INTRODUCTION
Inflammatory Bowel Disease (IBD) impairs the quality of life of many children and adults. The disorder of intestinal inflammation results from chronic conditions, such as Crohn's disease and ulcerative colitis. Twenty percent of patients diagnosed with IBD are in the pediatric age range though mostly greater than 6 years of age.1 The incidence of this chronic inflammatory condition is on the rise in children. Studies in Sweden, Norway and the United States have demonstrated this dramatic increase with estimated incidence of 7–10 children out of 100,000 developing IBD in any given year.2,3,4 There are an estimated 50,000 – 100,000 children who presently have IBD in the United States.5 The incidence of Crohn’s in children appears twice that of ulcerative colitis.2,4 Though most cases of IBD in children are diagnosed in the second to third decades of life, very young children (<6 yrs of age) can also present with IBD. In this group, ulcerative colitis appears as common as Crohn’s.6 This review will focus on the special aspects of pediatric IBD and the implications on the diagnosis and management of this disease with significant morbidity.
ETIOLOGY
Though the etiology is unclear, IBD is believed to result from an interaction of genetics, host immunity and environmental factors. One of the most important risk factor for developing IBD is a positive family history of the disorder.7 Other possible factors include a child’s living conditions,8,9 maternal smoking and older maternal age during pregnancy.10 Controversial factors include protective role of breast-feeding and whether certain vaccines, in particular measles vaccines, are risk factors for developing IBD.11 The most recent evidence does not suggest this latter association.12
Despite extensive effort, a gene defect responsible for pediatric onset IBD has not been identified. However, genetics appears to play a significant role in patients who present earlier in life. Monozygotic twins have a 50% concordance risk for Crohn’s and children of parents with Crohn’s have a 33% risk of developing the disease.13,14 A single gene for IBD has yet to be identified but the number of susceptibility loci associated with IBD has grown exponentially. The gene for NOD2/CARD15 (caspase activation recruitment domain), an important protein in innate immunity, was one of the first associated risk alleles for Crohn’s. with a 20–40 fold increased risk of developing disease if a person has two risk alleles.15 More recently, genomewide association studies (GWAS) have identified over 100 independent gene loci associated with the disease.16 GWAS in children and young adults have reproduced loci implicated in the GWAS of adult onset Crohn’s disease.17 Interestingly, there is extensive crossover of genes between Crohn’s and ulcerative colitis revealing the common link between these chronic inflammatory conditions and the spectrum of the disease.16,17,18 The genetic loci identified in patients with Crohn’s and ulcerative colitis implicate many biologically relevant immune pathways such as IL-23 and IL-10. For the most part, though overlap exists, Crohn’s genes variations appear to be in pathways involved in microbe recognition and immune system responses such as autophagy while in UC genes appear to be involved in intestinal barrier integrity and function.16 In infants, one genetic mutation of significant interest is found in the interleukin-10 (IL-10) pathway.19 This rare autosomal recessive mutation leads to an infantile form of severe IBD that sometimes requires bone marrow transplantation.
DIAGNOSIS
Similar to adults, pediatric IBD patients present most commonly with diarrhea and abdominal pain (Table 1). Rectal bleeding occurs more often in ulcerative colitis patients while Crohn’s patients will more likely have perianal disease. Further, weight loss is seen in most children with Crohn’s disease at the time of presentation. This malnutrition in these patients results from suboptimal dietary intake, increased gastrointestinal losses, malabsorption and possibly increased requirements associated with chronic inflammatory activity. In fact, patients may be mistakenly diagnosed with anorexia nervosa given the severity of their presentation and the fear that eating will lead to worsening of symptoms.
Table 1.
Presenting symptoms of new onset Crohn’s disease and ulcerative colitis in children (most common to least common).
