypoxia/reoxygenation. BMC Cell Biol. 11:91. doi: 10.1186/1471-2121-11-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bedel R, et al. Novel role for STAT3 in transcriptional regulation of NK immune cell targeting receptor MICA on cancer cells. Cancer Res. 2011;71(5):1615–1626. doi: 10.1158/0008-5472.CAN-09-4540. [DOI] [PubMed] [Google Scholar]