Abstract
Background and Purposes
Most colorectal tumors develop from adenomatous polyps, which are detected by colonoscopy. African Americans (AAs) have higher incidence of colorectal cancer (CRC) and greater mortality from this disease than Caucasian Americans (CAs). We investigated whether differences in predisposition to CRC and its surrogate (colonic adenomas) between these ethnic groups were related to numbers of cancer stem or stem-like cells (CSCs) in colonocytes.
Methods
We analyzed colonic effluent from 11 AA and 14 CA patients who underwent scheduled colonoscopy examinations at the John D. Dingell Veterans Affairs Medical Center. We determined proportions of cells that expressed the CSC markers CD44 and CD166 by flow cytometry.
Results
The proportion of colonocytes that were CD44+CD166– in effluent from patients with adenomas was significantly greater than from patients without adenomas (P = 0.01); the proportion of CD44+CD166+ colonocytes was also greater (P = 0.07). Effluent from AAs with adenomas had 60 % more CD44+166– colonocytes than from CAs with adenomas. Using cutoff values of 8 % for AAs and 3 % for CAs, the proportion of CD44+166– colonocytes that had positive predictive value for detection of adenomas was 100 % for AAs and CAs, determined by receiver operator characteristic curve analysis.
Conclusion
The proportion of CD44+166– colonocytes in colonic effluent can be used to identify patients with adenoma. AAs with adenomas have a higher proportion of CD44+166– colonocytes than CA. The increased proportion of CSCs in colonic tissue from AA might be associated with the increased incidence of CRC in this population.
Keywords: Colonic adenoma, Colon cancer stem cells, African American, Caucasians, Risk of colorectal cancer, ROC analysis
Introduction
Colorectal cancer (CRC) is the third most common malignancy in the USA; the estimated incidence is approximately 150,000 cases and 50,000 deaths per year [1]. Many of these deaths could be prevented with early detection and better screening modalities. Although most CRCs originate from adenomatous polyps, intracellular events associated with development and progression remain to be elucidated.
Increasing evidence suggests that many epithelial cancers, including CRC, are diseases driven by subpopulations of self-renewing cancer stem/cancer stem-like cells (CSCs) [2]. They resemble their adult stem cell counterparts. Although the origin of CSCs is not fully known, it is widely believed that they arise upon mutations of normal stem cells or progenitors [2]. Colon CSCs are thought to exist as undifferentiated cells at the base of the functional unit of epithelial cells in the crypts of Lieberkühn of colonic mucosa [3]. The undifferentiated cells migrate up the luminal surface where they become differentiated and are shed in the fecal stream as exfoliated colonocytes.
Currently, CSCs can be identified on the basis of specific surface epitopes. Cells expressing these surface epitopes have the ability to form tumors at a much diluted concentration in SCID mice and histologically resemble the primary tumor from which they were derived [4, 5]. Although colon CSCs were initially characterized as cells expressing CD133, subsequent reports have indicated that the vast majority of CD133 positive cells were not CSCs and thus CD133 could not be relied on as a single marker of colon CSCs [6]. For example, Chu et al. did not observe enhanced tumor-initiating capacity of CD133-positive cells isolated from three different primary colon tumors to form tumors in mice [7], and Feng et al. [8] found no difference in the tumor-initiating capacity of CD133-positive or negative HCT116 cells [8]. Recent studies suggest that cells expressing CD44, CD166, and EpCAM/ESA (epithelialspecific antigen, also known as EPCAM) surface markers derived from both CD133+ and CD133– colon cancers have the ability to form tumors, which could be used as markers for colon CSCs [4, 5].
Colorectal cancer (CRC) is an age-related disease in that the incidence of CRC increases sharply with advancing age. Recently, we reported that the number of colonic adenomas, the precursor of colon adenocarcinoma, increase linearly with advancing age and that this is associated with increased CSCs in macroscopically normal mucosa, as evidenced by the increased expression of CD44, CD166, and ESA [9].
