Abstract
OBJECTIVE
Diabetes confers a very high risk of lower-extremity amputation (LEA); however, few studies have assessed whether blood glucose control can reduce LEA risk among patients with diabetes, especially in practice settings where low-income patients predominate.
RESEARCH DESIGN AND METHODS
We performed a prospective cohort study (2000–2009) on patients with diabetes that included 19,808 African Americans and 15,560 whites. The cohort was followed though 31 May 2012. Cox proportional hazards regression models were used to estimate the association of HbA1c with LEA risk.
RESULTS
During a mean follow-up of 6.83 years, 578 LEA incident cases were identified. The multivariable-adjusted hazard ratios of LEA associated with different levels of HbA1c at baseline (<6.0% [reference group], 6.0–6.9, 7.0–7.9, 8.0–8.9, 9.0–9.9, and ≥10.0%) were 1.00, 1.73 (95% CI 1.07–2.80), 1.65 (0.99–2.77), 1.96 (1.14–3.36), 3.02 (1.81–5.04), and 3.30 (2.10–5.20) (P trend <0.001) for African American patients with diabetes and 1.00, 1.16 (0.66–2.02), 2.28 (1.35–3.85), 2.38 (1.36–4.18), 2.99 (1.71–5.22), and 3.25 (1.98–5.33) (P trend <0.001) for white patients with diabetes, respectively. The graded positive association of HbA1c during follow-up with LEA risk was observed among both African American and white patients with diabetes (all P trend <0.001). With stratification by sex, age, smoking status, blood pressure, LDL cholesterol, BMI, use of glucose-lowering agents, and income, this graded association of HbA1c with LEA was still present.
CONCLUSIONS
The current study conducted in a low-income population suggests a graded association between HbA1c and the risk of LEA among both African American and white patients with type 2 diabetes.
Diabetes is considered the “epidemic of the 21st century,” affecting ~24 million individuals in the U.S. alone (1). Individuals with diabetes have a markedly increased risk of lower-extremity amputation (LEA) compared with individuals without diabetes (2,3). LEA ranks as the most feared adverse health outcome among people with diabetes because its impact on health and quality of life makes it difficult for the patients to return to leisure, educational, and employment activities. LEAs are very costly. The most recent data for care of diabetes revealed that in 2012, the cost to care for diabetes was 245 billion USD. Clearly, contributions to this cost include the care of those with complications, including amputation (4). In 2001, the direct costs of inpatient care and prostheses for the estimated 42,424 patients with diabetes undergoing LEA totaled 1.65 billion USD in the U.S. (5). As an important public health issue, LEA has drawn a great deal of attention from both the medical community and government, including Healthy People 2020, Agency for Healthcare Research and Quality, in an attempt to reduce the incidence of amputation (6,7). The incidence of LEA and LEA discharge rates declined significantly in the U.S. population (8,9).
Although several epidemiological studies report positive associations between glycemia and LEA (10–14), their conclusions are often tempered because of small sample sizes or short follow-up times. On the other hand, clinical trials have failed to provide conclusive evidence about glucose lowering and LEA risk because of the relatively low incidence of LEA (15–18). There is significant necessity to provide robust data to confirm the associations between glycemia and LEA in the population of patients with diabetes. We conducted a prospective epidemiological study with a large study sample of patients with diabetes and long follow-up time to detect the association between glycemia measured by HbA1c and the risk of LEA. In addition, most studies have only used a single baseline measurement of HbA1c to predict LEA risk, which may introduce potential bias from only baseline HbA1c measurement. A recent finding published in Diabetes Care (8) called our attention to racial disparities in LEA that suggested potential care differences or other factors implicated in LEA; however, very few studies have assessed the race-specific association of HbA1c with LEA risk. The aim of the current study is to examine the race-specific association between different levels of HbA1c at baseline and during follow-up with the risk of incident LEA among African American and white patients with diabetes in the Louisiana State University Hospital–Based Longitudinal Study (LSUHLS).
RESEARCH DESIGN AND METHODS
The Louisiana State University Health Care Services Division (LSUHCSD) operates seven public hospitals and affiliated clinics in Louisiana that provide quality medical care to the residents of Louisiana regardless of their income or insurance coverage (19–24). Overall, LSUHCSD facilities have served ~1.6 million patients (35% of the Louisiana population) since 1997. Administrative, anthropometric, laboratory, clinical diagnosis, and medication data collected at these facilities are available in electronic form for both inpatients and outpatients from 1997. Using these data, we have established the LSUHLS (19). A cohort of patients with diabetes was established by using the ICD-9 (code 250) through the LSUHLS database between 1 January 1999 and 31 December 2009. Both inpatients and outpatients were included, and all patients were under primary care. LSUHCSD’s internal diabetes disease-management guidelines call for physician confirmation of diabetes diagnoses by applying the American Diabetes Association criteria: a fasting plasma glucose level ≥126 mg/dL, 2-h glucose level ≥200 mg/dL after a 75-g 2-h oral glucose tolerance test, and one or more classic symptoms plus a random plasma glucose level ≥200 mg/dL (25). The first record of diabetes diagnosis was used to establish the baseline for each patient in the present analyses owing to the design of the cohort study. Before diagnosed with diabetes, these patients used our system for an average of 5.0 years. We validated the diabetes diagnosis in LSUHCSD hospitals. The agreement of diabetes diagnosis was 97%: 20,919 subjects of a sample of 21,566 hospital patients with discharge diagnoses based on ICD codes also had physician-confirmed diabetes by using the American Diabetes Association diabetes diagnosis criteria (25).
