Abstract
Purpose
Despite the high morbidity of reoperative renal surgery (RRS) in patients with multifocal recurrent renal carcinoma, most patients are able to preserve adequate renal function to obviate the need for dialysis. The economic burden of RRS has not been evaluated. We aim to provide a cost-effectiveness analysis for patients requiring RRS on a solitary kidney.
Materials and Methods
We reviewed the charts of patients treated at the National Cancer Institute (NCI) requiring RRS from 1989 to 2010. Functional, oncological and surgical outcomes were evaluated, and the costs of RRS were calculated. We then compared the costs of a 33 patients cohort who underwent RRS on a solitary kidney and a hypothetical cohort of patients that would undergo uncomplicated nephrectomy, fistula placement and dialysis. All costs were calculated based on Medicare reimbursement rates derived from Current Procedural Terminology (CPT) codes. A cost-effectiveness analysis was applied.
Results
Despite a high complication rate (45%), 87% of patients maintained adequate renal function to avoid dialysis and 96% remained metastasis free at an average follow up of 3.12 years (range 0.3-16.4). When compared to hypothetical dialysis cohort, the financial benefit of RRS was reached at 0.68 years.
Conclusions
RRS is a viable alternative for patients with multifocal renal cell carcinoma requiring multiple surgical interventions, especially when left with a solitary kidney. Despite the high complication rate, most patients are able to preserve renal function and have excellent oncological outcomes. The financial benefit of RRS is reached at less than 1 year.
Keywords: Reoperative renal surgery, repeat partial nephrectomy, cost effectiveness, nephron sparing surgery
In the era of modern medicine and with the proliferation of new medical and surgical treatments, the economic impact of various treatments must be carefully examined. While certain medicines or surgical techniques have undoubtedly improved both patient survival and quality of life (QOL), others have offered little hope, insignificant clinical benefit and significant financial burden. Given the burgeoning impact of expensive new therapies and technologies along with the increasing focus on health care expenditures, it is imperative for physicians to remain cognizant about financial implications of their therapy while caring for patients with complex medical issues.
Reoperative surgeries of the kidney are an example of medical care now available to patients as a result of improvements in surgical techniques, anesthesia, and ICU support. Patients with hereditary cancer syndromes and multifocal RCC are prone to recurrence of kidney tumors and are likely to require reoperative renal surgery. Additionally, the persistent nature of multifocal RCC represents a challenging clinical problem, and may often necessitate the need for repeat surgery on the ipsilateral renal unit. We have previously shown that repeat partial nephrectomy is an excellent treatment for patients diagnosed with renal cell carcinoma. 1-3 Nevertheless, reoperative renal surgery possesses its challenges and is associated with high perioperative morbidity. 1,3 Despite its high complication rate, RRS allows for renal preservation in most patients.3
Performing reoperative surgery on a solitary renal unit presents an even more difficult dilemma, as these patients may progress to metastatic disease without intervention, or end up on dialysis in the case of a kidney loss. While Liu et al recently reported on surgical, functional and oncological outcomes of RRS, the cost effective analyses of such procedures have not been evaluated. 3 In light of the oncological and functional benefit of repeat partial nephrectomy, this study sought to address the cost effectiveness of repeat partial nephrectomy as compared with hypothetical cohort of patients who underwent completion nephrectomy and dialysis.
Materials and Methods
We reviewed the charts of patients treated at the National Cancer Institute requiring reoperative renal surgery from 1989 to 2010. Thirty-three patients who underwent repeat partial nephrectomy for recurrent or de novo renal masses in a solitary kidney were identified. Data gathered included total time in the operating room (OR), duration of ICU stay, duration of hospital stay, specific procedures done during hospitalization, OR returns, procedures done after hospitalization, and requirement for any blood products (including packed red blood cells, FFP, cryoprecipitate, or platelets). All imaging performed during hospitalization and follow up (CT, MRI, US, X-rays) were also included in the study. Additional data included interval time to next intervention (ablation, another partial nephrectomy, or completion nephrectomy), date of most recent follow up and most recent imaging. The functional outcomes were compared using preoperative and postoperative (at 3 months follow up) creatinine and eGFR.
