Abstract
Aim
Medical providers often do not perform chest compressions in accordance with recommended resuscitation guidelines for adults and children. Little is known regarding how well neonatal providers perform coordinated chest compressions and ventilations. The objective of this study was to characterize Neonatal Resuscitation Program (NRP) trained providers' adherence to NRP recommendations for coordinated chest compressions and ventilations in a simulated setting.
Methods
Fifty NRP providers performed coordinated chest compressions for three minutes on a neonatal manikin. A compression sensor (accelerometer) was used to monitor and record compression data. Data analyzed included ratio of compressions to ventilation pauses, delivered chest compressions per minute (CC/min), and duration of ventilation pauses.
Results
Delivered CC/min ranged from 61 to 136. The mean CC/min (99, SD 16) was significantly higher than the NRP-recommended value of 90 (p=0.002). Delivered CC/min did not differ from the first 30 seconds to the last 30 seconds of compressions (p=0.91). Duration of ventilation pauses was highly correlated with CC/min (Spearman's rho= -0.98, p<0.001), with a median duration of 0.92 seconds (IQ range (0.84, 1.02).
Conclusions
NRP trained providers often do not adhere to NRP recommendations for delivery of coordinated chest compressions during simulated cardiac depression. The mean CC/min performed is higher than recommended. Duration of ventilation pauses is highly correlated with delivered CC/min. Future studies should focus on methods to improve the timing of delivered chest compressions by NRP providers to conform to NRP recommendations.
Keywords: CPR, Neonatal, Manikin, Resuscitation, Chest compressions
Introduction
Neonatal chest compressions are essential for maintaining adequate cerebral and coronary perfusion during profound cardiac depression after birth. However, chest compressions and extensive cardiopulmonary resuscitation (CPR) are performed in only 0.08-0.12% of term infants after birth [1,2], so limited data exist regarding the quality of chest compressions and ventilations performed by neonatal providers. Chest compression performance in adult and pediatric populations often deviates from international resuscitation guidelines [3-7], raising the concern that the coordinated chest compressions performed in neonates also may not adhere to neonatal resuscitation guidelines.
Little is known regarding neonatal providers' performance of coordinated chest compressions and ventilations. A manikin study of European neonatal resuscitation guidelines for coordinated chest compressions and ventilations found that most providers did not deliver the targeted 40 ventilations/minute [8], but this study did not specifically report upon chest compressions performance. An infant manikin study of chest compressions performed by Advanced Pediatric Life Support providers demonstrated that >99% of compressions did not meet international recommendations regarding rate, depth, and duty cycle of compressions [9]. This was a study of continuous chest compressions; limited conclusions can be drawn related to coordinated chest compressions and ventilations.
Current Neonatal Resuscitation Program (NRP) guidelines include performing chest compressions coordinated with positive pressure ventilation in a 3:1 ratio, with 120 events performed per minute (90 compressions, 30 ventilations) [10]. Although these guidelines are widely published, little is known regarding how consistently providers follow these guidelines. Te aim of this study was to characterize NRP providers'adherence to NRP guidelines for the number of chest compressions and ventilationsdelivered per minute and the duration of time allocated to these interventions.
Methods
The Children's Hospital of Philadelphia Institutional Review Board approved this study (protocol # 811513). We enrolled fifty NRP providers who voluntarily participated as study subjects. A script was read to each subject describing a profoundly depressed neonate at birth. Each subject was instructed to use “the 2-thumb technique to perform coordinated chest compressions according to the NRP protocol” for 3 minutes on a SimNewB® manikin (Laerdal Medical, Stavanger, Norway), which represents a full term newborn female with growth parameters at the 50th percentile. No additional information was provided regarding optimal chest compressions. A study investigator provided ventilations when instructed by the subject using an infant self-inflating bag and neonatal facemask (Mercury Medical, Clearwater, FL, USA). A Heartstart 4000 (Philips Medical Systems, Andover, MA, USA) monitor/defibrillator continuously recorded the force and timing of chest compressions from a prototype neonatal compression sensor (accelerometer) (Laerdal Medical, Stavanger, Norway) placed under the subjects' thumbs. Subjects received no feedback during the study.
