Abstract
Objective:
Poor mental health, sleep problems, drinking motivations, and high-risk drinking are prevalent among college students. However, research designed to explicate the interrelationships among these health risk behaviors is lacking. This study was designed to assess the direct and indirect influences of poor mental health (a latent factor consisting of depression, anxiety, and stress) to alcohol use and alcohol-related consequences through the mediators of global sleep quality and drinking motives in a comprehensive model.
Method:
Participants were 1,044 heavy-drinking college students (66.3% female) who completed online surveys.
Results:
A hybrid structural equation model tested hypotheses involving relations leading from poor mental health to drinking motives and poorer global sleep quality to drinking outcomes. Results showed that poor mental health significantly predicted all four subscales of drinking motivations (social, coping, conformity, and enhancement) as well as poor sleep. Most of the drinking motives and poor sleep were found to explain alcohol use and negative alcohol consequences. Poor sleep predicted alcohol consequences, even after controlling for all other variables in the model. The hypothesized mediational pathways were examined with tests of indirect effects.
Conclusions:
This is the first study to assess concomitantly the relationships among three vital health-related domains (mental health, sleep behavior, and alcohol risk) in college students. Findings offer important implications for college personnel and interventionists interested in reducing alcohol risk by focusing on alleviating mental health problems and poor sleep quality.
Incidence of poor mental health among U.S. undergraduates is a growing concern on college campuses. In a recent nationally representative survey of nearly 100,000 college students, 64.7% felt overwhelmed, 62.2% felt exhausted, and 28.5% reported extreme anxiety within the past year (American College Health Association, 2010). In other multisite surveys of college students, 85% reported experiencing significant daily stress (MtvU and the Associated Press, 2008), and nearly one third of students reported feeling depressed enough that daily functions within the past year were impaired (American College Health Association, 2011). Students suffering from mental distress may have difficulty coping with the academic and social demands of college and thus may be at heightened risk for unhealthy behaviors. A substantial body of research demonstrates that poor mental health is a strong indicator of alcohol risks (e.g., Miller et al., 2002; O’Hare and Sherrer, 2000) and sleep problems (e.g., Brooks et al., 2009; Uhde et al., 2009). An understanding of how these three fundamental factors relate to one another may yield important information for novel approaches in designing prevention programs and enhancing services on college campuses.
Mental health and alcohol use
A nationally representative study documented that 80.7% of college students consumed alcohol in the past year and, of these, more than half (55.5%) engaged in heavy episodic drinking (four/five or more drinks in a row for women/men; Wechsler et al., 2002). Heavy episodic drinkers account for the vast majority of overall alcohol consumption on college campuses (e.g., Wechsler et al., 2002) and face heightened risk for a number of serious physical, academic, legal, and sexual consequences (Hingson et al., 2005, 2009). Alcoholrelated consequences are especially pronounced among students with mental health problems (Dawson et al., 2005; Weitzman, 2004). Even at comparable levels of drinking, college students with poor mental health are consistently shown to experience significantly more alcohol-related problems than peers with strong mental health (e.g., Camatta and Nagoshi, 1995; Dennhardt and Murphy, 2011; LaBrie et al., 2010b). Moreover, the robust direct link between poor mental health and alcohol problems has even been statistically maintained over and above a range of predictors, including alcohol consumption, demographics (e.g., age, sex, and race), and personality (e.g., irrational beliefs and impulsivity) (Camatta and Nagoshi, 1995; Weitzman, 2004).
Findings linking poor mental health to alcohol consumption, however, are mixed. Some studies report no significant relationship (Dennhardt and Murphy, 2011; Geisner et al., 2004; Ham and Hope, 2005; Oliver et al., 1998), whereas others link poor mental health—including depression (Pedrelli et al., 2011; Weitzman, 2004), anxiety (Cranford et al., 2009; Terlecki et al., 2011), and stress (Park et al., 2004; Rice and Van Arsdale, 2010)—to greater consumption. It is clear that investigations are needed to examine how poor mental health relates to both alcohol consumption and consequences as well as the extent to which consumption may mediate the link between mental health and consequences. Furthermore, studies focusing on heavy episodic drinkers, the subgroup most at risk for experiencing adverse drinking outcomes, may help to illuminate these relationships and advance harm-reduction efforts.
Mental health and drinking motives on alcohol outcomes
Students with poor mental health, relative to peers with strong mental health, tend to endorse stronger motivations for drinking (e.g., Cooper et al., 1995; Stewart et al., 2001; Thornton et al., 2012). Specifically, evidence supports that students with poor mental health usually drink to reduce or regulate negative internal (coping motives) or external (conformity motives) states (McNally et al., 2003; O’Hare and Shen, 2012; Stewart et al., 2001; Windle and Windle, 2012). In a review of 82 studies examining drinking motives (social, enhancement, and coping) among adolescents and young adults, Kuntsche et al. (2005) found that poor mental health (e.g., high levels of anxiety sensitivity, depression, and negative self-views) was associated with coping motives toward drinking. Among students with anxiety symptomatology, both coping and conformity motives appear to be most strongly endorsed (Lewis et al., 2008; Stewart et al., 2001).
Overall, drinking motives are positively related to alcohol consumption and consequences (e.g., Kuntsche et al., 2007; Westmaas et al., 2007) and mediate the link between mental health and alcohol outcomes (Goldsmith et al., 2009; Tragesser et al., 2007). However, distinct motivations for drinking are associated with unique drinking behaviors and risk for alcoholrelated problems. Socially based motives (e.g., to celebrate a special occasion with friends) are considered most normative and unrelated to problematic drinking (Cooper, 1994; Cooper et al., 1992; Kuntsche et al., 2006; Merrill and Read, 2010). Enhancement motives (e.g., for fun or excitement) are found to predict alcohol-related consequences, but only indirectly through heavy levels of drinking (Cooper et al., 1992; Merrill and Read, 2010; for review, see Kuntsche et al., 2006). The negative reinforcing motives of coping and conformity drinking remain strong predictors of alcohol-related consequences, over and above drinking levels (Cooper, 1994; Kassel et al., 2000; Lewis et al., 2008). Given the important role of different types of drinking motives in the connection between mental health and drinking outcomes, it is important to examine drinking motivations as mediators of this relationship.
Mental health and sleep
Sixty percent of college students are classified as “poor-quality” sleepers (Lund et al., 2010), with half experiencing lack of sleep or irregular sleep patterns (Buboltz et al., 2006; Tsai and Li, 2004) and 27% meeting the minimum threshold to be classified with at least one sleep disorder (e.g., insomnia and sleep apnea; Gaultney, 2010). These rates of inadequate and problematic sleep are on the rise among young adults (Hicks et al., 2001; Wolfson, 2010). Furthermore, adolescents and young adults may be especially prone to both mental health and sleep problems (Chorney et al., 2008; Ehlers et al., 2010; Hicks and Garcia, 1987). In fact, disturbances in sleep and self-reported sleep dissatisfaction represent core symptoms of depression (Brooks et al., 2009; Mayers et al., 2009; Moo-Estrella et al., 2005; Riemann et al., 2001). Anxiety is also strongly related to poorer sleep quality (e.g., Mayers et al., 2009; Uhde et al., 2009): The prevalence of insomnia in patients with anxiety disorders ranges from 70% to 90% (Maher et al., 2006). Moreover, longitudinal and experimental research has supported the prognostic importance of depression (Brooks et al., 2009; Patten et al., 2000; Szklo-Coxe et al., 2007), anxiety (Kennedy et al., 1991; for review, see Ware and Morin, 1997), and stress (Gross and Borkovec, 1982; Hicks and Garcia, 1987) on negative sleep outcomes. In people with comorbid anxiety and insomnia, for example, poor mental health preceded the onset of the insomnia in 73% of cases (Johnson et al., 2006). To account for these co-existing risk factors, the current study evaluated mental health as a predictor of sleep problems.
