Abstract
Self-report studies suggest that patients with Bulimia Nervosa (BN) evidence difficulties with interoceptive awareness. Indeed, interoceptive deficits may persist after recovery of BN and may be a biological trait that predisposes symptom development in BN. However, no studies to date have directly assessed interoceptive sensitivity, or accuracy in detecting and perceiving internal body cues, in patients with or recovered from BN. Nine women who had recovered from BN and 10 healthy control women completed the Heart Beat Perception Task (HBPT) in which individuals were required to estimate the number of heartbeats between intervals of time. Accuracy scores were compared between groups. Significant differences were found between the groups on the HBPT ((F 1,19)= 7.78, p=.013, Cohen’s d= 1.16) when controlling for age. These results suggest that deficits in interoceptive sensitivity are present in individuals recovered from BN. Thus interoceptive deficits may be one factor that bridges the gap between brain dysfunction and symptom presentation in BN.
Keywords: Eating Disorders, Neurobiology, Physiology, Biological, Heart Beat Perception Task
1. Introduction
Bulimia nervosa (BN) is a serious psychiatric disorder that causes significant and costly medical problems. The financial costs associated with treating BN are high (Stuhldreher et al., 2012). BN also has one of the highest mortality rates of all psychiatric disorders, estimated to occur in 3.9% of cases (Crow, et al., 2009a; Crow., 2009b). Despite the fact that 1.5% of the population develops BN during his or her lifetime, mechanisms underlying symptom presentation in BN are poorly understood (Hudson, Hiripi, Pope & Kessler, 2007). Evidence for the effectiveness of treatment of BN is accumulating (Brown & Keel, 2012), however, it remains important to improve the understanding of the psychophysiology of BN. New research, for example, suggests that BN has biological and genetic components (Hinney, Scherag, & Hebebrand, 2010), however, little research has been conducted to better understand the role that biological processes play in the development and maintenance of symptoms in BN. More research in this area is clearly required in order to develop better treatments and prevention strategies.
Key symptoms that characterize BN are eating a large amount of food in a short period of time, the experience of a loss of control and the use of compensatory behaviors such as vomiting (Americal Psychiatric Association, 1994). Bruch was the first to suggest that such symptoms result from “disturbances in accuracy of perception or cognitive interpretation of stimuli arising from the body” (Bruch, 1962, p. 189). In the eating disorder field, these disturbances have been described as problems in interoceptive awareness (Garfinkel, Moldofsky, Garner, Stancer, & Coscina, 1978). Recently, interoceptive sensitivity has been studied and refers to “the ability to perceive consciously signals arising from the body” (Pollatos, Fustos & Critchley, 2012, p. 1680). Disturbances in detecting and/or interpreting stimuli from the body, particularly hunger and satiety cues, could directly contribute to the development and maintenance of symptoms such as restrictive eating, binging and purging in BN. Difficulties detecting and interpreting stimuli from the body could lead to misinterpretation of hunger and satiety cues. Binging and purging symptoms may reflect a difficulty in internally regulating misinterpreted hunger and satiety cues. Research on the neurobiological basis of interoception suggests that interoceptive processing occurs in several stages and follows a posterior to anterior physical progression in the insula cortex. Physiological cues involved in maintaining internal homeostasis are thought to be detected without conscious awareness in the posterior portion of the insula. Further, it has been suggested that interoceptive awareness occurs as these signals are processed into the anterior insula as an individual reflects upon his or her physical state (Craig, 2009).
