Abstract
OBJECTIVE
To investigate the relationship of circulating matrix Gla protein (MGP) species with incident cardiovascular disease (CVD) or coronary heart disease (CHD) in type 2 diabetic patients.
RESEARCH DESIGN AND METHODS
EPIC-NL is a prospective cohort study among 40,011 Dutch men and women. At baseline (1993–1997), 518 participants were known to have type 2 diabetes. MGP levels were measured by ELISA techniques in baseline plasma samples. The incidence of fatal and nonfatal CVD and CVD subtypes—CHD, peripheral arterial disease (PAD), heart failure, and stroke—were obtained by linkage to national registers. Cox proportional hazard models were used to calculate hazard ratios (HRs), adjusted for sex, waist-to-hip ratio, physical activity, and history of CVD.
RESULTS
During a median 11.2 years of follow-up, 160 cases of CVD were documented. Higher circulating desphospho-uncarboxylated MGP (dp-ucMGP) levels were significantly associated with higher risk of CVD, with an HR per SD (HRSD) of 1.21 (95% CI 1.06–1.38), PAD (HRSD 1.32 [95% CI 1.07–1.65]), and heart failure (HRSD 1.75 [95% CI 1.42–2.17]) after adjustment. Higher circulating dp-ucMGP levels were not related to risk of CHD (HRSD 1.12 [95% CI 0.94–1.34]) or stroke (HRSD 1.05 [95% CI 0.73–1.49]). Circulating desphospho-carboxylated MGP and circulating total-uncarboxylated MGP levels were not associated with CVD or CVD subtypes.
CONCLUSIONS
High dp-ucMGP levels were associated with increased CVD risk among type 2 diabetic patients, especially with the subtypes PAD and heart failure, while other MGP species were not related to CVD risk. These results suggest that a poor vitamin K status is associated with increased CVD risk.
Coronary artery calcification is an independent predictor of cardiovascular disease (CVD) (1). Matrix Gla protein (MGP) is a vitamin K–dependent protein and a potent inhibitor of vascular calcification (2). The importance of MGP for vascular health has been demonstrated in MGP-deficient animals, who all died of massive arterial calcification within 6–8 weeks after birth (3). The cellular and molecular mechanisms by which MGP prevents ectopic calcium deposition are multifaceted, including 1) regulation of calcification by vascular smooth muscle cell (VSMC)-derived matrix vesicles and apoptotic body, 2) inhibition of calcium-phosphate precipitation, and 3) inhibition of VSMC trans differentiation (4). Vitamin K is required for the function of MGP through its role as a cofactor for the enzyme γ-glutamyl carboxylase, catalyzing the carboxylation of glutamic acid residues (Glu) into γ-carboxyglutamate (Gla) at five well-defined places in the protein (5). Human studies showed that high vitamin K intake is associated with reduced coronary artery calcification and reduced risk of CVD (6–9). These effects are thought to be mediated by increased activation of MGP (10).
MGP exists as various species, which differ in their state of phosphorylation or carboxylation: phosphorylated, nonphosphorylated (desphospho-MGP [dpMGP]), carboxylated (cMGP), or uncarboxylated (ucMGP). Total uncarboxylated MGP (t-ucMGP) is thought to be the sum of desphospho-uncarboxylated MGP (dp-ucMGP) and phosphorylated-uncarboxylated MGP (p-ucMGP) and mainly consists of p-ucMGP.
Development of assays to measure circulating MGP species enabled the investigation of these species in the circulation (11). These studies have shown that dp-ucMGP is a marker for vitamin K status, with high dp-ucMGP level reflecting a low vitamin K status (12–17). In line with these results, several studies indeed showed that high dp-ucMGP levels were associated with more calcification, though not consistently (13,16,18,19). Theoretically, dp-cMGP forms the mirror image of dp-ucMGP and is hypothesized to be associated with lower calcification, but results from human, observational studies are inconsistent (16,20). Finally, in cross-sectional studies, high t-ucMGP has been associated with decreased calcification (16,21–23).
Although vascular calcification may not be causally related to CVD, it has emerged as a strong and independent risk marker for CVD (1), but the association of MGP species with CVD events has not been investigated to date. Diabetes is associated with severe cardiovascular complications, including vascular calcification and accelerated atherosclerosis, leading to increased morbidity and mortality in diabetic patients (24–27) Therefore, we performed a prospective study to investigate the association between circulating MGP species and CVD or coronary heart disease (CHD) risk among a high-risk population, i.e., type 2 diabetic patients.
RESEARCH DESIGN AND METHODS
The EPIC-NL cohort is the Dutch contribution to the European Prospective Investigation into Cancer and Nutrition (EPIC) and consists of the Prospect-EPIC and MORGEN-EPIC cohorts (28). The Prospect-EPIC study includes 17,357 women 49–70 years of age living in Utrecht and vicinity who participated in the nationwide Dutch breast cancer screening program between 1993 and 1997. The MORGEN-EPIC cohort consists of 22,654 men and women 21–64 years of age selected from random samples of the Dutch population in three different towns. Participants were recruited in both studies from 1993 to 1997. At baseline, a general and a food-frequency questionnaire were administered, and a physical examination was performed for blood pressure measurements, anthropometry, and nonfasting blood sampling. All participants provided informed consent before study inclusion. The study complies with the Declaration of Helsinki and was approved by the institutional board of the University Medical Center Utrecht (Prospect) and the Medical Ethical Committee of The Netherlands Organization for Applied Scientific Research Nutrition and Food Research (MORGEN).
