Abstract
OBJECTIVE
To evaluate the effect of type 2 diabetes on the clinical course and prognosis of women with ST-segment elevation myocardial infarction (STEMI) and diabetes.
RESEARCH DESIGN AND METHODS
A total of 26,035 consecutive patients with STEMI who were hospitalized in 456 hospitals in Poland during 1 year were analyzed. The data were obtained from the Polish Registry of Acute Coronary Syndromes (PL-ACS).
RESULTS
Type 2 diabetes occurred more frequently in women than in men (28 vs. 16.6%; P < 0.0001). The proportion of women was larger among patients with diabetes (47.1 vs. 31.3%; P < 0.0001), and compared with women without diabetes, diabetic women had worse clinical profiles. Women with diabetes were most frequently treated conservatively. Both women and men with diabetes had significantly more advanced atherosclerotic lesions than women without diabetes. Women with diabetes had the highest in-hospital, 6-month, and 1-year mortality rates. Multivariate analysis indicated that type 2 diabetes was a significant independent risk factor for in-hospital and 1-year mortality in women with STEMI. Primary percutaneous coronary intervention (pPCI) was a significant factor associated with the decreased 1-year mortality in women without diabetes.
CONCLUSIONS
Type 2 diabetes was a significant independent risk factor for in-hospital and 1-year mortality in women with STEMI. Women with diabetes had the poorest early and 1-year prognoses after STEMI when compared with women without diabetes and men with diabetes. Although pPCI improves the long-term prognosis of women with diabetes, it is used less frequently than in women without diabetes or men with diabetes.
The increasing prevalence of type 2 diabetes represents a strong and independent coronary risk factor that increases cardiovascular morbidity and mortality—a leading cause of death among patients with type 2 diabetes. The available evidence indicates that cardiovascular disease develops significantly more frequently and markedly earlier in patients with diabetes than among patients without type 2 diabetes. It is well known that the risk of coronary artery disease in the general population of middle-aged men is 2.5-fold higher than in women, who develop cardiovascular disease ∼10 years later (1). A number of studies have shown that type 2 diabetes–related increases in cardiovascular risk are greater in women than in men (2,3). However, some researchers have questioned the reversal of the female advantage in populations with diabetes, especially after adjusting for classic coronary risk factors (4). Type 2 diabetes not only increases the risk of acute coronary syndrome (ACS) but also significantly aggravates the course of myocardial infarction and worsens the prognosis, as shown in a number of randomized and observational studies. Recent progress in thrombolytic treatment and primary percutaneous coronary intervention (pPCI) has significantly improved the prognoses of patients with ST-segment elevation myocardial infarction (STEMI). However, despite technological advances in myocardial revascularization and treatment, the mortality among patients with diabetes with ACS is still significantly higher, especially among women, compared with patients without diabetes. Although patients with diabetes make up a significant proportion of patients with STEMI, clinical studies relatively rarely address differences in the course of myocardial infarction in patients with diabetes, and even less often in women with diabetes. This may be a result of the generally insufficient participation of women (at most, 30% of the study population in the last century) in the majority of significant trials; this underrepresentation has influenced the formulation of the currently available standards and guidelines (5–7). Therefore, national registries provide valuable information on the true scale of the problem in any given country. The Polish Registry of Acute Coronary Syndromes (PL-ACS) (8) contains unique data that are useful for epidemiological analysis and provide information regarding various treatment strategies and their efficacy in the population of Polish women with type 2 diabetes and ACS. Therefore, an analysis of the clinical differences and prognoses of these high-risk patients with STEMI is warranted.
RESEARCH DESIGN AND METHODS
We analyzed data from 26,035 patients with STEMI admitted consecutively to 456 hospitals in Poland between 1 June 2005 and 31 May 2006. The data on their hospitalization were obtained from the PL-ACS. The registry’s methodology and an analysis of the first 100,193 patients have been previously described (8). In brief, the PL-ACS registry is an ongoing, nationwide, multicenter, prospective, observational study of consecutively hospitalized Polish patients representing the entire ACS spectrum. The registry is a joint initiative of the Silesian Center for Heart Diseases and the Polish Ministry of Health. A detailed protocol with inclusion and exclusion criteria, methods and logistics, and definitions of all of the fields in the registry dataset was prepared before the registry was started. All admitted patients with suspected ACS were screened for their eligibility to enter the registry, but they were not enrolled until ACS was confirmed. STEMI was defined as the presence of both 1) ST-segment elevation consistent with an infarction of ≥2 mm in the contiguous chest leads and/or ST-segment elevation of ≥1 mm in two or more standard leads or new left bundle branch block and 2) positive cardiac necrosis markers. The skilled physicians who were in charge of each individual patient collected the data. Internal checks for missing or conflicting data and values markedly out of the expected range were implemented using the registry software. In the Silesian Centre for Heart Diseases data management and analysis center, further edit checks were applied if necessary. The exact dates of deaths from all causes were obtained from the official mortality records of the National Health Fund. The vital status at 12 months after the STEMI was available for all of the patients who were included in this analysis.
