Abstract
Research suggests that loss of control (LOC) while eating (the sense that one cannot control what or how much one is eating) is a more salient feature of binge eating than the amount of food consumed. This study examined the unique contributions of LOC and episode size to negative affect surrounding eating episodes in binge eating disorder (BED) and obesity. Twenty-two obese adults with (n = 9) and without (n = 13) BED completed daily records of eating patterns and mood using ecological momentary assessment (EMA). Linear mixed modeling revealed that across groups, greater premeal self-reported LOC was associated with higher premeal negative affect independent of episode size. For individuals with BED, greater premeal self-reported LOC was associated with higher postmeal negative affect, regardless of the amount of food eaten, whereas for obese controls, the combination of LOC and consumption of large amounts of food was associated with lower postmeal negative affect. Results indicate that LOC, but not the quantity of food consumed, is associated with momentary distress related to aberrant eating in BED. Findings also highlight the need for further research investigating the emotional context surrounding aberrant eating in obese individuals without BED.
Recurrent binge eating is the hallmark feature of binge eating disorder (BED) and bulimia nervosa, two disorders characterized by considerable impairment and distress (1). Binge eating is strongly associated with obesity and weight gain (2), marking it as a behavior that is particularly relevant to study in obese samples. In accordance with the Diagnostic and Statistical Manual of Mental Disorders 1–4th Edition, binge eating episodes must consist of an unambiguously large amount of food accompanied by a sense of loss of control (LOC) over eating (i.e., objective binge eating (3)). Thus, individuals reporting subjective binge eating (i.e., consumption of an amount of food that is not unambiguously large, but is viewed as excessive by the respondent, accompanied by LOC (4)) would not meet the binge eating criterion for either of these disorders. However, research suggests that LOC is the most salient aspect of binge eating (5), and that this feature is more strongly associated with psychiatric symptomatology than the quantity of food consumed (6). To date, however, no research has systematically explored whether momentary precursors and consequences of aberrant eating episodes differ depending on the presence or absence of LOC and/or the consumption of unambiguously large amounts of food. As LOC eating is prevalent among obese individuals without eating disorders (7) and is related to psychiatric impairment independent of episode size as noted above (6), it is important to characterize the precipitants and consequences of this behavior in obesity even in the absence of BED.
The importance of quantity (i.e., consumption of an unambiguously large amount of food vs. an amount of food that is not unambiguously large) vs. subjective experience (i.e., presence or absence of LOC) of aberrant eating episodes has long been a source of contention in the eating disorders literature (8). Early studies show that binge eating episodes in bulimia nervosa often consist of relatively small amounts of food (i.e., fewer than 500–600 kilocalories; (9,10)), but that these episodes are nevertheless associated with as much momentary distress as eating episodes meeting the operational criteria for binge eating. Other research suggests that within both clinical and community samples, LOC, rather than episode size, accounts for the severity of eating disorder symptoms, psychiatric comorbidity, interpersonal dysfunction, and treatment-seeking behavior (11-14); however, it is currently unknown whether similar associations exist with regard to immediate distress surrounding eating episodes. Taken together, these findings suggest that the current diagnostic scheme for BED and bulimia nervosa may fail to capture a significantly impaired subset of the population who consequently may not receive adequate clinical attention for their eating disturbances. The current literature could be further strengthened by examining the unique contributions of self-reported LOC and episode size to the experience of momentary distress in the context of aberrant eating.
Binge eating episodes frequently occur against a backdrop of negative affect. According to affect regulation theories, binge eating may provide an escape from aversive emotions and subsequent self-awareness (15), or enable a “trade-off” whereby distressing emotional antecedents to binge eating (e.g., anxiety) are replaced by less distressing emotions consequent to binge eating (e.g., regret (16)). Affect regulation theories have been supported by both self-report and experimental data in individuals with BED (e.g., refs 5,17,18). However, these studies are often constrained by retrospective recall biases or by the use of an artificial setting. Over the past decade, ecological momentary assessment (EMA) methodology has been used to study the relation between mood and binge eating prospectively in the natural environment. EMA studies consistently demonstrate that binge eating in BED is preceded by the experience of negative emotions (19-23). Yet, the literature is less consistent regarding affective consequences of binge eating, with one study showing a slight (but nonsignificant) decrease in negative emotions immediately following a binge episode (19), and others showing an increase in postbinge negative affect (22,23). It is currently unclear whether antecedents and consequences vary according to objective size of an eating episode and/or the subjective experience of reported aberrant eating episodes. EMA methodology is well-suited to address this research question because of its ability to assess mood and eating behavior in “real time.”
