Abstract
OBJECTIVE
To determine the effect of soy germ pasta enriched in biologically active isoflavone aglycons on gastric emptying in type 2 diabetic patients with gastroparesis.
RESEARCH DESIGN AND METHODS
This randomized double-blind, placebo-controlled study compared soy germ pasta with conventional pasta for effects on gastric emptying. Patients (n = 10) with delayed gastric emptying consumed one serving per day of each pasta for 8 weeks, with a 4-week washout. Gastric emptying time (t1/2) was measured using the [13C]octanoic acid breath test at baseline and after each period, and blood glucose and insulin concentrations were determined after oral glucose load.
RESULTS
Soy germ pasta significantly accelerated the t1/2 in these patients (161.2 ± 17.5 min at baseline vs. 112.6 ± 11.2 min after treatment, P = 0.009). Such change differed significantly (P = 0.009) from that for conventional pasta (153.6 ± 24.2 vs. 156.2 ± 27.4 min), without affecting glucose or insulin concentrations.
CONCLUSIONS
These findings suggest that soy germ pasta may offer a simple dietary approach to managing diabetic gastropathy.
Gastroparesis is a symptomatic chronic debilitating disorder of the stomach, characterized by delayed gastric emptying of solid and semisolid foods in the absence of mechanical obstruction. It affects 30–50% of patients with long-standing type 2 diabetes (T2D) (1,2) and is associated with upper gastrointestinal symptoms. It compromises the pharmacokinetics of orally administered drugs by altering rates of absorption and can also alter glycemia control. The withdrawal of the prokinetic cisapride (3) has compromised therapeutic options (4,5). Interestingly, dietary modifications have been suggested to potentially represent an alternative to drugs for diabetic gastroparesis (2). Our objective was to evaluate a novel soy germ pasta containing biologically active isoflavone aglycons (6,7) for effects on gastric emptying in T2D patients with gastroparesis.
RESEARCH DESIGN AND METHODS
This randomized, double-blind, placebo-controlled crossover study enrolled 10 adults (5 male and 5 female; mean ± SEM 62.7 ± 2.3 years of age; BMI 28.8 ± 1.0 kg/m2; HbA1c 64 mmol/mol) with T2D and delayed gastric emptying (t1/2 range 134–253 min; normal range <120 min). None had major complications of diabetes and all were maintained on a standard diabetes diet for >6 months and throughout the study. Prior use of medications that affect gastric emptying, soy-based products, or supplements and a history of gastrointestinal or liver disease were exclusion criteria. The study was conducted with informed consent and approved by the Human Ethics Committee of the University of Perugia School of Medicine.
Patients were randomized to two groups. One group (n = 5) consumed one serving per day of soy germ–enriched pasta (80 g) followed by conventional pasta for 8 weeks, with a 4-week washout between. The other group (n = 5) consumed these pastas in reverse sequence. The two pastas were indistinguishable. The composition of the soy germ pasta (Aliveris S.r.l., Perugia, Italy), which contained 2% soy germ, delivering 31–33 mg isoflavones per serving, is described elsewhere (6). At baseline, blood was collected after fasting and 30, 60, 90, and 120 min after a standard meal for measurement of plasma glucose and serum insulin by standard methods. The next day, gastric emptying time was measured using the [13C]octanoic acid breath test (8,9). These tests were repeated after 8, 12, and 20 weeks, and the severity of symptoms of gastroparesis was also assessed using the Gastroparesis Cardinal Symptom Index (GCSI) questionnaire (10). Methods and data analysis are described in more detail in the Supplementary Data.
RESULTS
Compliance to soy germ pasta was confirmed by an elevated mean plasma isoflavone concentration of 68 ± 9 ng/mL (11), and for conventional pasta from counting of returned packages.