According to protocol, patients with diabetes were identified as those with known (treated or not) type 2 diabetes prior to admission or with type 2 diabetes diagnosed during hospitalization (except transient glucose intolerance in relation to ACS). The distinction between new-onset diabetes and transient glucose intolerance in relation to ACS was left to the judgment of the attending physician with respect to the current guidelines. No patients were routinely screened for the presence of diabetes at discharge. We compared baseline clinical characteristics, treatment strategy, pharmacotherapy, and outcomes among women with and without type 2 diabetes and men with diabetes, with a special focus on the impact of the treatment strategy on early and 12-month mortality. Multivariate analysis in the entire study population of women was performed to assess the effect of type 2 diabetes on in-hospital and 12-month mortality. Additionally, multivariate analysis was performed separately in women with diabetes. The variables included in the multivariate analyses were the following: age, arterial hypertension, hypercholesterolemia, smoking, obesity, anterior myocardial infarction, sudden cardiac arrest prior to admission, previous myocardial infarction, Killip class upon admission, multivessel coronary disease, and reperfusion strategy.
Statistical analysis
Continuous variables are reported as mean ± SD or median and interquartile range, as appropriate. Categorical variables are expressed as numbers (percentages). Student t tests or, when the assumption of normality was violated, Mann-Whitney U tests were used for the comparison of continuous variables. For the comparison of categorized variables, the χ2 test was used. Follow-up mortality was analyzed using the Kaplan-Meier method, and the differences between groups were compared with log-rank tests. In the multivariate analyses, a multivariate logistic regression was used for in-hospital mortality, and multivariate Cox proportional hazards regression model was used for 12-month mortality. The results of these analyses are presented as odds ratios or hazard ratios with 95% CIs. A two-sided P value ≤0.05 was considered significant. For all calculations, STATISTICA 7.1 software (StatSoft, Inc., Tulsa, OK) was used.
RESULTS
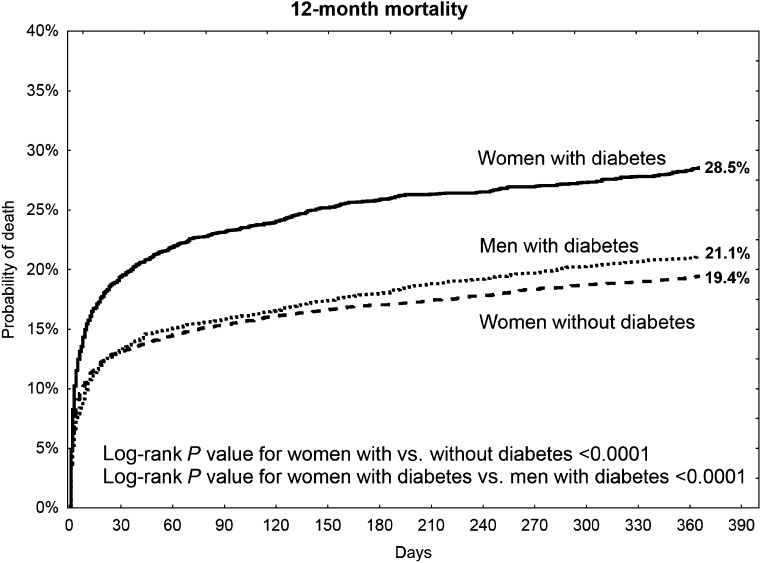
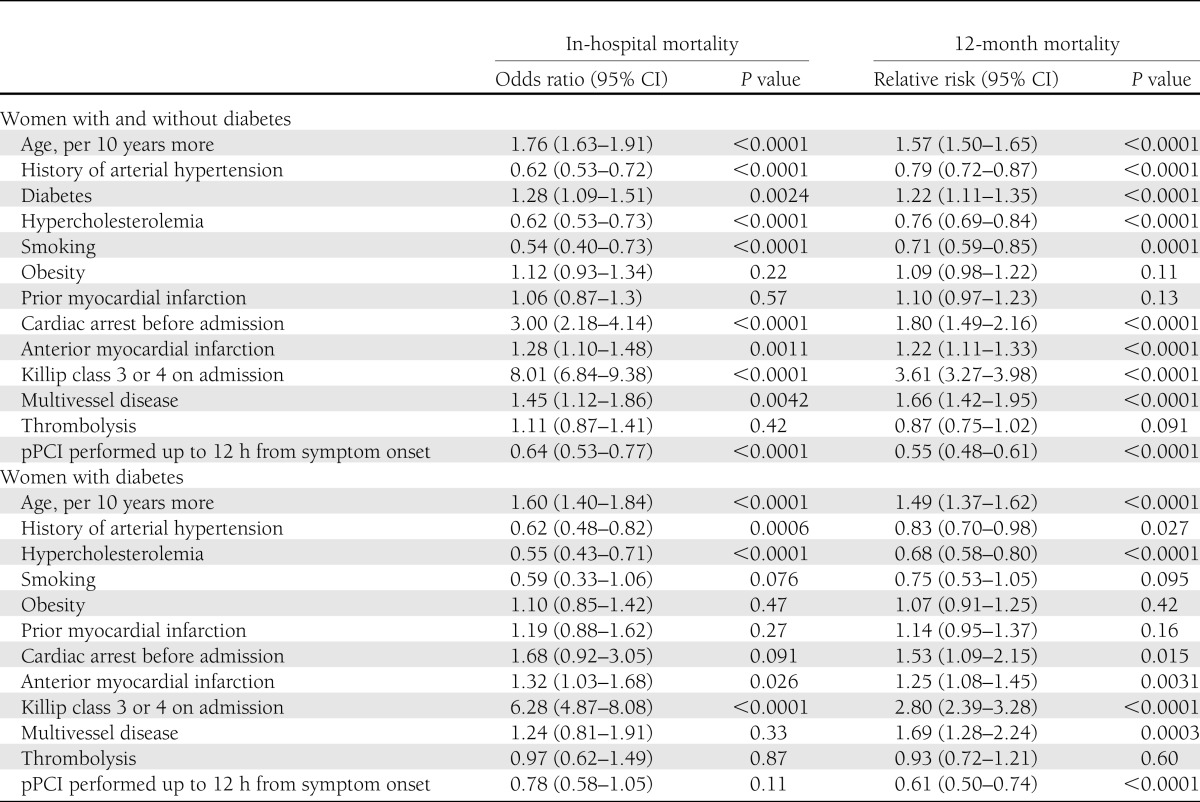
Among the STEMI patients, type 2 diabetes occurred in 5,346 (20.5%) subjects and was significantly more frequent in women than in men (28 vs. 16.6%; P < 0.0001). The proportion of women was larger among patients with diabetes than among patients without diabetes (47.1 vs. 31.3%; P < 0.0001). Women with diabetes were older by a mean of 2.7 years than women without diabetes and by a mean of 6.2 years than men with diabetes. Among women with STEMI, type 2 diabetes was predominant in the age range of 60–90 years, whereas women without diabetes were observed more often in the age-groups of 20–60 and >90 years. Women with diabetes had worse clinical profiles (versus women without diabetes), including significantly more frequent arterial hypertension, hypercholesterolemia, obesity, and previous myocardial infarction. However, they were less frequent smokers. Compared with men with diabetes, they more frequently had arterial hypertension and obesity, whereas men were significantly more frequent smokers and had more previous myocardial infarctions (Table 1). Women with diabetes were more frequently admitted to noncardiology wards, and their hospitalization lasted 1 day longer on average. They were significantly less frequently admitted within the first 3 h after onset of chest pain, with the longest delay to admission being >12 h out of the large number of women. The presence of type 2 diabetes was associated with a worse course of myocardial infarction in