The current study included 35,368 patients with newly diagnosed diabetes (15,560 white and 19,808 African American) who were 30–94 years of age without a history of LEA and with complete repeated data on all risk factor variables. In these patients with diabetes, ~77.3% qualify for free care (by virtue of being low income and uninsured—any individual or family unit whose income is ≤200% of federal poverty level), ~4.9% of patients are self-pay (uninsured, but incomes not low enough to qualify for free care), ~5.2% of patients are covered by Medicaid, ~10.4% of patients have Medicare, and ~2.2% of patients are covered by commercial insurance. The study and analysis plan were approved by both the Pennington Biomedical Research Center and Louisiana State University Health Sciences Center Institutional Review Boards. We did not obtain informed consent from participants involved in our study because we used anonymized data compiled from electronic medical records.
Baseline and follow-up measurements
The patient’s characteristics, including age of diabetes diagnosis, sex, race/ethnicity, family income, smoking status, types of health insurance, body weight, height, BMI, blood pressure, total cholesterol, HDL cholesterol, LDL cholesterol, triglycerides, HbA1c, estimated glomerular filtration rate (eGFR), history and incidence of peripheral arterial disease, ulcer, and foot deformity, and medication (antihypertensive drugs, cholesterol-lowering drugs, and antidiabetes drugs) within half a year after the diabetes diagnosis (baseline) and during follow-up after the diabetes diagnosis (follow-up), were extracted from the computerized hospitalization records. Foot risk factors were identified using ICD-9 codes based on existing literature (26,27), which included peripheral arterial disease (ICD-9 codes 443.81, 440.2, 440.20, 440.21, 440.22, 440.23, 440.24, 440.29, 440.8, 440.9, 442.2, 442.3, 443.0, 443.1, 443.81, 443.89, 443.9, 444.22, 444.81, 2507.x, and 785.4), ulcer (ICD-9 codes 707.1x and 707.9), and foot deformity (ICD-9 codes 94.0, 713.5, 727.1, 735.0, 735.2, and 735.4–735.9). The updated mean values of HbA1c, LDL cholesterol, BMI, blood pressure, and eGFR over time were measured first at baseline and second as an updated mean of annual measurement, calculated for each participant from baseline to each year of follow-up. For example, at 1 year the updated mean is the average of the baseline and 1-year values and at 3 years it is the average of baseline, 1-year, 2-year, and 3-year values. In case of an event during follow-up, the period for estimating updated mean value was from baseline to the year before this event occurred (10,28). The average number of HbA1c measurements during the follow-up period was 7.4 times.
Prospective follow-up
Follow-up information was obtained from the LSUHLS inpatient and outpatient database by using the unique number assigned to every patient who visits the LSUHCSD hospitals. The diagnosis of LEA was the primary end point of interest of the study and was defined according to the ICD-9 (codes 84.10–84.17). Since 1997, diagnoses of LEA were made by the treating physicians based on a clinical assessment and examinations as considered relevant by the clinician in charge of treatments. Follow-up of each cohort member continued until the date of the diagnosis of LEA, the date of the last visit if the subject stopped use of LSUHCSD hospitals, death, or 31 May 2012.
Statistical analyses
The association between HbA1c and the risk of LEA was analyzed by using Cox proportional hazards models. HbA1c was evaluated in the following two ways: 1) as six categories (HbA1c <6.0% [42 mmol/mol] [reference group], 6.0–6.9% [42–52 mmol/mol], 7.0–7.9% [53–63 mmol/mol], 8.0–8.9% [64–74 mmol/mol], 9.0–9.9% [75–85 mmol/mol], and ≥10.0% [86 mmol/mol]) and 2) as a continuous variable. Different levels of HbA1c were included in the models as dummy variables, and the significance of the trend over different categories of HbA1c was tested in the same models by giving an ordinal numerical value for each dummy variable. All analyses were adjusted for age and sex and further for smoking, income, types of insurance, BMI, systolic blood pressure, LDL cholesterol, eGFR, peripheral arterial disease, ulcer, and foot deformity at baseline and during follow-up, use of antihypertensive drugs, use of diabetes medications, and use of cholesterol-lowering agents. When we analyzed the association between updated mean of HbA1c and LEA risk, we adjusted for updated means of BMI, LDL cholesterol, systolic blood pressure, and eGFR instead of baselines of these variables. For avoidance of the potential bias due to severe diseases at baseline, additional analyses were carried out excluding the subjects who were diagnosed with LEA during the first 2 years of follow-up. Statistical significance was considered to be P < 0.05. All statistical analyses were performed with PASW for Windows, version 20.0 (IBM SPSS, Chicago, IL) and SAS for Windows, version 9.3 (SAS Institute, Cary, NC).