Three sources of ascertainment of diabetes were used: self-report, hospital discharge diagnoses, and urinary strip test (in the Prospect part of the cohort only). Potential cases of diabetes ascertained by these sources were verified against medical and pharmacy records. Details of the ascertainment sources and verification procedures have previously been described (29).
At baseline, 615 participants were verified to have type 2 diabetes. Those who did not give permission for linkage with vital status registries were excluded (n = 10). After exclusion of participants with missing data on CVD (n = 25) and blood samples (n = 62), 518 participants were left for analysis.
MGP species
The measurement of plasma t-ucMGP was performed with a competitive mono antibody ELISA as previously described (11). This ELISA identifies all MGP species carrying the uncarboxylated Gla domain, irrespective of whether the MGP species are phosphorylated or fragmented. In contrast to t-ucMGP, analyses of dp-ucMGP and dp-cMGP were conducted with a dual-antibody (“sandwich”) ELISA. Both assays use a monoclonal antibody against the dpMGP sequence 3–15 as capture antibody (mAb-dpMGP; VitaK BV, Maastricht, the Netherlands). The dp-ucMGP assay is based on the use of detection monoclonal antibody directed against the ucMGP sequence 35–49 in human MGP (mAb-ucMGP; VitaK BV), while for dp-cMGP this was directed against the cMGP sequence 35–54 in human MGP (mAb-cMGP; VitaK BV). All measurements were performed in duplicate, and average values are given throughout this article.
Outcome assessment
Morbidity follow-up data on CVD events were obtained from the Dutch Centre for Health Care Information, which holds a standardized computerized register of hospital discharge diagnoses. All diagnoses were coded according to the ICD-9. Follow-up was complete until the first of January 2008. The database was linked to the cohort on the basis of birth date, sex, postal code, and general practitioner with a validated probabilistic method (30). Information on vital status was obtained through linkage with the municipal registries. Causes of death were collected from Statistics Netherlands. End points for the present analysis were CVD and the subtypes CHD, peripheral arterial disease (PAD), heart failure, and stroke. CVD was defined as CHD, PAD, heart failure, and stroke (CVD, 410–414, 427.5, 428, 415.1, 443.9, 430–438, 440–442, 444, 798.1, 798.2, and 798.9; CHD, 410–414, 427.5, 798.1, 798.2, and 798.9; PAD, 440–444; heart failure, 428; and stroke, 430–434 and 436). These end points included both fatal and nonfatal cases of CVD, CHD, PAD, heart failure, and stroke.
Other measurements
The general questionnaire contained questions on demographic characteristics, the presence of chronic diseases, and risk factors for chronic diseases. Smoking was categorized into current, past, and never smoker. Level of education was categorized as low (primary education up to those completing advanced elementary education), average (intermediate vocational education and higher general secondary education) or high (higher vocational education and university). Physical activity was assessed using a questionnaire validated in an elderly population and categorized according to the Cambridge Physical Activity Index (31). During the baseline physical examination screening, systolic and diastolic blood pressure measurements were performed twice in the supine position on the right arm using a Boso Oscillomat (Bosch & Son, Jungingen, Germany) (Prospect-EPIC) or on the left arm using a random zero sphygmomanometer (MORGEN-EPIC), from which the mean was taken. Height and weight were measured, and BMI was calculated. Time since diabetes diagnosis was calculated by subtracting the age of diagnosis from the age at baseline examination. HbA1c concentrations were measured in erythrocytes using an immunoturbidimetric latex test. All measurements were performed according to standard operating procedures.
Data analysis
Participant characteristics are presented as means with SDs or percentages. The duration of follow-up was calculated as the interval between date of study entry (1993–1997) and the occurrence of a cardiovascular event, death, loss to follow-up, or 1 January 2008: whichever came first.
Cox proportional hazard models were used to calculate crude and adjusted hazard ratios (HRs) and 95% CIs for the associations between MGP species (continuous) and CVD or CVD subtypes. Potential confounding factors (age, sex, BMI, waist-to-hip ratio, smoking habits, physical activity, education, systolic and diastolic blood pressure, and total cholesterol) were selected based on univariable associations of potential confounders with both CVD or CVD subtypes and MGP species and whether adjustment for the confounder changed the HR by >10%. Variables selected this way were incorporated into a multivariate model by means of a stepwise selection approach. The confounders that were entered into the model were age, sex, waist-to-hip ratio, and Cambridge physical activity index (CPAI) (model 1). The second model additionally included history of CVD or CVD subtypes (model 2). In a separate model, we also checked whether adjusting for duration of diabetes, HbA1c, concentrations, blood lipids, and blood pressure influenced the results. We repeated the analyses after excluding not verified type 2 diabetic patients (n = 67). Moreover, analyses were repeated with outcomes fatal CVD (n = 36) and all-cause mortality (n = 114).