women. They were more frequently admitted with cardiogenic shock and pulmonary edema, more often developed in-hospital cardiac arrest, and more often had lower left ventricular ejection fractions. Compared with men with diabetes, women with diabetes more frequently had pulmonary edema and in-hospital cardiac arrest but less frequently had out-of-hospital cardiac arrest. During hospitalization, atrial fibrillation was relatively more frequent in women with diabetes, and these women had the highest heart rate compared with the other analyzed groups. Compared with women without diabetes and men with diabetes, women with diabetes underwent coronary angiography the least often. Among patients without diabetes, atherosclerotic lesions were significantly less severe in women than in men (more frequently had normal coronary arteries and single-vessel disease and less frequently had double-vessel or multivessel disease). In women, the use of a conservative strategy was the most frequent, whereas invasive strategies, including pPCI, were least frequently used. Stent implantation percentages were similar in all study groups. There were no significant differences in the frequency of thrombolytic treatment. The presence of type 2 diabetes in women was associated with increased onset-to-needle time by 30 min on average and increased onset-to-balloon time by 18 min. There were no between-group differences in thrombolysis in myocardial infarction (TIMI) grade flow prior to PCI. In women with diabetes, TIMI flow grade 0 after PCI was more frequent than in women without diabetes. During hospitalization, women with diabetes were more frequently treated with acetylsalicylic acid, heparins, β-blockers, calcium (Ca) blockers, statins, ACE inhibitors (ACE-i), nitrates, diuretics, and insulin, but they less often received thienopyridines or clopidogrel than women without diabetes. Compared with men with diabetes, women with diabetes less frequently received thienopyridine derivatives (ticlopidine and clopidogrel), unfractionated heparin, β-blockers, or statins, but they more often received low-molecular-weight heparin (LMWH), Ca blockers, nitrates, diuretics, and insulin. At discharge, women with diabetes were less often prescribed thienopyridines in general or clopidogrel and were more frequently prescribed acetylsalicylic acid, statins, ACE-i, Ca blockers, nitrates, and diuretics, compared with women without diabetes. Compared with men with diabetes, they received thienopyridines, clopidogrel, β-blockers, and statins significantly less often but more frequently received Ca blockers and nitrates. Women with diabetes had the poorest early and 12-month prognoses and the highest in-hospital, 6-month, and 1-year mortality rates. Survival at 1 year after a myocardial infarction was lowest in women with diabetes; only 71.5% survived, compared with 80.6% of women without diabetes and 78.9% of men with diabetes (Table 1 and Fig. 1). Analysis of the impact of treatment strategy on early and 12-month mortality indicated that, regardless of the method of treatment, women with diabetes had higher mortality rates when compared with women without diabetes. However, an invasive strategy was associated with the lowest early and 12-month mortality rates in both study groups (Table 2). In multivariate analysis, type 2 diabetes was a significant independent predictor of higher in-hospital and 12-month mortality in women with STEMI (Table 3). Factors that increased the risk of both early and 12-month mortality in women with diabetes included age, cardiogenic shock or pulmonary edema on admission, and anterior myocardial infarction. Multivessel coronary disease was a significant risk factor for 1-year mortality in women with diabetes. Primary PCI was significantly associated with lower 1-year mortality in women with diabetes.
Table 1.