Sleep and alcohol outcomes
Poor sleep is associated with alcohol misuse and problems among adolescents (Johnson and Breslau, 2001; Pieters et al., 2010; Tynjälä et al., 1997) and college students (Kenney et al., 2012). Furthermore, sleep problems have prospectively predicted alcohol misuse in community samples (e.g., Weissman et al., 1997), relapse among alcoholics (e.g., Brower et al., 1998, 2001), and alcohol use among adolescents (sleep problems at age 3–5 years predicted early onset of alcohol use at age 12–14 years; Wong et al., 2004), over and above psychiatric problems. In laboratory studies, sleep-restricted and sleep-deprived participants consistently exhibit diminished attention, increased risk-taking behaviors, and impairment of motor response (e.g., simulated driving and computerized tasks) from alcohol intake relative to control participants (Roehrs and Roth, 1998; Roehrs et al., 1994).
The well-documented predictive influence of poor sleep on alcohol-related risk may be explained, in part, by neurocognitive functioning. Sleep deprivation is found to significantly reduce neural activity in the prefrontal cortex region of the brain, an area essential for higher order executive functioning such as decision-making, self-monitoring, and conflict resolution (Thomas et al., 2000, 2003). In several studies, sleep deprivation has been shown to impair executive functioning, including problem-solving, inhibitory functioning, and divergent thinking capacity (Linde and Bergstrom, 1992; Nilsson et al., 2005; Wimmer et al., 1992). Particularly in high-risk college drinking contexts, poor sleep may thus deprive students of important physical and cognitive capacities that are needed to evade potential harms and to make rational and informed decisions. More recently, poor sleep quality has been linked to increased endorsement of drinking motives (Digdon and Landry, 2013). In the current study, we sought to gain a better understanding of the role of sleep quality in the relationship between mental health and alcohol risk while also assessing drinking motives, a well-established predictor of alcohol risk and known correlate of both mental health and sleep quality.
Current study aims and hypotheses
Previous work has called for in-depth examination of factors in the college environment that may interact with mental health vulnerabilities to increase health risks (Hunt and Eisenberg, 2010). The goal of the current study was to extend the understanding of co-occurring mental health, sleep, and alcohol problems by proposing and testing a model to examine the interrelationship of these risk factors in a large collegiate sample. Moreover, social, enhancement, coping, and conformity motives were assessed as mediators of the relationship between mental health and alcohol outcomes. The current sample of heavy-drinking college students is relevant given the relatively high prevalence of mental health, sleep problems, and alcohol problems during the period of college. Assessing the risk factors within one integrative model provides important insights into the unique direct and indirect influences of poor mental health (depression, anxiety, and stress) on drinking motives, global sleep quality, alcohol use, and alcohol consequences, over and above all other predictors.
Combining these variables into a collective model, we hypothesized that poor mental health would independently predict greater endorsement of poor sleep quality as well as each of the drinking motives. Among the drinking motives, however, we expected that poor mental health would most strongly predict negatively reinforcing coping and conformity motives. In turn, we expected that most of the four drinking motives would predict alcohol use and negative consequences. Anchored in previous research, enhancement motives were hypothesized to predict alcohol use (Cooper et al., 1992; Kuntsche et al., 2006; Merrill and Read, 2010), and coping and conformity motives were expected to be strong predictors of alcohol consequences (Cooper, 1994; Lewis et al., 2008).
Method
Participants
In the fall of 2010, 6,000 undergraduate students from two West Coast universities were recruited to participate in a larger intervention study. One university was a large, public university with a total enrollment of approximately 30,000, whereas the other was a midsized, private university with approximately 5,600 undergraduate students. Of the 6,000 (3,000 per campus) students invited, 2,689 students (44.8%) completed a brief initial screening survey, and participants who reported engaging in at least one heavy episodic drinking occasion in the past month (n = 1,493; 55.5%) were invited to complete the main survey. Of those invited, 1,367 students (91.6%) completed the baseline survey and received a nominal stipend for participation.
The final sample included 1,044 participants—558 (53.4%) from the first campus and 486 (46.6%) from the second campus—who completed all measures used in the current study. This sample was 66.3% female and reported a mean age of 20.13 years (SD = 1.36). The majority of participants were White (64.7%), and the remaining were Asian (12.9%), Black (2.4%), Hawaiian/Pacific Islander (2.0%), multiracial (11.3%), and other (6.7%). Also, 12.4% reported their ethnicity as Hispanic. With respect to class year, 14.4% were first-year students, 20.3% were sophomores, 25.8% were juniors, and 39.5% were seniors.
Procedures
Students were invited via postal mail and email to participate in a study that involved web-based surveys. Invitations contained the web address to the online survey and a unique participant identification number that students entered to gain access to the survey. When clicking on the web page, they were directed to the screening survey, with eligible participants immediately routed to the main survey.
Measures
Mental health.
The Depression Anxiety Stress Scale (DASS-21; Lovibond and Lovibond, 1995) is a 21-item questionnaire used to measure different mental health symptoms as represented in its three subscales (7 items each) of depression (e.g., “I felt that life was meaningless”), anxiety (e.g., “I felt I was close to panic”), and stress (e.g., “I tended to overreact to situations”). The DASS-21, which assessed symptoms experienced in the past week, did not assess sleeping behaviors, thus avoiding conceptual overlap with the sleep quality scale. Response options ranged from 0 (did not apply to me at all) to 3 (applied to me very much), and items were summed within each subscale to form depression (α = .85), anxiety (α = .77), and stress (α = .84) composites. Higher scores represented poorer mental health on their respective dimensions. Studies have demonstrated the validity and internal consistency of the DASS-21 in clinical and nonclinical samples (Antony et al., 1998; Henry and Crawford, 2005).
Drinking motives.
Motivations for drinking alcohol were assessed using the 20-item Drinking Motives Questionnaire (Cooper, 1994), a well-validated measure of drinking motives (MacLean and Lecci, 2000; Stewart et al., 2001). Respondents were prompted with, “Thinking of the times you drank in the past 30 days, how often would you say that you drank for the following reasons?” Each reason includes five response options: 1 (almost never/never) to 5 (almost always/always), with five items summed to create each of the following four subscales—social (α = .89; e.g., “Because it helps you enjoy a party”), coping (α = .88; e.g., “To forget your worries”), enhancement (α = .88; e.g., “Because you like the feeling”), and conformity (α = .91; “Because your friends pressure you to drink”).
Global sleep quality.
This variable was assessed using the 19-item Pittsburgh Sleep Quality Index (PSQI; Buysse et al., 1989). Items assess past-month sleep habits, including average bed and rise times, hours slept per night, trouble sleeping (e.g., felt too cold/hot or had bad dreams), use of sleeping medications, and daytime drowsiness. The scores were summed to calculate the final global measure score ranging from 0 to 21 (α = .68). Higher cumulative scores indicate poorer global sleep quality (Buysse et al., 1989; Fichtenberg et al., 2001). The PSQI has demonstrated good test–retest reliability (Backhaus et al., 2002; Buysse et al., 1989) and criterion validity (Backhaus et al., 2002; Fichtenberg et al., 2001; Grandner et al., 2006).
Alcohol use.
The Daily Drinking Questionnaire (Collins et al., 1985) was used to assess the number of drinks participants consumed in a typical week in the past month. For each day of the week (e.g., Monday), participants indicated, using open-ended responses, the typical number of drinks they consumed on a given day (e.g., “On a typical Monday, I have X drinks”). These seven items, corresponding to the days of the week, were summed to yield an index of total drinks per week. The Daily Drinking Questionnaire has demonstrated good test–retest validity (Neighbors et al., 2006) and criterion validity (Neighbors et al., 2004).
Negative alcohol-related consequences.