RESULTS
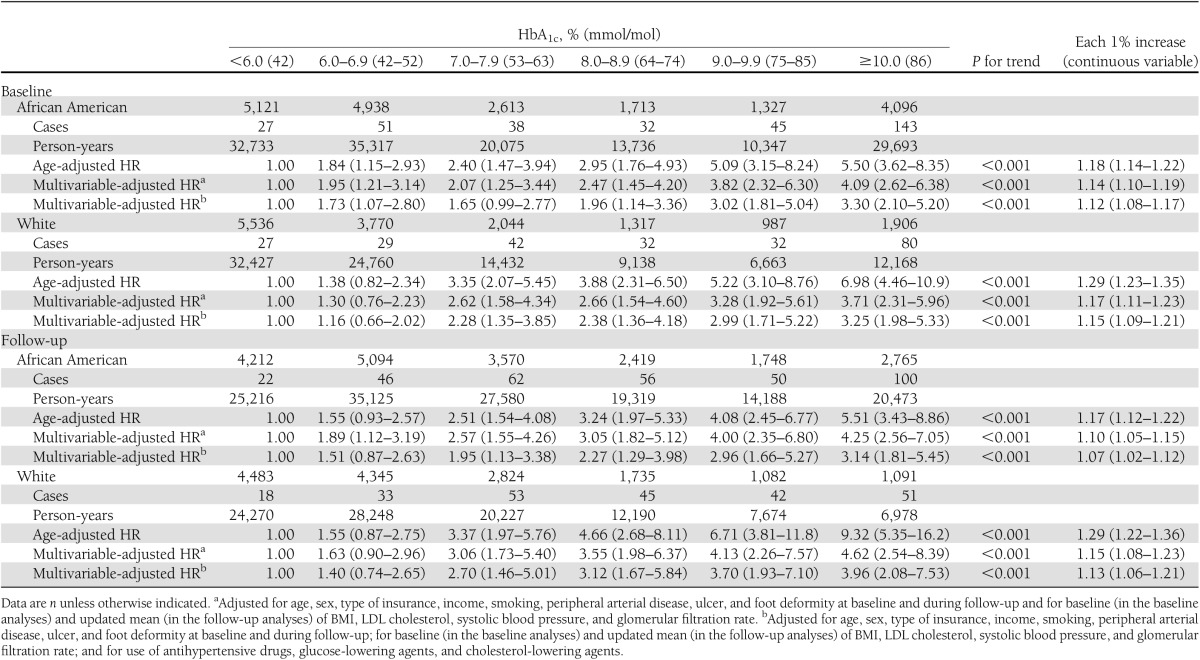
General characteristics of the study population are presented by race in Table 1. During a mean follow-up period of 6.83 years, 578 subjects (242 white and 336 African American) had an LEA. A significantly increased risk of LEA was observed among both African American and white patients with increasing baseline HbA1c (Table 2). After further adjustment for other confounding factors (smoking, income, type of insurance, BMI, systolic blood pressure, LDL cholesterol, eGFR, peripheral arterial disease, ulcer, and foot deformity at baseline and during follow-up and use of antihypertensive drugs, diabetes medications, and cholesterol-lowering agents), this graded association remained significant among white (Ptrend <0.001) and African American (Ptrend <0.001) patients with diabetes (Table 2). Each 1% increase in baseline HbA1c was associated with a 13% (95% CI 1.08–1.17) increased risk of LEA in African Americans and a 15% (95% CI 1.09–1.21) increased risk of LEA in whites. The risk of LEA associated with HbA1c was higher in white than African American patients with diabetes (χ2 = 17.8, df = 1, P for interaction <0.005).
Table 1.
