Abstract
OBJECTIVE
To investigate risk of a recurrent cardiovascular event and its predictors in a population-based cohort.
RESEARCH DESIGN AND METHODS
Participants of the Hoorn Study who had experienced a first cardiovascular event after baseline (n = 336) were followed with respect to a recurrent event. Absolute risk of a recurrent event was calculated for individuals with normal glucose metabolism, intermediate hyperglycemia, and type 2 diabetes. Cox regression models were used to investigate which variables, measured before the first vascular event, predicted a recurrent event using the stepwise backward procedure.
RESULTS
During a median follow-up of 4.1 years, 44% (n = 148) of the population developed a recurrent vascular event. The rate of recurrent events per 100 person-years was 7.2 (95% CI 5.8–8.7) in individuals with normal glucose metabolism, compared with 9.8 (6.6–14.0) in individuals with intermediate hyperglycemia and 12.5 (8.5–17.6) in individuals with type 2 diabetes. Higher age (hazard ratio 1.02 [95% CI 1.00–1.04]), male sex (1.56 [1.08–2.25]), waist circumference (1.02 [1.02–1.03]), higher systolic blood pressure (1.01 [1.01–1.02]), higher HbA1c (%, 1.13 [0.97–1.31]/ mmol/mol, 1.01 [1.00–1.03]), and family history of myocardial infarction (1.38 [0.96–2.00]) predicted a recurrent cardiovascular event.
CONCLUSIONS
Individuals with type 2 diabetes, but not individuals with intermediate hyperglycemia, are at increased risk for a recurrent vascular event compared with individuals with normal glucose metabolism. In people with a history of cardiovascular disease, people at increased risk of a recurrent event can be identified based on the patient’s risk profile before the first event.
Due to aging, the increasing prevalence of obesity and diabetes worldwide, and improved care after a first cardiovascular event, the number of people at risk for a recurrent cardiovascular event is increasing (1).
High blood pressure levels, dyslipidemia, smoking, and type 2 diabetes are known risk factors for a first cardiovascular event in the general population, with addition of glycemic level (HbA1c) in individuals with diabetes (2–4). Also, individuals in a prediabetic state (elevated glucose levels) are at increased risk for a first cardiovascular event compared with individuals with normal glucose metabolism (5).
In 1998, the cumulative incidence of recurrent events in patients with and without type 2 diabetes was described (5). Since then, care after a first cardiovascular event has improved, which might have affected absolute risk of a recurrent event. Less is known about predictors of a recurrent cardiovascular event in the general population. In general, established risk factors for a first event have not been found to be predictive for a recurrent event regarding various outcomes (6–8).
In the current study, we investigated whether people in a prediabetic state as well as people with type 2 diabetes are at increased risk of a recurrent cardiovascular event compared with people with normal glucose metabolism. To enable identification of individuals at high risk for a recurrent event and consequently effectively target screening, predictors of a recurrent cardiovascular event were determined, based on the patient’s risk profile before the first event.
RESEARCH DESIGN AND METHODS
Study population
The Hoorn Study is a population-based cohort study of type 2 diabetes and diabetes complications in the general population (9). A random sample of inhabitants listed in the municipal registry of Hoorn was invited to participate in the study. The participation rate was 71%, and data on 2,484 Dutch Caucasian men and women 50–75 years of age were obtained at baseline in 1989.
For the current study, 612 participants were excluded as data on cardiovascular diseases before baseline and during follow-up of the study were not available because they moved out of the town of Hoorn or did not give consent for extracting information from medical records. Compared with participants with complete data on cardiovascular diseases, participants with missing data on cardiovascular diseases had a higher mean BMI (+0.4 kg/m2, P = 0.02) and higher mean LDL cholesterol level (+0.12 mmol/L, P = 0.04) and were more often women (+7.5%, P < 0.01) and more likely to smoke (+4.8%, P = 0.01). Participants of the Hoorn Study who developed the first cardiovascular event during follow-up and became at risk for a recurrent cardiovascular event were selected (n = 340). After exclusion of individuals with missing values for any of the potential predictor variables, 336 individuals remained for the analyses.
All participants provided written informed consent. Ethical approval for the study was obtained from the Ethical Review Committee of the VU University Medical Center Amsterdam.