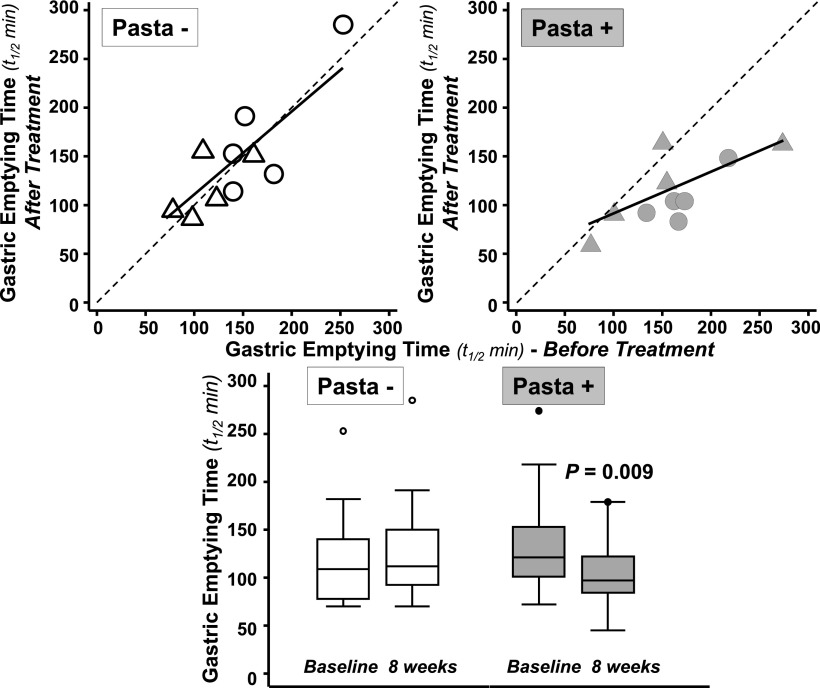
Figure 1 shows individual t1/2 values for gastric emptying measured at baseline and after consuming both pastas. No period, sequence, or washout effects were observed. The inclusion of soy isoflavone–enriched pasta to the standard American Diabetes Association (ADA) diet led to a significant acceleration in mean (±SEM) t1/2 in the 10 patients when compared with baseline values (t1/2 = 161.2 ± 17.5 vs. 112.6 ± 11.2 min, P = 0.009; P = 0.109 for the analysis limited to pairwise comparison of data from the end of each period). The regression coefficient for individual t1/2 values before and after soy germ pasta (0.478 [95% CI 0.134–0.822]; R2 = 0.562; P < 0.013) lies well below unity, indicating a substantial reduction of the t1/2 (Fig. 1). These findings are consistent with results from the crossover analysis, indicating that soy germ pasta improves gastric emptying time irrespective of the order in which it was given. By contrast, there was no significant difference in the group mean t1/2 values when conventional pasta lacking isoflavones was consumed (153.6 ± 24.2 vs. 156.2 ± 27.4 min, P = 0.76).
Figure 1.
Relationship between gastric emptying time (t1/2) in 10 patients with documented diabetic gastroparesis measured at baseline and after consuming soy germ pasta containing isoflavone aglycons and conventional pasta lacking isoflavones. The dotted line in the upper plots denotes no change after consuming pasta. Data points below this line indicate reduced gastric emptying time. The solid lines show the regression line of values after treatment on those before treatment during enriched pasta (Pasta+) or control pasta (Pasta−) feeding. Gray and hollow circles denote the data measured on entry into this crossover study and after the first pasta treatment (to be enrolled, these patients had to show a baseline emptying time >120 min); gray and hollow triangles denote values measured after the washout period, i.e., before and after the other pasta treatment. The lower plot (box plots) shows the distribution of gastric emptying times before and after 8-week treatment with the two pastas.
No statistical differences from baseline, or between the two pastas, were observed for the plasma glucose and insulin responses to a standard meal (Supplementary Table 1).
No statistical difference was observed in the GCSI scores between responses to the two pastas at crossover analysis, or in the analysis limited to pairwise comparison of data from the end of each study period. However, the median (range) total GCSI score was 8 (2–13) at baseline, and this significantly decreased to 5 (0–7) (P = 0.039) for the soy germ pasta group. The corresponding values for conventional pasta were 7 (0–21) and 6 (0–11) (P = 0.289), respectively.
CONCLUSIONS
The major findings of this pilot study of T2D patients with gastroparesis were that the inclusion of an isoflavone-enriched soy germ pasta on the background of an ADA diet led to a significant acceleration in the rate of gastric emptying, whereas conventional pasta lacking isoflavones had no effect.
The gastric emptying time measured on baseline conditions (either before or after the washout period) was longer (P = 0.073) than the upper limit of normal (120 min) (8,9) and consistent with delayed gastric emptying, even though the patients reported only mild symptomatology.
Concerns that accelerating gastric emptying could potentially lead to increased glycemia (12–14) were not supported from measurements of plasma glucose or insulin concentrations in response to a standard meal after normalization of the t1/2 by soy germ pasta. This is presumably because these patients adhered to an ADA maintenance diet, were not taking drugs, and were all in good glycemic control.
Although not the primary objective of our study, and not surprising given the relatively low baseline GCSI scores and small sample size, we found only a minor improvement in the severity of upper gastrointestinal symptoms after an improvement in t1/2. A larger study of patients with more severe symptoms would better address the effectiveness of soy germ pasta on symptomatology.
We speculate that isoflavones, when in contact with gastric mucosa, influence prostaglandin synthesis to modulate motility. Gene expression data from gastric mucosal biopsies of healthy adults has shown that soy germ pasta significantly alters the expression of many genes involved in gastric function. PTDGS, a gene encoding prostaglandin D2 synthase, the enzyme responsible for prostaglandin F2α synthesis, was upregulated fivefold by soy germ pasta (S.A., K.D.R.S., C.C., 2012, unpublished data).