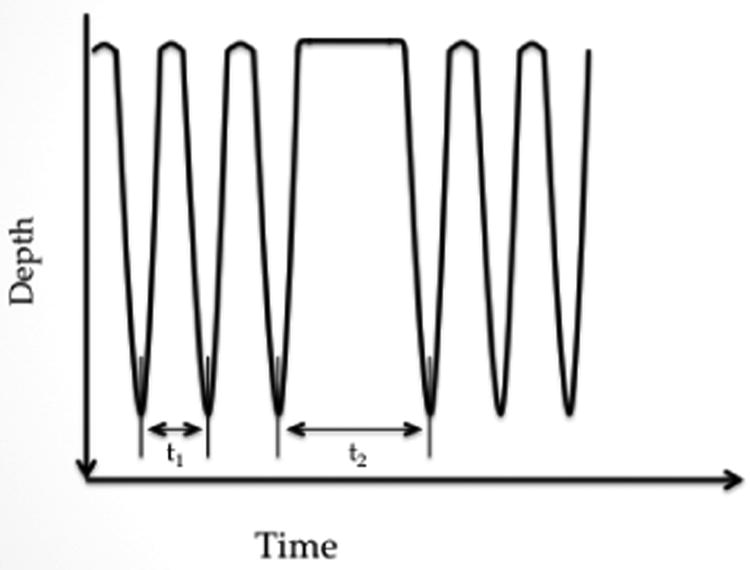
We used recorded data from the compression sensor to determine: ratio of compressions to ventilations, delivered chest compressions per minute (CC/min), and number and duration of ventilation pauses. Compression rate was calculated as the average reciprocal of the time interval between the maximal depth of one compression to the next, excluding ventilation pauses. Ventilation pauses were defined as time with no compression activity, from the peak of the last compression to the peak of the subsequent compression (Figure 1).
Figure 1.
Schematic of chest compressions. The time interval between peak depths of compressions excluding ventilation pauses (t1) was used to calculate compression rate. Ventilation pause was defined as the time between the peak of the last compression to the peak of the subsequent compression (t2).
Data analysis
Data analysis was performed only for subjects who utilized the recommended 3:1 ratio of compressions to ventilations using Stata 12.0 (StataCorp, College Station, TX, USA). Mean CC/min was compared to the NRP-recommended value of 90 with a one-sample t-test. Mean CC/min in the first 30 seconds was compared to the last 30 seconds with a paired t-test. “Correct CC/min” was defined as 80-100 CC/min, allowing a margin of 10 CC/min above and below the expected value of 90. Associations between correct CC/min and role in NRP and medical role were examined with χ2 and Fisher's exact test. Spearman's rank test was used to determine the correlation between CC/min and duration of ventilation pauses. A 2-sided p-value < 0.05 was considered statistically significant. A power analysis using data from a preliminary study indicated that a sample size of 50 would have > 99% power to detect a difference of 10 CC/min between the mean observed value and the hypothesized value of 90.
Results
The fifty subjects included pediatric residents (24%), neonatal fellows (14%), neonatal attending physicians (18%), neonatal nurses (28%), neonatal nurse practitioners/physician assistants/hospitalists (14%), and respiratory therapists (2%). Twelve subjects (24%) were NRP instructors or regional trainers. Te median time since NRP training for NRP providers was 7.5 months (IQ range 1, 12 months).
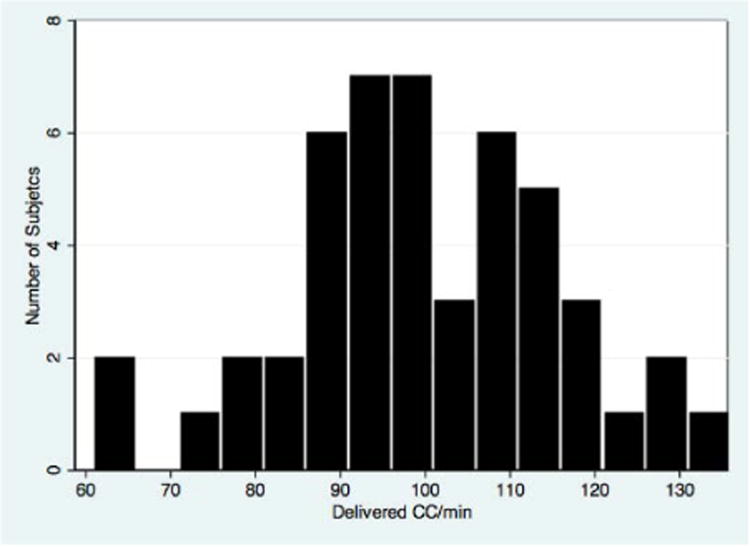
Of 50 subjects, 48 (96%) performed chest compressions and ventilations in the 3:1 ratio. One subject performed continuous chest compressions, and one performed compressions in a 4:1 ratio throughout the simulation. Te mean rate of chest compressions was 132 per minute (SD 22) (Table 1). Delivered CC/min ranged from 61 to 136 (Figure 2). Mean CC/min (99, SD16) was significantly higher than 90 (p<0.001). Mean CC/min did not differ between the first and last 30 seconds of compressions (p=0.91). Of the 48 evaluable subjects, 23 (48%) delivered between 80-100 CC/min. Tree (6%) delivered <80 CC/min, and 22 (46%) delivered >100 CC/min. There was no significant association between performing the correct number of CC/min and role on medical team (p=0.33) or role in NRP (p=0.14).
