Abstract
We examine the role of perceived stress and health behaviors (i.e., cigarette smoking, alcohol consumption, physical inactivity, sleep duration) in shaping differential mortality among whites, blacks, and Hispanics. We use data from the 1990 National Health Interview Survey (N=38,891), a nationally representative sample of United States adults, to model prospective mortality through 2006. Our first aim examines whether unhealthy behaviors and perceived stress mediate race/ethnic disparities in mortality. The black disadvantage in mortality, relative to whites, closes after adjusting for socioeconomic status (SES), but re-emerges after adjusting for the lower smoking levels among blacks. After adjusting for SES, Hispanics have slightly lower mortality than whites; that advantage increases after adjusting for the greater physical inactivity among Hispanics, but closes after adjusting for their lower smoking levels. Perceived stress, sleep duration, and alcohol consumption do not mediate race/ethnic disparities in mortality. Our second aim tests competing hypotheses about race/ethnic differences in the relationships among unhealthy behaviors, perceived stress, and mortality. The social vulnerability hypothesis predicts that unhealthy behaviors and high stress levels will be more harmful for race/ethnic minorities. In contrast, the Blaxter (1990) hypothesis predicts that unhealthy lifestyles will be less harmful for disadvantaged groups. Consistent with the social vulnerability perspective, smoking is more harmful for blacks than for whites. But consistent with the Blaxter hypothesis, compared to whites, current smoking has a weaker relationship with mortality for Hispanics, and low or high levels of alcohol consumption, high levels of physical inactivity, and short or long sleep hours have weaker relationships with mortality for blacks.
Keywords: Race, ethnicity, mortality, health behaviors, stress, USA
INTRODUCTION
There are persistent race/ethnic differences in mortality in the U.S. Non-Hispanic whites (henceforth “whites”) average longer lives than non-Hispanic blacks (henceforth “blacks”), and Hispanics have life expectancies that fall between those of blacks and whites (Hayward & Heron, 1999). Prior research emphasizes the importance of socioeconomic status (SES) for driving race/ethnic disparities in health (Bond Huie et al., 2003; Hayward et al., 2000; Kahn & Fazio, 2005; Sudano & Baker, 2006), but has not systematically examined the role of perceived stress and health behaviors for shaping mortality disparities. Given that unhealthy behaviors account for about 40% of deaths each year (Mokdad et al., 2004) and perceived stress shapes the practice of health behaviors and is linked to mortality (Krueger & Chang, 2008; Nielsen et al., 2008), we examine the role of perceived stress and unhealthy behaviors in shaping race/ethnic disparities in mortality among U.S. adults.
Race/Ethnicity, Stress, and Health Behaviors
Our first aim is to examine whether perceived stress and health behaviors mediate race/ethnic differences in overall mortality. Race/ethnic differences in the distribution of perceived stress and health behaviors may partially explain mortality disparities. However, if some unhealthy behaviors or high perceived stress are more prevalent among whites, then adjusting for those variables could increase the observed mortality differences between blacks and Hispanics, compared to whites.
Some studies show that, compared to whites, non-whites report greater exposure to stressful life events (e.g., death of a parent, incarceration), chronic stressors, discrimination, and perceived stress (Cohen & Williamson, 1988; Kessler et al., 1999; Turner & Avison, 2003). In contrast, Williams et al. (1997) find that blacks report fewer chronic stressors than whites, but higher levels of financial stress and stressful life events. But many studies of race/ethnic differences in stress do not generalize to the U.S. population because they use small, regional samples, or include restricted age ranges (e.g., Kessler et al., 1999; Turner & Avison, 2003; Williams et al., 1997).
Cigarette smoking accounts for over 300,000 deaths each year in the U.S. (Rogers et al., 2005). Throughout the 1970s and 1980s, blacks were less likely to smoke than whites, and when they did smoke, they typically smoked at lower levels and, among women, started at older ages (Geronimus et al., 1993; Sterling & Weinkam, 1989). By 1998, blacks and whites had similar rates of cigarette smoking, although Hispanics remained less likely than whites or blacks to smoke throughout that period (U.S. Department of Health and Human Services, 2000).
Physical inactivity is associated with increased risks of overall and cardiovascular disease mortality (Blair et al., 1992). In 1997, 38% of whites undertook no leisure time physical activity, compared to over 50% of blacks and Hispanics, and only 15% of whites, 10% of blacks, and 11% of Hispanics attained the recommended levels of exercise (U.S. Department of Health and Human Services, 2000).
Alcohol consumption has a J-shaped relationship with mortality, with the lowest mortality among moderate drinkers, and increased mortality among those who abstain or drink heavily (Thun et al., 1997). The increased mortality among those who abstain persists even after adjusting for those who stopped drinking for health reasons (Krueger & Chang, 2008; Rogers et al., 2000). Moderate levels of alcohol consumption have been linked to reduced risks of stroke and coronary heart disease (Reynolds et al., 2003), although high levels of drinking have been linked to elevated mortality from external causes, cardiovascular disease, cirrhosis, and some cancers (Thun et al., 1997). Compared to whites, blacks and Hispanics are more likely to abstain, although blacks have the highest frequency of heavy drinking and Hispanics consume more alcohol than whites on days that they drink (Dawson, 1998).
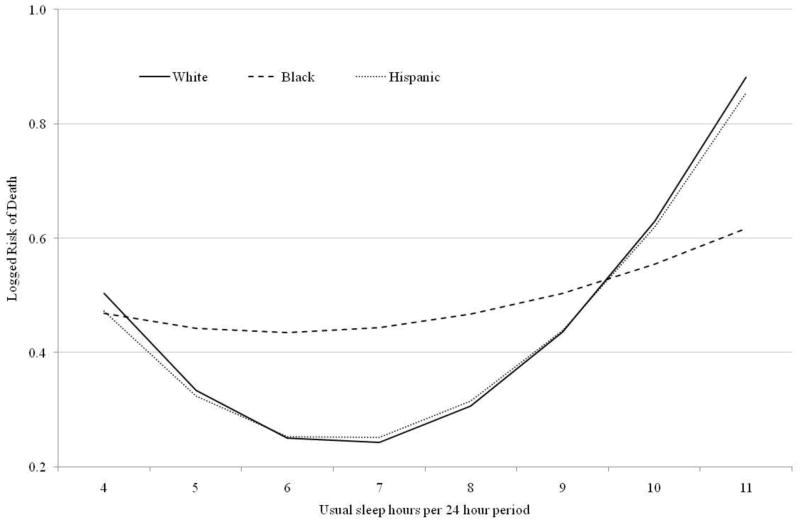
Sleep duration has a U-shaped relationship with mortality; those who sleep 7 to 8 hours per 24 hour period have lower risks of death than those who sleep longer or shorter hours (Ferrie et al., 2007). Compared to whites, blacks and Hispanics are less likely to sleep 7 to 8 hours, and are more likely to sleep longer or shorter hours (Krueger & Friedman, 2009).
Social Vulnerability and Blaxter Hypotheses: The Role of Race/Ethnicity
Our second aim is to examine whether the relationships among perceived stress, health behaviors, and prospective mortality differ across race/ethnic groups. Compared to whites, blacks and Hispanics experience more discrimination, limited socioeconomic opportunities, and residence in segregated communities that are marked by high levels of poverty and crime (Kessler et al., 1999; Massey, 2004), more liquor stores and advertising for alcohol and tobacco, and less access to exercise facilities (Moore et al., 1996; Powell et al., 2006). Based on these differences in social disadvantage, we test competing hypotheses about race/ethnic differences in the relationships among unhealthy behaviors, perceived stress, and mortality.