The possibility of a nonlinear relation was examined nonparametrically with restricted cubic splines (32), and no evidence for nonlinear associations was found.
For handling missing data for confounders, we used multiple imputations. We assumed that the missing data were at random. We generalized 10 imputed datasets and used Rubin rules to combine the estimates of the parameters (33). Two-sided P values <0.05 were considered statistically significant. All statistical analyses were conducted using IBM SPSS (version 20 for Windows).
RESULTS
Table 1 shows the baseline characteristics of the study population. The mean age of the study population was 58.1 years, and 17.8% were men. The diabetes duration was on average 6.3 years, and mean HbA1c was 8.0%. The medians of the circulating MGP levels of the different species were 156 pmol/L with an interquartile range (IQR) of 91–258 for dp-ucMGP, 1,062 pmol/L for dp-cMGP (IQR 716–1,240), and 4,308 nmol/L for t-ucMGP (IQR 3,514–5,079). During a mean follow-up of 9.9 years 160 incident cases of CVD, 99 incident cases of CHD, 38 incident cases of PAD, 28 incident cases of heart failure, and 26 incident cases of stroke were documented.
Table 1.
Baseline characteristics of 518 diabetic patients
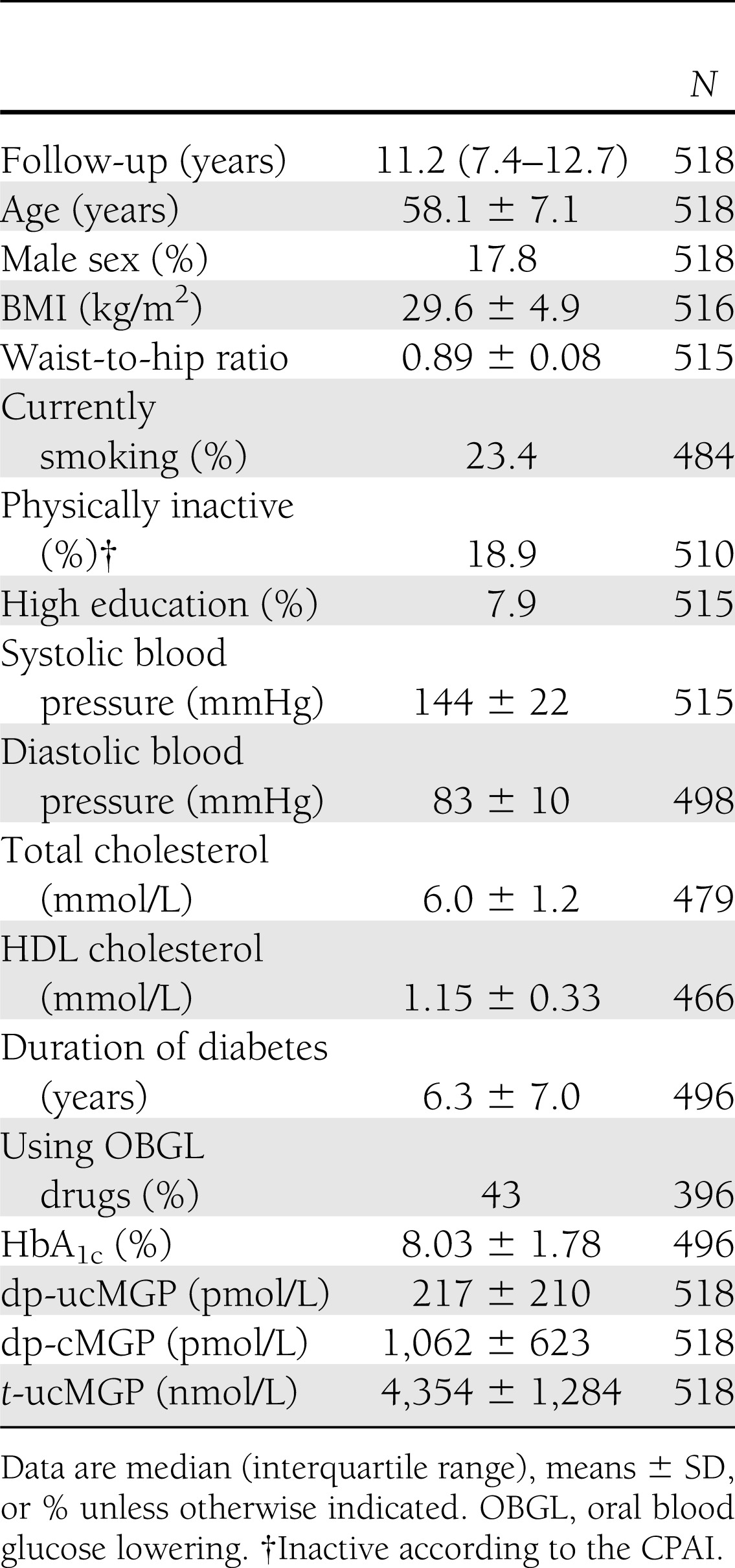
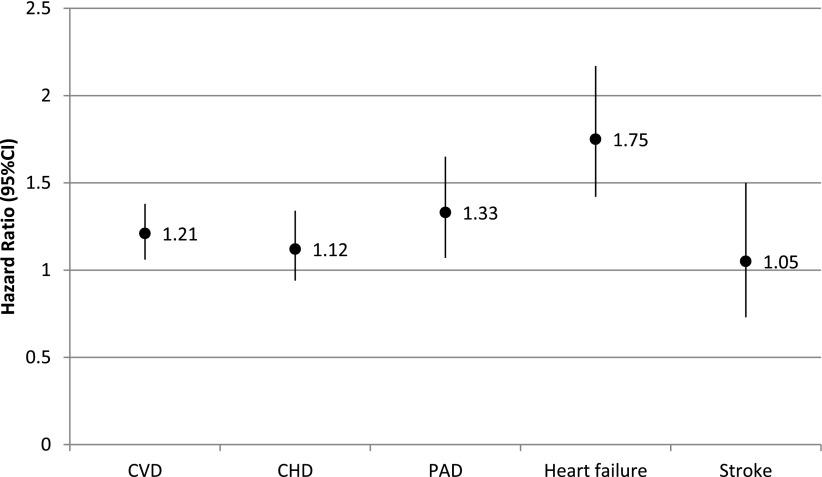
Table 2 shows the association between MGP species and CVD or CVD subtypes risk. After adjustment for age, sex, waist-to-hip ratio, CPAI, and history of CVD, higher circulating dp-ucMGP levels were significantly associated with higher risk