In conclusion, pasta enriched with biologically active isoflavone aglycons improved gastric emptying time in T2D patients, warranting consideration of this dietary intervention in the management of diabetic gastroparesis, especially given that there is currently no effective pharmacologic therapy.
Supplementary Material
Acknowledgments
K.D.R.S. and C.C. disclose financial interests in Aliveris S.r.l. No other potential conflicts of interest relevant to this article were reported.
K.D.R.S. and C.C. were the principal investigators, conceived and designed the study, and prepared the manuscript with support from the coauthors. E.N., D.C., and G.P. were responsible for recruitment, enrollment, and clinical care of the patients and performed the clinical and biochemical tests and data collection and processing. P.-M.B. performed the statistical analysis of data. S.A. performed the clinical and biochemical tests and data collection and processing. All authors reviewed the manuscript. K.D.R.S. and C.C. are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
The authors acknowledge Dr. Alessia Gherardi and Dr. Emanuela Floridi (University of Perugia) for assistance with clinical tests performed and the support of Aliveris S.r.l. and Bianconi (Bastardo, Umbria, Italy) for providing the soy germ pasta and conventional pasta used in this study.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc12-1615/-/DC1.
S.A. is currently affiliated with the Department of Oncological Sciences, Mount Sinai School of Medicine, New York, New York.
References
- 1.Horowitz M, Harding PE, Maddox AF, et al. Gastric and oesophageal emptying in patients with type 2 (non-insulin-dependent) diabetes mellitus. Diabetologia 1989;32:151–159 [DOI] [PubMed]
- 2.Horowitz M, O'Donovan D, Jones KL, Feinle C, Rayner CK, Samsom M. Gastric emptying in diabetes: clinical significance and treatment. Diabet Med 2002;19:177–194 [DOI] [PubMed]
- 3.Henney JE. From the Food and Drug Administration: withdrawal of troglitazone and cisapride. JAMA 2000;283:222810807369 [Google Scholar]
- 4.Parkman HP, Hasler WL, Fisher RS; American Gastroenterological Association. American Gastroenterological Association technical review on the diagnosis and treatment of gastroparesis. Gastroenterology 2004;127:1592–1622 [DOI] [PubMed]
- 5.Parkman HP, Hasler WL, Fisher RS; American Gastroenterological Association. American Gastroenterological Association medical position statement: diagnosis and treatment of gastroparesis. Gastroenterology 2004;127:1589–1591 [DOI] [PubMed]
- 6.Clerici C, Setchell KDR, Battezzati PM, et al. Pasta naturally enriched with isoflavone aglycons from soy germ reduces serum lipids and improves markers of cardiovascular risk. J Nutr 2007;137:2270–2278 [DOI] [PubMed] [Google Scholar]
- 7.Clerici C, Nardi E, Battezzati PM, et al. Novel soy germ pasta improves endothelial function, blood pressure, and oxidative stress in patients with type 2 diabetes. Diabetes Care 2011;34:1946–1948 [DOI] [PMC free article] [PubMed]
- 8.Ghoos YF, Maes BD, Geypens BJ, et al. Measurement of gastric emptying rate of solids by means of a carbon-labeled octanoic acid breath test. Gastroenterology 1993;104:1640–1647 [DOI] [PubMed]
- 9.Perri F, Ghoos YF, Maes BD, Geypens BJ, Ectors N, Geboes K, et al. Gastric emptying and Helicobacter pylori infection in duodenal ulcer disease. Dig Dis Sci 1996;41:462–468 [DOI] [PubMed]
- 10.Revicki DA, Rentz AM, Dubois D, et al. Development and validation of a patient-assessed gastroparesis symptom severity measure: the Gastroparesis Cardinal Symptom Index. Aliment Pharmacol Ther 2003;18:141–150 [DOI] [PubMed]
- 11.Setchell KDR, Cole SJ. Method of defining equol-producer status and its frequency among vegetarians. J Nutr 2006;136:2188–2193 [DOI] [PubMed]
- 12.Horowitz M, Cunningham KM, Wishart JM, Jones KL, Read NW. The effect of short-term dietary supplementation with glucose on gastric emptying of glucose and fructose and oral glucose tolerance in normal subjects. Diabetologia 1996;39:481–486 [DOI] [PubMed]
- 13.Schvarcz E, Palmer M, Aman J, Horowitz M, Stridsberg M, Berne C. Physiological hyperglycemia slows gastric emptying in normal subjects and patients with insulin-dependent diabetes mellitus. Gastroenterology 1997;113:60–66 [DOI] [PubMed]
- 14.Jones KL, Russo A, Stevens JE, Wishart JM, Berry MK, Horowitz M. Predictors of delayed gastric emptying in diabetes. Diabetes Care 2001;24:1264–1269 [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.