Baseline characteristics, treatment strategy, and outcomes in women with and without diabetes and in men with diabetes
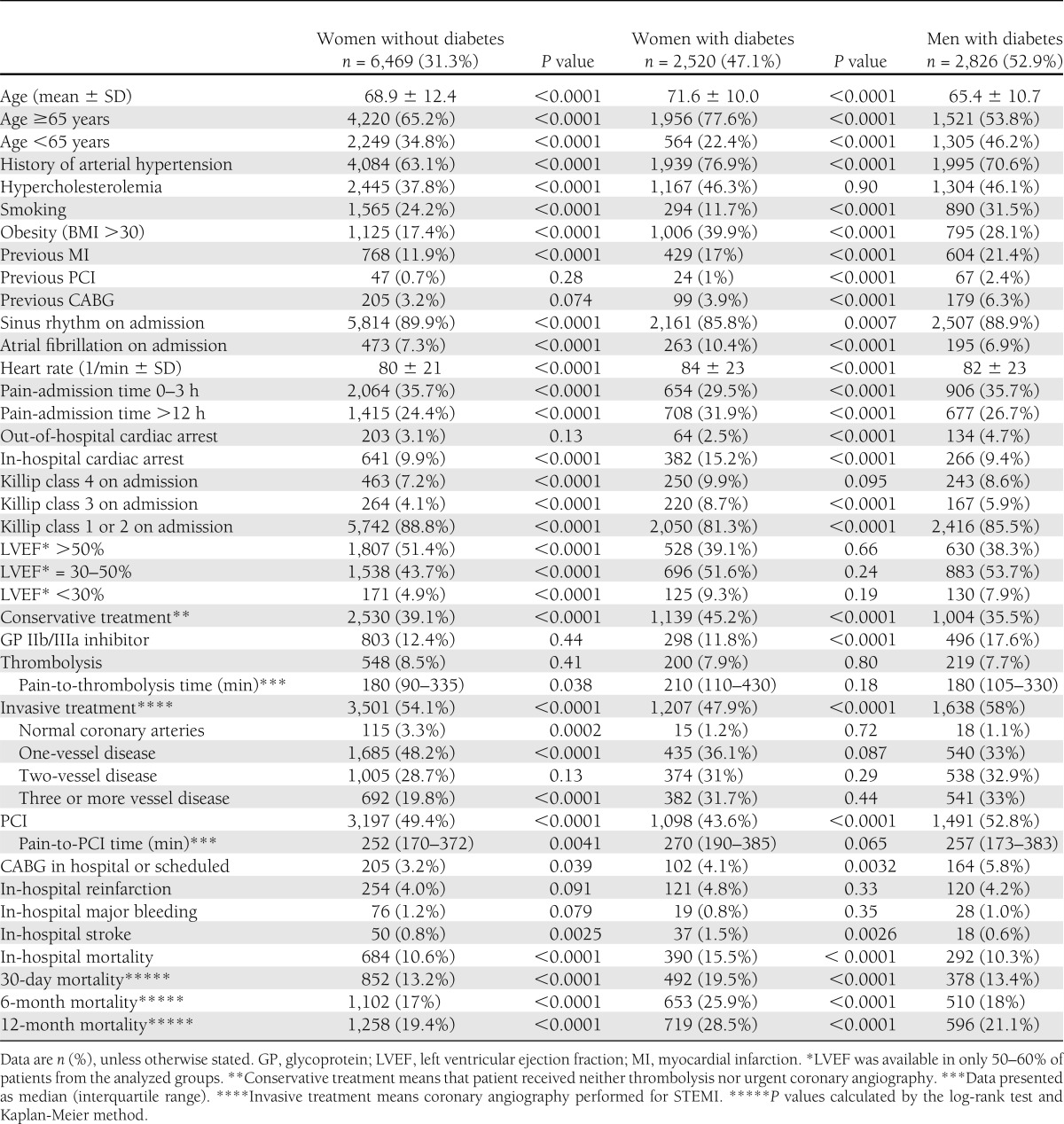
Figure 1.
One-year mortality in women with and without diabetes and in men with diabetes.
Table 2.
Early and 12-month mortality in women with and without diabetes depending on treatment strategy
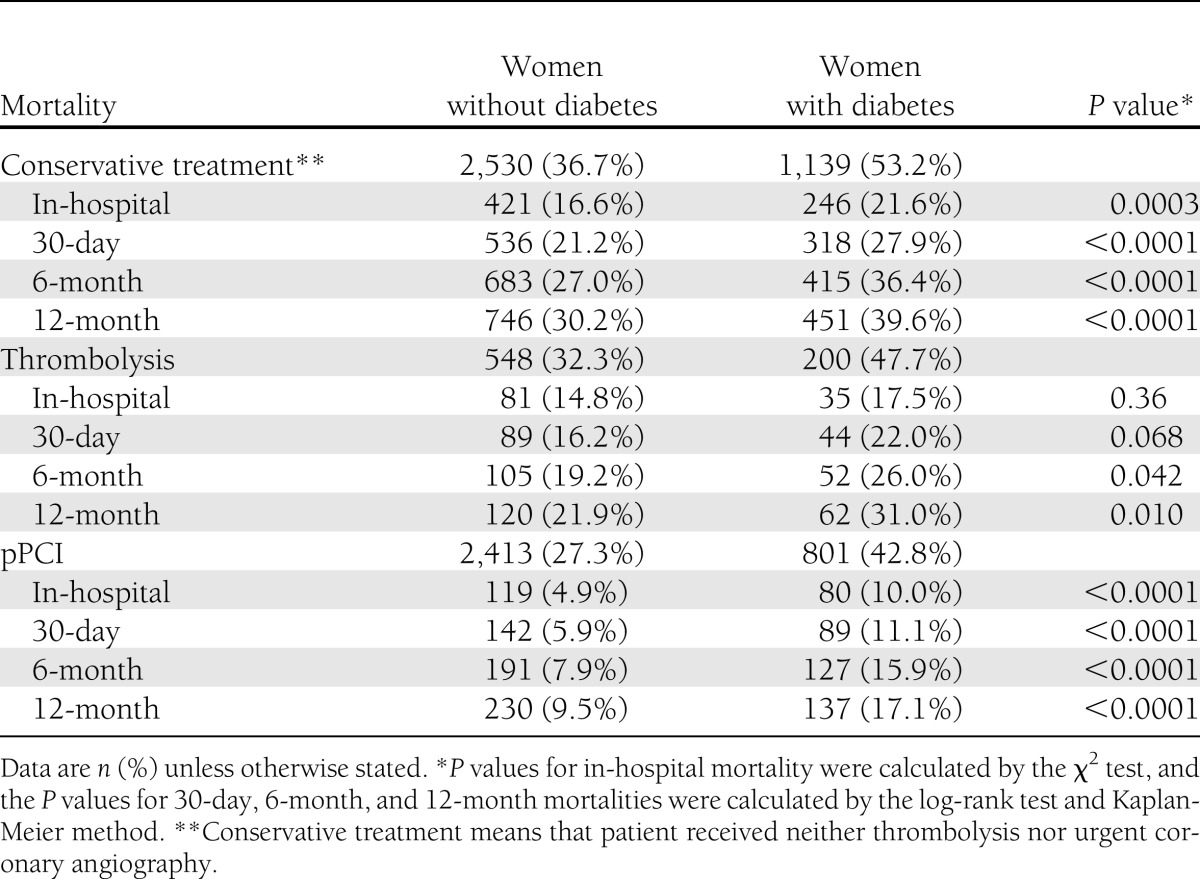
Table 3.