| Crohn’s Disease | Ulcerative Colitis |
|---|---|
| Abdominal pain | Rectal bleeding |
| Weight loss | Diarrhea |
| Growth failure | Urgency/Tenesmus |
| Anemia | Abdominal pain |
| Diarrhea | Anemia |
| Perianal disease | Weight loss |
| Fevers | Fevers |
| Arthritis | Arthritis |
| Skin lesions | Skin lesions |
Growth failure
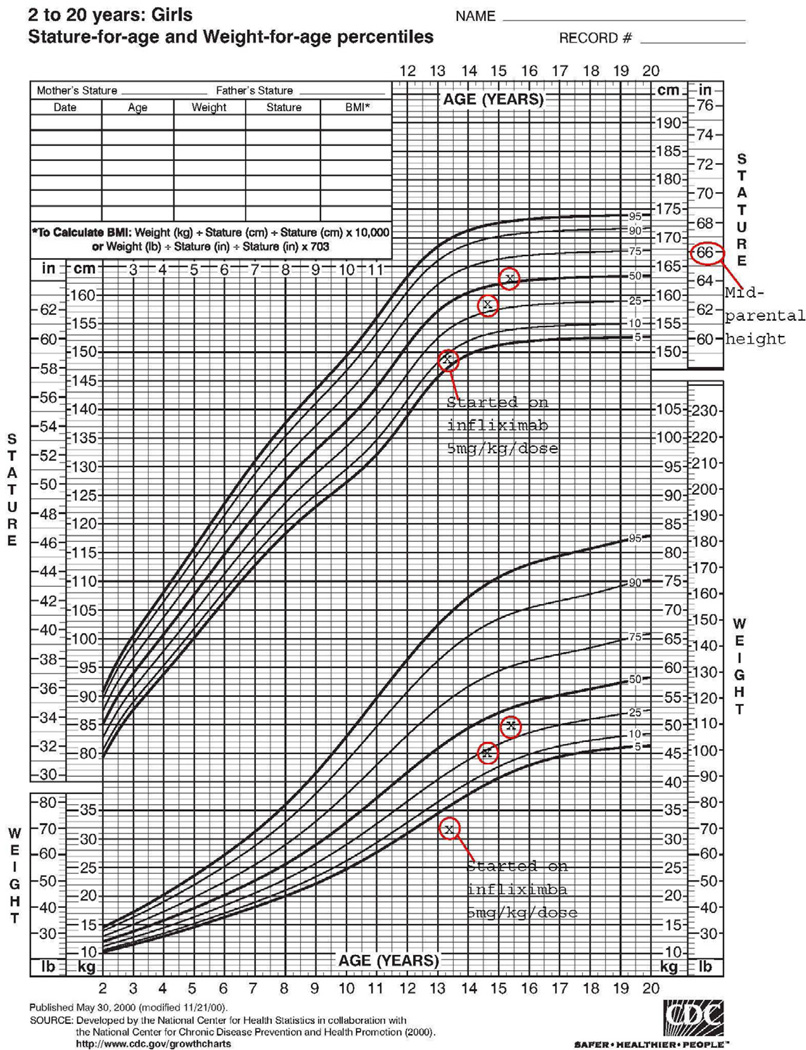
A unique aspect of pediatric IBD is the issues related to growth. Forty percent of children with Crohn’s disease have growth failure compared to <10% of ulcerative colitis patients.20 In fact, evidence of impaired linear growth may be the only presenting sign of IBD and can precede gastrointestinal symptoms (Figure 1). Growth failure is likely secondary to chronic malnutrition due to inadequate intake, excessive losses and increased energy requirement, as well as the effects of inflammation on growth.21,22 Interestingly, patients appear to have normal growth hormone levels, but insulin-like growth factor (IGF) 1 is reduced, suggesting hormone insensitivity possibly secondary to inflammation instead of deficiency.23 Medication can play a role in growth failure as well. Recurrent and chronic administration of high-dose corticosteroids may lead to decreased collagen production and hence decrease in linear growth.24 The medical and self esteem problems associated with growth failure in pediatric patients with IBD must be considered especially when contemplating usage of prolonged corticosteroid therapy.
Figure 1.
Growth curve of a young female with Crohn’s disease who was started on infliximab. Height is well below the mid parental height prior to initiation of infliximab. On anti-tumor necrosis factor therapy, the growth velocity dramatically improves to on par with the mid parental height.