of CVD, with an HR per SD (HRSD) of 1.21 (95% CI 1.06–1.38, P = 0.01). Higher circulating dp-ucMGP levels were significantly associated with higher risk of CHD in crude analyses (HRSD 1.24 [95% CI 1.06–1.45], P = 0.01). After full adjustment, the association attenuated to nonsignificant (HRSD 1.12 [95% CI 0.94–1.34], P = 0.21). Higher circulating dp-ucMGP levels were significantly associated with higher risk of PAD (HRSD 1.32 [95% CI 1.07–1.65], P = 0.01) and heart failure (HRSD 1.75 [95% CI 1.42–2.17], P < 0.001) but not with the risk of stroke (HRSD 1.05 [95% CI 0.73–1.49]) after full adjustment (Fig. 1).
Table 2.
Crude and adjusted HRs (95% CI) for the association of MGP* species with incident (fatal or nonfatal) CVD and CHD among 518 diabetic subjects
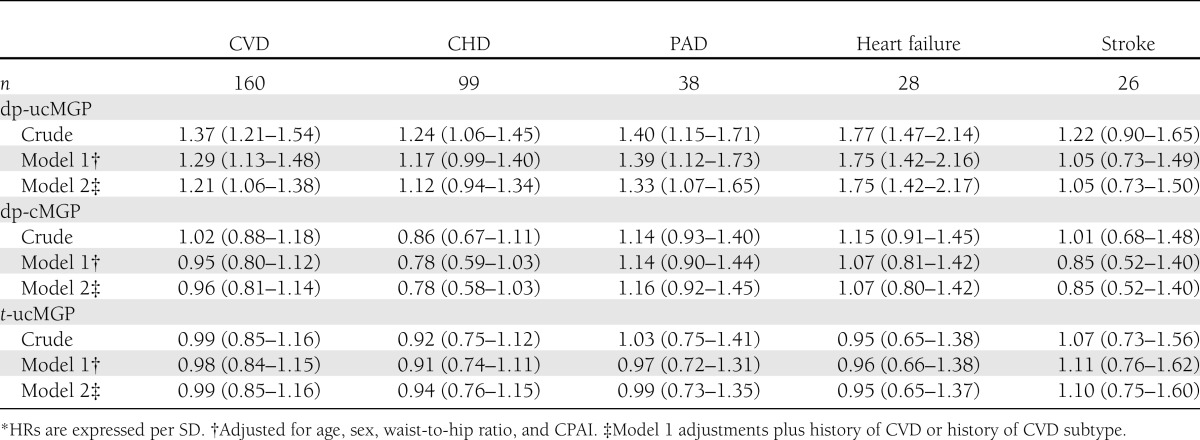
Figure 1.
Adjusted HRs (95% CI) for the association of dp-ucMGP levels with incident (fatal and nonfatal) CVD and CVD subtypes among 518 diabetic subjects. HRs are expressed per SD and adjusted for age, sex, waist-to-hip ratio, CPAI, history of CVD, and CVD subtypes.
Circulating dp-cMGP levels were not associated with CVD risk either in crude analyses or after full adjustment (HRSD 0.96 [95% CI 0.81–1.14], P = 0.64). They were borderline significantly associated with a lower CHD risk (HRSD 0.78 [95% CI 0.58–1.03], P = 0.08) after full adjustment. There was no association between circulating dp-cMGP levels and PAD (HRSD 1.16 [95% CI 0.92–1.45]), heart failure (HRSD 1.07 [95% CI 0.80–1.42]) or stroke (HRSD 0.85 [95% CI 0.52–1.40]) after full adjustment.