Multivariate analysis of early and 12-month mortality in women and in the subgroup of women with diabetes
CONCLUSIONS
In the PL-ACS registry, the percentage of patients with diabetes among patients with STEMI (20.5%) is comparable with the percentages in other registries including type 2 diabetes, which was identified in 19–23% of patients with ACS (2) and in 21% of patients with STEMI in the Global Registry of Acute Coronary Events (GRACE) and the Euro Heart Survey of Acute Coronary Syndromes (EHS-ACS), respectively (6,9,10). The increased percentage of type 2 diabetes in women compared with men with coronary artery disease and the higher proportion of women among patients with diabetes compared with patients without diabetes were comparable with the results of other investigators (6,7). Previous analysis of the PL-ACS data (11) revealed that type 2 diabetes is a significant independent factor for in-hospital and 1-year survival among women with STEMI. Women with diabetes had the worst early and 12-month outcomes after myocardial infarction when compared with other patient subgroups. Women with diabetes had undoubtedly worse clinical profiles, which is in accord with the results of most of the studies performed in patients with myocardial infarction and type 2 diabetes (6,7,12–14). The observation that the prevalence of type 2 diabetes increases with age and then declines, likely due to premature death as a result of early type 2 diabetes complications (15), is concordant with our analysis of the age structures in women with and without diabetes. For our population, increasingly high prevalences of obesity and arterial hypertension and decreasing rates of smoking typically do occur with age (16–18). Surprisingly, in the multivariate analysis of women with STEMI, none of the known risk factors except for age was a significant predictor of mortality, irrespective of type 2 diabetes. Nonetheless, similar paradoxes have already been reported (19–21). Taking into account the unquestionable benefits of reperfusion therapy for STEMI in patients with diabetes, one of the reasons for their poorer prognoses may be the fact that women with diabetes, despite their complex profiles, are “discriminated against” regarding the use of modern medical treatments. The registry indicated that as many as 45.2% of women with diabetes received only conservative treatment and that they were significantly less frequently selected for coronary angiography and pPCI. The fact that every second woman was not offered any reperfusion therapy likely led to significant clinical implications and resulted in the poorer prognosis of this group. The time delays from the onset of symptoms to admission and from admission to treatment and hospitalization in a noncardiology ward have been reported to be responsible for the large discrepancy in the use of treatment strategies (22–25). Against recommendations, paradoxically, a less frequent use of reperfusion therapy in patients with diabetes was noted in many of the earlier registries than in studies performed in the fibrinolysis era or after the introduction of modern invasive treatments (6,9,26,27). Unfortunately, most of these studies did not contain separate information on women with diabetes. Our multivariate analysis indicated that pPCI within 12 h after the onset of chest pain was an independent factor to improve the in-hospital and long-term prognoses of women in general and of women without diabetes, whereas in women with diabetes, only 12-month survival was improved. Although in many studies, reperfusion therapy was equally effective in patients with and without diabetes (12,28,29), a worse prognosis was noted for patients with diabetes than for subjects without diabetes, despite the comparable efficacy of the therapy to restore blood flow in the infarct-related arteries defined as TIMI grade 3 (12,27,29). In patients with diabetes, no ST-segment resolution or low myocardial blush grades are found significantly more often; these indicate worse myocardial perfusions (13,28,30). In the PL-ACS registry, among women with STEMI post-procedural TIMI grade 3, flow was similar in both groups, confirming the high direct efficacy of invasive treatment in accordance with the above-quoted results. Among patients without diabetes, men had more severe coronary atherosclerosis, whereas among patients with diabetes, there were no significant sex-related differences. However, the presence of type 2 diabetes in women was associated with the progression of atherosclerosis. A significantly lower percentage of normal coronary vessels and of single-vessel disease and a higher percentage of triple-vessel disease were noted. The more advanced atherosclerosis of women with diabetes was another significant factor predicting a worse prognosis, in accordance with the results of the multivariate analysis. It is known that significant lesions in vessels other than the infarct-related arteries lead to global left ventricular impairment and