Negative alcohol-related consequences were measured with a modified Rutgers Alcohol Problem Index (White and Labouvie, 1989). Participants were asked if they had experienced each of 23 specific consequences while drinking or because of alcohol use (e.g., “Had a fight, argument, or bad feelings with a friend”) in the past 3 months. To reduce skewness levels of these items, responses were binary coded to indicate whether respondents had experienced each consequence (1 = once or more, 0 = never; Palmer et al., 2010). Dichotomous scoring of this scale has been shown to be reliable and valid in identifying alcohol-related problems among college students (Martens et al., 2007b). Summing the number of these specific types of problems induced by the use of alcohol yielded an index of consequences, with a range of 0–23 (α = .86).
Results
Analytic plan
Using the EQS 6.2 program (Bentler, 2001), a hybrid structural equation model involving predictive relations consisting of a latent factor and measured variables was estimated (Crano and Lac, 2012). The hypothesized model was specified as follows: Poor mental health served as a latent factor represented by the indicators of depression, anxiety, and stress. Poor mental health was then allowed to explain each of the four subscales of drinking motives (social, coping, conformity, and enhancement) as well as global sleep quality. Each of the subscales of drinking motives and global sleep quality were simultaneously set to predict both alcohol use and consequences. Alcohol use was also permitted to account for alcohol consequences.
As measured variables somewhat departed from normality, this artifact was corrected with the robust adjustment for fit indices using a command available in the software (Bentler, 2001). The correction is the recommended approach to account for any departures from multivariate normality in structural equation modeling (Bentler and Dijkstra, 1985; Satorra and Bentler, 1994, 2001). Four of these robust fit indices were used to evaluate model fit. The preference is for a nonsignificant chi-square test, but the test is overly sensitive in rejecting a correct model if the sample size is large (Bollen, 1989; Kline, 1998). Also evaluated were two relative fit indices, including the comparative fit index (CFI) and the non-normed fit index (NNFI), both of which range from about 0.00 to 1.00, with a higher value indicative of a better fit (Ullman and Bentler, 2003). Also used to appraise the model was a residual-based index, the root mean square error of approximation (RMSEA), considered useful for detecting problems attributable to model misspecifications, with a value greater than .10 indicative of poor fit (Browne and Cudeck, 1993; MacCallum et al., 1996).
Descriptive information
According to the PSQI scoring rubric and classification system (Buysse et al., 1989), the majority of participants (54.3%) experienced poor global sleep quality. Furthermore, based on the established scoring criteria of the DASS-21, approximately half of the sample (49.5%) experienced some form of mental distress (i.e., nonnormal levels of depression, anxiety, or stress; Lovibond and Lovibond, 1995). Rates of poor sleep quality were higher for participants with some form of mental distress (58.6% vs. 32.2% for those without mental distress). Depressed mood was reported by 34.6% of participants. Also, 31.4% and 30.1% of participants reported some form of anxiety and nonnormal levels of stress, respectively. Means, standard deviations, and correlations of the measured variables are shown in Table 1.
Table 1.
Correlation matrix of variables
| M | SD | 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | |
| 1. Depression | 8.67 | 8.93 | – | – | – | – | – | – | – | – | – | – |
| 2. Anxiety | 6.14 | 7.17 | .65 | – | – | – | – | – | – | – | – | – |
| 3. Stress | 11.57 | 8.88 | .66 | .68 | – | – | – | – | – | – | – | – |
| 4. Social motives | 18.12 | 4.71 | .09 | .11 | .07 | – | – | – | – | – | – | – |
| 5. Coping motives | 9.34 | 4.46 | .35 | .30 | .24 | .34 | – | – | – | – | – | – |
| 6. Conformity motives | 7.43 | 3.66 | .18 | .18 | .15 | .19 | .39 | – | – | – | – | – |
| 7. Enhancement motives | 15.67 | 5.02 | .06 | .08 | .08 | .58 | .31 | .15 | – | – | – | – |
| 8. Poor global sleep quality | 6.22 | 3.32 | .34 | .31 | .35 | .07 | .19 | .09 | .08 | – | – | – |
| 9. Alcohol use | 10.97 | 9.65 | .02 | .08 | -.04 | .24 | .13 | .04 | .29 | .10 | – | – |
| 10. Negative alcohol consequences | 4.62 | 4.37 | .27 | .26 | .23 | .20 | .32 | .25 | .26 | .29 | .41 | – |
Notes: Correlations ≥ .06 are significant at p < .05; correlations ≥ .09 are significant at p < .01; correlations ≥ .11 are significant at p < .001.
Predictive model
The hypothesized model produced acceptable fit indices overall, χ2(20) = 76.20, p < .001 (CFI = .97; NNFI = .94; RMSEA = .052, 90% CI [.040, .064]). The multivariate Lagrange multiplier test (Bentler, 1990; Chou and Bentler, 1990) indicated that the model could be improved by incorporating the direct path from poor mental health to alcohol consequences. This inclusion was logically justified on the basis that those suffering from greater levels of mental distress are more susceptible to the problematic consequences stemming from inebriation (e.g., Camatta and Nagoshi, 1995; Dennhardt and Murphy, 2011; LaBrie et al., 2010b). The test also found that poor mental health was not directly predictive of alcohol use (β = -.06, n.s.).
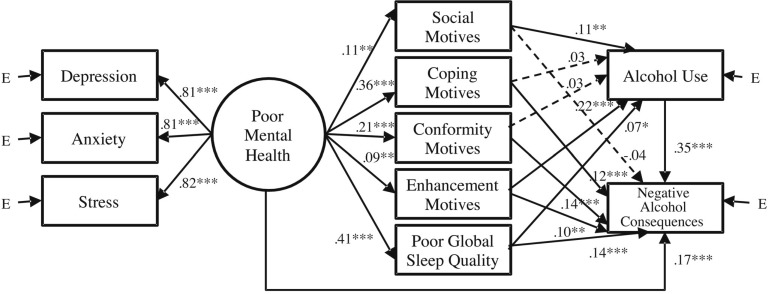
After we incorporated this single path, the model was re-estimated, as shown in Figure 1. This final model exhibited strong fit indices, χ2 (19) = 54.52, p < .001 (CFI = .98; NNFI = .96; RMSEA = .042, 90% CI [.029, .056]). Because the initial and final models were nested structures, a scaled chi-square difference test was performed (Ullman, 2006), which corroborated that the final model yielded a significant improvement in fit (p < .001). The factor loadings of depression, anxiety, and stress were strong in representing the latent factor of poor mental health. Poor mental health significantly contributed to higher levels of social motives, coping motives, conformity motives, enhancement motives, and poor sleep quality. Social motives, enhancement motives, and poor sleep quality concurrently and significantly predicted greater levels of alcohol use. Poor mental health, coping motives, conformity motives, enhancement motives, and poor sleep quality simultaneously predicted negative alcohol consequences. The variables accounted for 9.6% of the variance in alcohol use and 32.8% of the variance in negative alcohol consequences.
Figure 1.
Final model of poor mental health to alcohol consequences. Standardized coefficients are presented. E = error. Error terms arising from prediction of the four motives were estimated, and these four errors were allowed to be correlated with each other. *p < .05; **p < .01; ***p < .001.
Tests of indirect effects were conducted to examine the tenability of mediational processes depicted in Figure 1. As recommended by MacKinnon et al. (2007), bootstrapping was used to obtain more accurate estimates of indirect effects and standard errors (Fan, 2003). A significant indirect effect was evidenced from poor mental health (B = 0.48, 95% CI [0.27, 0.69], β = .12, p < .001) through all the model mediators to alcohol consequences. Results showed a significant indirect effect from mental health (B = 0.96, 95% CI [0.47, 1.45], β = .11, p < .001) through the mediators to total drinks. Significant indirect effects were also found from social motives (B = 0.04, 95% CI [0.01, 0.08], β = .05, p < .01), enhancement motives (B = 0.07, 95% CI [0.04, 0.11], β = .09, p < .001), and sleep quality (B = 0.05, 95% CI [0.01, 0.09], β = .03, p < .05) through the mediator of alcohol use to alcohol consequences.