No associations between circulating t-ucMGP levels and the risk of CVD or CVD subtypes were observed.
Restricting the outcome to CVD mortality, we observed a statistically significant association of dp-ucMGP (HRSD 1.31 [95% CI 1.05–1.64], P = 0.02) with CVD mortality. However, again, dp-cMGP and t-ucMGP were not associated with this end point (data not shown). Furthermore, the association of circulating dp-ucMGP with all-cause mortality was similar to the association with CVD mortality with a HRSD of 1.20 (95% CI 1.04–1.39).
Adjusting for diabetes duration, HbA1c concentrations, blood lipids, or blood pressure did not affect these results (data not shown). Excluding not verified type 2 diabetic patients yielded comparable results (data not shown).
CONCLUSIONS
To our knowledge, this is the first study investigating the association of circulating MGP species with the risk of cardiovascular events. In this prospective study, we observed that high circulating dp-ucMGP levels, reflecting a poor vitamin K status, were associated with increased CVD risk, especially with subtypes PAD and heart failure, in type 2 diabetic patients. We did not observe a significant association between dp-cMGP or t-ucMGP and CVD risk.
No previous studies have investigated the association between dp-ucMGP levels and CVD events; thus far, only the association between dp-ucMGP and mortality has been investigated. These studies have been performed in high-risk populations such as patients with aortic stenosis or heart failure and generally showed strong positive associations between dp-ucMGP and risk of total or cardiovascular mortality (18,34,35). Only a study by Schlieper et al. (20) found that hemodialysis patients with low dp-ucMGP levels had a nonsignificant HR of 1.71 (95% CI 0.92–3.17) for all-cause mortality and a nonsignificant HR of 1.83 (95% CI 0.90–3.70) for cardiovascular mortality, but these HRs were not adjusted for other risk factors. Our study confirmed that high dp-ucMGP levels are associated with higher mortality risk. In line with most studies on mortality, several studies, but not all, have shown that high dp-ucMGP levels are associated with increased calcification (13,16,18,19). We now extend these findings by showing that high circulating dp-ucMGP levels are also associated with increased CVD risk among diabetic patients. Since studies have consistently shown that high dp-ucMGP levels are associated with a poor vitamin K status (12–17), these results suggest that a poor vitamin K status is associated with increased CVD risk.
However, in order to describe clinical relevance, the added prognostic values of dp-ucMGP levels beyond traditional risk factors should be further investigated. In our study, we found an association between higher circulating dp-ucMGP and increased CVD risk. However, this association was stronger for the subtypes PAD and heart failure. This may be explained by the presence of two types of vascular calcification, i.e., intimal calcification and medial calcification. Intimal calcification is seen in sites of atherosclerotic plaques in which cellular necrosis, inflammation, and cholesterol deposition occur. The presence of this type of calcification is associated with atherosclerotic burden (36). Medial calcification, which occurs in the elastic lamina of large- and medium- to small-size arteries, is particularly present in peripheral arteries (36). Medial calcification is a metabolite-induced calcification in the absence of lipid deposits, leading to upregulation of osteogenic genes and proteins with subsequent matrix mineralization and bone and cartilage formation (37). This process requires a complex regulatory network involving both stimulators and inhibitors of calcification such as MGP, osteoprotegerin, and osteopontin (37). The specific association of dp-ucMGP with PAD suggests that this relation is mainly driven by a relation of dp-ucMGP with medial calcification. However, this needs to be further investigated.
Also, for the subtype heart failure we found a stronger association than for CVD. Although the role of MGP in vascular calcification is firmly established, the precise function of MGP in the heart is unknown. However, the lack of myocardial calcification in the MGP-deficient mice suggests an additional effect of MGP in the heart not related to inhibition of calcification (3). Furthermore, MGP has been associated with extracellular matrix binding and apoptosis, as well as tissue growth and development, and all these processes may be relevant to myocardial remodeling (38–40). Previously, raised MGP concentrations have been found as a rapid myocardial response to pressure overload, potentially induced by angiotensin II, suggesting a link between neurohormonal disturbances and MGP (41–43). This angiotensin II–mediated increase in MGP was seen in both cardiomyocytes and fibroblasts. In addition, Ueland et al. (35) found a strong correlation between dp-ucMGP and N-terminal pro-B-type natriuretic peptide, which further supports such a notion. Although further studies are needed, it is plausible that the association between dp-ucMGP and heart failure is at least partly caused through mechanisms that are independent of vascular calcification. Theoretically, dp-cMGP forms the mirror image of dp-ucMGP, and therefore we expected that high levels of dp-cMGP would be associated with lower CVD risk. No previous studies investigated the association between dp-cMGP levels and CVD events, but the association with mortality has been investigated. No association between dp-cMGP levels and mortality risk in patients with symptomatic aortic stenosis or chronic heart failure was observed (34,35). This is consistent with a previous cross-sectional study from our group, where we did not find an association between dp-cMGP and calcification (16). However, in hemodialysis patients low levels of dp-cMGP were associated with increased CVD mortality risk (HR 2.7 [95% CI 1.2–6.2]) (20). In our study, we could not detect an association between dp-cMGP and CVD risk. However, we observed a borderline significant association of high dp-cMGP levels with a reduced risk of CHD, similar to the results in hemodialysis patients (19). Because of the relatively small sample size of our study, we may have had limited power to detect a somewhat weaker association. Therefore, our results and those of Schlieper et al. (20) suggest that there might be an association between high dp-cMGP and reduced CHD risk. For further clarification of the role of dp-cMGP in CVD and CHD risk, more and larger population studies, as well as physiological studies, are warranted.