Baseline characteristics of African American and white patients with diabetes
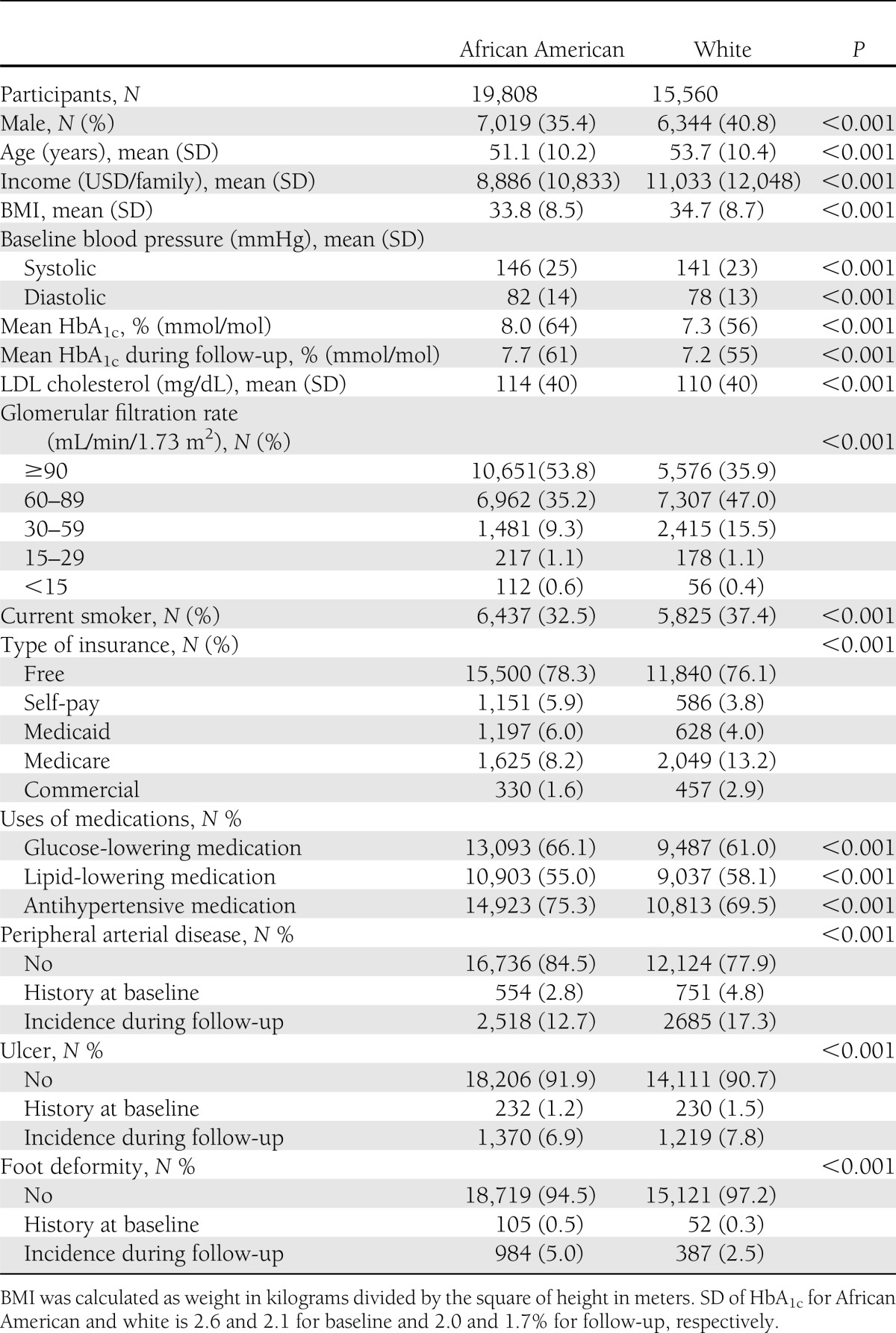
Table 2.
Hazard ratio (HR) (95% CI) of LEA according to different levels of HbA1c at baseline and during follow-up among African American and white patients with diabetes
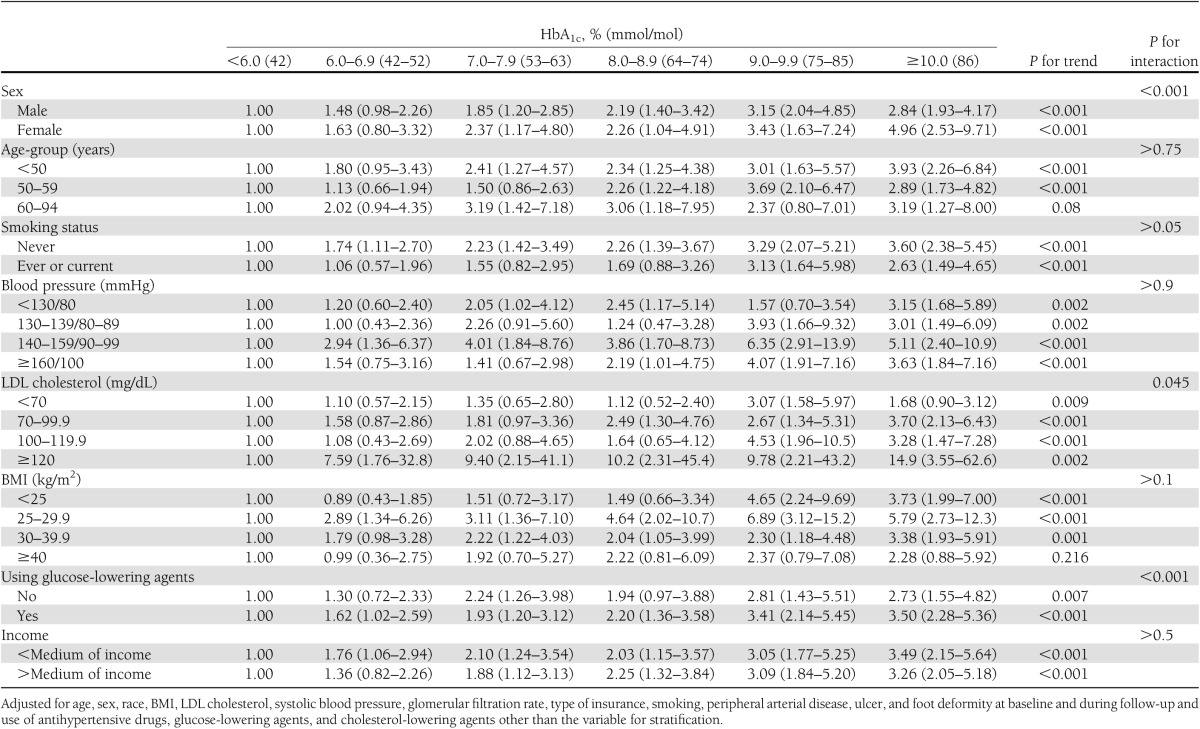
There was a significant interaction between sex and HbA1c on LEA risk (Table 3). When stratified by sex, the graded association of HbA1c at baseline with LEA risk was present and more significant in female patients with diabetes than male (P for interaction <0.001). When we stratified by age, smoking status, family income, blood pressure, LDL cholesterol, and BMI, the graded positive association of baseline HbA1c with LEA risk did not change (Table 3). Moreover, the graded positive association of HbA1c with LEA risk was also confirmed among patients with diabetes using glucose-lowering agents or not (all P trend<0.01) (Table 3).