Table 1.
Chest compression and ventilation characteristics.
| Characteristic | Mean Value | |
|---|---|---|
| Delivered chest compressions per minute | Total | 99 (SD 16) |
| First 30 seconds | 100 (SD19) | |
| Last 30 seconds | 100 (SD17) | |
| Rate of chest compressions (per minute) | 132 (SD 22) | |
| Ventilations per minute | 33 (SD 5) | |
| Length of Ventilation pause (seconds) | 0.92 (0.84, 1.02)* | |
Median value (IQ range)
Figure 2.
Distribution of delivered chest compressions/minute (CC/min) delivered by study subjects.
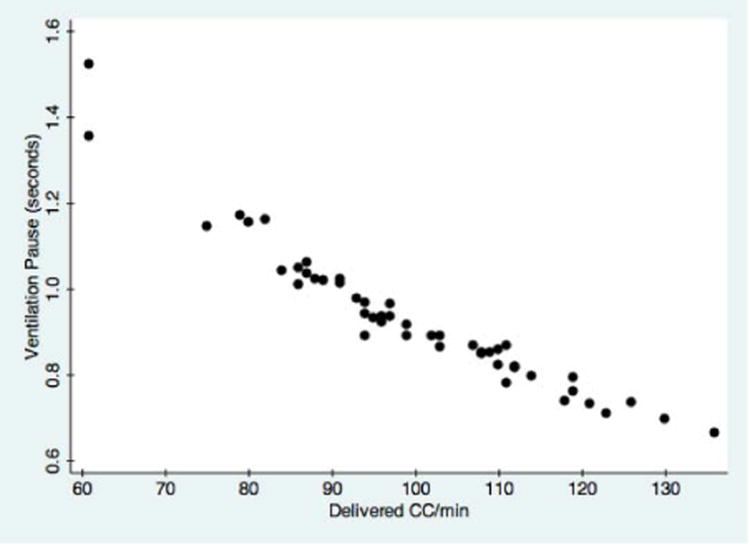
The mean number of pauses for ventilation per minute was 33 (SD 5). Duration of ventilation pausesranged from 0.66 to 1.52 seconds, with a median value of 0.92 seconds (IQ range 0.84, 1.02). Duration of ventilation pauses was highly correlated with CC/min; Spearman's rho= -0.98 (p<0.001). Ventilation breaks were longer when fewer CC/min were performed and shorter when more CC/min were performed (Figure 3).
Figure 3.
Scatter plot demonstrating the relationship between number of delivered chest compressions/minute (CC/min) and duration of ventilation pauses (seconds).
Discussion
We performed a neonatal manikin study to determine how consistently NRP providers adhere to NRP recommendations for chest compressions. Most providers performed the correct ratio of compressions to ventilations. There was large variation in number of delivered CC/min; most providers who were not in the targeted range of CC/min performed more CC/min than recommended. We did not observe any decay in delivered CC/min over time. Duration of ventilation pauses was highly correlated with CC/min, with longer ventilation pauses occurring when fewer CC/min were performed.
Our findings regarding delivered CC/min are comparable to other manikin studies of infant CPR. In a study investigating optimal hand position, subjects delivered a mean of 192 to 197 chest compressions over 2 minutes [11]. However, in that study, no ventilations were performed; the subjects simply said, “breathe” when ventilation should occur. An additional neonatal manikin study investigating the optimal ratio of chest compressions demonstrated that providers using a 3:1 ratio performed 194 compressions over 2 minutes [12]. It is unclear whether or how ventilation was delivered in that study. Subjects in our study had a similar mean number of delivered CC/min to these studies, even when positive pressure ventilation was actually performed. It is noteworthy that participants in those studies were briefly instructed on delivery of chest compressions prior to performing them, in contrast to our study, when subjects were told only to follow NRP protocol.