One previous study investigated the association between t-ucMGP and CVD or mortality risk (44). In coronary artery disease patients, each 1,000 nmol/L higher t-ucMGP level was associated with a 16% lower CVD risk and a 22% lower risk of all-cause mortality. However, the association of t-ucMGP levels with mortality was limited to participants without diabetes, whereas there was no significant association in diabetic patients (HR 1.10 [95% CI 0.85–1.41]). We also found no association between t-ucMGP levels and CVD risk in diabetic patients. This could be due to population differences: the study mentioned above resulted from a cohort selected for coronary artery disease, who have coronary artery calcification, while our participants were selected for the presence of diabetes. We assume that t-ucMGP may act differently in persons with or without calcification because t-ucMGP mainly consists of phosphorylated ucMGP species. The phosphoserines equip the molecule with strong affinity for vascular calcification, thereby causing a decrease in the plasma circulating levels of t-ucMGP, leading to lower t-ucMGP levels at higher levels of calcification (21).
Our study has certain limitations to consider. The assays for dp-ucMGP and dp-cMGP only detected the nonphosphorylated fraction of MGP. Biochemical tests for other circulating MGP species are currently not available. Further, circulating MGP levels do not necessarily reflect MGP tissue levels of the vasculature. We therefore can only speculate how circulating MGP levels as a biomarker are related to tissue MGP. Furthermore, the dp-ucMGP levels and dp-cMGP levels in our study were low compared with a healthy reference group (11). This could be due to the possible degradation of MGP in our samples because samples have been stored for a long time in straws. Finally, our study was limited to type 2 diabetic patients, which limits generalizability of our results to the general population. However, this study population is particularly relevant to exploring associations with CVD risk because approximately one-half of patients with type 2 diabetes will die of cardiovascular causes (45,46).
In conclusion, the findings of this prospective study among type 2 diabetic patients shows that high circulating dp-ucMGP levels are associated with increased CVD risk, especially with PAD and heart failure. Circulating dp-cMGP and t-ucMGP levels were not related to CVD risk. These results suggest that a poor vitamin K status is associated with increased CVD risk.
Acknowledgments
The EPIC-NL study was funded by the European Commission: Public Health and Consumer Protection Directorate 1993-2004; Research Directory-General 2005; Dutch Ministry of Public Health, Welfare and Sports; Netherlands Cancer Registry; LK Research Funds; Dutch Prevention Funds; Dutch Zorg Onderzoek Nederland; and World Cancer Research Fund (the Netherlands). This research was supported by a personal Dr. Dekker postdoctoral grant (2008T062) from the Netherlands Heart Foundation (to J.W.J.B.). Part of this research was funded by an unrestricted grant from the Nutricia Research Foundation (2011-22).
No potential conflicts of interest relevant to this article were reported.
G.W.D. designed the research, wrote the manuscript, and analyzed data. Y.T.v.d.S. designed the research and reviewed and edited the manuscript. E.J.M., C.V., W.M.M.V., and J.M.A.B. reviewed the edited the manuscript. J.W.J.B. designed the research and reviewed and edited the manuscript. G.W.D. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Greenland P, Bonow RO, Brundage BH, et al. American College of Cardiology Foundation Clinical Expert Consensus Task Force (ACCF/AHA Writing Committee to Update the 2000 Expert Consensus Document on Electron Beam Computed Tomography) Society of Atherosclerosis Imaging and Prevention. Society of Cardiovascular Computed Tomography ACCF/AHA 2007 clinical expert consensus document on coronary artery calcium scoring by computed tomography in global cardiovascular risk assessment and in evaluation of patients with chest pain: a report of the American College of Cardiology Foundation Clinical Expert Consensus Task Force (ACCF/AHA Writing Committee to Update the 2000 Expert Consensus Document on Electron Beam Computed Tomography) developed in collaboration with the Society of Atherosclerosis Imaging and Prevention and the Society of Cardiovascular Computed Tomography. J Am Coll Cardiol 2007;49:378–402 [DOI] [PubMed] [Google Scholar]
- 2.Shanahan CM, Proudfoot D, Farzaneh-Far A, Weissberg PL. The role of Gla proteins in vascular calcification. Crit Rev Eukaryot Gene Expr 1998;8:357–375 [DOI] [PubMed] [Google Scholar]