Although colonic adenomas and CRC occur in all ethnicities, greater prevalence and higher mortality from CRC is observed among African Americans (AAs) than among other ethnicities [10]. In addition, AAs have worse prognosis than Caucasians Americans (CAs), tend to be diagnosed at a later stage, and suffer from more differentiated tumors [11]. The cellular events and underlying biochemical mechanisms of the differences in the incidence of CRC between the two ethnic groups are poorly understood. We hypothesize that one of the differences in predisposition to CRC and its surrogate (colonic adenomas) between the two ethnic groups could be related to the presence of CSCs in the colonic mucosa. We have tested this hypothesis by examining the proportions of cells in colonic effluent, taken during colonoscopy, expressing CD44+166–,CD44–CD166+, and CD44+CD166+ phenotypes. The rationale for using these markers is based on the observation that the propensity of CSCs to form tumors in SCID mice is much greater if they co-express CD44 and CD166 [4]. This potential non-invasive methodology, which hitherto has not been described, reveals a relationship between adenomas in the colon and the proportion of CD44+166–-expressing cells in colonic effluent collected during colonoscopy.
Methods
Study Population and Colonoscopy
The study was approved by the Institutional Review Boards and Committees of the John D. Dingell-Veterans Affairs Medical Center (JDD-VAMC) and Wayne State University (WSU) School of Medicine. Eligible study subjects were between the ages of 40 and 80 years, scheduled for an outpatient colonoscopy at JDD-VAMC from April to August 2010. Patients who were excluded from the study were those with active malignant disease, inflammatory bowel disease, recent infection, and those with psychiatric or addictive disorder, hemorrhagic diathesis, or on warfarin. Patients were doubly consented, once by the gastroenterologist for the colonoscopy and again by the study coordinator, for participation in the study.
All study subjects received standard colonoscopy purgative preparation in accordance with the usual protocol. Briefly, the patients are asked to take a preparation consisting of 15 mg Bisacodyl the morning before their colonoscopy and one gallon of poly(ethylene glycol) (PEG) solution in the evening. Those scheduled for colonoscopy in the afternoon were instructed to drink the second half of the PEG solution 5 h before their appointment.
Colonocyte Isolation
During the colonoscopy a sample of retained colonic fluid “effluent” was aspirated through the working channel of the endoscope. Approximately 10–20 ml effluent was diluted with phosphate-buffered saline (PBS). Mucosal cells that primarily represent colonocytes were isolated by use of the Somatic Cell Sampling and Recovery (SCSR) fecal cell isolation kit [12] (NonInvasive Technologies, Elkridge, MD, USA) with modifications to the manufacturer's directions. Previous studies had revealed exfoliated cells to be primarily colonocytes, because they were found to express cytokeratins indicating epithelial lineage [13, 14]. Approximately 1–2 × 106 colonocytes were obtained per patient.
Flow Cytometry
All reagents and instrumentation used for flow cytometry were from BD Biosciences (San Jose, CA, USA). Colonocyte supernatant was removed, cells were washed in ice cold Pharmingen stain buffer (PSB) and resuspended in 50 ll PSB. The cells were stained with fluorophore-conjugated monoclonal antibodies as follows: with anti-CD45-PerCP-Cy5.5 (clone 2D1), anti-CD44-PECy7 (G44-26), and anti-CD166-PE (clone 3A6) or isotype-matched IgG1-PerCP-Cy5.5 (×40), IgG2b-PE-Cy7, and IgG1-PE (BD Pharmingen, San Diego, CA, USA) as a negative control. The cells, stained with antibodies, were incubated for 50 min at 4 °C then washed and resuspended in 1 ml PSB. Compbeads Plus particles were stained in parallel, in accordance with the manufacturer's directions, to provide compensation controls. Flow cytometry was performed on a FACS Vantage SE SORP and data analyzed with CellQuest.