Laboratory Testing
Similar to adults with IBD, standard diagnostic laboratory testing is employed in pediatric patients. Patients are evaluated for anemia, iron deficiency, elevation in markers of inflammation (i.e. ESR, C-reactive protein, fecal calprotectin), hypoalbuminemia as a marker of poor nutrition and stool studies are used to exclude infections as a cause for symptoms. Unique to the pediatric IBD patients is the fact that some, especially those with milder disease, may present with no laboratory abnormality. In one study, 21% of pediatric patients with mild Crohn’s disease and 54% with mild ulcerative colitis had normal ESR, hemoglobin, platelet count and albumin. In contrast, those with moderate/severe disease had normal parameters in approximately 4% of the cohort.25 Fecal calprotectin, a protein derived from neutrophils, is a marker, that can be non-invasively obtained, and appears as a good marker for diagnosing IBD and detecting flares.26
There is a growing knowledge regarding immunologic markers for categorizing patients with IBD. Antineutrophil cytoplasmic antibody (ANCA), anti-Saccharomyces cerevisiae antibody (ASCA), an antibody to the Escherichia coli-related outer membrane porin C (anti-OmpC) and anti-Cbir1 antibody (antibody against flagellin) have been used in trying to differentiate Crohn’s from ulcerative colitis as well providing insight into prognosis. Perinuclear ANCA (pANCA) is detected in the serum of 60–70% of patients with ulcerative colitis while in only 15–25% of patients with Crohn’s disease.27,28 This latter group exhibits an ulcerative colitis like Crohn’s picture with predominant colonic disease. Anit-Cbir1 antibody has been shown to be present in approximately 50% of pANCA positive Crohn’s patients as opposed to <5% of those with ulcerative colitis. This marker appears to help differentiate ulcerative colitis from Crohn’s patients who have ulcerative colitis type symptoms.29 On the other hand, ASCA (IgG or IgA) is highly predictive of Crohn’s disease,28,30 especially in the absence of ANCA. Patients less than 7 years of age appear to express a different antibody profile as they are more likely to have antibody to Cbir1 in comparison to older children who have higher rates of ASCA.31 Antibodies also serve a prognostic role. In children with Crohn’s, the sum of positive antibodies predicts more complicated disease. As the number and magnitude of these antibodies increases so does the incidence of internal penetrating and stricturing disease leading to high surgery rates.32
Endoscopic Evaluation
Endoscopic evaluation remains the gold standard for the diagnosis of IBD. Children should undergo both an upper endoscopy and colonoscopy during the initial evaluation for IBD. The upper gastrointestinal tract may be involved in over 50% of patients with IBD.32 Although findings in the upper tract may be non-specific, it can provide additional information in patients with indeterminate disease. Inflammation is most commonly noted in the stomach and although non-specific gastritis is common in Crohn’s disease, it can also be present in patients with ulcerative colitis and hence it does not reliably differentiate between the two diseases.33 Children with upper gastrointestinal disease can have symptoms such as nausea, vomiting and weight loss but a proportion can be asymptomatic. To maximize yield, biopsies are done of macroscopically involved and non-involved tissue in both the upper and lower gastrointestinal tract.
Small bowel imaging
Small bowel imaging is strongly recommended in all children suspected to have IBD especially in patients who had unsuccessful ileal intubation or the diagnosis is indeterminate. Historically, the small bowel follow through (SBFT) examination has been the radiological technique of choice but with advancement in technology, other approaches such as such as ultrasound, computer tomography (CT), magnetic resonance imaging (MRI) and video wireless capsule endoscopy have increased options available for disease characterization. Ultrasound provides a noninvasive radiation free method to evaluate for bowel wall thickening with sensitivity of 75–95% and specificity of 67–100% for the diagnosis of Crohn’s disease.34 Limitations of ultrasound include operator dependency, technical difficulties depending on body habitus and inability to evaluate superficial lesions. CT, especially with negative luminal contrast in CT enterography or CT enteroclysis studies allows visualization of bowel-wall inflammation as well as fistulas and abscesses,35,36 but exposes children to significant radiation. MRI has the advantage of limiting radiation but it is more costly and requires a child to lie still for an extensive period of time. Oral enterography with intraluminal contrast and intravenous gadolinium has made the MRI as diagnostically effective or even superior to CT enterography and SBFT for detection of small bowel abnormalities and extra-enteric complications.37
TREATMENT
The therapeutic goal in treating patients with IBD is mucosal healing and long lasting remission. Treatment of pediatric patients with IBD should focus on the individual patient and requires a common sense approach with consideration of symptoms and quality of life including growth while minimizing side effects. There is a paucity of therapies approved specifically for children with IBD, hence most of the treatment regimens are extrapolated from adult studies. Similar to adults with IBD, children with IBD have been treated in a stepwise approach with less powerful medication tried first. However, as experience with biologic therapies and immunomodulators has increased, this approach has been challenged with consideration towards changing the natural history of the disease in patients presenting so early in their lives.
Steroid sparing strategies are preferable in the treatment of pediatric patients. Corticosteroids have multiple side effects including impairment of growth and aesthetic complications (acne, cushingoid facies, etc). Hence minimizing or avoiding usage of corticosteroids is always preferable in children with IBD.