Numerous studies exploring various biological aspects of BN suggest that possible interoceptive deficits are involved in the development and maintenance of BN. For example, several studies have demonstrated that the threshold for detecting body cues in BN is higher than in controls; therefore, those with BN appear to require more intense stimuli in order to detect a baseline level of stimulation. These studies suggest that interoceptive deficits may be present and have examined pain processing, hunger, satiety, sensitivity to gastric distention, and taste detection in BN (De Zwaan, Biener, Bach, Wiesnagrotzki & Stacher, 1996; Geliebter & Hashim, 2001; Kissileff et al., 1996; Lautenbacher, Pauls, Strian, Pirke, & Krieg, 1991; Papezova, Yamamotova & Uher, 2005; Rodin, Bartoshuk, Peterson, & Schank, 1990; Stein et al., 2003; Sunday & Halmi, 1990; Zimmerli, Walsh, Guss, Devlin, & Kissileff, 2006). Findings are consistent with neuroimaging studies in BN that have indicated decreased activation in both the posterior and anterior insula in those currently with BN (Bohon & Stice, 2011) and increased activation in the anterior insula in women recovered from BN (Obendorfer et al., 2013). Therefore, interoceptive processing deficits may be related to abnormal functioning in interoceptive neural networks.
Prior to this study, disturbances in interoception have been assessed in BN by a self-report measure (the Interoceptive Awareness scale on the Eating Disorder Inventory); results suggest that those with BN have lower scores than controls when measured by this subscale (Fassino, Piero, Gramaglia, & Abbate-Daga, 2004; Lilenfeld, Wonderlich, Riso, Crosby, & Mitchell, 2006; Pryor, Wiederman, & McGilley, 1996; Taylor, Parker, Bagby, & Bourke, 1996). However, to date, no studies have used an objective physiological measure to assess the biological aspects of interoception in BN, which is important for reliability and validity.
And, although there are proposed physiological processes that are related to disturbed interoception in BN, no studies to date have directly assessed interoceptive sensitivity in BN. The gold standard task for assessing interoception deficits, and specifically interoceptive sensitivity, is the Heart Beat Perception Task (HBPT). The HBPT assesses one’s accuracy in detecting and perceiving his or her heartbeats (Schandry, 1981). Individuals with anxiety disorders, particularly panic disorder, have shown increased accuracy in heartbeat detection whereas individuals with anorexia nervosa have demonstrated decreased accuracy in heartbeat detection (Domschke, Stevens, Pfleiderer, Gerlach 2005). In healthy adults, studies have shown that accurate performance on the HBPT task activated both posterior and anterior regions of the insula (Pollatos, Gramann, & Schandry, 2007; Pollatos et al., 2008; Wiens, 2005). Additionally, HBPT scores have been shown to correlate with right insula volume in healthy adults (Critchley, 2005). The HBPT can be considered to measure one’s ability to detect internal interoceptive stimuli without confounding by competing external stimuli such as in pain, gastric, and taste processing. In addition, the HBPT is simple to administer, and an EKG is the only piece of equipment needed to complete the task. This task can, therefore, be administered in clinical settings and in non-medical facility laboratories.
In this study, women recovered from BN nervosa (BN-R) were studied in order to control for the confounding effects of binge-purge symptoms. Physiological effects of active binging and purging include longer QTc intervals as measured on an EKG, changes in blood sugar levels, EEG abnormalities, abdominal and urinary disturbances, dental problems and inflammation of the esophagus (Peebles, Hardy, Wilson, & Lock, 2010). Physiological effects of active restricting, binging and purging, particularly EKG abnormalities, may confound one’s ability to detect and perceive his or her heart beat.
In order understand the biological traits that may lead to the development of BN, we chose to study interoceptive sensitivity using the HBPT in BN-R. Interoceptive sensitivity in BN is important to study since directly measuring the interoceptive sensitivity of non-food related body cues in BN could help elucidate whether disturbances in interoception are due to intentional repression of food related body cues or organic global interoceptive deficits. Such disturbances in detecting and/or interpreting stimuli from the body, particularly hunger and satiety cues, could directly contribute to the development and maintenance of symptoms such as restrictive eating, binging and purging in BN. Therefore, interoception is important to study. We hypothesized that BN-R would display deficits on the HBPT task relative to healthy control participants, therefore, suggesting that interoceptive sensitivity deficits are present after symptom resolution in BN.