One unanticipated finding in the EMA literature has been the degree to which binge eating occurs among obese individuals without a full diagnosis of BED. Indeed, in one early study ~2/3 of obese control participants self-reported binge eating during the EMA assessment timeframe (20), and another study reported no differences between BED and control groups in the frequency of self-identified binge eating episodes (21). Moreover, in contrast to laboratory-based studies which have found that individuals with BED consume more food during binge meals than obese controls (24,25), Greeno and colleagues (20) found no differences between obese individuals with and without BED in terms of the kilocalorie content of self-reported binge meals using EMA. These unexpected findings may be related to reliance on respondent’s subjective perception, rather than standardized investigator-based criteria, to identify binge eating episodes. Indeed, recent work by our group (26) demonstrated that when EMA data were augmented by the use of 24-h dietary recall to quantify eating episodes, individuals with BED reported significantly more binge eating episodes during a 1-week period than obese controls. Nevertheless, these studies suggest that aberrant eating is prevalent among obese individuals, even in the absence of BED.
The aim of the current study was to examine, within a sample of obese adults with and without BED, precursors to and consequences of aberrant eating episodes characterized by the presence of LOC, consumption of an unambiguously large amount of food, or the combination of both. Based on the previous literature (19-23), we hypothesized that LOC would be a strong predictor of pre- and postepisode negative affect whereas the amount of food consumed would not. We further hypothesized that the interaction between LOC and the amount of food consumed would not improve the prediction of postepisode negative affect beyond the independent effects of LOC, as consistent with prior data (11-14). To our knowledge, no other study has investigated whether the immediate emotional context surrounding aberrant eating varies according to the subjective experience and/or quantity of eating episodes.
METHODS AND PROCEDURES
Participants
Data were collected as part of a larger study of binge eating behavior among obese adults with BED, obese adults without BED, and nonobese adults without BED (26). Obese adults (BMI (kg/m2) >30) with and without BED were recruited through community and university flyers, and referrals from an eating disorders treatment facility. Individuals were excluded due to pregnancy or breastfeeding, a current diagnosis of a psychotic disorder, previous gastrointestinal surgery, any medical illness requiring dietary modification, the use of medications associated with weight or eating change, concurrent treatment for BED, suicidal ideation, purging, and inability to read English. Inclusion and exclusion criteria were assessed during the phone screen (see “Procedures” section). A total of 75 participants were screened for the study, 40 of whom were enrolled, provided 1-day trial data (see “Procedures” section), and completed the EMA protocol (this number includes the non-obese participants without BED whose data were excluded from the current study). Two participants were excluded from data analyses for what appeared to be invalid EMA data. This left a total sample of 38 participants in the overall study, of whom 22 were included in the current study. Participants received $100 for study participation and were offered another $50 for attending all scheduled appointments. This study was approved by the University of North Dakota Institutional Review Board.
Procedures
Interested participants completed a phone screen to ascertain BED status. The phone screen consisted of assessing eating behaviors over the past month using the eating disorder module from the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders, 4th Edition Axis I Disorders/Patient Edition (SCID-I/P; (27)) supplemented by probes from the Eating Disorder Examination (4). Phone screens were administered by master’s-level assessors who were trained in the SCID-I/P and the Eating Disorder Examination.
After study eligibility was determined, participants attended an informational session at the research facility during which they provided written informed consent. Participants then received thorough instructions on how to use the handheld computer (Handspring Visor) for the EMA assessment protocol. Participants were instructed to complete EMA recordings of mood and eating behavior each time they initiated an eating episode; each time they completed an eating episode; before bedtime; and in response to six semi-random prompts by investigators, which occurred every 2–3 h between 8:00 AM and 10:00 PM (28). Each participant completed a 1-day trial period to ensure that they understood EMA procedures; trial data were not included in the analyses.
All 22 participants came to the research facility almost every day during the 7-day data collection period. In-person assessments for weekends were typically completed on Mondays. During these assessments, data from the handheld computer were uploaded and monitored for compliance, and research coordinators provided feedback to participants about the quality of the data. Missed EMA assessments were discussed and the research coordinator and participant attempted to problem-solve any issues that limited compliance with the protocol. The eating recordings were then used to interview the participants about their dietary intake.