Statistical Analysis
Because this was a pilot study with a relatively small number of subjects, we were unable to perform sample size calculation. All acquired data were entered in an Excel spreadsheet (2010 version, Microsoft, Richmond, VA, USA). Data were analyzed by use of SPSS version 16.0 (IBM, Somers, NY, USA).
Continuous variables are presented as mean and standard deviation, whereas categorical variables are presented as count and proportion. Two sample t tests and χ2 tests were used to compare means and proportions between the groups, as appropriate. When significant heterogeneity of variance was observed for the groups, corrections were made by using the appropriate tests. For all tests, a two-sided P value less than 0.05 was considered significant.
Receiver operator characteristic (ROC) curve analysis was used to classify subjects into one of two categories, in this case, adenomas and no adenomas, which were based on the proportion of colonocytes expressing CD44+CD166–. The latter represents the proportion of cells isolated from colonic effluent. Contingency tables were used to determine characteristics of different cutoff values.
Results
Study Population
Twenty-seven patients were enrolled in the study. Of those, three patients were removed and not included in the analyses. One was of Hispanic descent, one was a statistical outlier (an African American female with eight adenomatous polyps), and one Caucasian male had Crohn's disease. The final sample included analyses from 24 individuals (Table 1) averaging 58.7 ± 7.4 years of age, most of whom were males (88 %). The sample was 46 % AAs and 54 % CAs.
Table 1.
Patient characteristics
| Characteristic | AA (n = 11) | CA (n = 13) | All (n = 24) |
|---|---|---|---|
| Ethnicity (%) | 46 | 54 | 100 |
| Age (year) | 58.2 ± 6.3 | 59.1 ± 8.4 | 58.7 ± 7.4 |
| Gender (male, %) | 100 | 77 | 88 |
| Patients with adenomas (n, %) | 5 (45) | 8 (62) | 13 (54) |
| Adenomas per patient | 2.8 ± 1.3 | 2.6 ± 2.1 | 2.7 ± 1.8 |
| Location of adenomas (proximal, %) | 79 | 48 | 60 |
Numbers in parentheses are the percentage of patients with adenomas AA, African American; CA, Caucasian American; values are expressed as mean ± SD
Location but Not Number of Adenomas Differs by Ethnicity
Of the 24 patients, 13 had adenomas (54 %), of which five were from AAs, (45 %) and eight were from CAs (62 %). For patients with adenomas, the average number of adenomatous polyps was 2.7 ± 1.8. The number of adenomas per patient was comparable for AAs, 2.8 ± 1.3, and CAs, 2.6 ± 2.1; (t = 0.19, P = NS) (Table 1). The dominant side for adenomatous polyps was proximal for AAs (79 %) whereas it was distal for CAs (52 %) (Table 1), an observation similar to that noted by others [11, 15, 16]. All polyps were <1 cm.
Expression of CD44 and CD166 in Colonocytes Differs by Polyp Status
To determine colonocytes expressing CD44 and CD166 it is important to exclude cells of lymphoid origin which may also express these markers. CD45 is a pan leukocyte marker, but is not expressed in colonocytes [12]. In our investigation, CD45+ cells were excluded from analysis by use of software and the phenotypes reported are therefore implicitly CD45–.