2. Materials and Methods
2.1. Participants
Participants were women recovered from BN (BN-R; n = 9) and healthy control participants (HC; n = 10), between the ages 18 to 45 years. We chose to study only women as eating disorders among males are relatively rare (10%) and have atypical features (Mangweth-Matzek et al., 2010). BN-R were recruited nationally via postings on national eating disorder websites, treatment program websites, flyers distibuted at eating disorder conferences, and flyers sent to local eating disorder therapists as part of a larger fMRI study (data presented elsewhere). BN-R participants met a lifetime DSM–IV diagnosis of BN with no history of anorexia nervosa. The onset of their illness must have occurred at least 4 years prior to their participating in this study. This criteria was implemented in order to prevent the possible conversion from anorexia to BN, therefore, guaraneeing a diagnostically “pure” BN group. Participants were considered recovered if no eating disorder behaviors or symptoms were reported by the potential participant during a structured interview to be present within 12 months prior to the start of the study. Eating disorder behaviors included food restriction,any binging, or purging. Additionally, participants maintained a stable weight (± 3.0 kg) between 90% and 120% absolute body weight and had a regular menstral cycle within 12 months prior to the study. These criteria for recovery has been used to assess recovery in patients who previously met criteria for BN in other published studies by this research group (Frank et al., 2007). Healthy control women were recruited locally via posting distributed through out San Diego county and did not display current or previous psychopathology as determined by structured interviews (see below). Inclusion criteria for this group also included maintaining an absolute body weight between 90% and 120% of their ideal body weight since menarche and a lack of family members with an eating disorder history.
Exclusionary criteria for all participants included a) history of alcohol or substance abuse/dependence; b) any neurological/medical conditions; c) use of psychotropic medication within the three months prior to the study (participants were permitted to use birthcontrol and over the counter medications for minor pain and allergies); d) pregnancy. BN-R and healthy control participants were demographically matched on ethnicity. Participant demographics are presented in Table A.
Table A.
Sample Demographic/Clinical Data.
| Demographic |
BN-R
M (SD) |
Controls
M (SD) |
p |
|---|---|---|---|
| Average BMI | 21.86 (0.48) | 21.86 (0.56) | p>.05 |
| Lowest Lifetime BMI | 19.80 (1.25) | 21.8 (3.70) | p>.05 |
| Highest BMI | 24.89 (2.67) | 23.3 (2.14) | p>.05 |
| Age of Onset | 15.78 (2.05) | N/A | N/A |
| Average Years of Recovery |
8.08 (4.16) | N/A | N/A |
| Age | 30.00 (8.67) | 22.70 (2.11) | p=.02 |
| Percentage Caucasian | 67% | 80% | p>.05 |
| Percentage Asian | 33% | 20% | p>.05 |
2.2. Procedures
The study was approved by the University of California, San Diego Institutional Review Board and informed consent was obtained from all participants. Participants completed a brief phone screen that was administered by a trained research associate. If initial criteria were met, participants were administered the Structured Clinical Interview for the DSM-IV (SCID; First, Spitzer, Gibbon, Williams, 2002), Module H of the SCID (First, Spitzer, Gibbon, Williams, 2002), the Yale Brown Obsessive Compulsive Scale (YBOCS; Goodman et al., 1989) and the Yale Brown Cornell Eating Disorder Scale (YBC-EDS; Mazure, Halmi, Sunday, Romano & Einhorn, 1994) by either a psychiatrist or psychologist who received formal training in administering the aforementioned interviews. Participants completed a medical lab screening (which included an EKG) and if deemed medically stable, they were included in the study. Participant’s height and weight was measured and current BMI was calculated. Additionally, participants were asked to report one’s lowest lifetime BMI and highest lifetime BMI.
The HBPT was given in the morning immediately after participants finished a standardized breakfast. This task was completed at the University of California, San Diego Keck Imaging Center prior to participating in an fMRI study. Prior to completing the HBPT, sitting blood pressure was obtained. During the HBPT, the participants’ physiological responses (EKG, and respirations) were monitored through J&J Technology’s 12-lead C2 I-330 physiological monitoring system. The I-330 C2 uses a two-lead EKG and has a sampling rate of 1024 Hz, which is well above the minimal sampling rate suggested in research studies (Heilman & Porges, 2007). A trained research assistant placed and removed the appropriate leads on study participants.