We measured the duration of ventilation pauses to determine if providers maintain an established cadence of compressions when pausing for ventilation. We defined ventilation pause as the interval from the peak of the last compression to the peak of the subsequent compression, in keeping with published recommendations for reporting CPR [3]. Each ventilation pause should last one second: 0.5 seconds occur between the peaks of serial compressions, and one ventilation is interposed after every three compressions, leaving two 0.5 second intervals for ventilation (Figure 1). Te median duration of ventilation pauses in this study was 0.92 seconds, but this value ranged widely, from 0.66 to 1.52 seconds. Te duration of ventilation pauses was very closely correlated with CC/min, suggesting that providers maintain an established cadence of chest compressions, even when pausing for delivery of ventilation. Therefore, initiating CPR with the correct rate of chest compressions is likely important for optimizing the duration of ventilation pauses.
The large variability in the number of delivered CC/min was independent of subjects' role on the medical team or in NRP. This variability may therefore not reflect gaps in knowledge regarding NRP recommendations but an inability to perform compressions at the specified rate. Audio feedback is a potential tool to help address this inconsistency. Studies of feedback during adult and infant CPR have demonstrated improved performance when feedback is used [13-16]. A metronome set to 120 beats/min may help standardize the delivery of chest compressions and ventilations in neonates to more closely align with NRP recommendations.
This study had several limitations. We did not record depth of compressions or quality of ventilations. It is important to know how the allocation of resuscitation time affects these characteristics. Next, a self-inflating bag was used to deliver ventilation. Many hospitals use devices such as a T-piece or flow-inflating bag for newborn resuscitation; the duration of ventilation pauses may differ when those devices are used. Additionally, the same study investigator performed the ventilation for all subjects, potentially artificially standardizing ventilation pauses. However, the duration of time spent in ventilation pauses varied widely between subjects and was highly correlated with CC/min, suggesting that the subjects (rather than the investigator) controlled the length of time allocated to ventilation. Lastly, it is difficult to know how accurately simulated performance reflect performance on a human neonate. However, a study investigating the effect of using a modified “physiological” manikin for infant CPR found similar rates of chest compressions performed between the standard and “physiological” manikin [17].
Conclusions
NRP trained providers often deviate from NRP recommendations regarding delivery of coordinated chest compressions and ventilations in a simulated setting. Most providers who do not conform to NRP recommendations perform more CC/min than recommended. Duration of ventilation pauses is highly correlated with CC/min. Future studies should investigate the effect of real time feedback on NRP providers' performance of coordinated chest compressions.
Acknowledgments
We thank Dr. Robert Sutton for his advice in the preparation of this manuscript.
Funding: E. Foglia is supported by an NIH training grant: 5T32HD060550-03.D. Niles and V. Nadkarni receive grant support from Laerdal Foundation for Acute Medicine. Laerdal Medical donated the study compression sensor. Laerdal Medical did not participate in the decision to publish this manuscript.
Footnotes
Conflicts of Interest: P.H. Aasland is an employee of Laerdal Medical. No other authors have existing conflicts of interest.