Table 3.
Hazard ratio (HR) (95% CI) of LEA according to different levels of HbA1c at baseline among various subpopulations
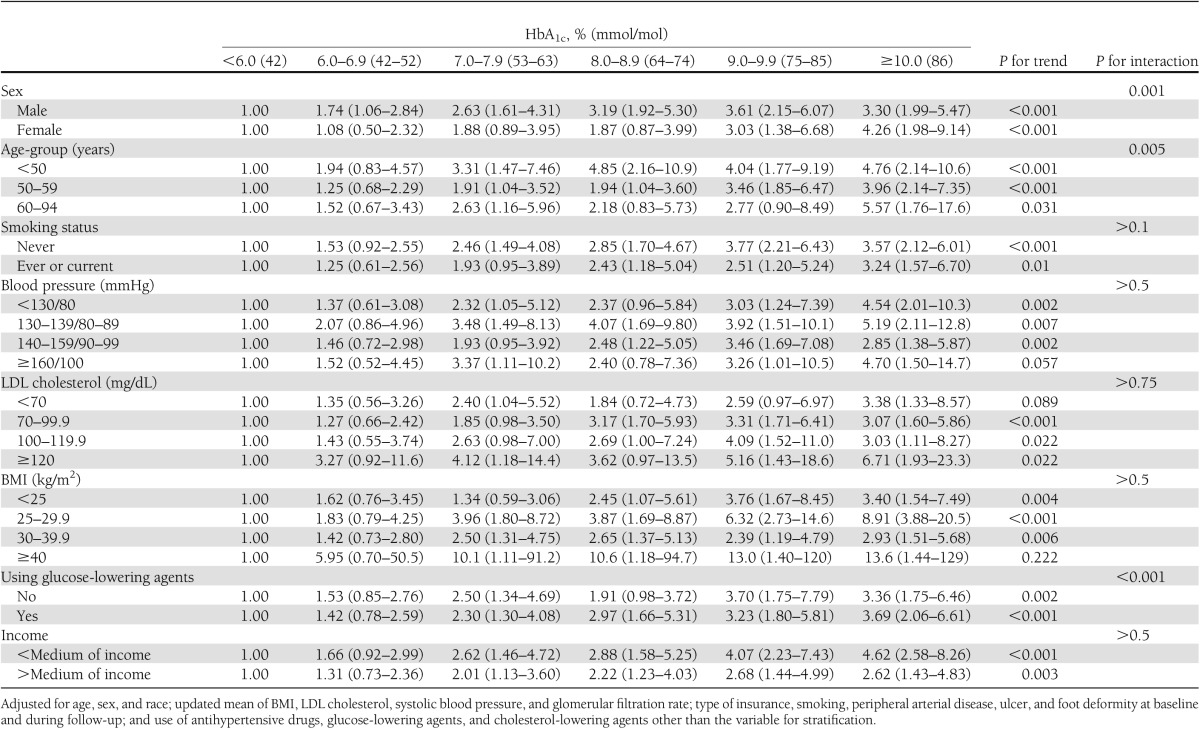
When we did an additional analysis by using an updated mean of HbA1c during follow-up, we found almost the same graded positive associations between baseline HbA1c levels and updated mean levels of HbA1c and LEA risk among both African American and white patients with diabetes (Tables 2 and 4). We did another analysis with the updated mean of HbA1c excluding baseline HbA1c. The mean of HbA1c decreased from 8.0% (64 mmol/mol) to 7.7% (61 mmol/mol) for African Americans and from 7.3% (56 mmol/mol) to 7.2% (55 mmol/mol) for whites, but the graded positive association between HbA1c and LEA did not change (Supplementary Table 1).