Discussion
In this study, and consistent with hypotheses, poor mental health was directly and positively predictive of drinking motives, poor sleep quality, and alcohol consequences. Poor mental health, however, was not found to be directly related to alcohol use in the model. The results in the model provide important insight into the interplay between three vital health-related domains—mental health, sleep behavior, and alcohol risk—while accounting for drinking motives in heavy-drinking college students.
Mediating effects of sleep quality and drinking motives
Previous research has found that the relation between drinking quantity and alcohol-related negative consequences in college students rarely exceeds a correlation of .60 (La-Brie et al., 2010a; Larimer et al., 2001; Turner et al., 2000). The current sample found a significant correlation of .41. These findings suggest that a substantial proportion of the experience of alcohol problems is insufficiently explained by drinking levels alone. The present study was conducted under the premise that students suffering from poor sleep may be susceptible to excessive drinking as well as problems over and above drinking. This relationship may be further exacerbated in students experiencing poor mental health who are already at heightened risk for experiencing negative alcohol consequences (Dawson et al., 2005; Weitzman, 2004). Moreover, we assessed four types of drinking motives, potential mediators of the relationship between poor mental health and alcohol risk.
Indeed, findings revealed problematic rates of poor mental health along with its direct effect on drinking motives, sleep, and alcohol consequences. Research indicates that poor sleep quality may increase alcohol risk via maladaptive coping capacities, such as using alcohol to self-medicate (Digdon and Landry, 2013; Taylor and Bramoweth, 2010). It is notable then that in this study, poor sleep quality remained significantly predictive of alcohol consequences, even after statistically controlling for both mental health and drinking motivations. Adverse effects stemming from poor-quality sleep (e.g., impaired decision-making and inhibitory functioning) may account for the link between poor sleep and consequences and present a worthwhile avenue for future studies. As expected, enhancement motives were predictive of alcohol use, and coping and conformity motives predicted alcohol-related consequences. Unexpectedly, enhancement motives also predicted consequences over and above drinking.
Mental health
High rates of co-occurring mental health and sleep problems that emerged for participants in our study are consistent with prior research (e.g., Brooks et al., 2009; Mayers et al. 2009; Moo-Estrella et al., 2005; Patten et al., 2000; Riemann et al., 2001). In the current study, sleep quality indirectly predicted alcohol consequences, such that poor mental health predicted poor sleep quality and poor sleep quality predicted alcohol-related consequences. First, this finding corroborates prospective research showing symptoms of poor mental health (e.g., self-criticalness or self-dislike, loss of interest, tiredness and fatigue, and negative thoughts) predictive of poorer sleep quality (Brooks et al., 2009; Johnson et al., 2006; Nelson and Harvey, 2003). Second, this study extends knowledge of this relationship by revealing the intermediate role of poor sleep quality in the link between poor mental health and the experience of alcohol consequences. Even after controlling for well-established predictors of alcohol risk (i.e., drinking motives) and drinking levels, poor sleep played an important role in the increased risk for consequences among those students experiencing psychological distress. An important finding was that poor mental health was not directly predictive of alcohol use in the model. These findings are consistent with previous research indicating no direct relationship between mental health and alcohol use among college students (Dennhardt and Murphy, 2011; Geisner et al., 2004; Ham and Hope, 2005; Oliver et al., 1998). Rather, poor mental health predicted poor sleep quality, which in turn predicted alcohol use. This finding may clarify our knowledge of how mental health is related to alcohol problems; it operates through motives, sleep quality, and alcohol consumption.
Sleep quality may be particularly important for students with poor mental health who, compared with peers, tend to lack protective social support networks (e.g., Delistamati et al., 2006; Pauley and Hesse, 2009) and the inherent ability to make safe decisions (e.g., Okwumabua et al., 2002). Among students already susceptible to alcohol use, inadequate sleep may further weaken their cognitive capacity to make safer drinking-related decisions or use self-protective behaviors, irrespective of consumption levels.
Implications
Greater attention and resources directed toward harmreduction efforts targeting students with poor mental health would be beneficial. Addressing students’ misperceptions that drinking can effectively resolve negative internal states or substitute for adaptive social functioning may help reduce expectancies and motives that increase the risk associated with drinking. Furthermore, teaching students alternative coping skills or harm-reduction skills to use in drinking contexts may be helpful. Protective behavioral strategies (e.g., drink only with close friends; Martens et al., 2005) or drinking control behaviors (e.g., practicing ways to be more comfortable in social settings without using alcohol; Sugarman and Carey, 2007) may be especially effective at reducing alcohol-related risk encountered by students with poor mental health. Protective behavioral strategies are shown to partially mediate the relationship between depressive symptoms and alcohol consequences, indicating that students with high levels of depression are less likely to use protective behavioral strategies and thus more likely to experience negative alcohol consequences (Martens et al., 2008). Yet students with poorer mental health are found to garner considerable benefit (i.e., lower levels of risky drinking and consequences) when they do implement protective behavioral strategies (LaBrie et al., 2009, 2010b). Thus, training students to use protective behavioral strategies could potentially attenuate the relationship between mental health deficiencies and alcohol consequences observed in the current study.
In addition, therapists, physicians, and other professional college staff should consider educating students about the risks associated with insufficient sleep and teach students how to improve sleep patterns (e.g., developing a sleep routine; exercising regularly; and avoiding caffeine, tobacco, or alcohol before bedtime). Identifying students at risk for mental health problems and sleep problems would help guide the design of tailored interventions. Previous research has found that implementing a screening and brief alcohol intervention program for high-risk drinkers in both university health and counseling centers was efficacious in reducing risky drinking (Martens et al., 2007a). Such contexts represent ideal platforms to begin targeting at-risk students while also leveraging the skills of staff equipped to implement brief interventions.
Limitations and future directions
The current study is limited in several ways. First, it is cross-sectional. Thus, despite evidence supporting the hypothesized directionality of processes, the nonexperimental design does not allow for unequivocal conclusions regarding cause-and-effect relationships. Prospective studies that assess mental health and subsequent sleep patterns and alcohol behaviors over time are needed. In addition, event-level methods that simultaneously account for students’ sleep and alcohol use behaviors in a given period (e.g., 1 week) may be helpful for future longitudinal research. Moreover, although the focus on heavy-drinking college students is pertinent in light of the high prevalence rates of mental health deficiencies, poor sleep quality, and risky drinking behaviors in this population, this demographic focus also limits the generalizability of the current findings. Researchers are encouraged to test similar hypotheses in the general adult population, in which the intersection of these various risky behavioral patterns may have been ongoing for longer periods and hence may demonstrate different interrelationships and implications.
With respect to measurement limitations, some of the assessment time frames of the questions were inconsistent. The time frames were chosen in accordance with their uses in previous literature (i.e., capturing mood and mental health of the past week, accurately recalling sleeping habits of the past month, and noting alcohol use patterns of a typical week in the past month) and sensitivity in reporting (i.e., to capture more severe alcohol consequences that occur less frequently, such as memory loss because of drinking, alcohol consequences were measured over the past 3 months). Furthermore, these measures tend to remain relatively stable over short periods. From an analytical perspective, the study focused on testing relations among variables and not on mean differences; therefore, results were less likely to be affected by increases in the average scores on measures if a longer time frame was used instead. Also concerning measurement issues, these analyses used an established measure of mental health in which the subscales of depression, anxiety, and stress were combined into a latent factor of mental health. Although we feel this operationalization was appropriate given that these subscales were found to be highly correlated, future studies that explore the distinct subscales of depression, anxiety, and stress are recommended.