The social vulnerability hypothesis predicts that that socially disadvantaged groups will be most vulnerable to the harms associated with unhealthy lifestyles (Krueger & Chang, 2008; Williams, 1997). Like those with low SES (Farmer & Ferraro, 2005; Pampel & Rogers, 2004), blacks and Hispanics experience numerous disadvantages that may threaten health, increase vulnerability to disease, and exacerbate the harms of unhealthy behaviors and high stress. The social vulnerability hypothesis predicts that the increased mortality associated with high perceived stress levels, current and former smoking, and physical inactivity will be more positive, and the convex relationships between mortality and alcohol consumption or sleep hours will be stronger for blacks and Hispanics than for whites.
The social vulnerability hypothesis also predicts that the combination of high stress and unhealthy behaviors will be particularly harmful for blacks and Hispanics. High stress levels and unhealthy behaviors can create a pernicious cycle; stress encourages unhealthy but soothing behaviors (Ng & Jeffery, 2003), while smoking, drinking, inadequate sleep, and physical inactivity can increase inflammation, anxiety, and other stress indicators (Friedman et al., 2005; Parrott, 1999; Salmon, 2001). This cycle may be especially harmful for blacks and Hispanics who might experience more numerous or severe stressors than whites (Kessler et al., 1999; Turner & Avison, 2003), but have fewer means for mitigating their stress (Thoits, 1995).
In contrast, the Blaxter (1990) hypothesis predicts that disadvantaged groups may have worse health than advantaged groups, but might be less vulnerable to the harms of unhealthy lifestyles. Although Blaxter (1990) focuses on socioeconomic disadvantage, her ideas may apply to race/ethnic disadvantage for four reasons. First, disadvantages including limited socioeconomic opportunities, segregation, discrimination, and few community resources for health promotion may have such a strong influence on mortality among blacks and Hispanics that unhealthy behaviors or high stress have little room to further diminish their survival. Second, to mitigate their disadvantage, some minority groups may be more likely than whites to access religious involvement, family support, or psychosocial resources that buffer them from the harms associated with unhealthy behaviors or stress (Williams, 1997).
Third, if blacks and Hispanics experience more stress than whites, they may habituate to that stress and ultimately be less affected than whites who experience stress only intermittently (Williams, 1997). Fourth, exposure to severe stressors (which may be most common among blacks and Hispanics) can encourage personal growth and positive psychosocial orientations, thereby buffering individuals from the harms of more routine stressors (Kessler et al., 2006). The Blaxter hypothesis predicts that the relationship between mortality and perceived stress, current and former smoking, and physical inactivity will be less positive, and the convex relationships between mortality and alcohol consumption or sleep hours will be weaker (or even concave) for blacks and Hispanics than for whites.
The Blaxter hypothesis further predicts that the combination of stress and unhealthy behaviors will be less harmful for blacks and Hispanics than whites. Unhealthy behaviors undertaken in response to stress might allow some individuals to effectively cope with that stress (Salmon, 2001; Warburton, 1992). This might be especially true for race/ethnic minorities who face numerous insults to their health and have less to lose by participating in otherwise unhealthy behaviors, especially if they have few resources for directly addressing the sources of their stress (Thoits, 1995). In contrast, whites may occupy social positions that allow them to address the roots of their stress and to reap the benefits of healthy lifestyles.
Support for the vulnerability or Blaxter hypotheses may vary across race/ethnic groups. However, prior research offers little guidance into which hypothesis might better describe the experiences of blacks or Hispanics. Finally, in contrast to both the vulnerability and Blaxter hypotheses, the null hypothesis suggests that the impact of perceived stress and unhealthy behaviors on the risk of death will not differ across race/ethnic groups.
DATA AND METHODS
We use the 1990 Health Promotion and Disease Prevention Supplement (HPDPS) to the National Health Interview Survey (NHIS). The HPDPS conducts in-person interviews with a nationally representative sample of non-institutionalized U.S. adults aged 18 and older (National Center for Health Statistics, 1993), and is linked to prospective mortality in the National Death Index (NDI) through December of 2006 (National Center for Health Statistics, 2010). We rely on hot-deck imputations of the SES data from the 1990 Family Resources Supplement to the NHIS (National Center for Health Statistics, 1992). Eliminating 5.4% of the records that cannot be linked to the NDI due to missing information on the matching characteristics or because they are missing health behavior, stress, or demographic data, results in 38,891 respondents (30,175 whites, 5,087 blacks, 2,533 Hispanics, 1,096 others), of whom 7,944 died. Our project is considered exempt from review by the institutional review board at the University of Colorado Denver, because we rely on publicly available data that are stripped of personal identifiers.
Variables and Measurement
We use two items that range from 1 to 4 to assess perceived stress. The first asks, “During the past two weeks, would you say that you experienced a lot of stress, a moderate amount of stress, relatively little stress, or almost no stress at all?” The second question asked about the “past year” rather than the “past two weeks.” We take the mean of the two items, standardize the resulting variable so we can interpret our results in terms of standard deviations, and add a constant to set the minimum value to 0. Higher values indicate more stress (maximum= 3.2). We create the index because the two items are highly correlated (r=.71) and have similar relationships with the other key variables.
Our perceived stress measure has several advantages for our study. First, our measure avoids the problem of asking a standard list of stressors that could exclude the salient stressors for members of some minority groups, such as exposure to violence and racial discrimination (Thoits, 1995; Williams, 1997). The limited specificity of our perceived stress measure is balanced by its value for making comparisons across race/ethnic groups. Second, stress perceptions may be more important than counts of stressors for shaping health behaviors (Ng & Jeffery, 2003). Third, perceived stress has established relationships with mortality and SES (Krueger & Chang, 2008; Nielsen et al., 2008). Finally, perceived stress can be assessed with fewer items than more detailed stress indices, which facilitates its inclusion in large, nationally representative surveys.
Current smoking is coded as the number of packs smoked per day, calculated as the number of cigarettes divided by 20. Former smoking is coded as the number of packs smoked per day prior to quitting. Both variables equal 0 for never smokers (the referent). Physical inactivity is assessed with an index that sums the standardized values of three items (α= .67): whether individuals exercise or play sports regularly (yes or no), how many years they have exercised regularly (range: 0 to 90), and whether they are more active, about as active, or less active than others their age (range: 1 to 3). We create an index because each item has similar relationships with the other key variables. We standardize the resulting index so that we can interpret our results in terms of standard deviations. Higher values indicate greater inactivity.
Alcohol consumption and sleep duration have non-monotonic relationships with mortality. We measure each variable continuously and test different functions for their relationships with mortality by raising each variable to all combinations of two of the following powers: .5, 1, 1.5, and 2 (see Greenland, 1995). We select the best combination based on improvements in model fit. Alcohol consumption indicates how many drinks respondents consumed in the past two weeks, and is raised to the powers of .5 and 1.5. Sleep duration indicates the hours slept in a usual 24 hour period, and is raised to the powers of 1 and 1.5.
Based on tabulations of each health behavior variable and race/ethnicity, we top- and bottom-code the behavior variables to limit the influence of extreme values and to ensure that we have enough observations across their ranges, by race/ethnicity, to permit reasonable inferences. Current and former smoking originally ranged from 0 to 4.5 packs, but we top-code them at 2 packs; alcohol consumption ranged from 0 (including abstainers) to 168 drinks in a 2 week period, but we top-code it at 22 drinks; physical inactivity ranged from 0 to about 5.6, but very few individuals were among the most physically active (the low end of the index), so we bottom-code it at 2.5; and sleep hours ranged from 0 to 23 hours, but we recode it to range from 4 or less hours, to 11 or more hours. Separate analyses that compare truncated and non-truncated health behavior variables found nearly identical coefficients, but the models with the truncated variables have markedly smaller BIC values and more efficient parameter estimates.