Those patients in our cohort who ended up losing their renal units during hospitalization were only estimated to have incurred expense of hospitalization with no savings derived from avoiding dialysis. The costs of complications (conversion to total nephrectomy, dialysis, ureteral obstruction) were included in the cost estimates for the RRS cohort. For the hypothetical cohort requiring completion nephrectomy, we only included the costs of uncomplicated nephrectomy, uncomplicated AV fistula placement, and dialysis.
All costs were calculated using current Medicare reimbursement rates derived from Current Procedural Terminology (CPT) codes and Medicare reimbursement rates. Physician fees were included in the estimates and were estimated with facility fees. The national payment rate was used for physician fees. Despite the varying time frames that the patients had RRS and the possible varying costs of different procedures at respective times, all cost estimates were based on the 2010 calendar year.
Additionally, to account for potential errors in estimating costs for the cohort requiring the RRS, we have performed modeling with the assumption that the actual costs were underestimated by as much as 50%. The figure incorporating such analysis and modeling was also created.
Results
Table 1 shows clinical characteristics of patients in the RRS cohort. We identified 33 patients treated with repeat partial nephrectomy on a solitary renal unit. Four of those 33 (12%) patients incurred no benefit from repeat partial nephrectomy (1 patient had a postoperative MI and died in the immediate postoperative period, 3 patients had conversion of partial nephrectomy to total nephrectomy).
Table 1. Clinical characteristics of patients requiring RRS on a solitary kidney.
| Number of patients (%) | 33 (100) |
| Number of patients who avoided dialysis (%) | 29 (87) |
| Number of procedures | 39 |
| Median age at procedure (range) | 53 (28-79) |
| No. pts with cancer syndrome (%) | 25 (76) |
| VHL (%) | 24 (72) |
| HPRC- Type 1 (%) | 1 (3) |
| Men (%) | 67 |
| Median No. Tumors Removed (range) | 9 (1-55) |
The perioperative complication rate was 45%, with details of complications outlined in Table 2. Renal function is also shown in Table 3 and demonstrates that those retaining their renal units maintained at least 90% of the starting renal function. The most common complication was ureteral obstruction or urine leak requiring cystoscopy with ureteral stent placement, subsequently requiring return for cystoscopy and stent removal.
Table 2. Perioperative complications.
| Mortality (%) | 1 (3) |
| Ileus (%) | 1 (3) |
| Cardiac arrhythmia (%) | 1 (3) |
| Mesenteric repair (%) | 1 (3) |
| A fib (%) | 2 (6) |
| Prolonged intubation (%) | 1 (3) |
| Pleural effusion requiring thoracentesis (%) | 1 (3) |
| Ureteral obstruction (%) | 6 (18) |
| Ventral hernia (%) | 1 (3) |
| Pleurotomy (%) | 2 (6) |
| Return to OR (%) | 7 (21) |
| Acute Renal Failure (%) | 1 (3) |
| Loss of renal unit (%) | 3 (9) |
| #Patients retained renal unit (%) | 29 (87) |
Table 3. Renal functional outcomes*.
| Pre op | Post op | % from preop | P value | |
|---|---|---|---|---|
| Creatinine, mg/dl (range) | 1.5 (1.0-2.0) | 1.6 (0.82-2.9) | −6 | p=0.02 |
| eGFR ml/min/1.73 m2 (range) | 51 (35.1-73.1) | 47 (25.3-74.8) | −9 | p = 0.08 |
Calculations performed on data from 28 patients
Renal functional outcomes are indicated in Table 3. It demonstrates that 87% of patients kept functioning renal units. While there was a significant decline of preoperative renal function, in those with remaining renal units, greater than 90% of the starting renal function was preserved. Oncological outcomes demonstrated a 96% metastasis free survival at a mean follow up of 3.12 year. The mean time in to next intervention for the cohort was 3.12 years (0-16.4 years) with seven patients requiring repeat intervention.
Data from the hospital stay is listed in Table 4. It indicates the complexity of the procedures with some surgeries lasting as long as 11 hours, some requiring 32 units of blood, and some hospitalizations requiring 12 days of ICU stay. Costs are outlined in Table 5.