Cardiovascular disease
For the selection of patients at risk, information on cardiovascular diseases during follow-up was used. Incidence of cardiovascular morbidity and cardiovascular mortality during follow-up were the end points of interest.
Incidence of cardiovascular disease or cardiovascular mortality during follow-up was assessed using medical records of general practitioners and the local hospital and was coded according to ICD-9. Vital status was obtained from the municipal administration registries, and causes of death were coded by reviewing death certificates. For the first cardiovascular event as well as the recurrent cardiovascular event, nonfatal cardiovascular disease was defined as myocardial infarction (ICD-9 code 410), angina pectoris (ICD-9 code 413), congestive heart failure (ICD-9 code 427 and 428–428.4), coronary heart disease (ICD-9 code 410–414, 8036, and 8038), or stroke (ICD-9 code 436). In addition, for the recurrent cardiovascular event, cardiovascular mortality was defined as ICD-9 codes 390–459 (diseases of the circulatory system) or 798 (sudden death, cause unknown) because sudden death in general is of cardiovascular origin (10).
Measurement of potential predictor variables
At baseline, fasting glucose concentration and 2-h postload glucose concentration after a 75-g oral glucose tolerance test were measured in plasma with the glucose dehydrogenase method (Merck, Darmstadt, Germany). For fasting glucose, the intra-assay coefficients of variation were 4.8 (normal glucose tolerance), 6.1 (impaired glucose tolerance), and 7.1% (diabetes). The interassay coefficient of variation was 1.4% (11). HbA1c was determined by ion-exchange high-performance liquid chromatography with a Modular Diabetes Monitoring System (Bio-Rad, Veenendaal, the Netherlands). Fasting and postload glucose concentrations and HbA1c for the diagnosis of type 2 diabetes were used to categorize participants according to the 2011 World Health Organization criteria (12). Individuals already treated for diabetes with insulin, oral hypoglycemic agents, or a physician-prescribed diet were categorized as known diabetic patients, irrespective of their glucose levels.
Weight and height were measured in barefooted participants wearing light clothing. BMI was calculated as weight (kg) divided by height squared (m2). Waist circumference was measured at the level midway between the lowest rib margin and the iliac crest. Hip circumference was measured at the widest level over the greater trochanters. The mean value of two measurements was used. Waist-to-hip ratio was calculated as waist circumference divided by hip circumference. Blood pressure was measured in a sitting position after 5 min of rest using a random-zero sphygmomanometer (Hawksley-Gelman, Lancing, Sussex, U.K.). Systolic and diastolic blood pressure were calculated as the mean of duplicate measurements. Serum lipids and lipoproteins were measured using enzymatic techniques (Boehringer-Mannheim, Mannheim, Germany) as described elsewhere (13). Information about cigarette smoking and family history of myocardial infarction and/or stroke and medication use was assessed by self-administered questionnaires. Family history was defined as positive when any of an individual’s parents, brothers, sisters, or children had a history of myocardial infarction or stroke before 60 years of age.
Statistical analysis
Baseline characteristics are presented as means ± SD or percentages and are compared between participants with and without a recurrent cardiovascular event during follow-up. Number of recurrent cardiovascular events per 100 person-years was calculated and compared between participants with normal glucose metabolism, intermediate hyperglycemia, and type 2 diabetes.
The following potential predictors obtained at the baseline screening, before the occurrence of the first event, were tested for prediction of a recurrent cardiovascular event during follow-up in a general population using multivariable Cox proportional hazards regression models: age at first cardiovascular event, sex, BMI, waist circumference, waist-to-hip ratio, systolic and diastolic blood pressure, total, LDL, and HDL cholesterol, triglycerides, fasting glucose, 2-h glucose, presence of intermediate hyperglycemia or type 2 diabetes, HbA1c, smoking status, and family history of myocardial infarction or stroke. All variables were entered into the Cox proportional hazards regression model, and nonsignificant variables (P > 0.2) were removed sequentially. In case of high similarity between variables (e.g., diabetes and HbA1c), the weakest predictor was removed from the analysis. The Cox proportional hazards assumption was confirmed by plotting log minus log survival curves.