We code race/ethnicity as non-Hispanic whites (the referent), non-Hispanic blacks, Hispanics, and all others. When testing for interactions by race/ethnicity, we exclude “others” because they are a small and heterogeneous group. Educational attainment is continuous and ranges from 0 to 18 or more years. Monthly family income is adjusted for family size, divided by 100, and logged to account for the diminishing impact of income on mortality as income increases (Krueger et al., 2003). We also include a family income portfolio, a proxy for wealth that indicates the number of income sources, per family member, received from jobs, self-employment, interest, dividends, pensions, and other income (Krueger et al., 2003). We also adjust for employment status, sex, marital status, foreign born status, and birth year.
Statistical Methods
Cox proportional hazard models examine the risk of death. Because survival is a direct function of age, we use age as the time to event or censor—rather than as a covariate—in our models (Korn et al., 1997). Although the effects of some variables varied with age (not shown), our substantive findings were similar throughout the age range examined. Thus, we rely on the proportional hazards assumption; our models provide the average effects of our covariates on the risk of death across age (Allison, 1984). All analyses incorporate sample weights and estimate Taylor linearized standard errors to account for the complex sampling frame (StataCorp, 2009).
We use the following strategy to test for interactions. First, we create each set of two-way interactions by multiplying the variables for race/ethnicity by each health behavior; race/ethnicity by perceived stress; and each health behavior by perceived stress. We create three-way interactions by multiplying the variables for race/ethnicity, perceived stress, and each health behavior. Second, we test each set of interactions in a separate model and retain only those groups of interactions for which there is “strong” evidence in favor of their inclusion as indicated by improvements in the BIC statistic by 6 or more points (Raftery, 1995). In no case were all of the two-way interactions or any of the three-way interactions significant.1
We test for interactions with each health behavior separately. Models that include interactions with all of the health behaviors simultaneously provide substantively similar coefficients but with wider standard errors due to multicolinearity among the interaction terms. All of the interactive models adjust for the main effects of all of the health behaviors and the sociodemographic and SES variables.
RESULTS
Table 1 presents the means of the covariates by vital status and by race/ethnicity. The means of dichotomous variables are proportions. Before adjusting for other covariates, those who survive the follow-up period average higher perceived stress levels, lower levels of current and former smoking (recall that never smokers are coded as 0 on these variables), and lower levels of physical inactivity than decedents. Because alcohol consumption and sleep hours have non-monotonic relationships with mortality, the descriptive results show both continuous and categorical versions. Survivors were more likely than decedents to consume 3 or more drinks in the last 2 weeks, and to sleep 7 or 8 hours per night. Table 1 also shows that, compared to whites, blacks and Hispanics have lower levels of perceived stress, current and former smoking, and alcohol consumption; are less likely to report 7–8 hours of sleep; and report higher levels of never smoking and physical inactivity.
Table 1.
Weighted Means and Proportions of the Covariates, by Vital Status and by Race/Ethnicity, U.S. Adults, 1990–2006.
| Vital Status | Race/Ethnicity | ||||||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| Survived | Died | p-valuea | White | Black | Hispanic | p-valuea | |
| Race/Ethnicity (categories) | < 0.001 | ||||||
| Non-Hispanic white | 0.77 | 0.84 | -- | -- | -- | ||
| Non-Hispanic black | 0.11 | 0.10 | -- | -- | -- | ||
| Hispanic | 0.08 | 0.04 | -- | -- | -- | ||
| Other | 0.04 | 0.01 | -- | -- | -- | ||
| Stress and Health Behaviors | |||||||
| Perceived Stress | 2.04 | 1.59 | < 0.001 | 2.02 | 1.77 | 1.65 | < 0.001 |
| Cigarette Smoking (number) | < 0.001 | < 0.001 | |||||
| Current packs smoked | 0.23 | 0.27 | 0.26 | 0.17 | 0.14 | ||
| Former packs smoked | 0.21 | 0.37 | 0.27 | 0.12 | 0.12 | ||
| Never smoker (=1) | 0.53 | 0.41 | 0.48 | 0.58 | 0.60 | ||
| Drinks last 2 weeks | 4.54 | 3.66 | < 0.001 | 4.64 | 3.30 | 3.89 | < 0.001 |
| Drinks last 2 weeks (categories) | < 0.001 | < 0.001 | |||||
| Abstain | 0.28 | 0.33 | 0.27 | 0.35 | 0.33 | ||
| 1 to 2 drinks | 0.33 | 0.41 | 0.34 | 0.37 | 0.34 | ||
| 3 to 7 drinks | 0.16 | 0.09 | 0.16 | 0.12 | 0.14 | ||
| More than 7 drinks | 0.23 | 0.18 | 0.23 | 0.16 | 0.19 | ||
| Index of Physical Inactivity | 4.31 | 4.48 | < 0.001 | 4.30 | 4.51 | 4.48 | < 0.001 |
| Sleep Hours per 24 Hours | 7.25 | 7.46 | < 0.001 | 7.27 | 7.36 | 7.30 | 0.019 |
| Sleep Hours (categories) | < 0.001 | < 0.001 | |||||
| 6 or fewer hours | 0.24 | 0.24 | 0.23 | 0.30 | 0.26 | ||
| 7 to 8 hours | 0.67 | 0.60 | 0.68 | 0.56 | 0.63 | ||
| 9 or more hours | 0.08 | 0.16 | 0.09 | 0.14 | 0.11 | ||
| Survival and Gender | |||||||
| All-Cause Mortality (died=1) | 0.00 | 1.00 | 0.19 | 0.17 | 0.10 | < 0.001 | |
| Age at Death or Censor | 56.1 | 74.8 | < 0.001 | 60.6 | 56.5 | 53.9 | < 0.001 |
| Age at Interview | 39.5 | 65.7 | < 0.001 | 45.4 | 41.2 | 38.0 | < 0.001 |
| Male (=1) | 0.47 | 0.50 | < 0.001 | 0.48 | 0.44 | 0.45 | 0.001 |
| N (unweighted) | 30,947 | 7,944 | 30,175 | 5,087 | 2,533 | ||
All p-values come from Wald tests that account for the complex sampling frame used by the HPDPS.
Table 2 presents Cox proportional hazard coefficients from models that examine whether perceived stress and health behaviors explain race/ethnic differences in mortality (our first aim). Model 1 shows that, compared to whites, blacks have 1.27 (=e0.239) times the risk of death and Hispanics have 1.08 (=e0.077) times the risk of death when adjusting for sex, foreign born status, and birth year. After adjusting for marital status and SES (Model 2), compared to whites, blacks do not have significantly higher risks of death, and Hispanics have slightly lower risks of death.
Table 2.