Table 4.
Hazard ratio (HR) (95% CI) of LEA according to different levels of HbA1c during follow-up among various subpopulations
After exclusion of the subjects who were diagnosed with LEA during the first 2 years of follow-up (n = 208), the multivariable-adjusted HRs of LEA associated with different levels of HbA1c did not change (data not shown).
CONCLUSIONS
Our study found a graded positive association between HbA1c at baseline and during follow-up and the risk of LEA among both African American and white patients with diabetes. This graded positive association was more significant in white than African American patients with diabetes.
LEA ranked first when participants rated their decrease in quality of life in the UK Prospective Diabetes Study (UKPDS) compared with other complications including blindness in one eye, stroke, heart failure, etc. (29). Health care providers encourage and strive to achieve good glycemic control for patients with diabetes; however, there are limited data on the specific effect of glycemic control on LEA risk among patients with diabetes. One meta-analysis of prospective studies demonstrated that there is a substantial increase in risk of LEA associated with hyperglycemia in individuals with diabetes (30); however, small sample sizes (1,044–3,642 participants), short follow-up (7–14 years), and few LEA cases (44–118 cases) in each study limit the statistical power for subgroup analyses. There are limited clinical trial data on the specific effect of glycemic control on LEA. In the PROspective pioglitAzone Clinical Trial In macroVascular Events (PROactive) study (18), there were 28 amputations among 2,605 participants in the pioglitazone group and 26 of 2,633 in the placebo group, and the event rate was lower in UKPDS than in PROactive (15,17). Thus, it is quite difficult for a previous single prospective study or clinical trial to provide conclusive evidence about glucose lowering and LEA risk (10,11,15–18). There is an urgent necessity to provide robust data to confirm the associations between glycemia control and LEA risk in the population with diabetes. In the current study, during a mean follow-up of 6.8 years, 578 LEA incident cases among 35,368 participants with diabetes were identified. We found a graded positive association by various HbA1c intervals of clinical relevance or by using HbA1c as a continuous variable at baseline and during follow-up with LEA risk among both African American and white patients with diabetes. In addition, we found that this graded positive association was present in patients with diabetes with and without glucose-lowering agent treatment and in patients with diabetes with different age, sex, smoking status, family income, blood pressure levels, LDL cholesterol, and BMI groups.
Potential explanations for the increased risk of LEA associated with hyperglycemia are likely to be mediated by number of mechanisms, which include but are not limited to peripheral sensory neuropathy, peripheral vascular disease, and soft-tissue sepsis. First, the importance of hyperglycemia in the development of peripheral neuropathy is well documented (31). Neuropathy is significantly associated with the presence of foot ulceration (32). Second, hyperglycemia contributes greatly to peripheral vessel disease in patients with diabetes (33). Finally, infection is present in the majority of foot ulcers, and hyperglycemia probably impairs host defense against infection. In the European Study Group on Diabetes and the Lower Extremity (Eurodiale) study (34), peripheral arterial disease was diagnosed in 49% of the subjects and infection in 58% among patients with diabetic foot ulcers. Patients with peripheral neuropathy often fail to notice minor trauma resulting in ulceration, infection, and nonhealing diabetic foot ulcers to the ultimate LEA. Therefore, poor glycemic control increases the risk for amputation. Improved glycemic control can potentially modify the risk of sensory neuropathy (35) and possibly the progression of peripheral arterial disease (36).
There are several strengths in our study, including the large sample size, high proportion of African Americans, long follow-up time, and use of administrative databases to avoid differential recall bias. We have used both baseline HbA1c levels and updated mean values of HbA1c during follow-up in the analyses, which can avoid potential bias from a single baseline measurement. In addition, participants in this study used the same public health care system, which minimizes the influence from the accessibility of health care, particularly when comparing African Americans and whites. One limitation of our study is that our analysis was not performed on a representative sample of the population, which limits the generalizability of the results; however, LSUHCSD hospitals are public hospitals and cover >1.6 million patients, most of whom are low-income persons in Louisiana. The results of the current study will have wide applicability for the population with low income and without health insurance in the U.S. Second, the validity of LEA diagnoses in our study has not been confirmed by specialists. However, the method using hospital discharge registers to diagnose LEA has been widely used in American and European cohort studies, such as the Kaiser Permanente Medical Care Program (37) and the U.K. Survey (38). The validity of the diagnoses of LEA by using hospital discharge registers in these cohort studies is available (agreement 97–99%) (37,38). Third, even though our analyses adjusted for an extensive set of confounding factors, residual confounding due to the measurement error in the assessment of confounding factors and unmeasured factors such as physical activity, education, and dietary factors cannot be excluded.