Conclusions
This is the first study to examine concurrently the influence of poor mental health on sleep quality as well as both drinking and alcohol consequences in a comprehensive model. Moreover, we included a measure of drinking motives, a well-established correlate of both poor mental health and alcohol outcomes. Results documented high rates of mental distress, poor global sleep quality, and co-occurring mental health–sleep–alcohol problems in this large sample of heavy-drinking college students. Findings advance the understanding of the interrelationships among these prevalent and risky behaviors to facilitate prevention initiatives aimed at helping students vulnerable to multiple health risks.
Footnotes
This research was supported by National Institute on Alcohol Abuse and Alcoholism Grant R01 AA 012547-06A2 and by a grant from the Alcoholic Beverage Medical Research Foundation (ABMRF)/The Foundation for Alcohol Research.
References
- American College Health Association. American College Health Association–National college health assessment II: Reference group data report spring 2009 (abridged) Linthicum, MD: Author; 2010. [Google Scholar]
- American College Health Association. American College Health Association–National college health assessment II: Reference group executive summary spring 2011. Hanover, MD: Author; 2011. Retrieved from http://www.acha-ncha.org/docs/ACHA-NCHA-II_ReferenceGroup_ExecutiveSummary_ Spring2011.pdf. [Google Scholar]
- Antony MM, Bieling PJ, Cox BJ, Enns MW, Swinson RP. Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales in clinical groups and a community sample. Psychological Assessment. 1998;10:176–181. [Google Scholar]
- Backhaus J, Junghanns K, Broocks A, Riemann D, Hohagen F. Test-retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. Journal of Psychosomatic Research. 2002;53:737–740. doi: 10.1016/s0022-3999(02)00330-6. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Fit indexes, Lagrange multipliers, constraint changes and incomplete data in structural models. Multivariate Behavioral Research. 1990;25:163–172. doi: 10.1207/s15327906mbr2502_3. [DOI] [PubMed] [Google Scholar]
- Bentler PM. EQS 6 structural equations program manual. Encino, CA: Multivariate Software. 2001 [Google Scholar]
- Bentler PM, Dijkstra T. Efficient estimation via linearization in structural models. In: Krishnaiah PR, editor. Multivariate analysis 6. Amsterdam, The Netherlands: North-Holland; 1985. pp. 9–42. [Google Scholar]
- Bollen KA. New York, NY: Wiley; 1989. Structural equations with latent variables. [Google Scholar]
- Brooks PR, Girgenti AA, Mills MJ. Sleep patterns and symptoms of depression in college students. College Student Journal. 2009;43:464–473. [Google Scholar]
- Brower KJ, Aldrich MS, Hall JM. Polysomnographic and subjective sleep predictors of alcoholic relapse. Alcoholism: Clinical and Experimental Research. 1998;22:1864–1871. [PubMed] [Google Scholar]
- Brower KJ, Aldrich MS, Robinson EAR, Zucker RA, Greden JF. Insomnia, self-medication, and relapse to alcoholism. American Journal of Psychiatry. 2001;158:399–404. doi: 10.1176/appi.ajp.158.3.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Newbury Park, CA: Sage; 1993. pp. 445–455. [Google Scholar]
- Buboltz WC, Loveland J, Jenkins SM, Brown F, Soper B, Hodges J. College student sleep: Relationship to health and academic performance. In: Landaw MV, editor. College students: Mental health and coping strategies. Hauppauge, NY: Nova Science; 2006. pp. 1–39. [Google Scholar]
- Buysse DJ, Reynolds CF, III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Camatta CD, Nagoshi CT. Stress, depression, irrational beliefs, and alcohol use and problems in a college student sample. Alcoholism: Clinical and Experimental Research. 1995;19:142–146. doi: 10.1111/j.1530-0277.1995.tb01482.x. [DOI] [PubMed] [Google Scholar]
- Chorney DB, Detweiler MF, Morris TL, Kuhn BR. The interplay of sleep disturbance, anxiety, and depression in children. Journal of Pediatric Psychology. 2008;33:339–348. doi: 10.1093/jpepsy/jsm105. [DOI] [PubMed] [Google Scholar]
- Chou C-P, Bentler PM. Model modification in covariance structure modeling: A comparison among likelihood ratio, Lagrange multiplier, and Wald tests. Multivariate Behavioral Research. 1990;25:115–136. doi: 10.1207/s15327906mbr2501_13. [DOI] [PubMed] [Google Scholar]
- Collins RL, Parks GA, Marlatt GA. Social determinants of alcohol consumption: The effects of social interaction and model status on the self-administration of alcohol. Journal of Consulting and Clinical Psychology. 1985;53:189–200. doi: 10.1037//0022-006x.53.2.189. [DOI] [PubMed] [Google Scholar]
- Cooper ML. Motivations for alcohol use among adolescents: Development and validation of a four-factor model. Psychological Assessment. 1994;6:117–128. [Google Scholar]
- Cooper ML, Frone MR, Russell M, Mudar P. Drinking to regulate positive and negative emotions: A motivational model of alcohol use. Journal of Personality and Social Psychology. 1995;69:990–1005. doi: 10.1037//0022-3514.69.5.990. [DOI] [PubMed] [Google Scholar]
- Cooper ML, Russell M, Skinner JB, Windle M. Development and validation of a three-dimensional measure of drinking motives. Psychological Assessment. 1992;4:123–132. [Google Scholar]
- Cranford JA, Eisenberg D, Serras AM. Substance use behaviors, mental health problems, and use of mental health services in a probability sample of college students. Addictive Behaviors. 2009;34:134–145. doi: 10.1016/j.addbeh.2008.09.004. [DOI] [PubMed] [Google Scholar]
- Crano WD, Lac A. The evolution of research methodologies in social psychology: A historical analysis (pp. 159–174. In: Kruglanski AW, Stroebe W, editors. Handbook of the history of social psychology. New York, NY: Psychology Press; 2012. [Google Scholar]
- Dawson DA, Grant BF, Stinson FS. The AUDIT-C: Screening for alcohol use disorders and risk drinking in the presence of other psychiatric disorders. Comprehensive Psychiatry. 2005;46:405–416. doi: 10.1016/j.comppsych.2005.01.006. [DOI] [PubMed] [Google Scholar]
- Delistamati E, Samakouri MA, Davis EA, Vorvolakos T, Xenitidis K, Livaditis M. Interpersonal Support Evaluation List (ISEL)—college version: Validation and application in a Greek sample. International Journal of Social Psychiatry. 2006;52:552–560. doi: 10.1177/0020764006074184. [DOI] [PubMed] [Google Scholar]
- Dennhardt AA, Murphy JG. Associations between depression, distress tolerance, delay discounting, and alcohol-related problems in European American and African American college students. Psychology of Addictive Behaviors. 2011;25:595–604. doi: 10.1037/a0025807. [DOI] [PubMed] [Google Scholar]
- Digdon N, Landry K. University students’ motives for drinking alcohol are related to evening preference, poor sleep, and ways of coping with stress. Biological Rhythm Research. 2013;44:1–11. [Google Scholar]
- Ehlers CL, Gilder DA, Criado JR, Caetano R. Sleep quality and alcohol-use disorders in a select population of young-adult Mexican Americans. Journal of Studies on Alcohol and Drugs. 2010;71:879–884. doi: 10.15288/jsad.2010.71.879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan X. Using commonly available software for bootstrapping in both substantive and measurement analyses. Educational and Psychological Measurement. 2003;63:24–50. [Google Scholar]