Cox Proportional Hazard Coefficients (Standard Errors) for the Relationships among Race/Ethnicity, Perceived Stress, Health Behaviors, and the Risk of Death, U.S. Adults, 1990–2006.
| Model 1a | Model 2b | Model 3 b | Model 4 b | Model 5 b | Model 6 b | Model 7 b | Model 8 b | |
|---|---|---|---|---|---|---|---|---|
| Race/Ethnicity | ||||||||
| White | ref. | ref. | ref. | ref. | ref. | ref. | ref. | ref. |
| Black | 0.239*** (0.074) | 0.038 (0.066) | 0.045 (0.068) | 0.157** (0.063) | 0.043 (0.066) | 0.022 (0.068) | 0.011 (0.059) | 0.126** (0.059) |
| Hispanic | 0.077** (0.032) | −0.080* (0.045) | −0.072* (0.042) | 0.028 (0.048) | −0.079* (0.043) | −0.099** (0.039) | −0.075 (0.052) | 0.013 (0.046) |
| Other | −0.222** (0.096) | −0.309*** (0.082) | −0.294*** (0.080) | −0.216*** (0.079) | −0.301*** (0.081) | −0.326*** (0.086) | −0.309*** (0.089) | −0.222** (0.088) |
| Stress and Health Behaviors | ||||||||
| Perceived Stress | 0.046*** (0.013) | 0.029** (0.013) | ||||||
| Cigarette Smoking | ||||||||
| Current packs smoked | 0.653*** (0.013) | 0.627*** (0.014) | ||||||
| Former packs smoked | 0.201*** (0.028) | 0.203*** (0.029) | ||||||
| Never smokers | ref. | ref. | ||||||
| Alcohol Consumption | ||||||||
| Drinks last 2 weeks ^.5 | −0.151*** (0.029) | −0.137*** (0.029) | ||||||
| Drinks last 2 weeks ^1.5 | 0.040*** (0.005) | 0.029*** (0.004) | ||||||
| Index of Physical Inactivity | 0.201*** (0.019) | 0.170*** (0.020) | ||||||
| Sleep Hours per 24 Hours | ||||||||
| Hours of sleep | −1.017*** (0.173) | −0.808*** (0.144) | ||||||
| Hours of sleep^1.5 | 0.263*** (0.045) | 0.211*** (0.039) | ||||||
| BIC | 58,712 | 58,176 | 58,163 | 57,597 | 58,136 | 57,976 | 58,077 | 57,334 |
Note:
p < 0.10;
p < 0.05;
p < 0.01 (two-tailed tests).
Model 1 also adjusts for sex, foreign born status, and birth year.
Models 2–8 also adjust for sex, foreign born status, birth year, education, family income, the income portfolio, employment status, and marital status.
Models 3 through 7 separately include each stress and health behavior measure. Perceived stress (Model 3) has little influence on race/ethnicity differences in and mortality, although a one standard deviation increase in the perceived stress index is associated with 1.05 (=e0.046) times the risk of death. After adjusting for smoking (Model 4), the black disadvantage in mortality (relative to whites) re-emerges, because blacks smoke less than whites. Similarly, the coefficient for Hispanics in Model 4 is marginally more positive than the coefficient in Model 2 (two-tailed p-value=0.10). Relative to never smokers, each pack per day increase in smoking is associated with 1.92 (=e0.653) times the risk of death among current smokers, and 1.22 (=e0.201) times the risk of death among former smokers.
Adjusting for alcohol consumption (Model 5) does little to change race/ethnic differences in mortality, relative to Model 2. The polynomial terms for alcohol consumption indicate a convex relationship with mortality. Model 6 adjusts for physical activity and finds that the mortality advantage for Hispanics, relative to whites, is slightly but not significantly greater than the advantage in Model 2 (two-tailed p-value=0.75), due to the higher levels of physical inactivity among Hispanics (see Table 1). A one standard deviation increase in physical inactivity is associated with 1.22 (=e0.201) times the risk of death. Sleep duration (Model 7) does little to change race/ethnic differences in mortality, compared to Model 2. But the polynomial terms indicate that sleep duration has a convex relationship with mortality.
Model 8 adjusts for all of the perceived stress and health behavior variables simultaneously and finds that blacks have 1.13 (=e0.126) times the risk of death of whites. The black disadvantage did not emerge when adjusting for the SES and demographic variables in Model 2—due to the lower rates of smoking among blacks—and is not significantly different from the coefficient for black in Model 1 (two-tailed p-value=.23). The coefficient for Hispanic in Model 8 is not significantly different from the coefficient in Model 1 (two-tailed p-value=.26) or Model 2 (two-tailed p-value=.15).
Table 3 presents four models that examine whether race/ethnicity moderates the impact of perceived stress and health behaviors on mortality (our second aim). Each panel focuses on the interactions among race/ethnicity, perceived stress, and one of the health behaviors. We exclude those interactions that fail to improve the model fit according to the BIC statistic. All models adjust for (but do not show) the socioeconomic and sociodemographic variables, as well as the main effects for the health behavior variables not included in the interaction.
Table 3.
Cox Proportional Hazard Coefficients (Standard Errors) for Interactions among Race/Ethnicity, Perceived Stress, and Health Behaviors, on the Risk of Death, U.S. Adults, 1990–2006.a
| Panel A: Cigarette Smoking | p-value | BIC Improvementb | ||
|---|---|---|---|---|
| Race/Ethnicity [White is referent] | ||||
| Black | 0.067 (0.053) | |||
| Hispanic | 0.009 (0.059) | |||
| Perceived Stress | 0.002 (0.020) | |||
| Cigarette Smoking [referent is never smokers] | ||||
| Current packs smoked | 0.581*** (0.037) | |||
| Former packs smoked | 0.099*** (0.029) | |||
| Interactions | ||||
| Stress * current packs | 0.019** (0.008) |
|
0.003 | 11.23 |
| Stress * former packs | 0.050** (0.020) | |||
| Black * current packs | 0.137 (0.127) |
|
0.003 | 6.44 |
| Black * former packs | 0.118*** (0.046) | |||
| Hispanic * current packs | −0.151*** (0.057) | |||
| Hispanic * former packs | 0.104 (0.085) | |||
|
| ||||
|
Panel B: Alcohol Consumption
| ||||
| Race/Ethnicity [White is referent] | ||||
| Black | −0.035 (0.035) | |||
| Hispanic | −0.057 (0.095) | |||
| Perceived Stress | 0.027* (0.014) | |||
| Alcohol Consumption | ||||
| Drinks in last 2 weeks^.5 | −0.169*** (0.024) | |||
| Drinks in last 2 weeks^1.5 | 0.035*** (0.004) | |||
| Interactions | ||||
| Black * drinks^.5 | 0.306*** (0.049) |
|
<0.001 | 15.74 |
| Black * drinks^1.5 | −0.050*** (0.009) | |||
| Hispanic * drinks^.5 | 0.152 (0.241) | |||
| Hispanic * drinks^1.5 | −0.032 (0.055) | |||
|
| ||||
|
Panel C: Physical Inactivity
| ||||
| Race/Ethnicity [White is referent] | ||||
| Black | 0.457* (0.255) | |||
| Hispanic | 0.713 (0.553) | |||
| Perceived Stress | 0.027* (0.014) | |||
| Physical inactivity | 0.183*** (0.019) | |||
| Interactions | ||||
| Black * inactivity | −0.073* (0.043) |
|
0.244 | 6.68 |
| Hispanic * inactivity | −0.156 (0.121) | |||
|
| ||||
|
Panel D: Usual Sleep Hours in a 24 Hour Period
| ||||
| Race/Ethnicity [White is referent] | ||||
| Black | −1.545 (0.986) | |||
| Hispanic | −0.222 (1.657) | |||
| Perceived Stress | 0.027* (0.015) | |||
| Sleep hours | ||||
| Sleep | −0.965*** (0.158) | |||
| Sleep^1.5 | 0.251*** (0.042) | |||
| Interactions | ||||
| Black * sleep | 0.774* (0.418) |
|
<0.001 | 7.69 |
| Black * sleep^1.5 | −0.198** (0.101) | |||
| Hispanic * sleep | 0.093 (0.772) | |||
| Hispanic * sleep^1.5 | −0.023 (0.199) | |||
Note:
p < 0.10;
p < 0.05;
p < 0.01 (two-tailed tests).