Participants were instructed to sit away from the back of their chairs and to place their hands in their lap while resting for ten-minutes prior to being administered the Schandry version of the HBPT. Average sitting heart and breathing rate were calculated during the ten-minute baseline period. A computer equipped with E-Prime software was used to indicate when the participants would start and stop counting heart beats. Standardized verbal instructions were given to each participant by a trained research assistant and were displayed on the computer screen. The computer program provided a start and stop tone for four time intervals (25s, 35s, 45s and 100s) and verbal instructions to silently count heart beats. When each time interval was completed, the participant verbally reported how many heart beats were counted during that interval. This number was recorded by the research assistant. The participant was not given feedback regarding her performance or the length of the time intervals.
3. Calculation
Accuracy rates on the HBT were computed using the modified Schandry methods (Ehlers & Breuer, 1992). A proportion score was computed by assessing the mean of four heartbeat perception intervals according to the following transformation: ¼ Σ(1- (∣recorded heart beats-counted heart beats∣)/recorded heartbeats). Computed by this method, scores range between 0 and 1, with higher scores indicating higher accuracy. Average breathing rate, sitting and standing heart rates and blood pressures were also calculated.
Statistical analyses were conducted using SPSS 15.0. Alpha level was set at .05 for all analyses. Differences on demographic variables were calculated using independent t-tests. Significant differences were present between groups on age; therefore, age was entered into the analyses as a covariate. The mean accuracy scores on the HBPT were analyzed by a one-way between groups ANCOVA. A one-way between group MANCOVA was used in order to assess differences between BN-R and controls on sitting and standing blood pressures, respiration and heart rates.
4. Results
Groups did not differ significantly on ethnicity, BMI, lowest lifetime BMI, and highest lifetime BMI (See Table A.). However, significant differences occurred between groups on age (see Table A; (F 1,19)= 6.70, p =.02)). The age range in the BN-R group was 21-44 years of age; two participants were 44 years old, however the remaining seven participants had an average age of 26. The age range in the control group fell between 21 and 27 years of age; the average age was 22.70. BN-R had an average of 8.08 years of recovery; standard deviation (SD) = 4.16 (See Table A.).
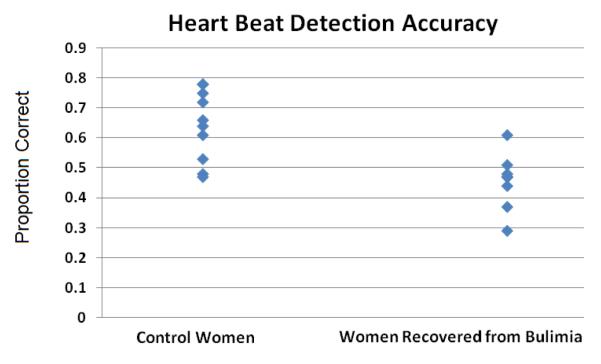
Figure A. shows the accuracy data on the HBPT plotted by group. As hypothesized, BNR were significantly less accurate on the HBPT relative to control women. The mean proportion correct in the BN-R group was .46 (SD = .09); the mean proportion correct in the control group was .64 (SD = .12) (F1,19)= 14.629, p =.001, Cohen’s d= 1.74. Additionally, scores on the HBPT were negatively correlated with age across both groups (Mean age for controls = 22.7 and BNR= 30.0 (Pearson’s r (19) = −.479, p = .038)). As a result, age was entered in as a covariate into the analyses; the results remained significant (F1,19) = 7.78, p =.013, Cohen’s d =1.16. No between group differences on sitting heart rate, blood pressure, and respiration rate were found (See Table B). Study results are important since this is the first study to assess and detect significant differences between BN-R and health controls on the HBPT. Results suggest poor performance on the HBPT in BN-R.
Figure A.
Mean proportion correct in healthy control females and females recovered from Bulimia Nervosa on the Heart Beat Perception Task.
Table B.