Nutritional therapy is usually unique to pediatric patients. Though compliance can be an obstacle, a pediatric Crohn’s disease study has shown that a short course of polymeric diet was more effective than corticosteroids in inducing healing.38 This contradicts a Cochrane review meta-analysis that shows corticosteroids as more efficacious than enteral therapy for inducing remission in Crohn’s.39
The benefits of early usage of immunomodulators in IBD were demonstrated in a pediatric trial for patients with Crohn’s disease. Children with Crohn’s disease were put on steroids alone or corticosteroids with 6-mercaptopurine (6-MP).40 The latter group was significantly more likely to be off steroids and in remission after 600 days of therapy than the group treated with corticosteroids only. Interestingly, there was no difference in linear growth velocity between the groups. The emergence of anti-Tumor Necrosis Factor α (anti-TNFα) has added a powerful weapon to the arsenal in the fight against IBD. Most providers will utilize biologics when they are unable to wean patients off steroids after 4–6 months of immunomodulatory therapy or if there is significant growth failure secondary to disease. The REACH trial was the first of its kind in pediatrics utilizing a multicenter approach to study the efficacy and safety of infliximab in over 110 children with Crohn’s disease. Close to 90% of patients had clinical response at 10 wks and over 50% were in remission at 54 weeks post starting of the medication.41 Further, this study demonstrated an increase in height velocity in patients treated with infliximab with dramatic catch-up growth (Figure 1). Infliximab has also been shown effective in pediatric ulcerative colitis though the response is not as robust as in Crohn’s disease.42 It is important to consider infliximab, surgery or cyclosporine in pediatric patients who are hospitalized with severe ulcerative colitis not responsive to corticosteroids after 3 days.42 In addition to infliximab, newer biologics which ones? already approved for treatment of adult patients with IBD are currently in trials for pediatric IBD.
Two areas of great interest in pediatric IBD treated with biologic therapies involve predicting which patients will respond to the treatment regimen and the debate on monotherapy (i.e. biologic therapy only) vs. concomitant therapy (i.e. biologic plus immunomodulator). Research is ongoing in identifying phenotypic and genotypic features of pediatric patients that would be most predictive of primary non-response to biologic therapy.43 This would allow for creation of a predictive model that can be used to discuss a patient’s potential for response to biologic therapy. As for the ongoing argument regarding monotherapy vs. concomitant therapy, the jury is still out in pediatric patients, balancing potential increased efficacy with risk of malignancy, specifically hepatosplenic T-cell lymphoma (HSTCL). The recent SONIC trial has shown improved response rates in adults naïve to immunomodulators on concomitant therapy vs. monotherapy with no increased risk of malignancy.44 However HSTCL, a rare but unfortunately usually fatal lymphoma, has been reported in a handful of IBD patients (primarily males and less than age of 21) treated with 6-MP/azathioprine alone, or these medications combined with infliximab or adalimumab.45,46 Providers need to have long discussions with families reviewing the risks, benefits and alternatives when considering monotherapy or concomitant therapy in pediatric IBD patients.
Bone health
Children with IBD may develop osteopenia as a result of inflammatory cytokine production, malnutrition, malabsorption or inadequate intake of calcium and vitamin D, prolonged inactivity and/or corticosteroid therapy.47 When compared to controls, children with IBD, especially those on prolonged courses of corticosteroids, may be at increased risk for fractures.48 Bone mineral density (BMD) as determined by Dual Energy X-ray Absorptiometry (DEXA) is an appropriate method for bone mass assessment. However, z-scores instead of the standard t-scores should be utilized to compare a child’s BMD with a same age and sex control.49 Quantitative CT (QCT) is an alternative method for measuring BMD as it allows a true volumetric BMD but can involve higher radiation doses than DEXA.50
Psychosocial issues
IBD not only causes physical issues but also psychosocial burden on children. Compared with healthy children, pediatric patients with IBD can have issues with behavioral/emotional functioning, particularly depression and anxiety, social functioning, and self-esteem. Depression and anxiety is rampant in children with IBD. Symptoms of depression and/or anxiety have been noted in 25–30% of children with IBD and 10–30% meet criteria for clinical depression or an anxiety disorder.50 These rates are similar to children with other chronic illnesses.51 The majority of studies have shown that disease activity can improve with treatment of psychological issues.52,53 Programs such as summer camps for children with IBD, peer groups and counseling may be productive especially to improve self esteem. Medical management of depression and anxiety can be quite helpful when indicated.