- 3.Luo G, Ducy P, McKee MD, et al. Spontaneous calcification of arteries and cartilage in mice lacking matrix GLA protein. Nature 1997;386:78–81 [DOI] [PubMed] [Google Scholar]
- 4.Schurgers LJ, Uitto J, Reutelingsperger CP. Vitamin K-dependent carboxylation of matrix Gla-protein: a crucial switch to control ectopic mineralization. Trends Mol Med 2013;19:217–226 [DOI] [PubMed] [Google Scholar]
- 5.Furie B, Bouchard BA, Furie BC. Vitamin K-dependent biosynthesis of gamma-carboxyglutamic acid. Blood 1999;93:1798–1808 [PubMed] [Google Scholar]
- 6.Beulens JW, Bots ML, Atsma F, et al. High dietary menaquinone intake is associated with reduced coronary calcification. Atherosclerosis 2009;203:489–493 [DOI] [PubMed] [Google Scholar]
- 7.Shea MK, O’Donnell CJ, Hoffmann U, et al. Vitamin K supplementation and progression of coronary artery calcium in older men and women. Am J Clin Nutr 2009;89:1799–1807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gast GC, de Roos NM, Sluijs I, et al. A high menaquinone intake reduces the incidence of coronary heart disease. Nutr Metab Cardiovasc Dis 2009;19:504–510 [DOI] [PubMed] [Google Scholar]
- 9.Geleijnse JM, Vermeer C, Grobbee DE, et al. Dietary intake of menaquinone is associated with a reduced risk of coronary heart disease: the Rotterdam Study. J Nutr 2004;134:3100–3105 [DOI] [PubMed] [Google Scholar]
- 10.Schurgers LJ, Cranenburg EC, Vermeer C. Matrix Gla-protein: the calcification inhibitor in need of vitamin K. Thromb Haemost 2008;100:593–603 [PubMed] [Google Scholar]
- 11.Cranenburg EC, Koos R, Schurgers LJ, et al. Characterisation and potential diagnostic value of circulating matrix Gla protein (MGP) species. Thromb Haemost 2010;104:811–822 [DOI] [PubMed] [Google Scholar]
- 12.Rennenberg RJ, de Leeuw PW, Kessels AG, et al. Calcium scores and matrix Gla protein levels: association with vitamin K status. Eur J Clin Invest 2010;40:344–349 [DOI] [PubMed] [Google Scholar]
- 13.Shea MK, O’Donnell CJ, Vermeer C, et al. Circulating uncarboxylated matrix gla protein is associated with vitamin K nutritional status, but not coronary artery calcium, in older adults. J Nutr 2011;141:1529–1534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Westenfeld R, Krueger T, Schlieper G, et al. Effect of vitamin K2 supplementation on functional vitamin K deficiency in hemodialysis patients: a randomized trial. Am J Kidney Dis 2012;59:186–195 [DOI] [PubMed] [Google Scholar]
- 15.Theuwissen E, Cranenburg EC, Knapen MH, et al. Low-dose menaquinone-7 supplementation improved extra-hepatic vitamin K status, but had no effect on thrombin generation in healthy subjects. Br J Nutr 2012;108:1652–1657 [DOI] [PubMed] [Google Scholar]
- 16.Dalmeijer GW, van der Schouw YT, Vermeer C, Magdeleyns EJ, Schurgers LJ, Beulens JW. Circulating matrix Gla protein is associated with coronary artery calcification and vitamin K status in healthy women. J Nutr Biochem 2013;24:624–628 [DOI] [PubMed] [Google Scholar]
- 17.Dalmeijer GW, van der Schouw YT, Magdeleyns E, Ahmed N, Vermeer C, Beulens JW. The effect of menaquinone-7 supplementation on circulating species of matrix Gla protein. Atherosclerosis 2012;225:397–402 [DOI] [PubMed] [Google Scholar]
- 18.Schurgers LJ, Barreto DV, Barreto FC, et al. The circulating inactive form of matrix gla protein is a surrogate marker for vascular calcification in chronic kidney disease: a preliminary report. Clin J Am Soc Nephrol 2010;5:568–575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rennenberg RJ, van Varik BJ, Schurgers LJ, et al. Chronic coumarin treatment is associated with increased extracoronary arterial calcification in humans. Blood 2010;115:5121–5123 [DOI] [PubMed] [Google Scholar]
- 20.Schlieper G, Westenfeld R, Krüger T, et al. Circulating nonphosphorylated carboxylated matrix gla protein predicts survival in ESRD. J Am Soc Nephrol 2011;22:387–395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cranenburg EC, Brandenburg VM, Vermeer C, et al. Uncarboxylated matrix Gla protein (ucMGP) is associated with coronary artery calcification in haemodialysis patients. Thromb Haemost 2009;101:359–366 [PubMed] [Google Scholar]
- 22.Koos R, Krueger T, Westenfeld R, et al. Relation of circulating Matrix Gla-Protein and anticoagulation status in patients with aortic valve calcification. Thromb Haemost 2009;101:706–713 [PubMed] [Google Scholar]
- 23.Parker BD, Schurgers LJ, Vermeer C, Schiller NB, Whooley MA, Ix JH. The association of uncarboxylated matrix Gla protein with mitral annular calcification differs by diabetes status: The Heart and Soul study. Atherosclerosis 2010;210:320–325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Amos AF, McCarty DJ, Zimmet P. The rising global burden of diabetes and its complications: estimates and projections to the year 2010. Diabet Med 1997;14(Suppl. 5):S1–S85 [PubMed] [Google Scholar]