Group Mean Scores on Physiological Data.
| Variable |
BN-R
M (SD) |
Controls
M (SD) |
p |
|---|---|---|---|
| Respiration | 13.9 (5.4) | 12.1(3.3) | p >.05 |
| Sitting Heart Rate | 77 (10.5) | 71 (11.4) | p >.05 |
| Sitting Blood Pressure | 111/72 | 107/68 | p >.05 |
5. Discussion
As hypothesized, significantly lower accuracy scores were found in BN-R group on the HBPT indicating that individuals recovered from BN have difficulty detecting and perceiving heartbeats when compared to controls (See Figure A.). Additionally, there were no differences between the groups on respiration, sitting blood pressure, and sitting heart rate, suggesting that HBPT differences are not due to differences between groups on autonomic function (See Table B.). These findings are consistent with previous physiological studies that have suggested that those with BN may struggle to detect various body cues (De Zwaan, et al., 1996; Geliebter & Hashim, 2001; Kissileff, et al., 1996; Lautenbacher, et al., 1991; Papezova, et al., 2005; Rodin, et al., 1990; Stein, et al., 2003; Sunday & Halmi, 1990; Zimmerli, et al., 2006). Results from this study, when coupled with previous research, suggest a global interoceptive processing deficit in those recovered from BN. Our findings suggest that interoception deficits, as assessed via the HBPT, are present after recovery. Therefore, interoceptive deficits could either be a biological trait that is present prior to the development of symptoms in BN or a consequence of having had BN. The presence of interoception deficits are supported by imaging studies that identify insular abnormalities in BN (Obendorfer et al., 2013). Irregular patterns of activation have been seen in the anterior and posterior insula, a structure that is critically involved in monitoring and modulating the physiological condition of the body, when women with BN were given interoceptive taste stimuli (Bohon & Stice, 2011).
Additionally, the HBPT demonstrates increased interoceptive sensitivity in children and adults with anxiety disorders (Domschke et al., 2009) and decreased sensitivity in anorexia nervosa (Pollatos et al. 2008). Results from this study suggest that deficits in interoceptive sensitivity, as evidenced by a low accuracy on the HBPT may differentiate eating disorders from other psychiatric disorders.
5.1. Limitations
The sample size was relatively small, which is common in initial studies examining diagnostically “pure” groups. And, diagnostically pure BN-R and control participants are rare and, therefore, difficult to recruit. However, given the diagnostic purity of the BN-R groups, it is not surprising that this sample size would yield significant differences between groups. Additionally, the large effect size detected on the primary aim suggests that significant differences between BN-R and control groups would be present in a larger sample. Nonetheless, replication of this study using more participants is needed.
Another study weakness was that controls who did not have any current or previous psychiatric diagnoses were used in the study. Some studies suggest that using control samples without any psychiatric comorbidity may lead towards significance found between groups (Klump et al., 2004), thus a more representative community sample should be used in further studies that assess interoception in BN. The control group used in this study demonstrated somewhat low HBPT accuracy scores when compared to control participants in other studies (Mean = .77, SD= .09; Pollastos, 2007). Some psychiatric disorders, such as anxiety disorders, have demonstrated increased scores on the HBPT (Domschke et al., 2010). Therefore, control groups that exclude previous or current psychiatric diagnoses may have different scores on the HBPT than control groups that permitted previous psychiatry history. Indeed, significance between groups was still found despite having lower than typical accuracy scores.
An additional weakness was the fact that the two groups were not matched on age. Research has suggested that interoceptive sensitivity is negatively correlated with age (Khalsa, Rudrauf and Tranel, 2009). Therefore, future studies assessing interoception in BN should recruit groups that are equal in age.