In summary, our study demonstrates that there is a graded association between HbA1c at baseline and during follow-up and the risk of LEA among both African American and white patients with diabetes. In the absence of conclusive evidence from randomized intervention trials, our study provides further epidemiological support for glucose lowering as a strategy to reduce amputation in patients with diabetes.
Supplementary Material
Acknowledgments
This work was supported by Louisiana State University’s Improving Clinical Outcomes Network.
No potential conflicts of interest relevant to this article were reported.
W.Z. wrote the manuscript and researched data. P.T.K. reviewed and edited the manuscript. R.H. and Y.W. researched data. J.J., S.B.H., W.T.C., and D.H.R. reviewed and edited the manuscript. G.H. wrote, reviewed, and edited the manuscript and researched data. G.H. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc13-0437/-/DC1.
References
- 1.Cowie CC, Rust KF, Ford ES, et al. Full accounting of diabetes and pre-diabetes in the U.S. population in 1988-1994 and 2005-2006. Diabetes Care 2009;32:287–294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Most RS, Sinnock P. The epidemiology of lower extremity amputations in diabetic individuals. Diabetes Care 1983;6:87–91 [DOI] [PubMed] [Google Scholar]
- 3.Humphrey LL, Palumbo PJ, Butters MA, et al. The contribution of non-insulin-dependent diabetes to lower-extremity amputation in the community. Arch Intern Med 1994;154:885–892 [PubMed] [Google Scholar]
- 4.American Diabetes Association Economic costs of diabetes in the U.S. in 2012. Diabetes Care 2013;36:1033–1046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gordois A, Scuffham P, Shearer A, Oglesby A, Tobian JA. The health care costs of diabetic peripheral neuropathy in the US. Diabetes Care 2003;26:1790–1795 [DOI] [PubMed] [Google Scholar]
- 6.Putting feet first in diabetes. Lancet 2005;366:1674. [DOI] [PubMed] [Google Scholar]
- 7.Jeffcoate W, Edmonds M, Rayman G, Shearman C, Stuart L, Turner B, Putting Feet First Implementation Group Putting feet first — national guidance at last. Diabet Med 2009;26:1081–1082 [DOI] [PubMed] [Google Scholar]
- 8.Li Y, Burrows NR, Gregg EW, Albright A, Geiss LS. Declining rates of hospitalization for nontraumatic lower-extremity amputation in the diabetic population aged 40 years or older: U.S., 1988-2008. Diabetes Care 2012;35:273–277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jeffcoate WJ, Margolis DJ. Incidence of major amputation for diabetes in Scotland sets a target for us all. Diabetes Care 2012;35:2419–2420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stratton IM, Adler AI, Neil HA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ 2000;321:405–412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Davis WA, Norman PE, Bruce DG, Davis TM. Predictors, consequences and costs of diabetes-related lower extremity amputation complicating type 2 diabetes: the Fremantle Diabetes Study. Diabetologia 2006;49:2634–2641 [DOI] [PubMed] [Google Scholar]
- 12.Moss SE, Klein R, Klein BE. The Wisconsin Epidemiologic Study of Diabetic Retinopathy. The 14-year incidence of lower-extremity amputations in a diabetic population. Diabetes Care 1999;22:951–959 [DOI] [PubMed] [Google Scholar]
- 13.Resnick HE, Carter EA, Sosenko JM, et al. Strong Heart Study Incidence of lower-extremity amputation in American Indians: the Strong Heart Study. Diabetes Care 2004;27:1885–1891 [DOI] [PubMed] [Google Scholar]
- 14.Lehto S, Rönnemaa T, Pyörälä K, Laakso M. Risk factors predicting lower extremity amputations in patients with NIDDM. Diabetes Care 1996;19:607–612 [DOI] [PubMed] [Google Scholar]
- 15.UK Prospective Diabetes Study (UKPDS) Group Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998;352:837–853 [PubMed] [Google Scholar]
- 16.Patel A, MacMahon S, Chalmers J, et al. ADVANCE Collaborative Group Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 2008;358:2560–2572 [DOI] [PubMed] [Google Scholar]
- 17.UK Prospective Diabetes Study (UKPDS) Group Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet 1998;352:854–865 [PubMed] [Google Scholar]
- 18.Dormandy JA, Charbonnel B, Eckland DJ, et al. PROactive investigators Secondary prevention of macrovascular events in patients with type 2 diabetes in the PROactive Study (PROspective pioglitAzone Clinical Trial In macroVascular Events): a randomised controlled trial. Lancet 2005;366:1279–1289 [DOI] [PubMed] [Google Scholar]