All models adjust for the socioeconomic and sociodemographic variables and for the main effects of all other health behavior variables (not shown)
This column shows the improvement in the BIC over a model that excludes the specified interaction terms.
Panel A presents the results for cigarette smoking. The main effects show no significant race/ethnic differences in mortality among never smokers when adjusting for the other variables. The non-significant coefficient for perceived stress suggests that stress is not associated with the risk of death among never smokers. Current and former smoking levels are positively associated with mortality among whites with no stress. The interactions between perceived stress and smoking indicate that the relationship between current and former smoking levels and mortality become more positive as stress increases. The interactions between race/ethnicity and smoking show that, compared to whites, the relationship between former smoking levels and mortality is more positive among blacks, and the relationship between current smoking levels and mortality is less positive among Hispanics.
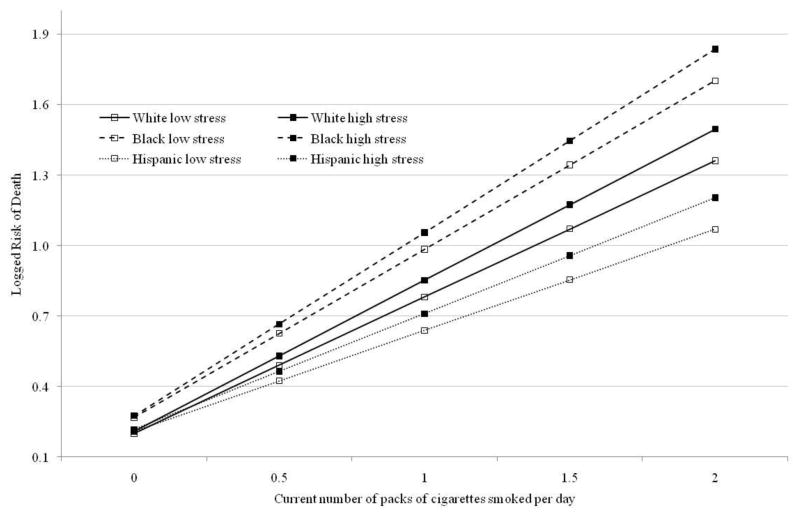
Figure 1 graphs the predicted logged risk of death (i.e., hazard coefficients) for current smokers, by race/ethnicity and at the minimum and maximum values of the perceived stress index, while holding all other covariates at their means. For all three race/ethnic groups, the risk of death increases with current smoking levels. Further, the risk of death associated with current smoking levels increases more rapidly as stress increases. Compared to whites, the risk of death for blacks who are current smokers is not significantly steeper (see Table 3), but the slope for current packs smoked among Hispanics is significantly shallower.
Figure 1.
Current smoking, stress, and mortality by race/ethnicity (from Table 3, Panel A)
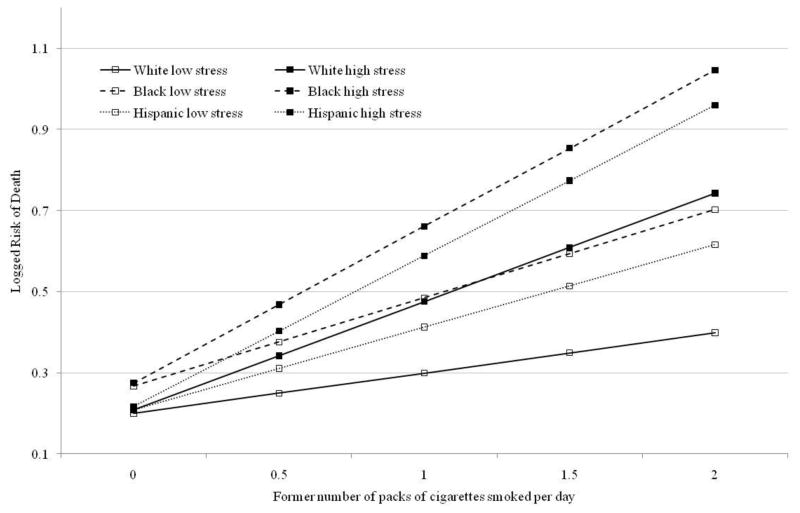
Figure 2 presents the expected logged risk of death for former smokers. Former smoking levels are positively associated with the risk of death for all race/ethnic groups, and the slopes for former smoking levels becomes steeper as perceived stress increases. Compared to whites, the slope for former smoking levels is significantly steeper for blacks.
Figure 2.
Former smoking, stress, and mortality by race/ethnicity (from Table 3, Panel A)
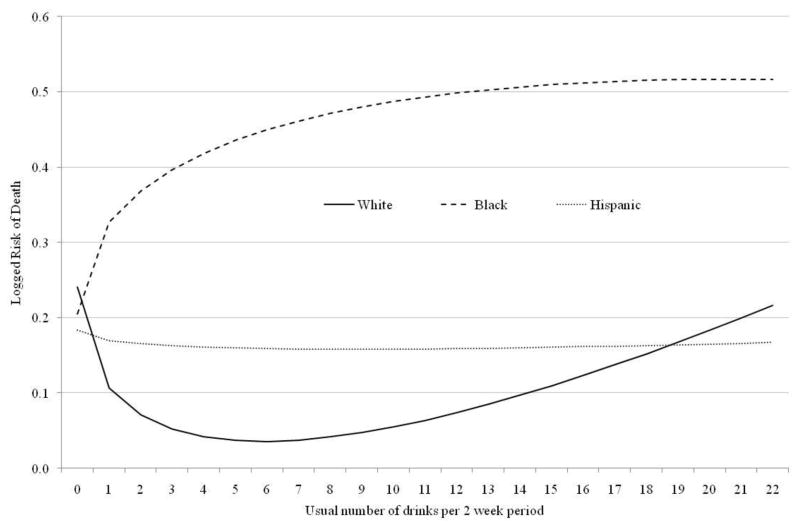
Table 3, Panel B presents the results for alcohol consumption. The main effects of the alcohol consumption variables demonstrate a convex relationship between drinking and mortality for whites. The interactions show that, compared to whites, the relationship between alcohol consumption and mortality is significantly different for blacks but not Hispanics. Figure 3 shows that whites exhibit a J-shaped relationship between alcohol consumption and mortality; those who drank 6 drinks in the past 2 weeks have the lowest risk of death, with increased mortality among those who drink more or less. The curve for Hispanics appears shallower, but it is not significantly different from the curve for whites (see Table 3). Among blacks, the risk of death is lowest among those who did not drink in the past 2 weeks, and increases at a decreasing rate as drinking increases.
Figure 3.