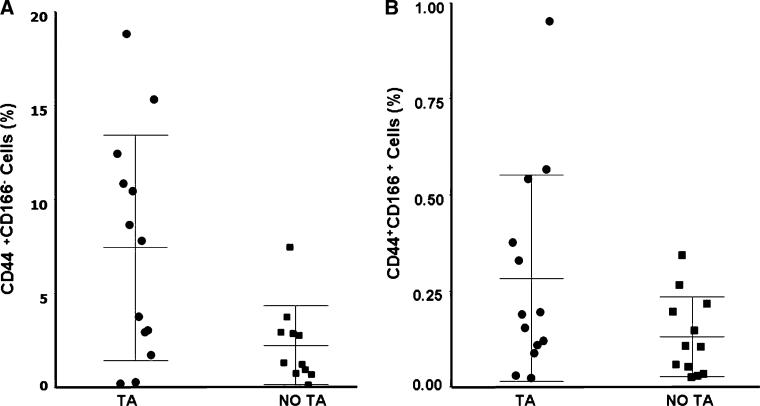
When subjects with and without adenomas were taken into account, the proportion of CD44+CD166– colonocytes was found to be 5.1 ± 5.2 %, (0.12–18.9 %). However, patients with adenomas had a 222 % higher proportion of cells expressing CD44+CD166– than those without adenomas; 7.4 ± 6.0 % versus 2.3 ± 2.1 %, respectively (Fig. 1a), a difference which was found to be highly significant, (P = 0.01). In contrast, no significant difference between CD44–CD166+ expression by the two groups was observed (data not shown). For the entire patient population, the proportion of colonocytes expressing CD44+166+ was found to be 0.21 ± 0.22 %, (0.024–0.96 %). As has been observed for CD44+CD166–, patients with adenomas also had a 133 % higher proportion of cells co-expressing CD44 and CD166 than those without adenomas; 0.28 ± 0.27 % versus 0.12 ± 0.10 %, respectively (Fig. 1b; P = 0.07).
Fig. 1.
Proportion of colonocytes expressing a CD44+CD166– and b CD44+CD166+ varies for patients with tubular adenoma (TA) and without tubular adenoma (No TA). Bars show mean ± SD)
Colonocyte CD44 and CD166 Expression in Different Ethnic and Age Groups
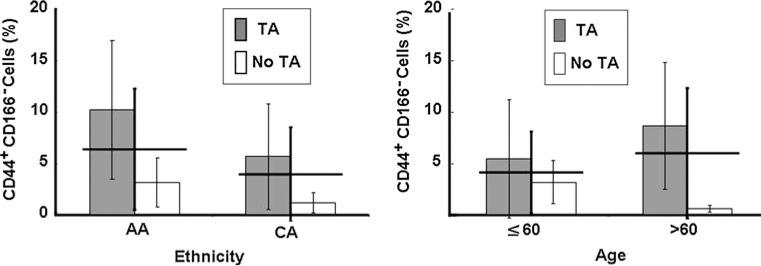
The effects of ethnicity and age on CD44 and CD166 expression by colonocytes from effluent were investigated. When the results from all subjects were analyzed we observed that the proportion of colonocytes expressing CD44+CD166– was 60 % higher for AAs than for CAs; 6.4 ± 5.9 % versus 4.0 ± 4.6 %, respectively, but the difference was not statistically significant (Fig. 2) (t = 1.1, P = NS). It was further observed that expression of CD44+CD166– by colonocytes from subjects aged ≤60 years with adenomas was 32 % lower than for those aged >60 years; 4.1 ± 4.0 % versus 6.0 ± 6.3 %, respectively; the difference was not statistically significant (Fig. 2), (t = 0.49, P = NS). In contrast, CD44–CD166+ expression by colonocytes in AA subjects was 33 % lower than in CAs; 0.32 ± 0.68 % versus 0.48 ± 0.84 %, respectively. Expression of CD44–CD166+ in colonocytes from patients aged ≤60 years was 38 % less than for those >60 years of age, 0.31 ± 0.65 % versus 0.50 ± 0.87 %, respectively. On the other hand, the proportion of colonocytes co-expressing CD44 and CD166 was found to be very similar between patients ≤60 years of age and those <60 years as well as between AAs and CAs (data not shown).
Fig. 2.