- Fichtenberg NL, Putnam SH, Mann NR, Zafonte RD, Millard AE. Insomnia screening in postacute traumatic brain injury: Utility and validity of the Pittsburgh Sleep Quality Index. American Journal of Physical Medicine & Rehabilitation. 2001;80:339–345. doi: 10.1097/00002060-200105000-00003. [DOI] [PubMed] [Google Scholar]
- Gaultney JF. The prevalence of sleep disorders in college students: Impact on academic performance. Journal of American College Health. 2010;59:91–97. doi: 10.1080/07448481.2010.483708. [DOI] [PubMed] [Google Scholar]
- Geisner IM, Larimer ME, Neighbors C. The relationship among alcohol use, related problems, and symptoms of psychological distress: Gender as a moderator in a college sample. Addictive Behaviors. 2004;29:843–848. doi: 10.1016/j.addbeh.2004.02.024. [DOI] [PubMed] [Google Scholar]
- Goldsmith AA, Tran GQ, Smith JP, Howe SR. Alcohol expectancies and drinking motives in college drinkers: Mediating effects on the relationship between generalized anxiety and heavy drinking in negative-affect situations. Addictive Behaviors. 2009;34:505–513. doi: 10.1016/j.addbeh.2009.01.003. [DOI] [PubMed] [Google Scholar]
- Grandner MA, Kripke DF, Yoon I-Y, Youngstedt SD. Criterion validity of the Pittsburgh Sleep Quality Index: Investigation in a non-clinical sample. Sleep and Biological Rhythms. 2006;4:129–136. doi: 10.1111/j.1479-8425.2006.00207.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross RT, Borkovec TD. Effects of a cognitive intrusion manipulation on the sleep-onset latency of good sleepers. Behavior Therapy. 1982;13:112–116. [Google Scholar]
- Ham LS, Hope DA. Incorporating social anxiety into a model of college student problematic drinking. Addictive Behaviors. 2005;30:127–150. doi: 10.1016/j.addbeh.2004.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry JD, Crawford JR. The short-form version of the Depression Anxiety Stress Scales (DASS-21): Construct validity and normative data in a large non-clinical sample. British Journal of Clinical Psychology. 2005;44:227–239. doi: 10.1348/014466505X29657. [DOI] [PubMed] [Google Scholar]
- Hicks RA, Fernandez C, Pellegrini RJ. Striking changes in the sleep satisfaction of university students over the last two decades. Perceptual and Motor Skills. 2001;93:660. doi: 10.2466/pms.2001.93.3.660. [DOI] [PubMed] [Google Scholar]
- Hicks RA, Garcia ER. Level of stress and sleep duration. Perceptual and Motor Skills. 1987;64:44–46. doi: 10.2466/pms.1987.64.1.44. [DOI] [PubMed] [Google Scholar]
- Hingson RW, Heeren T, Winter M, Wechsler H. Magnitude of alcohol-related mortality and morbidity among U.S. college students ages 18–24: Changes from 1998 to 2001. Annual Review of Public Health. 2005;26:259–279. doi: 10.1146/annurev.publhealth.26.021304.144652. [DOI] [PubMed] [Google Scholar]
- Hingson RW, Zha W, Weitzman ER. Magnitude of and trends in alcohol-related mortality and morbidity among US college students ages 18-24, 1998-2005. Journal of Studies on Alcohol and Drugs, Supplement. 2009;16:12–20. doi: 10.15288/jsads.2009.s16.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunt J, Eisenberg D. Mental health problems and help-seeking behavior among college students. Journal of Adolescent Health. 2010;46:3–10. doi: 10.1016/j.jadohealth.2009.08.008. [DOI] [PubMed] [Google Scholar]
- Johnson EO, Breslau N. Sleep problems and substance use in adolescence. Drug and Alcohol Dependence. 2001;64:1–7. doi: 10.1016/s0376-8716(00)00222-2. [DOI] [PubMed] [Google Scholar]
- Johnson EO, Roth T, Breslau N. The association of insomnia with anxiety disorders and depression: Exploration of the direction of risk. Journal of Psychiatric Research. 2006;40:700–708. doi: 10.1016/j.jpsychires.2006.07.008. [DOI] [PubMed] [Google Scholar]
- Kassel JD, Jackson SI, Unrod M. Generalized expectancies for negative mood regulation and problem drinking among college students. Journal of Studies on Alcohol. 2000;61:332–340. doi: 10.15288/jsa.2000.61.332. [DOI] [PubMed] [Google Scholar]
- Kennedy GJ, Kelman HR, Thomas C. Persistence and remission of depressive symptoms in late life. American Journal of Psychiatry. 1991;148:174–178. doi: 10.1176/ajp.148.2.174. [DOI] [PubMed] [Google Scholar]
- Kenney SR, LaBrie JW, Hummer JF, Pham AT. Global sleep quality as a moderator of alcohol consumption and consequences in college students. Addictive Behaviors. 2012;37:507–512. doi: 10.1016/j.addbeh.2012.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB. New York, NY: Guilford Press; 1998. Principles and practice of structural equation modeling. [Google Scholar]
- Kuntsche E, Knibbe R, Engels R, Gmel G. Drinking motives as mediators of the link between alcohol expectancies and alcohol use among adolescents. Journal of Studies on Alcohol and Drugs. 2007;68:76–85. doi: 10.15288/jsad.2007.68.76. [DOI] [PubMed] [Google Scholar]
- Kuntsche E, Knibbe R, Gmel G, Engels R. Why do young people drink? A review of drinking motives. Clinical Psychology Review. 2005;25:841–861. doi: 10.1016/j.cpr.2005.06.002. [DOI] [PubMed] [Google Scholar]
- Kuntsche E, Knibbe R, Gmel G, Engels R. Replication and validation of the Drinking Motive Questionnaire Revised (DMQ-R, Cooper, 1994) among adolescents in Switzerland. European Addiction Research. 2006;12:161–168. doi: 10.1159/000092118. [DOI] [PubMed] [Google Scholar]
- LaBrie JW, Hummer JF, Neighbors C, Larimer ME. Whose opinion matters? The relationship between injunctive norms and alcohol consequences in college students. Addictive Behaviors. 2010a;35:343–349. doi: 10.1016/j.addbeh.2009.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaBrie JW, Kenney SR, Lac A. The use of protective behavioral strategies is related to reduced risk in heavy drinking college students with poorer mental and physical health. Journal of Drug Education. 2010b;40:361–378. doi: 10.2190/DE.40.4.c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaBrie JW, Kenney SR, Lac A, Garcia JA, Ferraiolo P. Mental and social health impacts the use of protective behavioral strategies in reducing risky drinking and alcohol consequences. Journal of College Student Development. 2009;50:35–49. doi: 10.1353/csd.0.0050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larimer ME, Turner AP, Anderson BK, Fader JS, Kilmer JR, Palmer RS, Cronce JM. Evaluating a brief alcohol intervention with fraternities. Journal of Studies on Alcohol. 2001;62:370–380. doi: 10.15288/jsa.2001.62.370. [DOI] [PubMed] [Google Scholar]
- Lewis MA, Hove MC, Whiteside U, Lee CM, Kirkeby BS, Oster-Aaland L, Larimer ME. Fitting in and feeling fine: Conformity and coping motives as mediators of the relationship between social anxiety and problematic drinking. Psychology of Addictive Behaviors. 2008;22:58–67. doi: 10.1037/0893-164X.22.1.58. [DOI] [PubMed] [Google Scholar]
- Linde L, Bergström M. The effect of one night without sleep on problem-solving and immediate recall. Psychological Research. 1992;54:127–136. doi: 10.1007/BF00937141. [DOI] [PubMed] [Google Scholar]
- Lovibond SH, Lovibond PF. 2nd ed. Sydney, Australia: Psychology Foundation; 1995. Manual for the depression, anxiety and stress scales. [Google Scholar]