Measures
EMA
For the 7-day EMA protocol, each participant was asked to rate mood, stress, hunger, and level of control over eating immediately before and after any eating episode. Negative mood was assessed using the Positive and Negative Affect Scale (29). The Negative Affect Scale comprised the sum of five items (afraid, scared, upset, distressed, and jittery), all of which were rated on a 5-point scale, with a score of “1” indicating “Not at all” and a score of “5” indicating “Extremely” for each mood state. LOC assessment was based on the construct as described in the Eating Disorder Examination. That is, during the EMA orientation period discussed above, participants were instructed that LOC refers to the feeling that one cannot control what or how much one is eating, or the experience of feeling driven or compelled to start or continue eating. Ratings for premeal LOC (“Please rate how much control you currently feel over your eating”) were made on a 1- to 5-point Likert-type scale. A rating of 1 on the scale corresponded to “Complete control” and a five signified “Complete LOC”; postmeal, participants responded to a “yes/no” question as to whether they had experienced LOC while eating. For the current study, we opted to utilize LOC ratings prior to the eating episode to limit retrospective recall bias and to allow for examination of the full range of experience of LOC (i.e., use of a continuous vs. categorical variable). LOC ratings prior to eating episodes were significantly associated with those reported after eating episodes (t (463) = 8.20; P < 0.001), indicating that if individuals reported feelings of LOC before initiating an eating episode, they were likely to report having experienced LOC upon completing the episode as well.
Eating behavior
Upon presenting to the research institute each day, participants were queried about the details of each eating episode recorded on their handheld computer, as well as if they had forgotten to record any eating episodes. Next, the Nutritional Data System for Research (30) was used to generate nutritional intake data for each reported eating episode. The Nutritional Data System for Research is an interviewer-based assessment that provides nutrient intake data for foods eaten over a 24-h time interval. It has been described as the gold standard method of assessing food intake in the natural environment (31), and it has been used successfully for research in overweight and obese samples (32). Following each Nutritional Data System for Research interview, the nutritional data of interest were merged with the time-stamped EMA data in order to create a temporal profile of eating episodes and LOC ratings for the previous day.
Statistical analysis
Data were analyzed using SPSS 18.0. All analyses included participants with and without BED. A linear mixed model approach was used to examine the relation between the dependent variable of momentary mood, and the independent variables of LOC, episode size (i.e., kilocalorie content of eating episodes), and group. Mixed-effects analyses were based on a general linear model with a random intercept and random effect for study day. Serial correlation between observations was modeled using a heterogeneous first-order autoregressive structure. Two mixed model regressions were run: the first model examined premeal negative mood state, while the second model examined postmeal negative mood state. The second model controlled for premeal negative mood state. For each model, we tested all two- and three-way interactions among the independent variables. The intraclass correlation coefficient for the premeal negative affect model was 0.38 and for the postmeal negative affect model was 0.14.
RESULTS
Descriptive characteristics
Participants were 22 obese (M BMI = 38.90 ± 8.67) adults (86.4% female; n = 19), 9 of whom met criteria for BED and 13 of whom served as non-BED controls. Participants were 35.7 years old, on average (s.d. = 11.9), and described themselves as white (90.9%; n = 20), black (4.5%; n = 1), or American Indian/Alaska Native (4.5%; n = 1). Due to the small sample size and the relative homogeneity of the sample, demographic comparisons were not conducted.
A total of 2,009 separate EMA recordings were provided by the 22 participants over 166 separate participant days, which included 566 premeal recordings, 477 postmeal recordings, 838 responses to semi-random prompts (out of a possible total of 924 responses (six signals per day over the 7-day study period for each of 22 participants); 90.7%), and 128 before-bedtime recordings (out of a possible total of 154 recordings (one recording per day over the 7-day study period for each of 22 participants); 83.1%). The average number of recordings per day was 12.1 and the average number of eating episodes per day was 3.4. The average premeal LOC rating across all observations, including those obtained prior to meals, before bedtime, and in response to semi-random prompts, was 3.75 ± 1.16 (n = 1467; range = 1–5). The average kilocalories consumed per eating episode was 586.9 ± 625.4 (n = 251) for participants with BED and 569.0 ± 556.3 (n = 315) for participants without BED. For participants with BED, 11.9% of all eating episodes were classified as binge eating (i.e., consumption of at least 1,000 kilocalories accompanied by a LOC rating of 3 or greater on the 1- to 5-point Likert-type scale, indicating at least moderate LOC; 26) compared to 7.7% for participants without BED.
Premeal negative affect
For premeal negative affect, there was a significant main effect for LOC (t (1,427) = 4.61; P < 0.001; see Table 1), indicating that for all participants, greater LOC was associated with higher premeal negative affect regardless of the amount of food eaten. The pseudo R2 for the full model was 0.06, which is between a small (R2 = 0.02) and a medium (R2 = 0.14) effect size (33).