Colonocyte CD44+CD166– expression in African Americans (AAs) and Caucasian Americans (CAs; thick lines, mean ± SD). CD44+CD166– colonocytes in patients aged ≤60 and patients >60 (thick lines, mean ± SD). By ethnicity or age, patients with tubular adenoma (shaded bars) had a higher proportion of colonocytes expressing CD44+CD166– than those without adenomas. Values are expressed as mean ± SD
Colonocyte CD44+CD166– Expression with Ethnicity Predicts Polyp Status
ROC curve analysis of the proportion of colonocytes expressing CD44+CD166– which predicted the presence of adenomas, found the area under the curve (AUC) to be 0.79. When an optimum cut off score of 8.0 % for colonocytes expressing CD44+CD166– was used, all the subjects above that score had at least one adenoma (specificity = 100 %), but the sensitivity was only 54 % (13/25). The analysis was repeated for the two different ethnic groups. For AA participants (N = 11), the ROC analysis found an AUC score of 0.80 by using CD44+CD166– expression to predict the presence of adenomas. An optimum cutoff score of 8.0 % resulted in 80 % sensitivity, with 100 % specificity for AA participants (Table 2). The overall accurate classification rate of 91 % resulted in a positive predictive value of 100 % (4/4) and a negative predictive value of 86 % (6/7). For the CA participants (N = 13), the AUC was 0.88 using the CD44+CD166– expression to predict the presence of adenomas. With a cutoff score of 3.0 %, sensitivity was found to be 63 % and specificity 100 % for CA participants, which results overall in 77 % accurate classification, with 100 % (5/5) positive predictive value and 63 % (5/8) negative predictive value.
Table 2.
Contingency tables using CD44+ CD166– expression and ethnicity
| Contingency table for African Americans, 8.00 % cutoffa | Disease present |
|
|---|---|---|
| Adenomatous polyps (n = 5) | No polyps (n = 6) | |
| Predicted disease | ||
| Adenomatous polyps | 4 | 0 |
| No polyps | 1 | 6 |
| Contingency table for Caucasian Americans, 3.00 % cutoffb | Disease present |
|
|---|---|---|
| Adenomatous polyps (n = 8) | No polyps (n = 5) | |
| Predicted disease | ||
| Adenomatous polyps | 5 | 0 |
| No polyps | 3 | 5 |
10/11 of original cases grouped correctly
Sensitivity: 4/5 = 80 %
Specificity: 6/6 = 100 %
Positive predictive value: 4/4 = 100 %
Negative predictive value: 6/7 = 86 %
10/13 of original cases grouped correctly
Sensitivity: 5/8 = 63 %
Specificity: 5/5 = 100 %
Positive predictive value: 5/5 = 100 %
Negative predictive value: 5/8 = 63 %
Discussion
Colorectal cancer is the third most common cancer in the United States and the second leading cause of deaths, with an estimated 150,000 newly diagnosed cases and 50,000 deaths in 2010 [1]. The risk of developing CRC increases over the age of 50. However, early detection has been shown to improve survival. Currently available screening methods have significant limitations and do not take into account the basic mechanisms behind the development of CRC and its precursor, the adenomatous polyp. CRC stem cells are thought to be a predisposing factor for the development of CRC. Many studies suggest that epithelial cancers including CRC arise from a small subpopulation of CSCs as a result of oncogenic transformations [17]. Studies by our laboratory have revealed the presence of colon CSCs in humans, as evidenced by the expression of CD44, CD166, and ESA not only in premalignant adenomatous polyps, but also in normal appearing colonic mucosa, where expression of several CSC markers was found to increase with advancing age, indicating increased risk in developing colorectal cancer during aging [9]. We also reported that expression of each CSC marker in normal appearing colonic mucosa is approximately twofold higher in subjects with 3–4 polyps than those with 1–2 polyps [9]. However, no information is available about whether CSCs are shed into the colonic lumen by subjects with adenomatous polyps and whether they could be utilized as a predictor of the process of colon carcinogenesis. In this investigation, colonic effluent was obtained while patients were undergoing colonoscopy, in lieu of samples that can be obtained by the patients themselves (an objective of the fecal cell isolation kit). Our results reveal, for the first time, the presence of CSCs in colonocytes collected during colonoscopy, as evidenced by the expression of CD44 and CD166 in cells from the colonic effluent and subsequently analyzed by flow cytometry.