Table 4. Hospital stay data.
| Average procedure, hours (range) | 8 (4-11) |
| Average blood transfused, units (range) | 7 (0-32) |
| Average hospitalization, days (range) | 10 (6-30) |
| Average ICU stay, days (range) | 4 (1-12) |
| Average floor stay, days (range) | 7 (2-18) |
| Average time to follow- up, days (range) | 3 (0-16) |
Table 5. Outlined costs.
| Procedure | Current Procedural Terminology (CPT) code | Cost (USD) | Physician Fee (National Payment Amount) |
|---|---|---|---|
| Partial nephrectomy | 50240 | 13,000 | 1401.54 |
| Cystoscopy with removal of ureteral stent | 52310 | 2,277 | 161.50 |
| ICU Stay (per day) | 99291-99292 | 2,145 | 220.87, 110.62 |
| Floor stay (per day) | 99221-99223 | 832 | 97.34,132,194.32 |
| RBC (unit) | PO910 | 142 | n/a |
| FFP (unit) | P9023 | 51 | n/a |
| Platelet (unit) | P9019 | 67 | n/a |
| Cryoprecipitate (unit) | P9012 | 47 | n/a |
| CBC | 85025 | 11 | n/a |
| CMP | 80053 | 15 | n/a |
| Ultrasound (diagnostic and screening) | 76770 | 37.16 | 131.93 |
| CT with and without contrast | 74170 | 71.08 | 425.30 |
| MRI with and without contrast | 74183 | 113.65 | 682.11 |
| MRA with and without contrast | 74185 | 90.92 | 606.19 |
| X ray (chest, 2 views) | 71020 | 11.18 | 31.70 |
| Anesthesia | 00862 | 450 (1 hour), 690 (2 hours), 930 (3 hours), 1,170 (4 hours), 1,890 (7 hours), 2,010 (7.5 hours), 2,070 (7.5- 8 hours), 2,130 (8 hours) | Included in cost |
| Av fistula placement | 36825 | 5,900 | 841.07 |
| PACU | N/A | 365 | |
| Dialysis (per day) | 90999 | 90 | |
| Total nephrectomy | 50220 | 20,000 | 1091.07 |
| Kidney transplant | 50360, 50365 | 18,000-25,000 | 2773.58 |
| RFA | 50592 | 3790 | 3373.04 |
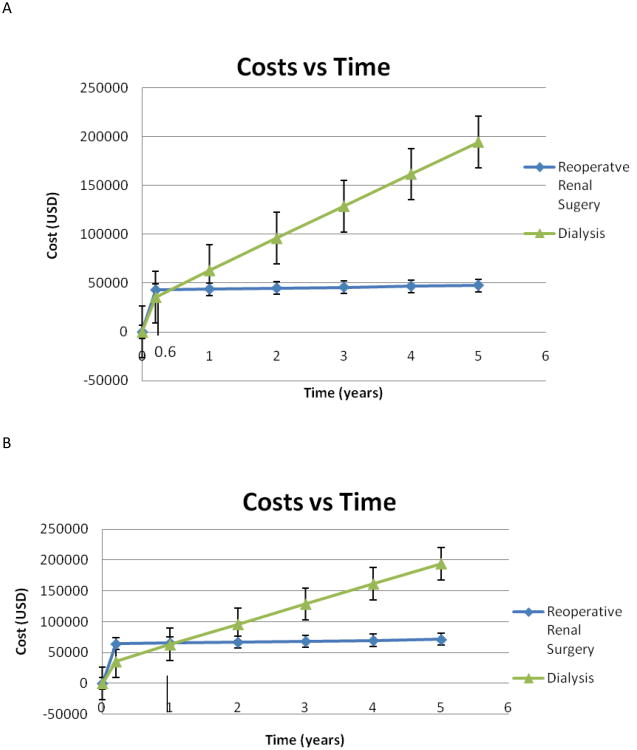
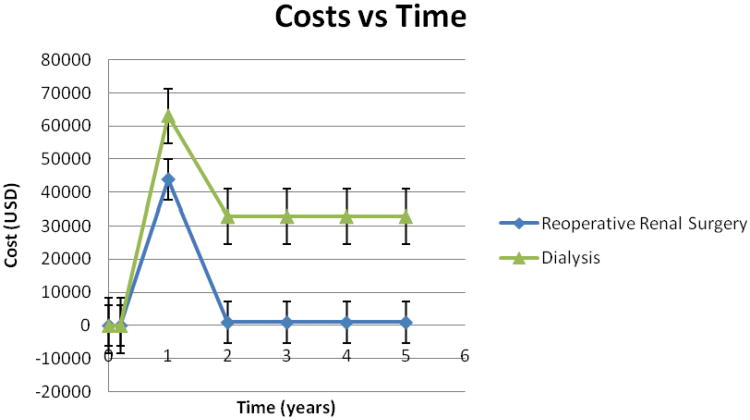
The financial benefit of RRS was estimated to be reached at 0.68 years (Figure 1A). Figure 1B demonstrates persistent financial benefit in less than 1 year for RRS group even after modeling accepting 50% underestimation of the surgical costs. Figure 2 shows the difference in costs of RRS vs dialysis per unit of time (1 year). The subsequent cost of dialysis of approximately $35,000 per year continue, while the future costs of follow up for patients treated with repeat surgery remain minimal until the next intervention.
Figure 1.
Analysis of cost benefit of reoperative renal surgery vs dialysis in relation to time. A: The actual model. Financial benefit of reoperative renal surgery is reached at 0.6 years. B: Model to show that if calculated costs of reoperative renal surgery are underestimated by 50%, financial benefit is reached at 1 year.
Figure 2.