- 19.Li W, Wang Y, Chen L, et al. Increasing prevalence of diabetes in middle or low income residents in Louisiana from 2000 to 2009. Diabetes Res Clin Pract 2011;94:262–268 [DOI] [PubMed] [Google Scholar]
- 20.Wang Y, Chen L, Horswell R, et al. Racial differences in the association between gestational diabetes mellitus and risk of type 2 diabetes. J Womens Health (Larchmt) 2012;21:628–633 [DOI] [PubMed] [Google Scholar]
- 21.Wang Y, Chen L, Xiao K, et al. Increasing incidence of gestational diabetes mellitus in Louisiana, 1997-2009. J Womens Health (Larchmt) 2012;21:319–325 [DOI] [PubMed] [Google Scholar]
- 22.Zhang Y, Li W, Wang Y, et al. Increasing prevalence of hypertension in low income residents within Louisiana State University Health Care Services Division Hospital System. Eur J Intern Med 2012;23:e179–e184 [DOI] [PubMed] [Google Scholar]
- 23.Hu G, Horswell R, Wang Y, et al. Body mass index and the risk of dementia among Louisiana low income diabetic patients. PLoS ONE 2012;7:e44537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang Y, Katzmarzyk PT, Horswell R, et al. Racial disparities in diabetic complications in an underinsured population. J Clin Endocrinol Metab 2012;97:4446–4453 [DOI] [PubMed] [Google Scholar]
- 25.American Diabetes Association Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 1997;20:1183–1197 [DOI] [PubMed] [Google Scholar]
- 26.Tseng CL, Sambamoorthi U, Helmer D, et al. The association between mental health functioning and nontraumatic lower extremity amputations in veterans with diabetes. Gen Hosp Psychiatry 2007;29:537–546 [DOI] [PubMed] [Google Scholar]
- 27.Sohn MW, Budiman-Mak E, Stuck RM, Siddiqui F, Lee TA. Diagnostic accuracy of existing methods for identifying diabetic foot ulcers from inpatient and outpatient datasets. J Foot Ankle Res 2010;3:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cederholm J, Gudbjörnsdottir S, Eliasson B, Zethelius B, Eeg-Olofsson K, Nilsson PM, NDR Systolic blood pressure and risk of cardiovascular diseases in type 2 diabetes: an observational study from the Swedish national diabetes register. J Hypertens 2010;28:2026–2035 [DOI] [PubMed] [Google Scholar]
- 29.Clarke P, Gray A, Holman R. Estimating utility values for health states of type 2 diabetic patients using the EQ-5D (UKPDS 62). Med Decis Making 2002;22:340–349 [DOI] [PubMed] [Google Scholar]
- 30.Adler AI, Erqou S, Lima TA, Robinson AH. Association between glycated haemoglobin and the risk of lower extremity amputation in patients with diabetes mellitus-review and meta-analysis. Diabetologia 2010;53:840–849 [DOI] [PubMed] [Google Scholar]
- 31.Harati Y. Diabetic peripheral neuropathies. Methodist Debakey Cardiovasc J 2010;6:15–19 [DOI] [PubMed] [Google Scholar]
- 32.Lavery LA, Armstrong DG, Vela SA, Quebedeaux TL, Fleischli JG. Practical criteria for screening patients at high risk for diabetic foot ulceration. Arch Intern Med 1998;158:157–162 [DOI] [PubMed] [Google Scholar]
- 33.Selvin E, Wattanakit K, Steffes MW, Coresh J, Sharrett AR. HbA1c and peripheral arterial disease in diabetes: the Atherosclerosis Risk in Communities study. Diabetes Care 2006;29:877–882 [DOI] [PubMed] [Google Scholar]
- 34.Prompers L, Huijberts M, Apelqvist J, et al. High prevalence of ischaemia, infection and serious comorbidity in patients with diabetic foot disease in Europe. Baseline results from the Eurodiale study. Diabetologia 2007;50:18–25 [DOI] [PubMed] [Google Scholar]
- 35.The Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Research Group Retinopathy and nephropathy in patients with type 1 diabetes four years after a trial of intensive therapy. N Engl J Med 2000;342:381–389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.The Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Research Group Effect of intensive diabetes management on macrovascular events and risk factors in the Diabetes Control and Complications Trial. Am J Cardiol 1995;75:894–903 [DOI] [PubMed] [Google Scholar]
- 37.Karter AJ, Ferrara A, Liu JY, Moffet HH, Ackerson LM, Selby JV. Ethnic disparities in diabetic complications in an insured population. JAMA 2002;287:2519–2527 [DOI] [PubMed] [Google Scholar]
- 38.Morris AD, McAlpine R, Steinke D, et al. Diabetes and lower-limb amputations in the community. A retrospective cohort study. DARTS/MEMO Collaboration. Diabetes Audit and Research in Tayside Scotland/Medicines Monitoring Unit. Diabetes Care 1998;21:738–743 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