increase the prevalence of pulmonary edema and cardiogenic shock (31,32). Additionally, in the PL-ACS registry, the course of STEMI in women with diabetes was significantly more frequently complicated by shock, pulmonary edema, and more severe cardiac injury, which are all associated with poorer prognosis. These trends were confirmed in a multivariate analysis showing that Killip class 3 or 4 is the most important predictor of in-hospital and 12-month mortality in women with diabetes, consistent with the findings of others (32,33). Women with diabetes significantly more frequently had higher heart rates, atrial fibrillation, and intraventricular conduction disorders, which have been shown to be significant predictors of outcomes after myocardial infarction (34–36). Although in light of the present knowledge it may be expected that women with diabetes are more prone to bleeding complications, the registry showed that type 2 diabetes was associated with higher rates of bleeding in men but not in women. This fact may be partly accounted for by the less frequent use of invasive strategies and clopidogrel in women with diabetes. Although patients with diabetes benefit relatively more from the recommended pharmacotherapy, in practice, they frequently receive less optimal treatment. The fact that other registries have reported the more frequent use of acetylsalicylic acid, β-blockers, ACE-i, and statins in women with diabetes (6,37–39) is promising. However, among patients with diabetes, β-blockers and statins were used significantly less frequently in women, which may partly account for the differences in mortality. Less frequent administration of glycoprotein IIb/IIIa inhibitors and suboptimal use of clopidogrel could also have a major effect on the outcome. In women with diabetes, nitrates and Ca blockers were also excessively used, although the use of Ca blockers is not currently recommended. These notable disparities in treatment strategies have previously been studied in detail in our population, and no reliable explanation was given aside from a few speculations, leading to the conclusion that women with STEMI are generally older and have more concomitant diseases than men. Whether this is the only reason for their conservative management and underuse of modern drugs remains unknown (11).
Multivessel coronary artery disease in patients with diabetes remains a classic indication for coronary artery bypass grafting (CABG). This guideline is constant and sustained, even in the era of drug-eluting stents and advanced PCI techniques (40), regardless of the continuing discussion over the superiority of either method of revascularization. However, this concerns the great majority of patients with stable angina who are scheduled for planned procedures after careful invasive and noninvasive assessments of ischemia. In the setting of STEMI, emergency CABG is allowed only in cases in which the coronary anatomy precludes PCI success or during which the PCI was not effective, leaving a large amount of myocardium at risk. In such cases, surgical revascularization can be completed in the initial 4 h (41). This is the main reason that CABG was the most infrequent option chosen in our study group. The disproportionate number of patients referred for CABG (emergent or staged) discourages us from performing analyses of PCI versus CABG in this group.
Our analysis has several limitations, which may bias its conclusions. First, this was not a randomized trial. Second, the treatment strategies were not defined by any protocol but were left to the discretion of the physician, according to current guidelines. Third, there was no routine oral glucose tolerance testing prior to discharge to identify subjects with prediabetes; this may have resulted in an unintentional decrease of the sample size and, therefore, an underestimation of the observed effects. Moreover, the registry does not include data on the myocardial perfusion grade; rather, we only analyzed the TIMI grade. There was also no follow-up for the prevalence of contrast-induced nephropathy, which constitutes an important but delayed complication of invasive treatment in patients with diabetes (42).
To conclude, women with diabetes had a worse clinical profile than women without diabetes and men with diabetes. The presence of type 2 diabetes was significantly associated with more advanced atherosclerosis in the coronary arteries. Type 2 diabetes is a significant, independent predictor of in-hospital and 1-year mortality in women with STEMI. The other independent factors that significantly increased the risk of in-hospital or 1-year mortality in women included age, cardiogenic shock or pulmonary edema, and anterior myocardial infarction. Although pPCI significantly improved 12-month outcomes in women with diabetes, it was used significantly less frequently compared with women without diabetes and men with diabetes.
Acknowledgments
No potential conflicts of interest relevant to this article were reported.