5.2. Study Implications and Future Directions
This is the first study to directly assess interoceptive sensitivity in BN. Results from this study suggest that there is poor interoceptive sensitivity in BN. Deficits in interoceptive sensitivity may play a role in the development and maintenance of symptoms found in BN such as the binge purge cycle. Interoceptive deficits could underlie disturbed hunger and satiety in BN and thus could contribute directly to binging symptoms. Those who develop BN may have difficulty perceiving hunger cues and therefore could easily skip meals and restrict food intake until feeling intense hunger, which then becomes difficult to control. Also difficulty detecting normal levels of fullness could cause overeating in those with BN. As a result, interoception may play a significant role in the presence and reoccurrence of symptoms in BN and thus is important for continued study.
Future studies in the area of interoceptive processing in BN are needed. It is important to assess whether interoceptive deficits can or cannot be changed in BN in addition to assessing whether future treatments should focus on improving interoceptive deficits or should focus on teaching patients how to compensate for interoceptive disturbance. Additionally, if interoceptive improvement is directly related to changes in symptoms in BN, then direct measures of interoceptive sensitivity such as the HBPT could be a helpful and precise measure of treatment efficacy. A better understanding of interoceptive sensitivity deficits in BN may inform the development of more precise eating disorder treatments and new objective measures of treatment efficacy.
6. Conclusions
Overall, this study is significant since it provides valuable information about interoceptive sensitivity in individuals recovered from BN. Results suggest that individuals recovered from BN have significant deficits in interoceptive sensitivity as determined by low accuracy scores on the HBPT compared to healthy controls. Deficits in interoceptive sensitivity may explain binging symptoms seen in BN. As a result, this study justifies conducting additional research on interoceptive processing in BN.
Highlights.
We examined interoceptive sensitivity in females recovered from bulimia nervosa and controls.
The Schandry version of the Heart Beat Perception task assessed interoceptive sensitivity.
Women recovered from bulimia have significant deficits in interoceptive sensitivity.
Acknowledgements
The authors graciously acknowledge the assistance in this project by the following people: Lauren Kipp, Angela Robertson and Sarah Lamb. The authors also thank Drs. Victor Carrion and Scott Hall for their comments on an earlier version of the manuscript.
Statement 1: Role of Funding Source Funding for this study was provided a National Institute of Mental Health grant (5U01MH76286; WHK). The NIMH had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Statement 2: Contributors Dr. Klabunde designed and conducted the study, undertook the statistical analyses and wrote the majority of the manuscript. Dr. Acheson assisted with several components of the manuscript and provided conceptual feedback about the study design. Dr. Boutelle provided statistical consult and contributed to the discussion section of the manuscript. Dr. Matthews provided conceptual feedback about the study design and contributed to the literature review. Dr. Kaye provided consult throughout the study design, implementation and manuscript preparation. All authors contributed to and have approved the final manuscript.
Statement 3: Conflict of Interest There are no conflicts of interest by any of the authors.
References