Immunizations
Protection against vaccine-preventable illnesses is critical in pediatric IBD patients given the immune compromised state of active disease and immunosuppression induced by the majority of treatments such as immunomodulators and biologics. However, safety and efficacy of immunizations must be considered before recommending administration in these patients. With the exception of the ones with live agents (measles, mumps, rubella; varicella; influenza intranasal spray), vaccines can be safely administered in IBD patients even on immunosuppressants and hence immunization in pediatric and adult IBD patients should not deviate from recommended schedules in the general population.54 Recommendations for live agent vaccines are listed in Table 2. For patients who do receive vaccines while immune suppressed, adequate immune response should be assessed and repeat dosing should be considered if the response is insufficient.
Table 2.
Recommendations for avoidance of live agent vaccines in patients with IBD.
| Condition or Treatments | Avoid live agent vaccines |
|---|---|
| Active disease | Significant protein-calorie malnutrition |
| Corticosteroids | Prednisone 20 mg/d equivalent, or 2 mg/kg per day if less than 10 kg, for 2 wk or more, and within 3 mo of stopping |
| 6-mercaptopurine/azathipurine | Effective doses and within 3 months of stopping |
| Methotrexate | Effective doses and within 3 months of stopping |
| Infliximab | Effective doses and within 3 months of stopping |
CONCLUSIONS
The incidence of IBD in children is on the rise and approximately one-quarter of patients with IBD present in childhood. Pediatric IBD patients can suffer both physically and psychosocially. An individualized therapeutic strategy approach in a child with IBD is necessary in terms of both medical and psychosocial management. Special attention should be paid towards growth, immunizations and mental health. IBD is a disorder with potential morbidities and lifelong challenges hence understanding the different entities that affect children with the disorder can improve overall care.
Key Points.
The number of children with Inflammatory Bowel Disease (IBD) is on the rise.
Crohn’s disease and ulcerative colitis, the main subtypes of this intestinal inflammatory disease affects both children and adults.
Children are developing physically, emotionally and immunologically. The interface between this development and IBD impacts presentation, diagnosis and management.
This review focuses on the special aspects of Pediatric IBD and how these influence management of children with IBD.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited m anuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERNCES
- 1.Dubinsky M. Special issues in pediatric inflammatory bowel disease. World J of Gastroenterology. 2008;14:413–420. doi: 10.3748/wjg.14.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hildebrand H, Finkel Y, Grahnquist L, et al. Changing pattern of paediatric inflammatory bowel disease in northern Stockholm 1990–2001. Gut. 2003;52:1432–1434. doi: 10.1136/gut.52.10.1432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Perminow G, Brackmann S, Lyckander LG, et al. A characterization in childhood inflammatory bowel disease, a new population-based inception cohort from South-Eastern Norway, 2005–07, showing increased incidence in Crohn's disease. Scand J Gastroenterol. 2009;44:446–56. doi: 10.1080/00365520802647434. [DOI] [PubMed] [Google Scholar]
- 4.Kugathasan S, Judd RH, Hoffmann RG, et al. Epidemiologic and clinical characteristics of children with newly diagnosed inflammatory bowel disease in Wisconsin: a statewide population-based study. J Pediatr. 2003;143:525–531. doi: 10.1067/s0022-3476(03)00444-x. [DOI] [PubMed] [Google Scholar]
- 5.Baldassano RN, Piccoli DA. Inflammatory bowel disease in pediatric and adolescent patients. Gastroenterol Clin North Am. 1999;2:445–458. doi: 10.1016/s0889-8553(05)70064-9. [DOI] [PubMed] [Google Scholar]