Follow-up time was defined as the time between baseline measurement and recurrent cardiovascular event or January 2009, whichever came first. Participants with causes of death other than the one under study (n = 56) were censored. To test for informative censoring, i.e., whether censoring of participants was related to the probability of a recurrent cardiovascular event, Cox regression analysis was repeated after exclusion of individuals with a cause of death other than the one under study.
For all hazard ratios (HRs), 95% CIs were calculated. Statistical analyses were performed using SPSS version 15.0 for Windows.
RESULTS
Of the 336 people included in this study, 148 (44%) developed a recurrent cardiovascular event during follow-up, of whom 100 people (68%) survived the recurrent event. The first cardiovascular event occurred on average 8.0 years (SD 4.7) after baseline. In individuals with a first event, median duration of follow-up after the index event was 4.1 years (interquartile range 1.1–8.2), and 148 individuals (44.2%) developed a recurrent cardiovascular event. In the total population, there were 62 people with intermediate hyperglycemia (18.5%) and 47 people were diagnosed with type 2 diabetes (14.0%). Besides the 21 people who were already familiar with type 2 diabetes at baseline, 26 people were newly diagnosed with diabetes, based on fasting glucose level (n = 14) and/or 2-h glucose level (n = 16) and/or HbA1c (n = 7). Participants with a recurrent cardiovascular event during follow-up were, at baseline, older, had a higher waist circumference and waist-to-hip ratio, had a higher level of systolic blood pressure, diastolic blood pressure, fasting blood glucose, and HbA1c, and were more likely to have diabetes than those without (Table 1). In participants with a recurrent cardiovascular event, the number of people with diabetes using glucose-lowering medication was higher compared with participants without a recurrent event. This difference between the two groups reflects a (nonsignificant) difference in the number of known diabetes cases at baseline in people with a recurrent event (48.3%) and people without a recurrent event (38.9%) compared with people with screening-detected diabetes.
Table 1.
Baseline characteristics of the population at risk for a recurrent cardiovascular event

The number of recurrent cardiovascular events per 100 person-years was 7.2 (95% CI 5.8–8.7) in individuals with normal glucose metabolism compared with 9.8 (6.6–14.0) in individuals with intermediate hyperglycemia and 12.4 (8.5–17.6) in individuals with type 2 diabetes at baseline. The number of people in whom the recurrent event was fatal was not significantly different between people with normal glucose metabolism (32.6%), intermediate hyperglycemia (29.6%), or type 2 diabetes (34.5%) (P = 0.93).
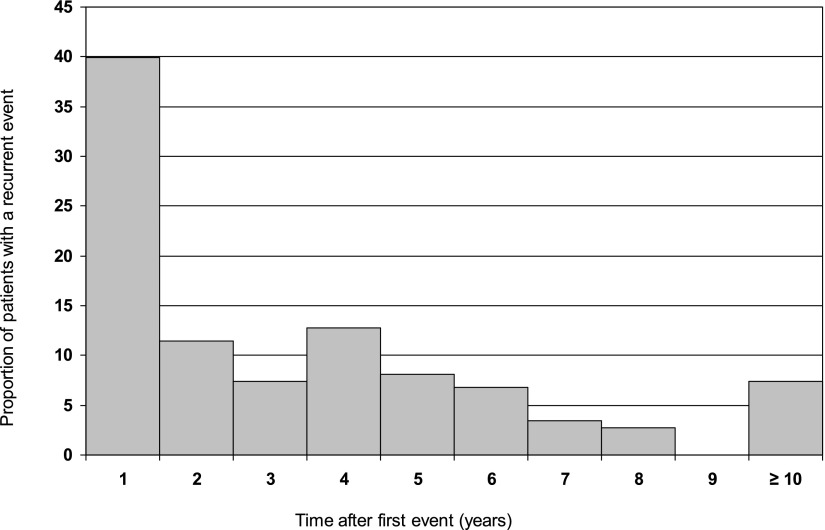
Figure 1 shows the proportion of patients that developed a recurrent event during each year of follow-up after the first event. In the population with the first cardiovascular event after baseline, 76 (51%) of the participants developed a recurrent event within 2 years after the first event. No differences were found between predictors of an early recurrent event compared with a recurrent event after 2 years or more (data not shown).