- American Psychiatric Association, A. P. Diagnostic and statistical manual of mental disorders. 4th - TR ed American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- Bohon C, Stice E. Negative affect and neural response to palatable food intake in bulimia nervosa. Appetite. 2012;58:964–970. doi: 10.1016/j.appet.2012.02.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TA, Keel PK. Current and emerging directions in the treatment of eating disorders. Substance Abuse Research and Treatment. 2012;6:33–61. doi: 10.4137/SART.S7864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruch H. Perceptual and conceptual disturbances in anorexia nervosa. Psychosomatic Medicine. 1962;24:187–194. doi: 10.1097/00006842-196203000-00009. [DOI] [PubMed] [Google Scholar]
- Craig AD. How do you feel — now? The anterior insula and human awareness. Neuroscience. 2009;10:59–70. doi: 10.1038/nrn2555. [DOI] [PubMed] [Google Scholar]
- Critchley HD. Neural mechanisms of autonomic, affective, and cognitive integration. Journal of Comparative Neurology. 2005;493:154–166. doi: 10.1002/cne.20749. [DOI] [PubMed] [Google Scholar]
- Crow SJ, Frisch MJ, Peterson CB, Croll J, Raatz SK, Nyman JA. Monetary costs associated with bulimia. International Journal of Eating Disorders. 2009;42:81–83. doi: 10.1002/eat.20581. [DOI] [PubMed] [Google Scholar]
- Crow SJ, Peterson CB, Swanson SA, Raymond NC, Specker S, Eckert ED, Mitchell JE. Increased mortality in bulimia nervosa and other eating disorders. American Journal of Psychiatry. 2009;166:1342–1346. doi: 10.1176/appi.ajp.2009.09020247. [DOI] [PubMed] [Google Scholar]
- De Zwaan M, Biener D, Bach M, Wiesnagrotzki S, Stacher G. Pain sensitivity, alexithymia, and depression in patients with eating disorders: are they related? Journal of Psychosomatic Research. 1996;41:65–70. doi: 10.1016/0022-3999(96)00088-8. [DOI] [PubMed] [Google Scholar]
- Domschke K, Stevens S, Pfleiderer B, Gerlach A:L. Interoceptive sensitivity in anxiety and anxiety disorders: an overview and integration of neurobiological findings. Clinical Psychology Review. 2010;30:1–11. doi: 10.1016/j.cpr.2009.08.008. [DOI] [PubMed] [Google Scholar]
- Ehlers A, Breuer P. Increased cardiac awareness in panic disorder. Journal of Abnormal Psychology. 1992;101:371–382. doi: 10.1037//0021-843x.101.3.371. [DOI] [PubMed] [Google Scholar]
- Fassino S, Piero A, Gramaglia C, Abbate-Daga G. Clinical, psychopathological and personality correlates of interoceptive awareness in anorexia nervosa, bulimia nervosa and obesity. Psychopathology. 2004;37(4):168–174. doi: 10.1159/000079420. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition (SCIDI/P) Biometrics Research, New York State Psychiatric Institute; New York: 2002. [Google Scholar]
- Frank G, Bailer UF, Meltzer CC, Price JC, Mathis CA, Wagner A, Becker C, Kaye WH. Regional cerebral blood flow after recovery from anorexia or bulimia nervosa. International Journal of Eating Disorders. 2007;40(6):488–92. doi: 10.1002/eat.20395. [DOI] [PubMed] [Google Scholar]
- Garfinkel PE, Moldofsky H, Garner DM, Stancer HC, Coscina DV. Body awareness in anorexia nervosa: disturbances in “body image” and “satiety”. Psychosomatic Medicine. 1978;40:487–498. doi: 10.1097/00006842-197810000-00004. [DOI] [PubMed] [Google Scholar]
- Geliebter A, Hashim SA. Gastric capacity in normal, obese, and bulimic women. Physiology & Behavior. 2001;74:743–746. doi: 10.1016/s0031-9384(01)00619-9. [DOI] [PubMed] [Google Scholar]
- Goodman WK, Price L, Rasmussen SA, Mazure C, Fleischman RL, Hill CL, Heninger GR, Charney DS. The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Archives of General Psychiatry. 1989;46:1006–1011. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- Heilman KJ, Porges SW. Accuracy of the LifeShirt (Vivometrics) in the detection of cardiac rhythms. Biological Psychology. 2007;75:300–305. doi: 10.1016/j.biopsycho.2007.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinney A, Scherag S, Hebebrand J. Genetic findings in anorexia and bulimia nervosa. Progress in Molecular Biology and Translational Science. 2010;94:241–270. doi: 10.1016/B978-0-12-375003-7.00009-1. [DOI] [PubMed] [Google Scholar]