Alcohol consumption and mortality by race/ethnicity (from Table 3, Panel B)
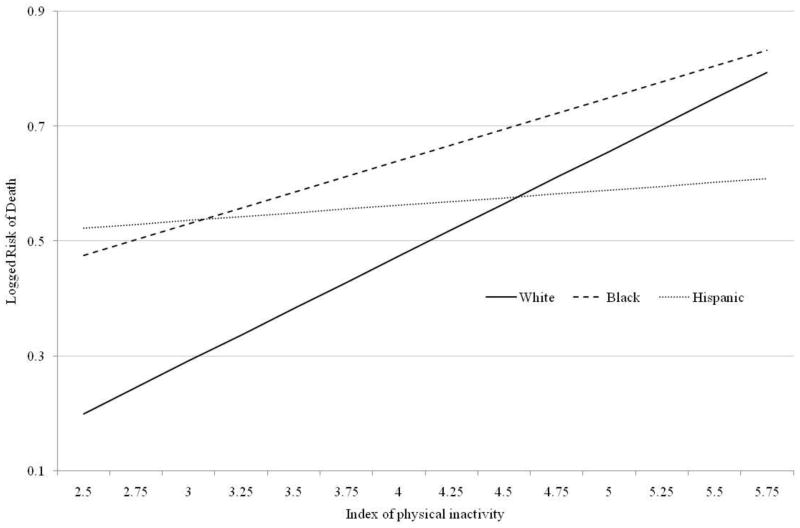
Table 3, Panel C presents the results for physical inactivity. The BIC statistic supports the inclusion of interactions between race and physical inactivity, although the interaction terms are not significant at the p<0.05 level. Therefore, we interpret these results with caution.2 Figure 4 shows that mortality increases with inactivity, although more slowly for blacks than whites. The slope for Hispanics is not significantly different from the slope for whites (see Table 3).
Figure 4.
Physical inactivity and mortality by race/ethnicity (from Table 3, Panel C)
Table 3, Panel D examines sleep hours. The main effects show a convex relationship between sleep hours and mortality for whites. The interactions show that, compared to whites, the relationship between sleep and mortality is significantly different among blacks, but not among Hispanics. Figure 5 illustrates that both whites and Hispanics exhibit a U-shaped relationship between sleep hours and mortality, with the lowest risk of death among those who usually sleep 7 hours, and increasing mortality among those who sleep more or fewer hours. However, the convex relationship between sleep hours and mortality is shallower for blacks than for whites or Hispanics.
Figure 5.
Sleep hours and mortality by race/ethnicity (from Table 3, Panel D)
DISCUSSION
Prior research offers scant insight into the role of unhealthy behaviors and perceived stress in shaping race/ethnic disparities in mortality. Our first aim examines whether perceived stress and unhealthy behaviors mediate race/ethnic differences in mortality. Compared to whites, adjusting for cigarette smoking increases the observed risk of death among blacks and closed the modest Hispanic advantage in mortality, because nonwhites smoke at lower levels than whites. Similarly, adjusting for physical inactivity increased the observed mortality advantage of Hispanics relative to whites, because Hispanics are more physically inactive. Perceived stress, alcohol consumption, and sleep hours do not mediate race/ethnic differences in survival.
To the extent that race/ethnicity works through SES to shape health behaviors and stress (Pampel et al., 2010; Williams et al., 1997), our models that adjust for SES provide conservative estimates of their impact on race/ethnic differences in mortality. Separate analyses that exclude the SES variables arrive at similar conclusions. Consistent with prior research, we find that SES accounts for a substantial share of race/ethnic differences in mortality (Bond Huie et al., 2003; Hayward et al., 2000; Kahn & Fazio, 2005), even resulting in a slight mortality advantage for Hispanics relative to whites (Markides & Coreil, 1986). But we also find that black-white differences in mortality re-emerge after adjusting for smoking, and the Hispanic mortality advantage, relative to whites, grows modestly larger after adjusting for physical inactivity but closes after adjusting for smoking.
Our second aim examines whether the relationships among perceived stress, health behaviors, and overall mortality differ across race/ethnic groups. Although our first aim focuses on average race/ethnic differences in mortality after adjusting for perceived stress and unhealthy behaviors, our second aim illuminates whether race/ethnic differences in mortality vary across levels of the health behaviors and perceived stress. Two hypotheses guide our research.
The social vulnerability hypothesis suggests that disadvantaged groups may be most vulnerable to the harms associated with unhealthy lifestyles (Farmer & Ferraro, 2005; Krueger & Chang, 2008; Pampel & Rogers, 2004). Consistent with the social vulnerability perspective, the black-white gap in mortality is smallest among never smokers, but widens with former smoking levels. Current smoking also has a stronger relationship with mortality for blacks than for whites, but that relationship is not significant. Smoking may be especially harmful among blacks because they also have poorer diets, greater exposure to carcinogens in the workplace, and reduced ability to metabolize the carcinogens in cigarette smoke (Stellman et al., 2003; Sterling & Weinkam, 1989), in addition to social disadvantages including segregation, discrimination, poverty, and limited health care access (Massey, 2004). The greater harm of smoking among blacks is especially problematic because tobacco companies disproportionately target blacks (Moore et al., 1996). Hispanics face disadvantages that are different (and, perhaps, less severe) than blacks, and we find no evidence that unhealthy behaviors are more harmful for Hispanics than for whites. We also find that perceived stress increases the mortality risk associated with current and former smoking levels. But the combination of high stress and smoking is not more harmful for blacks and Hispanics than for whites.
The Blaxter hypothesis suggests that compared to whites, blacks and Hispanics draw on social, cultural, or psychosocial resources to buffer them from the combined harm of social disadvantage, unhealthy behaviors, and high stress (Kessler et al., 2006; Williams, 1997). The disadvantages experienced by blacks and Hispanics may result in higher mortality than whites, but might also leave unhealthy behaviors and high stress less room to further harm their survival (Blaxter, 1990; Pampel et al., 2010). Consistent with the Blaxter hypothesis, we find that the black-white gap in mortality is greatest among those who drink moderately, are physically active, or sleep 7 or 8 hours. The gap narrows, however, among those who abstain or consume more alcohol, are physically inactive, or sleep longer or shorter hours
In the general population, individuals who drink moderately have the lowest risks of death (Thun et al., 1997), but that pattern holds only for whites and Hispanics. Among blacks, those who abstain from drinking have the lowest risk of death, while increasing alcohol consumption increases the risk of death, but at a slower rate than for whites. Similarly, sleep exhibits a U-shaped relationship with mortality in the general population (Ferrie et al., 2007), but that relationship is weaker among blacks than among whites or Hispanics. Although we cannot definitively reject the null hypothesis that the impact of physical inactivity is weaker among blacks than whites, the interactions clearly do not support the social vulnerability perspective.
Consistent with the Blaxter hypothesis, separate analyses find weak evidence that the relationship between perceived stress and the risk of death is less positive among blacks than among whites (see also Williams et al., 1997). The interactions between race/ethnicity and perceived stress are jointly significant (p=0.02), but their magnitude is quite small and they improved the BIC by only 3.37. Thus, we exclude the interactions from our models. We cannot definitively reject the hypothesis that stress has the same impact on survival across race/ethnic groups, but these findings clearly do not support the social vulnerability perspective.
Our finding that the relationship between current smoking levels and mortality is weaker among Hispanics than among whites is also consistent with the Blaxter hypothesis. However, the relationship between the risk of death and alcohol consumption, physical inactivity, and sleep duration are not significantly different among Hispanics and whites. Williams (1997) notes that the processes that drive mortality may vary across race/ethnic groups. Hispanics may be better able than blacks to emulate whites in U.S. society through a process of acculturation that leads to greater social opportunities, but also health behavior patterns that resemble those of whites (Antecol & Bedard, 2006).
Strengths and Limitations
The strengths of our analyses include the use of nationally representative data with large numbers of blacks, Hispanics, and whites, and numerous deaths over a sixteen year follow-up period. The HPDPS data come from face-to-face interviews that are conducted in English and Spanish, which is essential when studying Hispanics. The HPDPS also includes more detailed health behavior, perceived stress, and SES data than some prior studies (Sudano & Baker, 2006). Separate analyses assure the robustness of our findings; models that included interactions with or stratified by age, birth cohort, or sex found substantively similar results to those we show herein.