Table 1.
Linear mixed-model results for predicting pre- and postmeal negative affect based on binge eating disorder status, kilocalorie intake, and premeal loss of control
| Independent variable | Estimate | s.e. | d.f. | Test statistic |
|---|---|---|---|---|
| Premeal negative affect | ||||
| Intercept | 9.15 | 0.64 | 160.03 | t = 14.20*** |
| Study day | 0.12 | 0.06 | — | Wald z = 2.03* |
| Group | 1.57 | 1.25 | 148.31 | t = 1.26 |
| Kilocalories | 0.00 | 0.00 | 445.72 | t = 0.82 |
| LOC | 0.68 | 0.15 | 427.34 | t = 4.61*** |
| Group × kilocalories | 0.00 | 0.00 | 445.20 | t = −0.38 |
| Group × LOC | 0.40 | 0.29 | 427.45 | t = 1.36 |
| Kilocalories × LOC | 0.00 | 0.00 | 445.02 | t = 0.51 |
| Group × kilocalories × LOC | 0.00 | 0.00 | 444.89 | t = −0.77 |
| Postmeal negative affect | ||||
| Intercept | 2.51 | 0.49 | 22.61 | t = 5.12*** |
| Study day | 0.000 | 0.01 | — | Wald z = 0.70 |
| Group | −0.49 | 0.75 | 15.67 | t = −0.65 |
| Kilocalories | 0.00 | 0.00 | 69.28 | t = −1.46 |
| LOC | 0.17 | 0.10 | 37.56 | t = 1.68 |
| Premeal negative affect | 0.67 | 0.03 | 57.73 | t = 20.57*** |
| Group × kilocalories | 0.00 | 0.00 | 58.96 | t = −2.86** |
| Group × LOC | −0.15 | 0.20 | 40.28 | t = −0.73 |
| Kilocalories × LOC | 0.00 | 0.00 | 66.69 | t = −0.59 |
| Group × kilocalories × LOC | 0.00 | 0.00 | 59.18 | t = −2.28* |
Group, binge eating disorder or nonbinge eating disorder; LOC, loss of control.
P < 0.05,
P < 0.01,
P < 0.001.
Postmeal negative affect
For postmeal negative affect (adjusted for premeal negative affect), there were no main effects for LOC, kilocalories, or group status (Ps > 0.10; see Table 1). However, the two-way interaction between kilocalories and group was significant (t (1,59) = −2.86; P = 0.006). Figure 1 illustrates that for the BED group, postmeal negative affect was unrelated to the amount of food consumed; however, for individuals without BED, greater kilocalorie consumption was associated with lower postmeal negative affect. The three way-interaction between LOC, kilocalories, and group was also significant (t (1,59) = −2.28; P = 0.03), such that for the BED group, greater LOC was associated with greater postmeal negative affect, and lower LOC was associated with lower postmeal negative affect, regardless of the amount of food consumed. For individuals without BED, the combination of greater LOC and greater kilocalorie consumption was associated with lower postmeal negative affect. For participants without BED who reported low LOC, postmeal negative affect was unrelated to the amount of food consumed (see Figure 2). The pseudo R2 for the full model was 0.04, which is between a small (R2 = 0.02) and a medium (R2 = 0.14) effect size (33).
Figure 1.
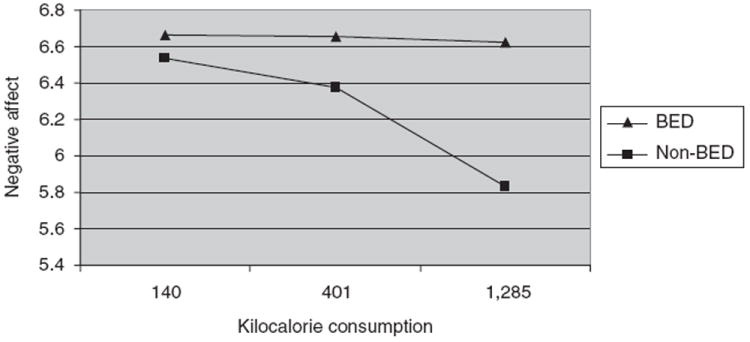
The two-way interaction between binge eating disorder status and kilocalorie consumption with respect to postmeal negative affect. BED, binge eating disorder. Higher scores on the y-axis indicate greater negative affect. Figure estimates are model-based.