Costs vs Time shown with costs per unit of time (1 year). The cost of RRS has an initial upstroke as the patient in the RRS cohort incurrs the initial cost of the procedure but steadies as the cost incurred per year is the cost of follow up. The costs of dialysis has an initial upstroke that represents the cost of AV fistula, uncomplicated nephrectomy and initial dialysis period with the cost per year of dialysis which are notably higher than the cost per year incurred by the patient undergoing RRS. The subsequent cost of dialysis of approximately $35,000 per year continue, while the future costs of follow up for patients treated with repeat surgery remain minimal until the next intervention.
Discussion
With improvements in surgical techniques, experience with challenging partial nephrectomies, and increased recognition of preservation of the renal function, the role of reoperative renal surgery has recently become a debated topic. While preserving substantial renal function, reoperative partial nephrectomies have been shown to be technically difficult and morbid.1-3 Some may question if such procedures should be offered to the patients in light of surgical risks Some may contend that patients may be better served forgoing RRS and proceeding with nephrectomy and renal replacement therapy. In addition to medical rationale, some may question the economic implications of such procedures since many patients require prolonged hospitalizations and carry a substantial financial burden to a health care system. In light of the growing financial considerations that patients, physicians, insurance companies, and the entire health care system faces today we performed the analysis evaluating the financial implications of RRS in patients who would otherwise be faced with renal replacement therapy.
To our own surprise, we have found that the cost benefits favor RRS and that savings are realized in a far less time than we expected (0.6 years). Even after adjustments for potential underestimation of costs, the cost savings are still reached in less than 1 year. Notably, in addition to major hospital expenses, every attempt was made to include any possible cost associated with the hospitalization, such as routine blood work and X-rays, and physician costs. The estimated cost for hospitalization per patient in the RRS cohort for the first year was US$43,787 for the first year and US$954 for each subsequent year (cost of postoperative and surveillance follow up visits). The estimated cost per patient in the hypothetical dialysis cohort was US$63,055 for the first year and US$32,850 for each subsequent year. Despite our careful efforts to avoid underestimating the costs associated with RRS, the financial benefit of the RRS over dialysis is substantial and unequivocal.