References
- 1.Perlman JM, Risser R. Cardiopulmonary resuscitation in the delivery room. Associated clinical events. Arch Pediatr Adolesc Med. 1995;149:20–25. doi: 10.1001/archpedi.1995.02170130022005. [DOI] [PubMed] [Google Scholar]
- 2.Wyckoff MH, Perlman JM, Laptook AR. Use of volume expansion during delivery room resuscitation in near-term and term infants. Pediatrics. 2005;115:950–955. doi: 10.1542/peds.2004-0913. [DOI] [PubMed] [Google Scholar]
- 3.Kramer-Johansen J, Edelson DP, Losert H, Köhler K, Abella BS. Uniform reporting of measured quality of cardiopulmonary resuscitation (CPR) Resuscitation. 2007;74:406–417. doi: 10.1016/j.resuscitation.2007.01.024. [DOI] [PubMed] [Google Scholar]
- 4.Abella BS, Sandbo N, Vassilatos P, Alvarado JP, O'Hearn N, et al. Chest compression rates during cardiopulmonary resuscitation are suboptimal: a prospective study during in-hospital cardiac arrest. Circulation. 2005;111:428–434. doi: 10.1161/01.CIR.0000153811.84257.59. [DOI] [PubMed] [Google Scholar]
- 5.Wik L, Kramer-Johansen J, Myklebust H, Sørebø H, Svensson L, et al. Quality of cardiopulmonary resuscitation during out-of-hospital cardiac arrest. JAMA. 2005;293:299–304. doi: 10.1001/jama.293.3.299. [DOI] [PubMed] [Google Scholar]
- 6.Abella BS, Alvarado JP, Myklebust H, Edelson DP, Barry A, et al. Quality of cardiopulmonary resuscitation during in-hospital cardiac arrest. JAMA. 2005;293:305–310. doi: 10.1001/jama.293.3.305. [DOI] [PubMed] [Google Scholar]
- 7.Sutton RM, Niles D, Nysaether J, Abella BS, Arbogast KB, et al. Quantitative analysis of CPR quality during in-hospital resuscitation of older children and adolescents. Pediatrics. 2009;124:494–499. doi: 10.1542/peds.2008-1930. [DOI] [PubMed] [Google Scholar]
- 8.Whyte SD, Sinha AK, Wyllie JP. Neonatal resuscitation--a practical assessment. Resuscitation. 1999;40:21–25. doi: 10.1016/s0300-9572(98)00143-9. [DOI] [PubMed] [Google Scholar]
- 9.Martin PS, Kemp AM, Theobald PS, Maguire SA, Jones MD. Do chest compressions during simulated infant CPR comply with international recommendations? Arch Dis Child. 2013;98:576–581. doi: 10.1136/archdischild-2012-302583. [DOI] [PubMed] [Google Scholar]
- 10.Kattwinkel J, Perlman JM, Aziz K, Colby C, Fairchild K, et al. Neonatal resuscitation: 2010 american heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Pediatrics. 2010;126:e1400–1413. doi: 10.1542/peds.2010-2972E. [DOI] [PubMed] [Google Scholar]
- 11.Christman C, Hemway RJ, Wyckoff MH, Perlman JM. The two-thumb is superior to the two-finger method for administering chest compressions in a manikin model of neonatal resuscitation. Arch Dis Child Fetal Neonatal Ed. 2011;96:F99–99. doi: 10.1136/adc.2009.180406. [DOI] [PubMed] [Google Scholar]
- 12.Hemway RJ, Christman C, Perlman J. The 3:1 is superior to a 15:2 ratio in a newborn manikin model in terms of quality of chest compressions and number of ventilations. Arch Dis Child Fetal Neonatal Ed. 2013;98:F42–45. doi: 10.1136/archdischild-2011-301334. [DOI] [PubMed] [Google Scholar]
- 13.Kern KB, Stickney RE, Gallison L, Smith RE. Metronome improves compression and ventilation rates during CPR on a manikin in a randomized trial. Resuscitation. 2010;81:206–210. doi: 10.1016/j.resuscitation.2009.10.015. [DOI] [PubMed] [Google Scholar]
- 14.Jäntti H, Silfvast T, Turpeinen A, Kiviniemi V, Uusaro A. Infuence of chest compression rate guidance on the quality of cardiopulmonary resuscitation performed on manikins. Resuscitation. 2009;80:453–457. doi: 10.1016/j.resuscitation.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 15.Oh JH, Lee SJ, Kim SE, Lee KJ, Choe JW, et al. Effects of audio tone guidance on performance of CPR in simulated cardiac arrest with an advanced airway. Resuscitation. 2008;79:273–277. doi: 10.1016/j.resuscitation.2008.06.022. [DOI] [PubMed] [Google Scholar]
- 16.Martin P, Theobald P, Kemp A, Maguire S, Maconochie I, et al. Realtime feedback can improve infant manikin cardiopulmonary resuscitation by up to 79%-A randomised controlled trial. Resuscitation. 2013;84:1125–1130. doi: 10.1016/j.resuscitation.2013.03.029. [DOI] [PubMed] [Google Scholar]
- 17.Martin PS, Kemp AM, Theobald PS, Maguire SA, Jones MD. Does a more “physiological” infant manikin design effect chest compression quality and create a potential for thoracic over-compression during simulated infant CPR? Resuscitation. 2013;84:666–671. doi: 10.1016/j.resuscitation.2012.10.005. [DOI] [PubMed] [Google Scholar]