Figure 2.
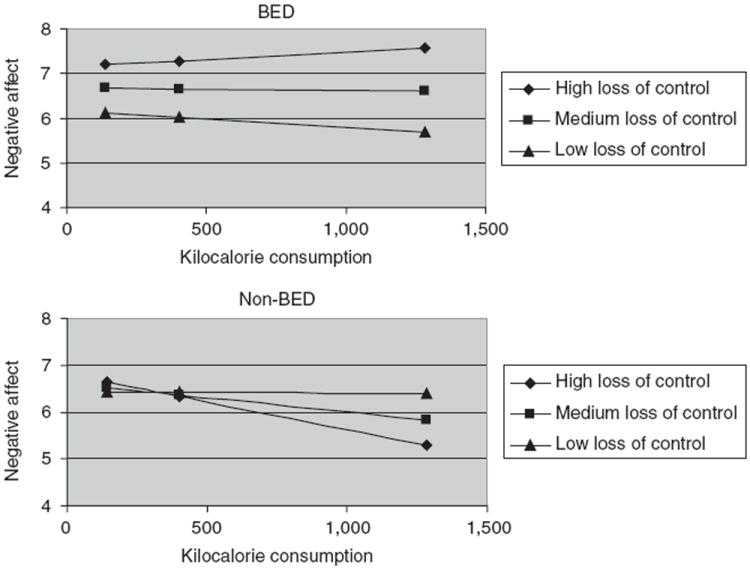
The three-way interaction among binge eating disorder status, loss of control, and kilocalorie consumption with respect to postmeal negative affect. BED, binge eating disorder. Higher scores on the y-axis indicate greater negative affect. Figure estimates are model-based.
DISCUSSION
The purpose of the current study was to examine the importance of LOC and the amount of food consumed in relation to pre- and postmeal negative affect among obese adults with and without BED. Consistent with our hypotheses, we found that LOC, but not the amount of food consumed, was associated with higher premeal negative affect regardless of diagnostic status. Moreover, for individuals with BED, greater feelings of LOC were associated with higher postmeal negative affect, regardless of the amount of food eaten. For obese controls, the combination of LOC and consumption of large amounts of food was associated with lower postmeal negative affect. Overall, results suggest that for individuals with BED, LOC is a salient feature in determining the immediate emotional context surrounding eating episodes.
Our finding that LOC, but not the quantity of food consumed, nor their interaction, was associated with premeal negative affect seems to suggest that low mood may be a trigger for LOC eating but not necessarily for overeating. This finding is consistent with affect regulation theories of binge eating (15) and suggests that obese individuals predisposed to aberrant eating may be more likely to disinhibit or abandon control over eating in the face of distressing feelings. Alternatively, LOC may be experienced as a way of “numbing out” or dissociating when confronted with difficult emotional stimuli (5). In turn, individuals may minimize awareness of the amount of food being consumed, which could explain the unimportance of episode size with regards to momentary negative affect. However, for individuals with BED, this purported coping method does not appear to be effective regardless of the amount of food consumed, as indicated by our finding that increased feelings of LOC were related to greater postmeal negative affect irrespective of kilocalorie consumption. These results are consistent with previous EMA studies of binge eating (22,23) and may support the trade-off theory of binge eating (16), which purports that specific aversive emotions experienced prior to binge eating (e.g., loneliness) are replaced by less aversive emotions subsequent to binge eating (e.g., guilt). However, further research regarding changes in specific mood states surrounding aberrant eating is needed.
More generally, these results appear to indicate that the current Diagnostic and Statistical Manual of Mental Disorders, 4th Edition criteria for binge eating (i.e., consumption of unambiguously large amounts of food accompanied by LOC) may not accurately reflect the experience of individuals with BED. Indeed, LOC, when accompanied by relatively small amounts of food, was as strongly related to postmeal distress as LOC accompanied by larger amounts of food. Thus, the overeating criterion for binge eating may not be necessary, and its elimination could potentially result in improved identification and treatment for individuals struggling with aberrant eating. In particular, interventions focused on tolerating negative affect may be helpful in reducing problematic eating among obese adults.
A different relationship between eating behavior and postmeal mood state was identified among obese controls, whereby the combination of greater feelings of LOC and increased kilocalorie consumption was related to lower postmeal negative affect. It is possible that because obese controls do not engage in recurrent binge eating (at least at a threshold warranting a BED diagnosis), the effects of binge eating are still positively reinforcing. Conversely, individuals with a persistent pattern of binge eating (i.e., those with BED) may experience greater negative consequences secondary to binge eating (e.g., interruptions in interpersonal relationships, occupational impairments (34)) during the course of their illness.