It is possible that cost savings of RRS are even greater than those reported in this study. Mir et al estimated the cost of open partial nephrectomy at $11,427 which is significantly lower than our estimated cost.4 While that study is based on costs at a single institution and evaluates less morbid surgeries, it leads us to believe that our cost estimates are reasonable at almost four times higher than the cost of uncomplicated nephrectomy. It is also probable that our estimates for hypothetical dialysis group are lower than actual costs, as we have purposely estimated the costs of the hypothetical dialysis arm to have no complications associated with completion nephrectomy, AV fistula or graft, and dialysis. Icks et al found that although 55% percent of costs can be attributed to dialysis procedures, other dialysis specific health care utilization strongly contributes to the cost.5 They demonstrated that hospitalization accounted for 14% of the per patient year costs, with shunt or catheter revision as the most frequent reasons.5
While RRS may carry significant surgical morbidity (including one mortality in our cohort), dialysis still accounts for a significant percentage of healthcare costs and significant complications. Patients receiving long-term hemodialysis have a yearly mortality rate of 15% to 20%.6,7 Evaluating the United States Renal Data System (USRDS), Ishani et al studied complications of 2358 dialysis patients with a median follow up of 3.2 years. Of these patients, a total of 527 (nearly 25%) had a hospital associated episode of septicemia.8 Either septicemia or bacteremia were associated with subsequent cardiovascular morbidity and mortality, peripheral vascular disease and stroke; with death rates from septicemia or bacteremia estimated to be up to 300 fold higher than in the general population.8 Additionally, vascular access procedures and complications account for over 20% of hospitalizations of dialysis patients in the United States and cost about $1 billion annually. 9,10
The other option for patients desiring to avoid hemodialysis is renal transplantation (not included in our modeling). While theoretically a more attractive option, renal transplantation is not a simple solution. It is reported that at the end of 2004, only about 23% of ESRD patients worldwide were living with a functioning kidney transplant and the remaining 77% were on dialysis.11 In the US, only 75% of patients who receive transplants survive at 5 years with 5-year graft survival rate of 75-80%. 7 While renal transplantation may indeed be an alternative, it is prone to graft failure with most patients requiring some period of dialysis. 7 It has been shown that as many as 33% of grafts fail at 5 years.7 Aside from the organ donor shortage, availability for transplantation of patients with solid tumors, and the cost of a renal transplant is estimated to be between US$18,000-US$25,000, not including anesthesia services, hospital stay, complications, possibility of rejection, or costs immunosuppressive drugs.
We acknowledge that the outcomes of dialysis or transplantation in our younger cohort may be quite different from the population quoted in the literature. Typically, the patients in the literature are older, have numerous comorbidities, and are frequently hospitalized. Because of this reasoning, in calculating the costs of the hypothetical dialysis arm we did not include any potential dialysis-related complications, readmissions, or additional expenses. Even with this correction and hypothetical 50% underestimation of the RRS costs (corrected in the model), the financial benefits of RRS are clear and are still achieved in less than 1 year.
The present study underscores the financial savings of the aggressive surgical intervention. Given a mean follow up for 3.12 years, the average cost saving per patient is estimated to be greater than US$100,000. For 29 patients who had benefit from repeat partial nephrectomy, the savings to the healthcare system was estimated to be greater than US$2,000,000 at only 3.12 years, with an increase in savings as the patients who continue to avoid dialysis. Notably, evaluating savings from a single patient in the cohort with the longest follow up of 16.4 years who remained dialysis free, economic benefit is likely to approach at least US$5 million (16 years × 30,000/year savings).
Consistent with prior reports on reoperative renal surgery this cohort has a similar complication profile and functional outcomes. Johnson et al reported on outcomes of repeat partial nephrectomy and found that complication rates are higher than in patients not previously operated.2 Similarly, Bratslavsky et al reported on a series of the patients treated at the NCI and found the major complication rate to be close to 50%.1 Liu et also showed a high perioperative complication rate (45%) in patients requiring RRS on a solitary kidney.3 Analyzing a small cohort of patients treated with post RFA partials, Kowalczyk et al found that the rate of reoperation and urine leak were higher than in the cohort requiring repeat partial nephrectomy.12 Of most importance, however, among all patients in these series, the vast majority avoided dialysis. Additionally, if the renal unit were preserved, at least 80% of preoperative renal function was maintained.13 Similarly to our prior reports, oncologic outcomes of the present study are encouraging.