The fact that the proportion of colonocytes expressing CD44+166– is significantly higher for patients with tubular adenomas than for those without suggests that the presence of CD44+CD166– phenotypes could be a predictor of adenomas. Additional support for our postulation of CD44+CD166– phenotype being a reliable predictor of adenomas is derived from receiver operator characteristic (ROC) curve analysis in which optimum cut off scores of 8 % for AAs and 3 % for CAs for CD44+CD166– colonocytes were 100 % specific for the presence of adenomas in AAs and CAs. In contrast, the proportion of colonocytes expressing CD44–CD166+ was not significantly different between the two groups of patients, indicating a lack of predictive value for CD44–CD166+ phenotype for early adenomas. This may not be surprising, because CD166 is a CSC marker for metastases [18], and all the polyps in the current investigation were <1 cm in size. This could also be one reason why colonocytes in the effluent co-expressing CD44 and CD166 could not be a reliable predictor of adenomas. Further support for this inference comes from the observation that the proportion of CD44 and CD166 is only marginally higher in patients with adenomas than those without.
It is becoming increasingly evident that incidence of and mortality from CRC are higher for AAs than for non-African Americans in the USA [10]. Neither the causative factor(s) nor the regulatory mechanisms for the increased incidence of CRC among AAs are clearly understood. One reason could be less screening among AAs than among other ethnic groups in the USA [10, 11]. However, with regard to the regulatory mechanisms, our current observation for the first time demonstrates a markedly higher proportion of CD44+CD166– colonocytes in colonic effluent of AAs with adenomas than in that of CAs. This suggests that induction of CSCs in the colonic mucosa of AAs could be one of the factors contributing to the increased incidence of this malignancy in this group. It has also been reported that AAs have more polyps on the proximal side and that advanced cancer is more frequent among AAs than CAs [11, 16]. Whether this could also be attributable to the induction of CSCs, specifically CD44+CD166–-expressing colonocytes, remains to be determined.
In conclusion, our results show that colonocytes isolated from colonic effluent express a set of markers associated with cancer stem or stem-like cell markers. We have further observed a marked increase in the proportion of colonocytes expressing CSC phenotype CD44+CD166– in patients with adenomas than in those without adenomas. Moreover, our observation that AAs with adenomas have a higher proportion of CD44+CD166– colonocytes than CAs suggests that CSCs could be a predisposing factor for the increased incidence of colorectal cancer in AAs.
Acknowledgments
We wish to thank Pastor George D. Wilkinson and Word of Life Christian Church in Flint Michigan for so graciously donating money for the reagents in this study. We also want to thank Dr Padmanabhan Nair of NonInvasive Technologies for the colonocyte isolation supplies. We also wish to acknowledge the Nursing Staff and Physicians of the Gastroenterology Unit at the JDD-VAMC for their support in helping with the patients who participated in the study. Most of all we wish to thank the patients of the JDD-VAMC for their heart-felt participation. This material is the result of work supported with resources and the use of facilities at the JDD-VAMC. The work was supported by the NIH/NIA Diversity Supplement 5R01AG014343-13 and the Department of Veterans Affairs to Dr Majumdar.
Footnotes
The contents of this manuscript do not represent the views of the Department of Veterans Affairs or the United States Government.
Conflict of interest None of the authors have any conflict of interest with the submitted manuscript.