Several limitations of our analyses warrant mention. First, although our data ask about stress for the year prior to interview and health behaviors generally persist throughout the life course, individuals may recall their stress and health behaviors imperfectly. Panel data could limit recall bias and permit examination of race/ethnic differences in health behaviors over the life-course, but the available panel data with detailed health behavior measures are not linked to prospective mortality and do not include broad age-ranges.
Second, our health behavior measures are imperfect. Nevertheless, separate analyses found virtually identical results when excluding former smokers who only smoked occasionally, or who quit in the past 2 months and who are likely to resume smoking. Further, the increased mortality among those who abstain from drinking persists after excluding those who abstain for health reasons. Although we do not have objective measures of physical inactivity or sleep duration, self-reported data have previously been linked to prospective mortality (Ferrie et al., 2007; Krueger & Chang, 2008; Pampel & Rogers, 2004). Finally, the HPDPS data do not provide information on dietary practices or inventories of stressful life events.
Conclusion
We found that black-white differences in mortality are greatest when levels of sleep, physical activity, and alcohol consumption are at the levels associated with the lowest mortality in the general population. Our models suggest that policies that promote 7 to 8 hours of sleep and increase physical activity would improve the health of all groups in the population while widening black-white disparities in mortality. Reducing smoking would improve survival in all groups, but would narrow the Hispanic advantage in mortality compared to whites. Efforts to improve survival should encourage healthier behaviors, but policies that aim to close disparities might be most effective if they target broad structural disadvantages. Policies that target the connection between structural disadvantages and early life and epigenetic mechanisms could close disparities throughout the life course and across generations (Kuzawa & Sweet, 2009; Montez & Hayward, 2011).
In sum, our findings confirm Williams’ (1997, p. 329) assertion that “merely controlling for SES is inadequate to understanding racial disparities in health.” We find that race/ethnic disparities in mortality that were diminished after adjusting for SES re-emerge after adjusting for health behaviors. Prior research often finds that unhealthy behaviors are most harmful to the health of low SES individuals (Krueger & Chang, 2008; Pampel & Rogers, 2004). But, with the exception of smoking, we find that unhealthy behaviors are less harmful for blacks than for whites. Thus, blacks may experience a constellation of disadvantages that shape their mortality in different ways than SES, perhaps because race is an ascribed status that marks a history of disadvantage that persists across generations.
RESEARCH HIGHLIGHTS.
Prevalence of health behaviors varies by race/ethnicity in the USA, so disparities widen or narrow when adjusting for specific behaviors
The relationship between health behaviors and mortality varies across race/ethnic groups
Long or short sleep hours, abstaining or excess alcohol consumption, and physical inactivity harm blacks less than whites
Except for cigarette smoking, unhealthy behaviors have similar relationships with mortality among both whites and Hispanics
Perceived stress has little impact on race/ethnic differences in mortality
Acknowledgments
This paper has benefited from presentation at the 2008 meetings of the American Sociological Association in Boston, MA. We acknowledge administrative support from the University of Colorado Population Program (NICHD R21 HD51146), the University of Houston (NIDA R24 DA019798), and the Leonard Davis Institute of Health Economics at the University of Pennsylvania, and research support from the National Institutes of Health (NICHD K12-HD043459).
Footnotes
Given our sample size, mortality rate, and variation in our covariates, we have statistical power to detect three-way interactions of small magnitude. Further, models that include all of the two-way and three-way interactions, regardless of their statistical significance, identify virtually identical patterns as those captured by the simpler models we present, but failed to fit the data better according to the BIC statistic. Thus, we find neither statistical nor substantive support for including additional interaction terms in our models.
Separate analyses ensure that the results from our interactive models are not driven by a few influential observations or outliers. First, we calculated dfbetas for each covariate and failed to find any observations that had an undue influence on our key estimates. Second, we calculated likelihood displacement statistics, which indicate the influence on twice the log likelihood of removing a particular observation. Depending on the interactions included in a particular model, we identified up to 491 observations that had a relatively large influence on the likelihood function. But our findings were unchanged when excluding those observations.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Allison PD. Event history analysis: Regression for longitudinal event data. Newbury Park, CA: Sage; 1984. [Google Scholar]
- Antecol H, Bedard K. Unhealthy assimilation: Why do immigrants converge to American health status levels? Demography. 2006;43:337–360. doi: 10.1353/dem.2006.0011. [DOI] [PubMed] [Google Scholar]
- Blair SN, Kohl HW, Gordon NF, Paffenbarger RS. How much physical activity is good for health? Annual Review of Public Health. 1992;13:99–126. doi: 10.1146/annurev.pu.13.050192.000531. [DOI] [PubMed] [Google Scholar]
- Blaxter M. Health and lifestyles. London: Tavistock; 1990. [Google Scholar]
- Bond Huie SA, Krueger PM, Rogers RG, Hummer RA. Wealth, race, and mortality. Social Science Quarterly. 2003;84:667–684. [Google Scholar]
- Cohen S, Williamson GM. Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S, editors. The social psychology of health. Newbury Park, CA: Sage; 1988. pp. 31–67. [Google Scholar]
- Dawson DA. Beyond black, white, and Hispanic: Race, ethnic origin and drinking patterns in the United States. Journal of Substance Abuse. 1998;10:321–339. doi: 10.1016/s0899-3289(99)00009-7. [DOI] [PubMed] [Google Scholar]
- Farmer MM, Ferraro KF. Are racial disparities in health conditional on socioeconomic status? Social Science and Medicine. 2005;60:191–204. doi: 10.1016/j.socscimed.2004.04.026. [DOI] [PubMed] [Google Scholar]
- Ferrie JE, Shipley MJ, Cappuccio FP, Brunner E, Miller MA, Kumari M, Marmot MG. A prospective study of change in sleep duration: Associations with mortality in the Whitehall II cohort. Sleep. 2007;30:1659–1666. doi: 10.1093/sleep/30.12.1659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman EM, Hayney MS, Love GD, Urry HL, Rosenkranz MA, Davidson RJ, Singer BH, Ryff CD. Social relationships, sleep quality, and interleukin-6 in aging women. Proceedings of the National Academy of Sciences. 2005;102:18757–18762. doi: 10.1073/pnas.0509281102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus AT, Neidert LJ, Bound J. Age patterns of smoking in us black and white women of childbearing age. American Journal of Public Health. 1993;83:1258–1264. doi: 10.2105/ajph.83.9.1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenland S. Dose-response and trend analysis in epidemiology: Alternatives to categorical analysis. Epidemiology. 1995;6:356–365. doi: 10.1097/00001648-199507000-00005. [DOI] [PubMed] [Google Scholar]
- Hayward MD, Heron M. Racial inequality in active life among adult Americans. Demography. 1999;36:77–91. [PubMed] [Google Scholar]
- Hayward MD, Crimmins EM, Miles T, Yang Y. The significance of socioeconomic status in explaning the racial gap in chronic health conditions. American Sociological Review. 2000;65:910–930. [Google Scholar]