- 25.Lüscher TF, Creager MA, Beckman JA, Cosentino F. Diabetes and vascular disease: pathophysiology, clinical consequences, and medical therapy: Part II. Circulation 2003;108:1655–1661 [DOI] [PubMed] [Google Scholar]
- 26.Wu KK, Huan Y. Diabetic atherosclerosis mouse models. Atherosclerosis 2007;191:241–249 [DOI] [PubMed] [Google Scholar]
- 27.Schauer IE, Snell-Bergeon JK, Bergman BC, et al. Insulin resistance, defective insulin-mediated fatty acid suppression, and coronary artery calcification in subjects with and without type 1 diabetes: The CACTI study. Diabetes 2011;60:306–314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Beulens JW, Monninkhof EM, Verschuren WM, et al. Cohort profile: the EPIC-NL study. Int J Epidemiol 2010;39:1170–1178 [DOI] [PubMed] [Google Scholar]
- 29.Sluijs I, van der A DL, Beulens JW, et al. Ascertainment and verification of diabetes in the EPIC-NL study. Neth J Med 2010;68:333–339 [PubMed] [Google Scholar]
- 30.Herings RM, Bakker A, Stricker BH, Nap G. Pharmaco-morbidity linkage: a feasibility study comparing morbidity in two pharmacy based exposure cohorts. J Epidemiol Community Health 1992;46:136–140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wareham NJ, Jakes RW, Rennie KL, et al. Validity and repeatability of a simple index derived from the short physical activity questionnaire used in the European Prospective Investigation into Cancer and Nutrition (EPIC) study. Public Health Nutr 2003;6:407–413 [DOI] [PubMed] [Google Scholar]
- 32.Durrleman S, Simon R. Flexible regression models with cubic splines. Stat Med 1989;8:551–561 [DOI] [PubMed] [Google Scholar]
- 33.Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York, Wiley, 1987 [Google Scholar]
- 34.Ueland T, Gullestad L, Dahl CP, et al. Undercarboxylated matrix Gla protein is associated with indices of heart failure and mortality in symptomatic aortic stenosis. J Intern Med 2010;268:483–492 [DOI] [PubMed] [Google Scholar]
- 35.Ueland T, Dahl CP, Gullestad L, et al. Circulating levels of non-phosphorylated undercarboxylated matrix Gla protein are associated with disease severity in patients with chronic heart failure. Clin Sci (Lond) 2011;121:119–127 [DOI] [PubMed] [Google Scholar]
- 36.Johnson RC, Leopold JA, Loscalzo J. Vascular calcification: pathobiological mechanisms and clinical implications. Circ Res 2006;99:1044–1059 [DOI] [PubMed] [Google Scholar]
- 37.Abedin M, Tintut Y, Demer LL. Vascular calcification: mechanisms and clinical ramifications. Arterioscler Thromb Vasc Biol 2004;24:1161–1170 [DOI] [PubMed] [Google Scholar]
- 38.Vermeer C. Gamma-carboxyglutamate-containing proteins and the vitamin K-dependent carboxylase. Biochem J 1990;266:625–636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nishimoto SK, Nishimoto M. Matrix Gla protein C-terminal region binds to vitronectin. Co-localization suggests binding occurs during tissue development. Matrix Biol 2005;24:353–361 [DOI] [PubMed] [Google Scholar]
- 40.Cario-Toumaniantz C, Boularan C, Schurgers LJ, et al. Identification of differentially expressed genes in human varicose veins: involvement of matrix gla protein in extracellular matrix remodeling. J Vasc Res 2007;44:444–459 [DOI] [PubMed] [Google Scholar]
- 41.Hwang DM, Dempsey AA, Lee CY, Liew CC. Identification of differentially expressed genes in cardiac hypertrophy by analysis of expressed sequence tags. Genomics 2000;66:1–14 [DOI] [PubMed] [Google Scholar]
- 42.Rysä J, Leskinen H, Ilves M, Ruskoaho H. Distinct upregulation of extracellular matrix genes in transition from hypertrophy to hypertensive heart failure. Hypertension 2005;45:927–933 [DOI] [PubMed] [Google Scholar]
- 43.Mustonen E, Pohjolainen V, Aro J, et al. Upregulation of cardiac matrix Gla protein expression in response to hypertrophic stimuli. Blood Press 2009;18:286–293 [DOI] [PubMed] [Google Scholar]
- 44.Parker BD, Schurgers LJ, Brandenburg VM, et al. The associations of fibroblast growth factor 23 and uncarboxylated matrix Gla protein with mortality in coronary artery disease: the Heart and Soul Study. Ann Intern Med 2010;152:640–648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.International Diabetes Federation IDF Diabetes Atlas. Brussels, Belgium, 2011. Available from http://www.idf.org/diabetesatlas. Accessed 18 January 2013 [Google Scholar]
- 46.Lundman B, Engström L. Diabetes and it’s complications in a Swedish county. Diabetes Res Clin Pract 1998;39:157–164 [DOI] [PubMed] [Google Scholar]