E.R. wrote the manuscript and researched the data. M.S. reviewed and edited the manuscript and researched the data. J.K. contributed to the discussion and reviewed and edited the manuscript. M.G. researched the data, performed statistical analysis, and reviewed the manuscript. L.P. reviewed and edited the manuscript and researched the data. E.R. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Rydén L, Standl E, Bartnik M, et al. Task Force on Diabetes and Cardiovascular Diseases of the European Society of Cardiology (ESC) European Association for the Study of Diabetes (EASD) Guidelines on diabetes, pre-diabetes, and cardiovascular diseases: executive summary. Eur Heart J 2007;28:88–136 [DOI] [PubMed] [Google Scholar]
- 2.Huxley R, Barzi F, Woodward M. Excess risk of fatal coronary heart disease associated with diabetes in men and women: meta-analysis of 37 prospective cohort studies. BMJ 2006;332:73–78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee WL, Cheung AM, Cape D, Zinman B. Impact of type 2 diabetes on coronary artery disease in women and men: a meta-analysis of prospective studies. Diabetes Care 2000;23:962–968 [DOI] [PubMed]
- 4.Larsson CA, Gullberg B, Merlo J, Rastam L, Lindblad U. Female advantage in AMI mortality is reversed in patients with type 2 diabetes in the Skaraborg Project. Diabetes Care 2005;28:2246–2248 [DOI] [PubMed]
- 5.Kanaya AM, Grady D, Barrett-Connor E. Explaining the sex difference in coronary heart disease mortality among patients with type 2 diabetes mellitus: a meta-analysis. Arch Intern Med 2002;162:1737–1745 [DOI] [PubMed] [Google Scholar]
- 6.Franklin K, Goldberg RJ, Spencer F, et al. Implications of diabetes in patients with acute coronary syndromes. The Global Registry of Acute Coronary Events. Arch Intern Med 2004;164:1457–1463 [DOI] [PubMed] [Google Scholar]
- 7.Dotevall A, Hasdai D, Wallentin L, Battler A, Rosengren A, Data from the Euro Heart Survey ACS Diabetes mellitus: clinical presentation and outcome in men and women with acute coronary syndromes. Diabet Med 2005;22:1542–1550 [DOI] [PubMed] [Google Scholar]
- 8.Poloński L, Gasior M, Gierlotka M, et al. Polish Registry of Acute Coronary Syndromes (PL-ACS). Characteristics, treatments and outcomes of patients with acute coronary syndromes in Poland. Kardiol Pol 2007;65:861–872; discussion 873–874 [PubMed] [Google Scholar]
- 9.Hasdai D, Behar S, Wallentin L, et al. A prospective survey of the characteristics, treatments and outcomes of patients with acute coronary syndromes in Europe and the Mediterranean basin; the Euro Heart Survey of Acute Coronary Syndromes (Euro Heart Survey ACS). Eur Heart J 2002;23:1190–1201 [DOI] [PubMed] [Google Scholar]
- 10.Bartnik M, Rydén L, Ferrari R, et al. Euro Heart Survey Investigators The prevalence of abnormal glucose regulation in patients with coronary artery disease across Europe. The Euro Heart Survey on diabetes and the heart. Eur Heart J 2004;25:1880–1890 [DOI] [PubMed] [Google Scholar]
- 11.Sadowski M, Gasior M, Gierlotka M, Janion M, Poloński L. Gender-related differences in mortality after ST-segment elevation myocardial infarction: a large multicentre national registry. EuroIntervention 2011;6:1068–1072 [DOI] [PubMed] [Google Scholar]
- 12.Granger CB, Califf RM, Young S, et al. Outcome of patients with diabetes mellitus and acute myocardial infarction treated with thrombolytic agents: The Thrombolysis and Angioplasty in Myocardial Infarction (TAMI) Study Group. J Am Coll Cardiol 1993;21:920–925 [DOI] [PubMed] [Google Scholar]
- 13.De Luca G, Gibson CM, Bellandi F, et al. Diabetes mellitus is associated with distal embolization, impaired myocardial perfusion, and higher mortality in patients with ST-segment elevation myocardial infarction treated with primary angioplasty and glycoprotein IIb-IIIa inhibitors. Atherosclerosis 2009;207:181–185 [DOI] [PubMed] [Google Scholar]
- 14.Meisinger C, Heier M, von Scheidt W, Kirchberger I, Hörmann A, Kuch B. Gender-specific short and long-term mortality in diabetic versus nondiabetic patients with incident acute myocardial infarction in the reperfusion era (the MONICA/KORA Myocardial Infarction Registry). Am J Cardiol 2010;106:1680–1684 [DOI] [PubMed] [Google Scholar]
- 15.Rosengren A, Wallentin L, Simoons M, et al. Age, clinical presentation, and outcome of acute coronary syndromes in the Euroheart acute coronary syndrome survey. Eur Heart J 2006;27:789–795 [DOI] [PubMed] [Google Scholar]
- 16.Lubiszewska B, Skóra E, Kruk M, et al. Prevalence of classical risk factors in Polish women with premature coronary artery disease. Kardiol Pol 2010;68:1032–1037 [PubMed] [Google Scholar]
- 17.Kawecka-Jaszcz K, Pośnik-Urbańska A, Jankowski P. Prevalence of arterial hypertension in Poland—impact of gender. Arterial Hypertension 2007;11:377–383 [Google Scholar]
- 18.Kozak-Szkopek E, Baraniak J, Mieczkowska J. Prevalence of coronary heart disease risk factors in the sixth decade of life. Gerontologia Polska 2006;14:18–24 [Google Scholar]
- 19.Ivanuša M, Ivanuša Z, Jelaković B, Miličić D. The influence of hypertension on in-hospital outcome in patients with acute myocardial infarction. Med Glas 2009;6:53–59 [Google Scholar]
- 20.Gourlay SG, Rundle AC, Barron HV. Smoking and mortality following acute myocardial infarction: results from the National Registry of Myocardial Infarction 2 (NRMI 2). Nicotine Tob Res 2002;4:101–107 [DOI] [PubMed] [Google Scholar]