- Kahn JR, Fazio EM. Economic status over the life course and racial disparities in health. Journal of Gerontology: Social Sciences. 2005;60B:76–84. doi: 10.1093/geronb/60.special_issue_2.s76. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Mickelson KD, Williams DR. The prevalence, distribution, and mental health correlates of perceived descrimination in the United States. Journal of Health and Social Behavior. 1999;40:208–230. [PubMed] [Google Scholar]
- Kessler RC, Galea S, Jones RT, Parker HA. Mental illness and suicidality after Hurricane Katrina. Bulletin of the World Health Organization. 2006;84:930–939. doi: 10.2471/blt.06.033019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korn EL, Graubard BI, Midthune D. Time-to-event analysis of longitudinal follow-up of a survey: Choice of the time-scale. American Journal of Epidemiology. 1997;145:72–80. doi: 10.1093/oxfordjournals.aje.a009034. [DOI] [PubMed] [Google Scholar]
- Krueger PM, Rogers RG, Hummer RA, LeClere FB, Bond Huie SA. Socioeconomic status and age: The effect of income sources and portfolios on adult mortality in the United States. Sociological Forum. 2003;18:465–482. [Google Scholar]
- Krueger PM, Chang VW. Being poor and coping with stress: Health behaviors and the risk of death. American Journal of Public Health. 2008;98:889–896. doi: 10.2105/AJPH.2007.114454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger PM, Friedman EM. Sleep duration in the United States: A cross-sectional population based study. American Journal of Epidemiology. 2009;169:1052–1063. doi: 10.1093/aje/kwp023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuzawa CW, Sweet E. Epigenetics and the embodiment of race: Developmental origins of us racial disparities in cardiovascular health. American Journal of Human Biology. 2009;21:2–15. doi: 10.1002/ajhb.20822. [DOI] [PubMed] [Google Scholar]
- Markides KS, Coreil J. The health of Southwestern hispanics: An epidemiological paradox. Public Health Reports. 1986;101:253–265. [PMC free article] [PubMed] [Google Scholar]
- Massey DS. Segregation and stratification: A biosocial perspective. Du Bois Review. 2004;1:7–25. [Google Scholar]
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. Journal of the American Medical Association. 2004;291:1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- Montez JK, Hayward MD. Early life conditions and later life mortality. In: Rogers RG, Crimmins EM, editors. International handbook of adult mortality. New York: Springer; 2011. [Google Scholar]
- Moore DJ, Williams JD, Qualls WJ. Target marketing of tobacco and alcohol related products to ethnic minority groups in the United States. Ethnicity & Disease. 1996;6:83–98. [PubMed] [Google Scholar]
- National Center for Health Statistics. 1990 family resources supplement to the national health interview survey. Hyattsville, MD: US Department of Health and Human Services; 1992. [Google Scholar]
- National Center for Health Statistics. National health interview survey, 1990: Health promotion and disease prevention sample person supplement. Hyattsville, MD: US Department of Health and Human Services; 1993. [Google Scholar]
- National Center for Health Statistics. National health interview survey, multiple cause of death public use data file: 1986–2006 survey years. Hyattsville, MD: US Department of Health and Human Services; 2010. [Google Scholar]
- Ng DM, Jeffery RW. Relationships between perceived stress and health behaviors in a sample of working adults. Health Psychology. 2003;22:638–642. doi: 10.1037/0278-6133.22.6.638. [DOI] [PubMed] [Google Scholar]
- Nielsen NR, Kristensen TS, Schnohr P, Gronbaek M. Perceived stress and cause-specific mortality among men and women: Results from a prospective cohort study. American Journal of Epidemiology. 2008;168:481–491. doi: 10.1093/aje/kwn157. [DOI] [PubMed] [Google Scholar]
- Pampel FC, Rogers RG. Socioeconomic status, smoking, and health: A test of competing theories of cumulative advantage. Journal of Health and Social Behavior. 2004;45:306–321. doi: 10.1177/002214650404500305. [DOI] [PubMed] [Google Scholar]
- Pampel FC, Krueger PM, Denney JT. Socioeconomic disparities in health behaviors. Annual Review of Sociology. 2010;36:349–370. doi: 10.1146/annurev.soc.012809.102529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parrott AC. Does cigarettes smoking cause stress? American Psychologist. 1999;54:817–820. doi: 10.1037//0003-066x.54.10.817. [DOI] [PubMed] [Google Scholar]
- Powell LM, Slater S, Chaloupka FJ, Harper D. Availability of physical activity-related facilities and neighborhood demographic and socioeconomic characteristics: A national study. American Journal of Public Health. 2006;96:1676–1680. doi: 10.2105/AJPH.2005.065573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raftery AE. Bayesian model selection in social research. Sociological Methodology. 1995;25:111–163. [Google Scholar]
- Reynolds K, Lewis LB, Nolen JDL, Kinney GL, Sathya B, He J. Alcohol consumption and risk of stroke: A meta-analysis. Journal of the American Medical Association. 2003;289:579–588. doi: 10.1001/jama.289.5.579. [DOI] [PubMed] [Google Scholar]
- Rogers RG, Hummer RA, Nam C. Living and dying in the USA: Behavioral, health, and social differentials of adult mortality. New York, NY: Academic; 2000. [Google Scholar]
- Rogers RG, Hummer RA, Krueger PM, Pampel FC. Mortality attributable to cigarette smoking in the United States. Population and Development Review. 2005;31:259–292. doi: 10.1111/j.1728-4457.2005.00065.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salmon P. Effects of physical exercise on anxiety, depression, and sensitivity to stress: A unifying theory. Clinical Psychology Review. 2001;21:33–61. doi: 10.1016/s0272-7358(99)00032-x. [DOI] [PubMed] [Google Scholar]
- StataCorp. Stata statistical software: Release 11.0. College Station, TX: Stata Press; 2009. [Google Scholar]
- Stellman SD, Chen Y, Muscat JE, Djordjevic MV, Richie JP, Lazarus p, Thompson S, Altorki N, Berwick M, Citron ML, Harlap S, Kaur TB, Neugut AI, Olson S, Travaline JM, Witorsch P, Shang ZF. Lung cancer risk in white and black Americans. Annals of Epidemiology. 2003;13:294–302. doi: 10.1016/s1047-2797(02)00420-9. [DOI] [PubMed] [Google Scholar]
- Sterling TD, Weinkam JJ. Comparisons of smoking-related risk factors among black and white males. American Journal of Industrial Medicine. 1989;15:319–333. doi: 10.1002/ajim.4700150307. [DOI] [PubMed] [Google Scholar]
- Sudano JJ, Baker DW. Explaining us racial/ethnic disparities in health declines and mortality in late middle age: The roles of socioeconomic status, health behaviors, and health insurance. Social Science & Medicine. 2006;62:909–922. doi: 10.1016/j.socscimed.2005.06.041. [DOI] [PubMed] [Google Scholar]
- Thoits PA. Stress, coping, and social support processes: Where are we? What next? Journal of Health and Social Behavior. 1995;35:53–79. [PubMed] [Google Scholar]
- Thun MJ, Peto R, Lopez AD, Monaco JH, Henley J, Heath CW, Doll R. Alcohol consumption and mortality among middle-aged and elderly U.S. Adults. New England Journal of Medicine. 1997;337:1705–1714. doi: 10.1056/NEJM199712113372401. [DOI] [PubMed] [Google Scholar]
- Turner RJ, Avison WR. Status variations in stress exposure: Implications for the interpretation of research on race, socioeconomic status, and gender. Journal of Health and Social Behavior. 2003;44:488–505. [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Healthy people 2010: Understanding and improving health. 2. Washington, DC: U.S. Government Printing Office; 2000. [Google Scholar]
- Warburton DM. Smoking within reason. Journal of Smoking Related Diseases. 1992;3:55–59. [Google Scholar]
- Williams DR. Race and health: Basic questions, emerging directions. Annals of Epidemiology. 1997;7:322–333. doi: 10.1016/s1047-2797(97)00051-3. [DOI] [PubMed] [Google Scholar]
- Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health: Socioeconomic status, stress, and discrimination. Journal of Health Psychology. 1997;2:335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]