- 6.Heyman MB, Kirschner BS, Gold BD, et al. Children with early-onset inflammatory bowel disease (IBD): analysis of a pediatric IBD consortium registry. J Pediatr. 2005;6:35–40. doi: 10.1016/j.jpeds.2004.08.043. [DOI] [PubMed] [Google Scholar]
- 7.Ahmad T, Satsangi J, McGovern D, et al. The genetics of inflammatory bowel disease. Aliment Pharmacol Ther. 2001;15:731–748. doi: 10.1046/j.1365-2036.2001.00981.x. [DOI] [PubMed] [Google Scholar]
- 8.Feeney MA, Murphy F, Clegg AJ, et al. A case-control study of childhood environmental risk factors for the development of inflammatory bowel disease. Eur J Gastroenterol Hepatol. 2002;14:529–534. doi: 10.1097/00042737-200205000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Blanchard JF, Bernstein CN, Wajda A, et al. Small-area variations and sociodemographic correlates for the incidence of Crohn’s disease and ulcerative colitis. Am J Epidemiol. 2001;154:328–335. doi: 10.1093/aje/154.4.328. [DOI] [PubMed] [Google Scholar]
- 10.Montgomery SM, Wakefield AJ, Ekbom A. Sex-specific risks for pediatric onset among patients with Crohn’s disease. Clin Gastroenterol Hepatol. 2003;1:303–309. [PubMed] [Google Scholar]
- 11.Corrao G, Tragnone A, Caprilli R, et al. Risk of inflammatory bowel disease attributable to smoking, oral contraception and breastfeeding in Italy: a nationwide case-control study. Cooperative Investigators of the Italian Group for the Study of the Colon and the Rectum (GISC) Int J Epidemiol. 1998;27:397–404. doi: 10.1093/ije/27.3.397. [DOI] [PubMed] [Google Scholar]
- 12.Robertson DJ, Sandler RS. Measles virus and Crohn’s disease: a critical appraisal of the current literature. Inflamm Bowel Dis. 2001;7:51–57. doi: 10.1097/00054725-200102000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Laharie D, Debeugny S, Peeters M, et al. Inflammatory bowel disease in spouses and their offspring. Gastroenterology. 2001;120:816–819. doi: 10.1053/gast.2001.22574. [DOI] [PubMed] [Google Scholar]
- 14.Halfvarson J, Bodin L, Tysk C, et al. Inflammatory bowel disease in a Swedish twin cohort: a long-term follow-up of concordance and clinical characteristics. Gastroenterology. 2003;124:1767–1773. doi: 10.1016/s0016-5085(03)00385-8. [DOI] [PubMed] [Google Scholar]
- 15.Bonen DK, Cho JH. The genetics of inflammatory bowel disease. Gastroenterology. 2003;124:521–536. doi: 10.1053/gast.2003.50045. [DOI] [PubMed] [Google Scholar]
- 16.McCauley JL, Abreu MT. Genetics in diagnosing and managing inflammatory bowel disease. Gatroenterol Clin North Am. 2012;31:513–522. doi: 10.1016/j.gtc.2012.01.002. [DOI] [PubMed] [Google Scholar]
- 17.Imielinski M, Baldassano RN, Griffiths A, et al. Common variants at five new loci associated with early-onset inflammatory bowel disease. Nature Genetics. 2009;41:1335–1340. doi: 10.1038/ng.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cho JH. The genetics and immunopathogenesis of inflammatory bowel disease. Nature Reviews Immunology. 2008;8:458–466. doi: 10.1038/nri2340. [DOI] [PubMed] [Google Scholar]
- 19.Glocker EO, Kotlarz D, Boztug K, et al. Inflammatory bowel disease and mutations affecting the interleukin-10 receptor. N Engl J Med. 2009;21:2033–2045. doi: 10.1056/NEJMoa0907206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kanof ME, Lake AM, Bayless TM. Decreased height velocity in children and adolescents before the diagnosis of Crohn’s disease. Gastroenterology. 1988;95:1523–1527. doi: 10.1016/s0016-5085(88)80072-6. [DOI] [PubMed] [Google Scholar]
- 21.Savage MO, Beattie RM, Camacho-Hubner C, et al. Growth in Crohn’s disease. Acta Paediatr Suppl. 1999;88:89–92. doi: 10.1111/j.1651-2227.1999.tb14360.x. [DOI] [PubMed] [Google Scholar]
- 22.Ballinger A. Fundamental mechanisms of growth failure in inflammatory bowel disease. Horm Res. 2002;58(Suppl 1):7–10. doi: 10.1159/000064756. [DOI] [PubMed] [Google Scholar]