- 21.Nikolsky E, Stone GW, Grines CL, et al. Impact of body mass index on outcomes after primary angioplasty in acute myocardial infarction. Am Heart J 2006;151:168–175 [DOI] [PubMed] [Google Scholar]
- 22.Trichon BH, Roe MT. Acute coronary syndromes and diabetes mellitus. Diab Vasc Dis Res 2004;1:23–32 [DOI] [PubMed]
- 23.Sadowski M, Janion-Sadowska A, Gąsior M, Gierlotka M, Janion M, Poloński L. Gender-related benefit of transport to primary angioplasty: is it equal? Cardiol J 2011;18:254–260 [PubMed] [Google Scholar]
- 24.Ting HH, Bradley EH, Wang Y, et al. Factors associated with longer time from symptom onset to hospital presentation for patients with ST-elevation myocardial infarction. Arch Intern Med 2008;168:959–968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dziewierz A, Siudak Z, Dykla D, et al. Management and mortality in patients with non-ST-segment elevation vs. ST-segment elevation myocardial infarction. Data from the Malopolska Registry of Acute Coronary Syndromes. Kardiol Pol 2009;67:115–120; discussion 121–122 [PubMed] [Google Scholar]
- 26.Collet JP, Montalescot G. The acute reperfusion management of STEMI in patients with impaired glucose tolerance and type 2 diabetes. Diab Vasc Dis Res 2005;2:136–143 [DOI] [PubMed] [Google Scholar]
- 27.Harjai KJ, Stone GW, Boura J, et al. Primary Angioplasty in Myocardial Infarction Investigators Comparison of outcomes of diabetic and nondiabetic patients undergoing primary angioplasty for acute myocardial infarction. Am J Cardiol 2003;91:1041–1045 [DOI] [PubMed] [Google Scholar]
- 28.Angeja BG, de Lemos J, Murphy SA, et al. TIMI Study Group Impact of diabetes mellitus on epicardial and microvascular flow after fibrinolytic therapy. Am Heart J 2002;144:649–656 [DOI] [PubMed] [Google Scholar]
- 29.Zhang Q, Shen J, Zhang RY, et al. Outcomes after primary coronary intervention with drug-eluting stent implantation in diabetic patients with acute ST elevation myocardial infarction. Chin Med J (Engl) 2007;120:1862–1867 [PubMed] [Google Scholar]
- 30.Marso SP, Miller T, Rutherford BD, et al. Comparison of myocardial reperfusion in patients undergoing percutaneous coronary intervention in ST-segment elevation acute myocardial infarction with versus without diabetes mellitus (from the EMERALD Trial). Am J Cardiol 2007;100:206–210 [DOI] [PubMed] [Google Scholar]
- 31.Lekston A, Tajstra M, Gąsior M, et al. Impact of multivessel coronary disease on one-year clinical outcomes and five-year mortality in patients with ST-elevation myocardial infarction undergoing percutaneous coronary intervention. Kardiol Pol 2011;69:336–343 [PubMed] [Google Scholar]
- 32.Shindler DM, Palmeri ST, Antonelli TA, et al. Diabetes mellitus in cardiogenic shock complicating acute myocardial infarction: a report from the SHOCK Trial Registry. SHould we emergently revascularize Occluded Coronaries for cardiogenic shocK? J Am Coll Cardiol 2000;36(3 Suppl. A):1097–1103 [DOI] [PubMed] [Google Scholar]
- 33.Vis MM, Sjauw KD, van der Schaaf RJ, et al. In patients with ST-segment elevation myocardial infarction with cardiogenic shock treated with percutaneous coronary intervention, admission glucose level is a strong independent predictor for 1-year mortality in patients without a prior diagnosis of diabetes. Am Heart J 2007;154:1184–1190 [DOI] [PubMed] [Google Scholar]
- 34.Foo K, Sekhri N, Knight C, et al. The effect of diabetes on heart rate and other determinants of myocardial oxygen demand in acute coronary syndromes. Diabet Med 2004;21:1025–1031 [DOI] [PubMed] [Google Scholar]
- 35.Schmitt J, Duray G, Gersh BJ, Hohnloser SH. Atrial fibrillation in acute myocardial infarction: a systematic review of the incidence, clinical features and prognostic implications. Eur Heart J 2009;30:1038–1045 [DOI] [PubMed] [Google Scholar]
- 36.Vivas D, Pérez-Vizcayno MJ, Hernández-Antolín R, et al. Prognostic implications of bundle branch block in patients undergoing primary coronary angioplasty in the stent era. Am J Cardiol 2010;105:1276–1283 [DOI] [PubMed] [Google Scholar]
- 37.Vaur L, Danchin N, Hanania G, et al. Management and short-term outcome of diabetic patients hospitalized for acute myocardial infarction: results of a nationwide French survey. Diabetes Metab 2003;29:241–249 [DOI] [PubMed] [Google Scholar]
- 38.Hasin T, Hochadel M, Gitt AK, Behar S, Bueno H, Hasin Y. Comparison of treatment and outcome of acute coronary syndrome in patients with versus patients without diabetes mellitus. Am J Cardiol 2009;103:772–778 [DOI] [PubMed] [Google Scholar]
- 39.Norhammar A, Stenestrand U, Lindbäck J, Wallentin L. Women younger than 65 years with diabetes mellitus are a high-risk group after myocardial infarction: a report from the Swedish Register of Information and Knowledge about Swedish Heart Intensive Care Admission (RIKS-HIA). Heart 2008;94:1565–1570 [DOI] [PubMed] [Google Scholar]
- 40.Farkouh ME, Domanski M, Sleeper LA, et al. FREEDOM Trial Investigators Strategies for multivessel revascularization in patients with diabetes. N Engl J Med 2012;367:2375–2384 [DOI] [PubMed] [Google Scholar]
- 41.Wijns W, Kolh P, Danchin N, et al. Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) European Association for Percutaneous Cardiovascular Interventions (EAPCI) Guidelines on myocardial revascularization. Eur Heart J 2010;31:2501–2555 [DOI] [PubMed] [Google Scholar]
- 42.Mehran R, Aymong ED, Nikolsky E, et al. A simple risk score for prediction of contrast-induced nephropathy after percutaneous coronary intervention: development and initial validation. J Am Coll Cardiol 2004;44:1393–1399 [DOI] [PubMed] [Google Scholar]