Although beyond the scope of this manuscript, it is important to recognize quality of life (QOL) gained by the avoidance of renal replacement therapy.14-18 More specifically, Health-related QOL (HRQOL) is a multidimensional, patient- centered concept that encompasses physical health and symptoms, functional status, mental well- being and social functioning.14 In assessing HRQOL, a study by Carmichael et al used the Kidney Disease QOL questionnaire (KDQOL) which is a multidimensional, reliable and validated tool specially designed for dialysis patients. Using these tools, it was found that satisfactory sleep, dialysis related symptoms, effect of kidney disease on lifestyle and burden of kidney disease were the most important determinants of HRQOL for this population. 14 Given the literature on QOL in dialysis patients, it is likely that patients in the RRS cohort have a QOL that is greater than patients in the hypothetical dialysis cohort on the premise of renal function alone.15-18
The present study is not without limitations. It is retrospective in nature and studies patients with bilateral multifocal RCC that are not as common to other institutions which may limit a broader applicability of the findings. Also, the financial impact of active surveillance was not included in this analysis but it would most likely be the least expensive method of therapy. We routinely follow our patients with most hereditary tumors until the largest lesion reaches 3cm.19 Surveillance beyond this threshold in increases the risk for the development of metastatic disease and introduces a totally new calculation for financial burden associated with treatment of disseminated disease. The financial impact of using thermal ablative therapies instead of RRS was not evaluated in this study and warrants further analyses with the understanding that these techniques may not be appropriate for all patients who are candidates for RRS. 12 We have previously discussed challenges and limitations of ablations in patients with multifocal RCC elsewhere, indicating that ablation on a previously operated kidney may not be anatomically possible due to adhesions of the adjacent structures and viscera.12 Despite the limitations of this study, these data provide a compelling argument regarding the economic benefits of reoperative renal surgery.
Conclusion
In addition to renal functional preservation and excellent oncologic outcomes, reoperative renal surgery offers substantial financial benefit to the healthcare system. With increase in the popularity of nephron sparing surgery and recognition of the importance of preserved renal function, the RRS may become a more common procedure, especially in patients with a solitary renal unit. As clinicians become more mindful of costs associated with such procedures, the performance of RRS will likely lead to a significant decrease in healthcare costs, while benefiting the patient and the health care insurers.
Acknowledgments
We would like to thank Dr. Martin L. Brown of the Health Services and Economics Branch of the NIH/NCI for his assistance with this project.
This research was supported by the Intramural Research Program of the NIH, National Cancer Institute, Center for Cancer Research.
References
- 1.Bratslavsky G, Liu JJ, Johnson AD, Sudarshan S, Choyke PL, Linehan WM, et al. Salvage partial nephrectomy for hereditary renal cancer: feasibility and outcomes. J Urol. 2008;179:67. doi: 10.1016/j.juro.2007.08.150. [DOI] [PubMed] [Google Scholar]
- 2.Johnson A, Sudarshan S, Liu J, Linehan WM, Pinto PA, Bratslavsky G. Feasibility and outcomes of repeat partial nephrectomy. J Urol. 2008;180:89. doi: 10.1016/j.juro.2008.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liu NW, Khurana K, Sudarshan S, Pinto PA, Linehan WM, Bratslavsky G. Repeat partial nephrectomy on the solitary kidney: surgical, functional and oncological outcomes. J Urol. 2010;183:1719. doi: 10.1016/j.juro.2010.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mir SA, Cadaddu JA, Sleeper JP, Lotan Y. Cost Comparison of Robotic, Laparoscopic, and Open Partial Nephrectomy. Journal of Endoneurology. 25(3) doi: 10.1089/end.2010.0510. 3-2-0011. [DOI] [PubMed] [Google Scholar]