- 23.Ballinger AB, Azooz O, El-Haj T, et al. Growth failure occurs through a decrease in insulin-like growth factor 1 which is independent of undernutrition in a rat model of colitis. Gut. 2000;46:694–700. doi: 10.1136/gut.46.5.695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hyams JS, Moore RE, Leichtner AM, et al. Relationship of type I procollagen to corticosteroid therapy in children with inflammatory bowel disease. J Pediatr. 1988;112:893–898. doi: 10.1016/s0022-3476(88)80210-5. [DOI] [PubMed] [Google Scholar]
- 25.Mack DR, Lanton C, Markowitz J, et al. Laboratory values for children with newly diagnosed Inflammatory Bowel Disease. Pediatrics. 2007;119:1113–1119. doi: 10.1542/peds.2006-1865. [DOI] [PubMed] [Google Scholar]
- 26.Kostakis ID, Cholidou KG, Vaiopoulos AG, et al. Fecal calprotectin in pediatric inflammatory bowel disease: a systematic review. Dig Dis Sci. 2013;58:309–319. doi: 10.1007/s10620-012-2347-5. [DOI] [PubMed] [Google Scholar]
- 27.Targan SR. The utility of ANCA and ASCA in inflammatory bowel disease. Inflamm Bowel Dis. 1999;5:61–63. doi: 10.1097/00054725-199902000-00008. discussion 66–67. [DOI] [PubMed] [Google Scholar]
- 28.Ruemmele FM, Targan SR, Levy G, et al. Diagnostic accuracy of serological assays in pediatric inflammatory bowel disease. Gastroenterology. 1998;115:822–829. doi: 10.1016/s0016-5085(98)70252-5. [DOI] [PubMed] [Google Scholar]
- 29.Targan SR, Landers CJ, Yang H, et al. Antibodies to CBir1 flagellin define a unique response that is associated independently with complicated Crohn's disease. Gastroenterology. 2005;128:2020–2028. doi: 10.1053/j.gastro.2005.03.046. [DOI] [PubMed] [Google Scholar]
- 30.Dubinsky MC, Ofman JJ, Urman M, et al. Clinical utility of serodiagnostic testing in suspected pediatric inflammatory bowel disease. Am J Gastroenterol. 2001;96:758–765. doi: 10.1111/j.1572-0241.2001.03618.x. [DOI] [PubMed] [Google Scholar]
- 31.Markowitz J, Kugathasan S, Dubinsky MC, et al. Age of diagnosis influences serologic responses in children with Crohn’s disease: a possible clue to etiology. Inflamm Bowel Dis. 2009;15:714–719. doi: 10.1002/ibd.20831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dubinsky MC, Kugathasan S, Mei L, et al. Increased immune reactivity predict aggressive complicating Crohn’s disease in children. Clin gastoenterol Hepatol. 2008;6:1105–1111. doi: 10.1016/j.cgh.2008.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Castellaneta SP, Afzal NA, Greenberg M, Deere H, Davies S, Murch SH, Walker-Smith JA, Thomson M, Srivistrava A. Diagnostic role of upper gastrointestinal endoscopy in pediatric inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2004;39:257–261. doi: 10.1097/00005176-200409000-00006. [DOI] [PubMed] [Google Scholar]
- 34.Sharif F, McDermott M, Dillon M, et al. Focally enhanced gastritis in children with Crohn’s disease and ulcerative colitis. Am J Gastroenterol. 2002;97:1415–1420. doi: 10.1111/j.1572-0241.2002.05785.x. [DOI] [PubMed] [Google Scholar]
- 35.Fraquelli M, Colli A, Casazza G, et al. Role of US in detection of Crohn disease: meta-analysis. Radiology. 2005;236:95–101. doi: 10.1148/radiol.2361040799. [DOI] [PubMed] [Google Scholar]
- 36.Salbeni S, Rondonotti E, Iozzelli A, et al. Imaging of the small bowel in Crohn’s disease: A review of old and new techniques. World J of Gastro. 2007;13:3279–3287. doi: 10.3748/wjg.v13.i24.3279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bodily KD, Fletcher JG, Solem CA, et al. Crohn disease: mural attenuation and thickness at contrast-enhanced CT enterography—correlation with endoscopic and histologic findings of inflammation. Radiology. 2006;238:505–516. doi: 10.1148/radiol.2382041159. [DOI] [PubMed] [Google Scholar]
- 38.Lee SS, Kim AY, Yang SK, et al. Crohn disease of the small bowel: comparison of CT enterography, MR enterography, and small-bowel follow-through as diagnostic techniques. Radiology. 2009;251:751–761. doi: 10.1148/radiol.2513081184. [DOI] [PubMed] [Google Scholar]
- 39.Borrelli O, Cordischi L, Cirulli M, Paganelli M, Labalestra V, Uccini S, Russo PM, Cucchiara S. Polymeric diet alone versus corticosteroids in the treatment of active pediatric Crohn's disease: a randomized controlled open-label trial. Clin Gastroenterol Hepatol. 2006;4:744–753. doi: 10.1016/j.cgh.2006.03.010. [DOI] [PubMed] [Google Scholar]