Figure 1.
Time between first and recurrent cardiovascular event.
In univariable Cox proportional hazards regression analysis, higher age at time of the first cardiovascular event, male sex, higher levels of systolic blood pressure, diastolic blood pressure, fasting blood glucose, HbA1c, and BMI, former smoker, type 2 diabetes, and family history of a myocardial infarction were significant predictors for a recurrent cardiovascular event. Presence of intermediate hyperglycemia was associated with a higher risk of a recurrent cardiovascular event compared with normal glucose metabolism; however, this relationship was not statistically significant (HR 1.14 [95% CI 0.79–1.65]). Because of high similarity between fasting and 2-h blood glucose, HbA1c, and presence of type 2 diabetes, fasting and 2-h blood glucose and presence of type 2 diabetes were excluded from the model. Multivariable Cox proportional hazards regression analysis revealed that higher age (1.02 [1.00–1.04]), male sex (1.56 [1.08–2.25]), waist circumference (1.02 [1.00–1.03]), higher systolic blood pressure (1.01 [1.01–1.02]), higher level of HbA1c (%, 1.13 [0.97–1.31]/mmol/mol, 1.01 [1.00–1.03]), and a family history of myocardial infarction (1.38 [0.96–2.00]) predicted a recurrent cardiovascular event (Table 2).
Table 2.
Multivariable model with predictors of a recurrent cardiovascular event during follow-up in the general population
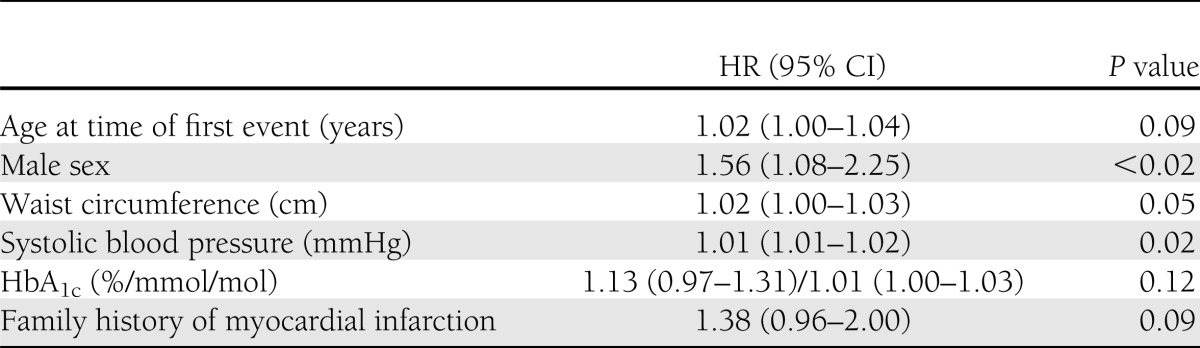
Repeating the analysis after exclusion of individuals who died of a cause other than cardiovascular, the same variables significantly predicted a recurrent event: age at time of first event (HR 1.03 [95% CI 1.00–1.05]), male sex (1.57 [1.05–2.35]), waist circumference (1.02 [1.00–1.04]), systolic blood pressure (1.01 [1.00–1.02]), HbA1c (%, 1.21 [1.01–1.46]/mmol/mol, 1.02 [1.00–1.04]), and family history of myocardial infarction (1.56 [1.04–2.33]).
CONCLUSIONS
In this population-based cohort study, 44.2% of the population developed a second cardiovascular event during a median of 4.1 years of follow-up after the first event. Risk of a recurrent cardiovascular event was similar between individuals with normal glucose metabolism and intermediate hyperglycemia and increased in individuals with type 2 diabetes compared with individuals without diabetes. Age at time of first event, male sex, waist circumference, systolic blood pressure, HbA1c, and family history of myocardial infarction were positively associated with a recurrent cardiovascular event in the general population.