- 5.Icks A, Haastert B, Gandjour A, Chernyak N, Rathmann W, Giani G, et al. Costs of dialysis--a regional population-based analysis. Nephrol Dial Transplant. 2010;25:1647. doi: 10.1093/ndt/gfp672. [DOI] [PubMed] [Google Scholar]
- 6.Rocco MV, Frankenfield DL, Hopson SD, McClellan WM. Relationship between clinical performance measures and outcomes among patients receiving long-term hemodialysis. Ann Intern Med. 2006;145:512. doi: 10.7326/0003-4819-145-7-200610030-00009. [DOI] [PubMed] [Google Scholar]
- 7.Lin SJ, Koford JK, Baird BC, Habib AN, Reznik I, Chelamcharla M, et al. The association between length of post-kidney transplant hospitalization and long-term graft and recipient survival. Clin Transplant. 2006;20:245. doi: 10.1111/j.1399-0012.2005.00476.x. [DOI] [PubMed] [Google Scholar]
- 8.Ishani A, Collins AJ, Herzog CA, Foley RN. Septicemia, access and cardiovascular disease in dialysis patients: the USRDS Wave 2 study. Kidney Int. 2005;68:311. doi: 10.1111/j.1523-1755.2005.00414.x. [DOI] [PubMed] [Google Scholar]
- 9.Hakim R, Himmelfarb J. Hemodialysis access failure: a call to action. Kidney Int. 1998;54:1029. doi: 10.1046/j.1523-1755.1998.00122.x. [DOI] [PubMed] [Google Scholar]
- 10.Feldman HI, Kobrin S, Wasserstein A. Hemodialysis vascular access morbidity. J Am Soc Nephrol. 1996;7:523. doi: 10.1681/ASN.V74523. [DOI] [PubMed] [Google Scholar]
- 11.Grassmann A, Gioberge S, Moeller S, Brown G. ESRD patients in 2004: global overview of patient numbers, treatment modalities and associated trends. Nephrol Dial Transplant. 2005;20:2587. doi: 10.1093/ndt/gfi159. [DOI] [PubMed] [Google Scholar]
- 12.Kowalczyk KJ, Hooper HB, Linehan WM, Pinto PA, Wood BJ, Bratslavsky G. Partial nephrectomy after previous radio frequency ablation: the National Cancer Institute experience. J Urol. 2009;182:2158. doi: 10.1016/j.juro.2009.07.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bratslavsky G, Linehan WM. Long-term management of bilateral, multifocal, recurrent renal carcinoma. Nat Rev Urol. 2010;7:267. doi: 10.1038/nrurol.2010.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carmichael P, Popoola J, John I, Stevens PE, Carmichael AR. Assessment of quality of life in a single centre dialysis population using the KDQOL-SF questionnaire. Qual Life Res. 2000;9:195. doi: 10.1023/a:1008933621829. [DOI] [PubMed] [Google Scholar]
- 15.Ginieri-Coccossis M, Theofilou P, Synodinou C, Tomaras V, Soldatos C. Quality of life, mental health and health beliefs in haemodialysis and peritoneal dialysis patients: investigating differences in early and later years of current treatment. BMC Nephrol. 2008;9:14. doi: 10.1186/1471-2369-9-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kimmel PL, Emont SL, Newmann JM, Danko H, Moss AH. ESRD patient quality of life: symptoms, spiritual beliefs, psychosocial factors, and ethnicity. Am J Kidney Dis. 2003;42:713. doi: 10.1016/s0272-6386(03)00907-7. [DOI] [PubMed] [Google Scholar]
- 17.Niu SF, Li IC. Quality of life of patients having renal replacement therapy. J Adv Nurs. 2005;51:15. doi: 10.1111/j.1365-2648.2005.03455.x. [DOI] [PubMed] [Google Scholar]
- 18.Patel SS, Shah VS, Peterson RA, Kimmel PL. Psychosocial variables, quality of life, and religious beliefs in ESRD patients treated with hemodialysis. Am J Kidney Dis. 2002;40:1013. doi: 10.1053/ajkd.2002.36336. [DOI] [PubMed] [Google Scholar]
- 19.Duffey BG, Choyke PL, Glenn G, Grubb RL, Venzon D, Linehan WM, et al. The relationship between renal tumor size and metastases in patients with von Hippel-Lindau disease. J Urol. 2004;172:63. doi: 10.1097/01.ju.0000132127.79974.3f. [DOI] [PubMed] [Google Scholar]