- 40.Zachos M, Tondeur M, Griffiths AM. Enteral nutritional therapy for induction of remission in Crohn's disease. Cochrane Database Syst Rev. 2007 doi: 10.1002/14651858.CD000542.pub2. 1:CD000542. [DOI] [PubMed] [Google Scholar]
- 41.Markowitz J, Grancher K, Kohn N, et al. A multicenter trial of 6-mercaptopurine and prednisone in children with newly diagnosed Crohn’s disease. Gastroenterology. 2000;119:895–902. doi: 10.1053/gast.2000.18144. [DOI] [PubMed] [Google Scholar]
- 42.Hyams J, Crandall W, Kugathasan S, et al. Induction and maintenance infliximab therapy for the treatment of moderate-to-severe Crohn's disease in children. Gastroenterology. 2007;132:863–873. doi: 10.1053/j.gastro.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 43.Turner D, Mack D, Leleiko N, et al. Severe pediatric ulcerative colitis: a prospective multicenter study of outcomes and predictors of response. Gastroenterology. 2010;138:2282–2291. doi: 10.1053/j.gastro.2010.02.047. [DOI] [PubMed] [Google Scholar]
- 44.Dubinsky MC, Mei L, Friedman M, et al. Genome wide association (GWA) predictors of anti-TNFalpha therapeutic responsiveness in pediatric inflammatory bowel disease. Inflamm Bowel Dis. 2010;16:1357–1366. doi: 10.1002/ibd.21174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sandborn WJ, Rutgeerts PJ, Reinisch W, et al. One Year Data from the Sonic Study: A Randomized, Double-Blind Trial Comparing Infliximab and Infliximab Plus Azathioprine to Azathioprine in Patients with Crohn's Disease Naive to Immunomodulators and Biologic Therapy. Gastroenterology. 2009;136:A:116. [Google Scholar]
- 46.Rosh JR, Gross T, Mamula P, et al. Hepatosplenic T-cell lymphoma in adolescents and young adults with Crohn’s disease: A cautionary tale? Inflamm Bowel Dis. 2007;13:1024–1030. doi: 10.1002/ibd.20169. [DOI] [PubMed] [Google Scholar]
- 47.Cucciara S, Escher JC, Hildebrand H. Pediatric inflammatory bowel diseases and the risk of lymphoma: should we revise our treatment strategies. J of Pediatric Gastroenterology and Nutrition. 2009;48:257–267. doi: 10.1097/mpg.0b013e31818cf555. [DOI] [PubMed] [Google Scholar]
- 48.Sentongo TA, Semaeo EJ, Stettler N, et al. Vitamin D status in children, adolescents, and young adults with Crohn disease. Am J Clin Nutr. 2002;76:1077–1081. doi: 10.1093/ajcn/76.5.1077. [DOI] [PubMed] [Google Scholar]
- 49.Van Staa TP, Cooper C, Brusse LS, et al. Inflammatory bowel disease and the risk of fracture. Gastroenterology. 2003;125:1591–1597. doi: 10.1053/j.gastro.2003.09.027. [DOI] [PubMed] [Google Scholar]
- 50.Sylvester FA. IBD and skeletal health: children are not small adults! Inflamm Bowel Dis. 2005;11:1020–1023. doi: 10.1097/01.mib.0000188341.96726.15. [DOI] [PubMed] [Google Scholar]
- 51.Bachrach LK. Osteoporosis and measurement of bone mass in children and adolescents. Endocrinol Metab Clin North Am. 2005;34:521–535. doi: 10.1016/j.ecl.2005.04.001. [DOI] [PubMed] [Google Scholar]
- 52.Mackner L, Crandall W, Szigethy E. Psychosocial functioning in pediatric inflammatory bowel disease. Inflamm Bowel Dis. 2006 Mar;12(3):239–244. doi: 10.1097/01.MIB.0000217769.83142.c6. [DOI] [PubMed] [Google Scholar]
- 53.Mawdsley JE, Rampton DS. Psychological stress in IBD: new insights into pathogenic and therapeutic implications. Gut. 2005;54:1481–1491. doi: 10.1136/gut.2005.064261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Deter HC, Keller W, von Wietersheim J, et al. Psychological treatment may reduce the need for healthcare in patients with Crohn’s disease. Inflamm Bowel Dis. 2007;13:745–752. doi: 10.1002/ibd.20068. [DOI] [PubMed] [Google Scholar]
- 55.Sands BE, Cuffari C, Katz J, Kugathasan S, Onken J, Vitek C, Orenstein W. Guidelines for immunizations in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2004;10:677–692. doi: 10.1097/00054725-200409000-00028. [DOI] [PubMed] [Google Scholar]