- Lund HG, Reider BD, Whiting AB, Prichard JR. Sleep patterns and predictors of disturbed sleep in a large population of college students. Journal of Adolescent Health. 2010;46:124–132. doi: 10.1016/j.jadohealth.2009.06.016. [DOI] [PubMed] [Google Scholar]
- MacCallum RC, Browne MW, Sugawara HM. Power analysis and determination of sample size for covariance structure modeling. Psychological Methods. 1996;1:130–149. [Google Scholar]
- MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annual Review of Psychology. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacLean MG, Lecci L. A comparison of models of drinking motives in a university sample. Psychology of Addictive Behaviors. 2000;14:83–87. doi: 10.1037//0893-164x.14.1.83. [DOI] [PubMed] [Google Scholar]
- Maher MJ, Rego SA, Asnis GM. Sleep disturbances in patients with post-traumatic stress disorder: Epidemiology, impact and approaches to management. CNS Drugs. 2006;20:567–590. doi: 10.2165/00023210-200620070-00003. [DOI] [PubMed] [Google Scholar]
- Martens MP, Cimini MD, Barr AR, Rivero EM, Vellis PA, Desemone GA, Horner KJ. Implementing a screening and brief intervention for high-risk drinking in university-based health and mental health care settings: Reductions in alcohol use and correlates of success. Addictive Behaviors. 2007a;32:2563–2572. doi: 10.1016/j.addbeh.2007.05.005. [DOI] [PubMed] [Google Scholar]
- Martens MP, Ferrier AG, Sheehy MJ, Corbett K, Anderson DA, Simmons A. Development of the Protective Behavioral Strategies Survey. Journal of Studies on Alcohol. 2005;66:698–705. doi: 10.15288/jsa.2005.66.698. [DOI] [PubMed] [Google Scholar]
- Martens MP, Martin JL, Hatchett ES, Fowler RM, Fleming KM, Karakashian MA, Cimini MD. Protective behavioral strategies and the relationship between depressive symptoms and alcohol-related negative consequences among college students. Journal of Counseling Psychology. 2008;55:535–541. doi: 10.1037/a0013588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martens MP, Neighbors C, Dams-O’Connor K, Lee CM, Larimer ME. The factor structure of a dichotomously scored Rutgers Alcohol Problem Index. Journal of Studies on Alcohol and Drugs. 2007b;68:597–606. doi: 10.15288/jsad.2007.68.597. [DOI] [PubMed] [Google Scholar]
- Mayers AG, Grabau EAS, Campbell C, Baldwin DS. Subjective sleep, depression and anxiety: Inter-relationships in a nonclinical sample. Human Psychopharmacology: Clinical and Experimental. 2009;24:495–501. doi: 10.1002/hup.1041. [DOI] [PubMed] [Google Scholar]
- McNally AM, Palfai TP, Levine RV, Moore BM. Attachment dimensions and drinking-related problems among young adults: The mediational role of coping motives. Addictive Behaviors. 2003;28:1115–1127. doi: 10.1016/s0306-4603(02)00224-1. [DOI] [PubMed] [Google Scholar]
- Merrill JE, Read JP. Motivational pathways to unique types of alcohol consequences. Psychology of Addictive Behaviors. 2010;24:705–711. doi: 10.1037/a0020135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller BE, Miller MN, Verhegge R, Linville HH, Pumariega AJ. Alcohol misuse among college athletes: Self-medication for psychiatric symptoms? Journal of Drug Education. 2002;32:41–52. doi: 10.2190/JDFM-AVAK-G9FV-0MYY. [DOI] [PubMed] [Google Scholar]
- Moo-Estrella J, Pérez-Benítez H, Solís-Rodríguez F, Arankowsky-Sandoval G. Evaluation of depressive symptoms and sleep alterations in college students. Archives of Medical Research. 2005;36:393–398. [Google Scholar]
- MtvU and the Associated Press. College stress and mental health poll, Executive summary. 2008 Retrieved from http://www.halfofus.com/_media/_pr/mtvU_AP_College_Stress_and_Mental_Health_Poll_Executive_Summary.pdf. [Google Scholar]
- Neighbors C, Dillard AJ, Lewis MA, Bergstrom RL, Neil TA. Normative misperceptions and temporal precedence of perceived norms and drinking. Journal of Studies on Alcohol. 2006;67:290–299. doi: 10.15288/jsa.2006.67.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neighbors C, Larimer ME, Lewis MA. Targeting misperceptions of descriptive drinking norms: Efficacy of a computer-delivered personalized normative feedback intervention. Journal of Consulting and Clinical Psychology. 2004;72:434–447. doi: 10.1037/0022-006X.72.3.434. [DOI] [PubMed] [Google Scholar]
- Nelson J, Harvey AG. Pre-sleep imagery under the microscope: A comparison of patients with insomnia and good sleepers. Behaviour Research and Therapy. 2003;41:273–284. doi: 10.1016/s0005-7967(02)00010-4. [DOI] [PubMed] [Google Scholar]
- Nilsson JP, Söderström M, Karlsson AU, Lekander M, Akerstedt T, Linderoth NE, Axelsson J. Less effective executive functioning after one night’s sleep deprivation. Journal of Sleep Research. 2005;14:1–6. doi: 10.1111/j.1365-2869.2005.00442.x. [DOI] [PubMed] [Google Scholar]
- O’Hare T, Shen C. Substance use motives and severe mental illness. Journal of Dual Diagnosis. 2012;8:171–179. [Google Scholar]
- O’Hare T, Sherrer MV. Co-occurring stress and substance abuse in college first offenders. Journal of Human Behavior in the Social Environment. 2000;3:29–44. [Google Scholar]
- Okwumabua JO, Duryea EJ, Wong SP. Decision making correlates of depressive symptoms among African-American adolescents: Implications for prevention approaches. American Journal of Health Education. 2002;33:28–35. [Google Scholar]
- Oliver JM, Reed CKS, Smith BW. Patterns of psychological problems in university undergraduates: Factor structure of symptoms of anxiety and depression, physical symptoms, alcohol use, and eating problems. Social Behavior and Personality: An International Journal. 1998;26:211–232. [Google Scholar]
- Park CL, Armeli S, Tennen H. The daily stress and coping process and alcohol use among college students. Journal of Studies on Alcohol. 2004;65:126–135. doi: 10.15288/jsa.2004.65.126. [DOI] [PubMed] [Google Scholar]
- Patten CA, Choi WS, Gillin JC, Pierce JP. Depressive symptoms and cigarette smoking predict development and persistence of sleep problems in US adolescents. Pediatrics. 2000;106:E23. doi: 10.1542/peds.106.2.e23. [DOI] [PubMed] [Google Scholar]
- Pauley PM, Hesse C. The effects of social support, depression, and stress on drinking behaviors in a college student sample. Communication Studies. 2009;60:493–508. [Google Scholar]
- Pedrelli P, Farabaugh AH, Zisook S, Tucker D, Rooney K, Katz J, Fava M. Gender, depressive symptoms and patterns of alcohol use among college students. Psychopathology. 2011;44:27–33. doi: 10.1159/000315358. [DOI] [PubMed] [Google Scholar]
- Pieters S, Van Der Vorst H, Burk WJ, Wiers RW, Engels RCME. Puberty-dependent sleep regulation and alcohol use in early adolescents. Alcoholism: Clinical and Experimental Research. 2010;34:1512–1518. doi: 10.1111/j.1530-0277.2010.01235.x. [DOI] [PubMed] [Google Scholar]
- Rice KG, Van Arsdale AC. Perfectionism, perceived stress, drinking to cope, and alcohol-related problems among college students. Journal of Counseling Psychology. 2010;57:439–450. [Google Scholar]
- Riemann D, Berger M, Voderholzer U. Sleep and depression—Results from psychobiological studies: An overview. Biological Psychology. 2001;57:67–103. doi: 10.1016/s0301-0511(01)00090-4. [DOI] [PubMed] [Google Scholar]
- Roehrs T, Beare D, Zorick F, Roth T. Sleepiness and ethanol effects on simulated driving. Alcoholism: Clinical and Experimental Research. 1994;18:154–158. doi: 10.1111/j.1530-0277.1994.tb00896.x. [DOI] [PubMed] [Google Scholar]