We detected a significant two-way interaction between group and kilocalorie intake with respect to postmeal negative affect, such that among the obese controls, greater intake was related to decreased postmeal negative affect, whereas within the BED sample, intake was unrelated to postmeal negative affect. This finding may reflect disturbances in sensitivity to food as a reward among obese individuals (35). Several studies have found that obese individuals differ from those of nonoverweight status in terms of their behavioral and neurological responsivity to food cues (e.g., (36)), and preliminary data suggest that differences are even more pronounced in obese individuals with BED (37). There are competing theories about the nature of reward sensitivity in obesity, with some investigators hypothesizing that hypersensitivity to food as a reward leads to obesity, as the inherent reinforcing properties of food lead to over-consumption (38). By contrast, others suggest hyposensitivity to food as a reward as an alternative pathway to obesity, whereby individuals overeat to compensate for a reward deficit (39). It is unclear whether obese individuals with and without BED differ in terms of the nature of their neurological response to food cues. Future research should elucidate the differences we found between individuals with and without BED in relation to associations between quantity of eating episodes and subsequent mood state.
Strengths of the current study include the use of Nutritional Data System for Research data to quantify eating episodes, which not only enhances the validity of our findings, but also minimized reliance on participants’ subjective perception of eating episodes (i.e., whether or not to label an episode as a binge). In addition, the use of EMA data speaks to the ecological validity of our findings. Finally, to our knowledge, EMA methodology has not yet been utilized to study the importance of LOC and episode size with respect to momentary negative affect, making this a novel contribution to the binge eating and obesity literature.
The current study also has several limitations. Our sample size was quite small and, because of this limitation, we were unable to compare different types of categorical eating episodes (i.e., objective binge eating vs. subjective binge eating vs. overeating without LOC) in terms of affective precursors and consequences. Nevertheless, examining the amount of food eaten and LOC ratings continuously allowed us to include a large number of data points across participants and sampling time-points. Moreover, although EMA data limit retrospective recall bias, data collected were still based on self-report, which is prone to other types of biases (e.g., social desirability bias). Because an abbreviated form of the Positive and Negative Affect Scale was utilized in the EMA protocol, we were not able to examine specific facets of negative affect (e.g., guilt) in relation to eating episodes; as noted previously, future studies should investigate changes in specific mood states surrounding aberrant eating. Daily monitoring of mood and eating behavior, and presenting for repeated in-person assessments over the study period, could have altered participants’ behavior, thus compromising the reliability of our data; however, previous research has demonstrated that EMA assessment produces minimal reactive effects in terms of eating disorder behaviors (40). Finally, LOC ratings were collected prior to and subsequent to, but not during eating episodes. It is possible that in some instances, LOC may have developed during the course of the meal. However, due to the practicality and possible reactive effects of obtaining such measurements, it was not feasible to assess LOC during eating episodes.
In summary, the current study suggests that overeating and LOC have differential contributions to the emotional context surrounding eating episodes in obesity. Results have important implications for both the classification and theoretical understanding of binge eating, namely, suggesting that for individuals with BED, LOC, regardless of the amount of food consumed, is related to increased feelings of distress. Findings also underscore the importance of further investigating binge eating and emotional eating in obese individuals without BED, as these types of pathological eating episodes appear to be prevalent and related to distressing emotions even in the absence of full-syndrome BED. Further research is needed to better understand the long-term emotional consequences of LOC and overeating in obesity with and without BED.
Acknowledgments
This study was funded by the National Eating Disorders Association, The Midwest Regional Postdoctoral Program in Eating Disorders Research (grant T32-MH082761), and the Minnesota Obesity Center (P30-DK050456).
Footnotes
DISCLOSURE
The authors declared no conflict of interest.