References
- 1.Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010;60:277–300. doi: 10.3322/caac.20073. [DOI] [PubMed] [Google Scholar]
- 2.Jordan CT, Guzman ML, Noble M. Cancer stem cells. N Engl J Med. 2006;355:1253–1261. doi: 10.1056/NEJMra061808. [DOI] [PubMed] [Google Scholar]
- 3.Ricci-Vitiani L, Fabrizi E, Palio E, De Maria R. Colon cancer stem cells. J Mol Med. 2009;87:1097–1104. doi: 10.1007/s00109-009-0518-4. [DOI] [PubMed] [Google Scholar]
- 4.Dalerba P, Dylla SJ, Park IK, et al. Phenotypic characterization of human colorectal cancer stem cells. Proc Natl Acad Sci USA. 2007;104:10158–10163. doi: 10.1073/pnas.0703478104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.O'Brien CA, Pollett A, Gallinger S, Dick JE. A human colon cancer cell capable of initiating tumour growth in immunodeficient mice. Nature. 2007;445:106–110. doi: 10.1038/nature05372. [DOI] [PubMed] [Google Scholar]
- 6.Sanders MA, Majumdar APN. Colon cancer stem cells: implications in carcinogenesis. Front Biosci. 2011;16:1651–1662. doi: 10.2741/3811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chu P, Clanton DJ, Snipas TS, et al. Characterization of a sub-population of colon cancer cells with stem cell-like properties. Int J Cancer. 2009;124(6):1312–1321. doi: 10.1002/ijc.24061. [DOI] [PubMed] [Google Scholar]
- 8.Feng HL, Liu YQ, Yang LJ, et al. Expression of CD133 correlates with differentiation of human colon cancer cells. Cancer Biol Ther. 2010;9(3):216–223. doi: 10.4161/cbt.9.3.10664. [DOI] [PubMed] [Google Scholar]
- 9.Patel BB, Yu Y, Du J, Levi E, Phillip PA, Majumdar AP. Age-related increase in colorectal cancer stem cells in macroscopically normal mucosa of patients with adenomas: a risk factor for colon cancer. Biochem Biophys Res Commun. 2009;378:344–347. doi: 10.1016/j.bbrc.2008.10.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Agrawal S, Bhupinderjit A, Bhutani MS, et al. Colorectal cancer in African Americans. Am J Gastroenterol. 2005;100:515–523. doi: 10.1111/j.1572-0241.2005.41829.x. discussion 514. [DOI] [PubMed] [Google Scholar]
- 11.Dimou A, Syrigos KN, Saif MW. Disparities in colorectal cancer in African-Americans vs Whites: before and after diagnosis. World J Gastroenterol. 2009;15:3734–3743. doi: 10.3748/wjg.15.3734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Somatic Cell Sampling & Recovery Fecal Cell Isolation Kit: Protocols and Recommendations. Technologies N; Elkridge: 2009. http://noninvasivetech.com/ [Google Scholar]
- 13.Albaugh GP, Iyenger V, Lohani A, Malayeri M, Bala S, Nair PP. Isolation of exfoliated colonic epithelial cells, a novel, noninvasive approach to the study of cellular markers. Int J Cancer. 1992;52:347–350. doi: 10.1002/ijc.2910520303. [DOI] [PubMed] [Google Scholar]
- 14.Iyenger V, Albaugh GP, Lohani A, Nair PP. Human stools as source of viable colonic epithelial cells. FASEB. 1991;5:2856–2859. doi: 10.1096/fasebj.5.13.1655550. [DOI] [PubMed] [Google Scholar]
- 15.Thornton JG, Morris AM, Thornton JD, Flowers CR, McCash-land TM. Racial variation in colorectal polyp and tumor location. J Natl Med Assoc. 2007;99:723–728. [PMC free article] [PubMed] [Google Scholar]
- 16.Nouraie M, Hosseinkhah F, Brim H, Zamanifekri B, Smoot DT, Ashktorab H. Clinicopathological features of colon polyps from African-Americans. Dig Dis Sci. 2010;55:1442–1449. doi: 10.1007/s10620-010-1133-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kanwar SS, Yu Y, Nautiyal J, Patel BB, Majumdar AP. The Wnt/beta-catenin pathway regulates growth and maintenance of colonospheres. Mol Cancer. 2010;9:212. doi: 10.1186/1476-4598-9-212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weichert W, Knosel T, Bellach J, Dietel M, Kristiansen G. ALCAM/CD166 is overexpressed in colorectal carcinoma and correlates with shortened patient survival. J Clin Pathol. 2004;57:1160–1164. doi: 10.1136/jcp.2004.016238. [DOI] [PMC free article] [PubMed] [Google Scholar]