The incidence rate was ∼60% higher in individuals with diabetes compared with nondiabetic individuals. In 1998, Haffner et al. (5) reported that the risk of a myocardial infarction, stroke, or cardiovascular death in individuals with a prior myocardial infarction was 2.6–2.8 times higher in individuals with diabetes than in individuals without diabetes. Compared with the results of Haffner et al., the current study showed a remarkably lower risk of a recurrent event in individuals with diabetes, which is still considerably high compared with individuals with normal glucose metabolism. Differences in absolute risk of a recurrent event between the two studies might be explained by differences in diabetes care or differences in characteristics of the population between the two regions. Improved care after a first cardiovascular event might have caused a lower incidence rate. Individuals with intermediate hyperglycemia are at increased risk of a first cardiovascular event compared with individuals with normal glucose metabolism (14). In contrast, risk of a recurrent cardiovascular event was not increased in individuals with intermediate hyperglycemia compared with individuals with normal glucose metabolism. The occurrence of a first event in individuals with intermediate hyperglycemia might have led to an early diagnosis of diabetes or early treatment of risk factors, resulting in a lower risk of a recurrent event comparable to individuals with normal glucose metabolism.
Cholesterol levels were not predictive of a recurrent event in this general population, which was also found in a recent study investigating predictors for a recurrent cardiovascular disease in type 2 diabetic patients (15). The Framingham model for estimation of risk of a subsequent coronary heart disease within 2 years included, among others, total and HDL cholesterol level (16). In recurrence risk research, individuals are selected based on the occurrence of the first event similar to the recurrent event, which has an effect on the distribution of risk factors in the selected population. Therefore, the relative risk of predictors for a recurrent event can be lower compared with the relative risk of a predictor for a first event (17).
In the interpretation of the results of this study, some limitations must be taken into account. First, the small sample size could have led to wide confidence intervals leading to nonsignificant associations. However, according to the suggestion of 10–15 cases or noncases per predictor included in the model (18), our sample size should have been sufficient for a precise estimate. Second, predictors of a recurrent cardiovascular event were obtained before occurrence of the first event. Risk factor levels might have altered after the first event as a result of treatment initiation, possibly leading to an underestimation of the magnitude of the predictors. Nevertheless, patients at increased risk of a recurrent event can be identified. Third, a substantial number of the people with diabetes were detected during the baseline screening, which explains the small number of people with diabetes receiving glucose-lowering medication at baseline. Mean duration of diabetes might be lower and risk profile might be less severe compared with the entire diabetes population, limiting generalizability of the study results. Fourth, because of the long follow-up of this population-based cohort study, noncardiovascular mortality rate was relatively high. In Cox regression analysis, individuals dying from other causes of death are assumed to be similar to surviving participants. Sensitivity analysis after exclusion of individuals with other causes of death did not change the selection of predictors but increased the magnitude of the predictors. Finally, information on morbidity and mortality was not available for all participants of the Hoorn Study. We compared cardiovascular risk factor levels of participants who gave permission with participants who did not give permission for registry. We did not observe major differences in risk factor levels at baseline between these two groups, reducing the chance that the internal validity was affected by these missing values on the outcome measure.
In this study, we investigated the number of recurrent cardiovascular events in a population-based cohort, including information on the rate of recurrent cardiovascular events in people with intermediate hyperglycemia and predictors of recurrent events in this population-based cohort. The results of this study indicate that individuals with type 2 diabetes are at increased risk for a recurrent cardiovascular event compared with individuals with normal glucose metabolism. This increased risk was not seen in individuals with intermediate hyperglycemia compared with individuals with normal glucose metabolism. In people with a history of cardiovascular disease, people at increased risk of a recurrent cardiovascular event can be identified based on the patient’s risk profile before the first event.
Acknowledgments
The Hoorn Study has been made possible by Vrije Universiteit Amsterdam, the VU University Medical Center, the Dutch Diabetes Research Foundation, the Dutch Organization for Scientific Research, the Netherlands Heart Foundation, and the Health Research and Development Council of the Netherlands.
No potential conflicts of interest relevant to this article were reported.