References
- 1.Treasure J, Claudino AM, Zucker N. Eating disorders. Lancet. 2010;375:583–593. doi: 10.1016/S0140-6736(09)61748-7. [DOI] [PubMed] [Google Scholar]
- 2.Yanovski SZ. Binge eating in obese persons. In: Fairburn CG, Brownell KD, editors. Eating Disorders and Obesity: A Comprehensive Handbook. Guilford Press; New York: 2002. pp. 403–407. [Google Scholar]
- 3.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, text revision. American Psychiatric Association; Washington, DC: 2000. [Google Scholar]
- 4.Fairburn CG, Cooper Z. The Eating Disorder Examination. In: Fairburn CG, Wilson GT, editors. Binge Eating: Nature, Assessment, and Treatment. 12. Guilford Press; New York: 1993. pp. 317–360. [Google Scholar]
- 5.Telch CF, Pratt EM, Niego SH. Obese women with binge eating disorder define the term binge. Int J Eat Disord. 1998;24:313–317. doi: 10.1002/(sici)1098-108x(199811)24:3<313::aid-eat9>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 6.Wolfe BE, Baker CW, Smith AT, Kelly-Weeder S. Validity and utility of the current definition of binge eating. Int J Eat Disord. 2009;42:674–686. doi: 10.1002/eat.20728. [DOI] [PubMed] [Google Scholar]
- 7.Darby A, Hay P, Mond J, Rodgers B, Owen C. Disordered eating behaviours and cognitions in young women with obesity: relationship with psychological status. Int J Obes (Lond) 2007;31:876–882. doi: 10.1038/sj.ijo.0803501. [DOI] [PubMed] [Google Scholar]
- 8.Wilson GT. Diagnostic criteria for bulimia nervosa. Int J Eat Disord. 1992;11:315–319. [Google Scholar]
- 9.Rossiter EM, Agras WS. An empirical test of the DSM-III--R definition of binge. Int J Eat Disord. 1990;9:513–518. [Google Scholar]
- 10.Walsh BT, Kissileff HR, Hadigan CM. Eating behavior in bulimia. Ann N Y Acad Sci. 1989;575:446–454. doi: 10.1111/j.1749-6632.1989.tb53265.x. discussion 454. [DOI] [PubMed] [Google Scholar]
- 11.Pratt EM, Niego SH, Agras WS. Does the size of a binge matter? Int J Eat Disord. 1998;24:307–312. doi: 10.1002/(sici)1098-108x(199811)24:3<307::aid-eat8>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 12.Keel PK, Mayer SA, Harnden-Fischer JH. Importance of size in defining binge eating episodes in bulimia nervosa. Int J Eat Disord. 2001;29:294–301. doi: 10.1002/eat.1021. [DOI] [PubMed] [Google Scholar]
- 13.Latner JD, Hildebrandt T, Rosewall JK, Chisholm AM, Hayashi K. Loss of control over eating reflects eating disturbances and general psychopathology. Behav Res Ther. 2007;45:2203–2211. doi: 10.1016/j.brat.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 14.Mond JM, Latner JD, Hay PH, Owen C, Rodgers B. Objective and subjective bulimic episodes in the classification of bulimic-type eating disorders: another nail in the coffin of a problematic distinction. Behav Res Ther. 2010;48:661–669. doi: 10.1016/j.brat.2010.03.020. [DOI] [PubMed] [Google Scholar]
- 15.Heatherton TF, Baumeister RF. Binge eating as escape from self-awareness. Psychol Bull. 1991;110:86–108. doi: 10.1037/0033-2909.110.1.86. [DOI] [PubMed] [Google Scholar]
- 16.Kenardy J, Arnow B, Agras WS. The aversiveness of specific emotional states associated with binge-eating in obese subjects. Aust N Z J Psychiatry. 1996;30:839–844. doi: 10.3109/00048679609065053. [DOI] [PubMed] [Google Scholar]
- 17.Chua JL, Touyz S, Hill AJ. Negative mood-induced overeating in obese binge eaters: an experimental study. Int J Obes Relat Metab Disord. 2004;28:606–610. doi: 10.1038/sj.ijo.0802595. [DOI] [PubMed] [Google Scholar]
- 18.Telch CF, Agras WS. Do emotional states influence binge eating in the obese? Int J Eat Disord. 1996;20:271–279. doi: 10.1002/(SICI)1098-108X(199611)20:3<271::AID-EAT6>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 19.Wegner KE, Smyth JM, Crosby RD, et al. An evaluation of the relationship between mood and binge eating in the natural environment using ecological momentary assessment. Int J Eat Disord. 2002;32:352–361. doi: 10.1002/eat.10086. [DOI] [PubMed] [Google Scholar]
- 20.Greeno CG, Wing RR, Shiffman S. Binge antecedents in obese women with and without binge eating disorder. J Consult Clin Psychol. 2000;68:95–102. [PubMed] [Google Scholar]