- Roehrs T, Roth T. State-altering actions of ethanol, caffeine, and nicotine. In: Lydic R, Baghdoyan HA, editors. Handbook of behavioral state control-cellular and molecular mechanisms. New York, NY: CRC Press; 1998. pp. 421–432. [Google Scholar]
- Satorra A, Bentler PM. Corrections to test statistics and standard errors in covariance structure analysis. In: von Eye A, Clogg CC, editors. Latent variable analysis: Applications for developmental research. Thousand Oaks, CA: Sage; 1994. pp. 399–419. [Google Scholar]
- Satorra A, Bentler PM. A scaled difference chi-square test statistic for moment structure analysis. Psychometrika. 2001;66:507–514. doi: 10.1007/s11336-009-9135-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart SH, Loughlin HL, Rhyno E. Internal drinking motives mediate personality domain—Drinking relations in young adults. Personality and Individual Differences. 2001;30:271–286. [Google Scholar]
- Stewart SH, Zvolensky MJ, Eifert GH. Negative-reinforcement drinking motives mediate the relation between anxiety sensitivity and increased drinking behavior. Personality and Individual Differences. 2001;31:157–171. [Google Scholar]
- Sugarman DE, Carey KB. The relationship between drinking control strategies and college student alcohol use. Psychology of Addictive Behaviors. 2007;21:338–345. doi: 10.1037/0893-164X.21.3.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szklo-Coxe M, Young T, Finn L, Mignot E. Depression: Relationships to sleep paralysis and other sleep disturbances in a community sample. Journal of Sleep Research. 2007;16:297–312. doi: 10.1111/j.1365-2869.2007.00600.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor DJ, Bramoweth AD. Patterns and consequences of inadequate sleep in college students: Substance use and motor vehicle accidents. Journal of Adolescent Health. 2010;46:610–612. doi: 10.1016/j.jadohealth.2009.12.010. [DOI] [PubMed] [Google Scholar]
- Terlecki MA, Buckner JD, Larimer ME, Copeland AL. The role of social anxiety in a brief alcohol intervention for heavydrinking college students. Journal of Cognitive Psychotherapy. 2011;25:7–21. [Google Scholar]
- Thomas M, Sing H, Belenky G, Holcomb H, Mayberg H, Dannals R, Redmond D. Neural basis of alertness and cognitive performance impairments during sleepiness I. Effects of 24 h of sleep deprivation on waking human regional brain activity. Journal of Sleep Research. 2000;9:335–352. doi: 10.1046/j.1365-2869.2000.00225.x. [DOI] [PubMed] [Google Scholar]
- Thomas M, Sing HS, Belenky G, Holcomb HH, Mayberg HS, Dannals RF, Redmond DP. Neural basis of alertness and cognitive performance impairments during sleepiness II. Effects of 48 and 72 h of sleep deprivation on waking human regional brain activity. Thalamus & Related Systems. 2003;2:199–229. doi: 10.1046/j.1365-2869.2000.00225.x. [DOI] [PubMed] [Google Scholar]
- Thornton LK, Baker AL, Lewin TJ, Kay-Lambkin FJ, Kavanagh D, Richmond R, Johnson MP. Reasons for substance use among people with mental disorders. Addictive Behaviors. 2012;37:427–434. doi: 10.1016/j.addbeh.2011.11.039. [DOI] [PubMed] [Google Scholar]
- Tragesser SL, Sher KJ, Trull TJ, Park A. Personality disorder symptoms, drinking motives, and alcohol use and consequences: Cross-sectional and prospective mediation. Experimental and Clinical Psychopharmacology. 2007;15:282–292. doi: 10.1037/1064-1297.15.3.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai L-L, Li S-P. Sleep patterns in college students: Gender and grade differences. Journal of Psychosomatic Research. 2004;56:231–237. doi: 10.1016/S0022-3999(03)00507-5. [DOI] [PubMed] [Google Scholar]
- Turner AP, Larimer ME, Sarason IG. Family risk factors for alcohol-related consequences and poor adjustment in fraternity and sorority members: Exploring the role of parent-child conflict. Journal of Studies on Alcohol. 2000;61:818–826. doi: 10.15288/jsa.2000.61.818. [DOI] [PubMed] [Google Scholar]
- Tynjälä J, Kannas L, Levälahti E. Perceived tiredness among adolescents and its association with sleep habits and use of psychoactive substances. Journal of Sleep Research. 1997;6:189–198. doi: 10.1046/j.1365-2869.1997.00048.x. [DOI] [PubMed] [Google Scholar]
- Uhde TW, Cortese BM, Vedeniapin A. Anxiety and sleep problems: Emerging concepts and theoretical treatment implications. Current Psychiatry Reports. 2009;11:269–276. doi: 10.1007/s11920-009-0039-4. [DOI] [PubMed] [Google Scholar]
- Ullman JB. Structural equation modeling: Reviewing the basics and moving forward. Journal of Personality Assessment. 2006;87:35–50. doi: 10.1207/s15327752jpa8701_03. [DOI] [PubMed] [Google Scholar]
- Ullman JB, Bentler PM. Structural equation modeling. In: Schinka JA, Velicer WF, editors. Handbook of psychology. Hoboken, NJ: Wiley; 2003. pp. 607–634. [Google Scholar]
- Ware JC, Morin CM. Sleep in depression and anxiety. In: Pressman MR, Orr WC, editors. Understanding sleep: The evaluation and treatment of sleep disorders. Washington, DC: American Psychological Association; 1997. pp. 483–503. [Google Scholar]
- Wechsler H, Lee JE, Kuo M, Seibring M, Nelson TF, Lee H. Trends in college binge drinking during a period of increased prevention efforts. Findings from 4 Harvard School of Public Health College Alcohol Study surveys: 1993-2001. Journal of American College Health. 2002;50:203–217. doi: 10.1080/07448480209595713. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Greenwald S, Niño-Murcia G, Dement WC. The morbidity of insomnia uncomplicated by psychiatric disorders. General Hospital Psychiatry. 1997;19:245–250. doi: 10.1016/s0163-8343(97)00056-x. [DOI] [PubMed] [Google Scholar]
- Weitzman ER. Poor mental health, depression, and associations with alcohol consumption, harm, and abuse in a national sample of young adults in college. Journal of Nervous and Mental Disease. 2004;192:269–277. doi: 10.1097/01.nmd.0000120885.17362.94. [DOI] [PubMed] [Google Scholar]
- Westmaas J, Moeller S, Woicik PB. Validation of a measure of college students’ intoxicated behaviors: Associations with alcohol outcome expectancies, drinking motives, and personality. Journal of American College Health. 2007;55:227–237. doi: 10.3200/JACH.55.4.227-237. [DOI] [PubMed] [Google Scholar]
- White HR, Labouvie EW. Towards the assessment of adolescent problem drinking. Journal of Studies on Alcohol. 1989;50:30–37. doi: 10.15288/jsa.1989.50.30. [DOI] [PubMed] [Google Scholar]
- Wimmer F, Hoffmann RF, Bonato RA, Moffitt AR. The effects of sleep deprivation on divergent thinking and attention processes. Journal of Sleep Research. 1992;1:223–230. doi: 10.1111/j.1365-2869.1992.tb00043.x. [DOI] [PubMed] [Google Scholar]
- Windle M, Windle RC. Testing the specificity between social anxiety disorder and drinking motives. Addictive Behaviors. 2012;37:1003–1008. doi: 10.1016/j.addbeh.2012.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfson AR. Adolescents and emerging adults’ sleep patterns: New developments. Journal of Adolescent Health. 2010;46:97–99. doi: 10.1016/j.jadohealth.2009.11.210. [DOI] [PubMed] [Google Scholar]
- Wong MM, Brower KJ, Fitzgerald HE, Zucker RA. Sleep problems in early childhood and early onset of alcohol and other drug use in adolescence. Alcoholism: Clinical and Experimental Research. 2004;28:578–587. doi: 10.1097/01.alc.0000121651.75952.39. [DOI] [PubMed] [Google Scholar]