A.A.W.A.v.d.H. researched data and wrote the manuscript. E.v.R., S.D.M.B., S.C.C., and C.A.B. contributed to discussion and reviewed and edited the manuscript. C.D.A.S., J.M.D., and G.N. conceived and designed the study and reviewed and edited the manuscript. A.A.W.A.v.d.H. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Whiting DR, Guariguata L, Weil C, Shaw J. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract 2011;94:311–321 [DOI] [PubMed] [Google Scholar]
- 2.Conroy RM, Pyörälä K, Fitzgerald AP, et al. SCORE project group Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J 2003;24:987–1003 [DOI] [PubMed] [Google Scholar]
- 3.Stevens RJ, Kothari V, Adler AI, Stratton IM, United Kingdom Prospective Diabetes Study (UKPDS) Group The UKPDS risk engine: a model for the risk of coronary heart disease in type II diabetes (UKPDS 56). Clin Sci (Lond) 2001;101:671–679 [PubMed] [Google Scholar]
- 4.Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation 1998;97:1837–1847 [DOI] [PubMed] [Google Scholar]
- 5.Haffner SM, Lehto S, Rönnemaa T, Pyörälä K, Laakso M. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med 1998;339:229–234 [DOI] [PubMed] [Google Scholar]
- 6.Baglin T. Unraveling the thrombophilia paradox: from hypercoagulability to the prothrombotic state. J Thromb Haemost 2010;8:228–233 [DOI] [PubMed] [Google Scholar]
- 7.Gruberg L, Mercado N, Milo S, et al. Arterial Revascularization Therapies Study Investigators Impact of body mass index on the outcome of patients with multivessel disease randomized to either coronary artery bypass grafting or stenting in the ARTS trial: the obesity paradox II? Am J Cardiol 2005;95:439–444 [DOI] [PubMed] [Google Scholar]
- 8.Kent DM, Thaler DE. Is patent foramen ovale a modifiable risk factor for stroke recurrence? Stroke 2010;41(Suppl.):S26–S30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mooy JM, Grootenhuis PA, de Vries H, et al. Prevalence and determinants of glucose intolerance in a Dutch Caucasian population. The Hoorn Study. Diabetes Care 1995;18:1270–1273 [DOI] [PubMed] [Google Scholar]
- 10.Kannel WB, Plehn JF, Cupples LA. Cardiac failure and sudden death in the Framingham Study. Am Heart J 1988;115:869–875 [DOI] [PubMed] [Google Scholar]
- 11.Mooy JM, Grootenhuis PA, de Vries H, et al. Intra-individual variation of glucose, specific insulin and proinsulin concentrations measured by two oral glucose tolerance tests in a general Caucasian population: the Hoorn Study. Diabetologia 1996;39:298–305 [DOI] [PubMed] [Google Scholar]
- 12.World Health Organization. Use of Glycated Haemoglobin (HbA1c) in the Diagnosis of Diabetes Mellitus. Abbreviated Report of a WHO Consultation Geneva, World Health Org., 2011 (WHO/NMH/CHP/CPM/11.1) [PubMed]
- 13.de Vegt F, Dekker JM, Ruhé HG, et al. Hyperglycaemia is associated with all-cause and cardiovascular mortality in the Hoorn population: the Hoorn Study. Diabetologia 1999;42:926–931 [DOI] [PubMed] [Google Scholar]
- 14.Haffner SM, Stern MP, Hazuda HP, Mitchell BD, Patterson JK. Cardiovascular risk factors in confirmed prediabetic individuals. Does the clock for coronary heart disease start ticking before the onset of clinical diabetes? JAMA 1990;263:2893–2898 [DOI] [PubMed] [Google Scholar]
- 15.Giorda CB, Avogaro A, Maggini M, et al. Diabetes and Informatics Study Group Recurrence of cardiovascular events in patients with type 2 diabetes: epidemiology and risk factors. Diabetes Care 2008;31:2154–2159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.D'Agostino RB, Russell MW, Huse DM, et al. Primary and subsequent coronary risk appraisal: new results from the Framingham study. Am Heart J 2000;139:272–281 [DOI] [PubMed]
- 17.Dahabreh IJ, Kent DM. Index event bias as an explanation for the paradoxes of recurrence risk research. JAMA 2011;305:822–823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Peduzzi P, Concato J, Feinstein AR, Holford TR. Importance of events per independent variable in proportional hazards regression analysis. II. Accuracy and precision of regression estimates. J Clin Epidemiol 1995;48:1503–1510 [DOI] [PubMed] [Google Scholar]