- 21.Le Grange D, Gorin A, Catley D, Stone AA. Does momentary assessment detect binge eating in overweight women that is denied at interview? Eur Eat Disord Rev. 2001;9:309–324. [Google Scholar]
- 22.Hilbert A, Tuschen-Caffier B. Maintenance of binge eating through negative mood: a naturalistic comparison of binge eating disorder and bulimia nervosa. Int J Eat Disord. 2007;40:521–530. doi: 10.1002/eat.20401. [DOI] [PubMed] [Google Scholar]
- 23.Stein RI, Kenardy J, Wiseman CV, et al. What’s driving the binge in binge eating disorder?: A prospective examination of precursors and consequences. Int J Eat Disord. 2007;40:195–203. doi: 10.1002/eat.20352. [DOI] [PubMed] [Google Scholar]
- 24.Guss JL, Kissileff HR, Devlin MJ, Zimmerli E, Walsh BT. Binge size increases with body mass index in women with binge-eating disorder. Obes Res. 2002;10:1021–1029. doi: 10.1038/oby.2002.139. [DOI] [PubMed] [Google Scholar]
- 25.Yanovski SZ, Leet M, Yanovski JA, et al. Food selection and intake of obese women with binge-eating disorder. Am J Clin Nutr. 1992;56:975–980. doi: 10.1093/ajcn/56.6.975. [DOI] [PubMed] [Google Scholar]
- 26.Engel SG, Kahler KA, Lystad CM, et al. Eating behavior in obese BED, obese non-BED, and non-obese control participants: a naturalistic study. Behav Res Ther. 2009;47:897–900. doi: 10.1016/j.brat.2009.06.018. [DOI] [PubMed] [Google Scholar]
- 27.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders, Research Version, Patient Edition With Psychotic Screen. Biometrics Research, New York State Psychiatric Institute; New York: 1997. [Google Scholar]
- 28.Wheeler L, Reis HT. Self-recording of everyday life events: Origins, types, and uses. J Pers. 1991;59:339–354. [Google Scholar]
- 29.Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- 30.Schakel SF, Sievert YA, Buzzard IM. Sources of data for developing and maintaining a nutrient database. J Am Diet Assoc. 1988;88:1268–1271. [PubMed] [Google Scholar]
- 31.Feskanich D, Sielaff BH, Chong K, Buzzard IM. Computerized collection and analysis of dietary intake information. Comput Methods Programs Biomed. 1989;30:47–57. doi: 10.1016/0169-2607(89)90122-3. [DOI] [PubMed] [Google Scholar]
- 32.Raymond NC, Neumeyer B, Warren CS, Lee SS, Peterson CB. Energy intake patterns in obese women with binge eating disorder. Obes Res. 2003;11:869–879. doi: 10.1038/oby.2003.120. [DOI] [PubMed] [Google Scholar]
- 33.Cohen J. Statistical Power for the Behavioral Sciences. Erlbaum; Hillsdale, NJ: 1988. [Google Scholar]
- 34.Rieger E, Wilfley DE, Stein RI, Marino V, Crow SJ. A comparison of quality of life in obese individuals with and without binge eating disorder. Int J Eat Disord. 2005;37:234–240. doi: 10.1002/eat.20101. [DOI] [PubMed] [Google Scholar]
- 35.Stice E, Spoor S, Bohon C, Small DM. Relation between obesity and blunted striatal response to food is moderated by TaqIA A1 allele. Science. 2008;322:449–452. doi: 10.1126/science.1161550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stice E, Spoor S, Ng J, Zald DH. Relation of obesity to consummatory and anticipatory food reward. Physiol Behav. 2009;97:551–560. doi: 10.1016/j.physbeh.2009.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schienle A, Schäfer A, Hermann A, Vaitl D. Binge-eating disorder: reward sensitivity and brain activation to images of food. Biol Psychiatry. 2009;65:654–661. doi: 10.1016/j.biopsych.2008.09.028. [DOI] [PubMed] [Google Scholar]
- 38.Davis C, Strachan S, Berkson M. Sensitivity to reward: implications for overeating and overweight. Appetite. 2004;42:131–138. doi: 10.1016/j.appet.2003.07.004. [DOI] [PubMed] [Google Scholar]
- 39.Comings DE, Blum K. Reward deficiency syndrome: genetic aspects of behavioral disorders. Prog Brain Res. 2000;126:325–341. doi: 10.1016/S0079-6123(00)26022-6. [DOI] [PubMed] [Google Scholar]
- 40.Stein KF, Corte CM. Ecologic momentary assessment of eating-disordered behaviors. Int J Eat Disord. 2003;34:349–360. doi: 10.1002/eat.10194. [DOI] [PubMed] [Google Scholar]