- Hudson JI, Hiripi E, Pope HG, Jr., Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biological Psychiatry. 2007;61:348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kissileff HR, Wentzlaff TH, Guss JL, Walsh BT, Devlin MJ, Thornton JC. A direct measure of satiety disturbance in patients with bulimia nervosa. Physiology &Behavior. 1996;60:1077–1085. doi: 10.1016/0031-9384(96)00086-8. [DOI] [PubMed] [Google Scholar]
- Lautenbacher S, Pauls AM, Strian F, Pirke KM, Krieg JC. Pain sensitivity in anorexia nervosa and bulimia nervosa. Biological Psychiatry. 1991;29:1073–1078. doi: 10.1016/0006-3223(91)90249-l. [DOI] [PubMed] [Google Scholar]
- Lilenfeld LR, Wonderlich S, Riso LP, Crosby R, Mitchell J. Eating disorders and personality: a methodological and empirical review. Clin Psychol Rev. 2006;26(3):299–320. doi: 10.1016/j.cpr.2005.10.003. [DOI] [PubMed] [Google Scholar]
- Mangweth-Matzek B, Rupp CI, Hausmann A, Gusmerotti S, Kemmler G, Biebl W. Eating disorders in men: current features and childhood factors. Eating and Weight Disorders. 2010;15:15–22. doi: 10.1007/BF03325276. [DOI] [PubMed] [Google Scholar]
- Mazure C, M., Halmi KA, Sunday SR, Romano SJ, Einhorn AM. The Yale-Brown-Cornell Eating Disorder Scale: development, use, reliability and validity. Journal of Psychiatric Research. 1994;28:424–445. doi: 10.1016/0022-3956(94)90002-7. [DOI] [PubMed] [Google Scholar]
- Oberndorfer T, Frank G, Simmons A, Wagner A, McCurdy D, Fudge JL, Yang T, Paulus MP, Kaye W. Altered Insula Response to Sweet Taste Processing After Recovery from Anorexia and Bulimia Nervosa. American Journal of Psychiatry. 2013 doi: 10.1176/appi.ajp.2013.11111745. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papezova H, Yamamotova A, Uher R. Elevated pain threshold in eating disorders: physiological and psychological factors. Journal of Psychiatric Research. 2005;39:431–438. doi: 10.1016/j.jpsychires.2004.10.006. [DOI] [PubMed] [Google Scholar]
- Peebles R, Hardy KK, Wilson JL, Lock JD. Are diagnostic criteria for eating disorders markers of medical severity? Pediatrics. 2010;125:1193–1201. doi: 10.1542/peds.2008-1777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollatos O, Fustos J, Critchley HD. On the generalised embodiment of pain: how interoceptive sensitivity modulates cutaneous pain perception. Pain. 2012;153:1680–1686. doi: 10.1016/j.pain.2012.04.030. [DOI] [PubMed] [Google Scholar]
- Pollatos O, Gramann K, Schandry R. Neural systems connecting interoceptive awareness and feelings. Human brain mapping. 2007;28:9–18. doi: 10.1002/hbm.20258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollatos O, Kurz A, Albrecht J, Schreder T, Kleemann AM, Schopf V, Kopletz R, Wisemann M, Schandry R. Reduced Perception of Bodily Signals in Anorexia Nervosa. Eating Behaviors. 2008;2:001–008. doi: 10.1016/j.eatbeh.2008.02.001. [DOI] [PubMed] [Google Scholar]
- Pryor T, Wiederman MW, McGilley B. Laxative abuse among women with eating disorders: an indication of psychopathology? Int J Eat Disord. 1996;20(1):13–18. doi: 10.1002/(SICI)1098-108X(199607)20:1<13::AID-EAT2>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- Rodin J, Bartoshuk L, Peterson C, Schank D. Bulimia and taste: possible interactions. Journal of Abnormal Psychology. 1990;99:32–39. doi: 10.1037//0021-843x.99.1.32. [DOI] [PubMed] [Google Scholar]
- Schandry R. Heart beat perception and emotional experience. Psychophysiology. 1981;18:483–488. doi: 10.1111/j.1469-8986.1981.tb02486.x. [DOI] [PubMed] [Google Scholar]
- Stein D, Kaye WH, Matsunaga H, Myers D, Orbach I, Har-Even D, Frank G, Rao R. Pain perception in recovered bulimia patients. International Journal of Eating Disorders. 2003;34:331–336. doi: 10.1002/eat.10164. [DOI] [PubMed] [Google Scholar]
- Stuhldreher N, Konnopka A, Wild B, Herzog W, Zipfel S, Lowe B, Konig HH. Cost-of-illness studies and cost-effectiveness analyses in eating disorders: a systematic review. The International Journal of Eating Disorders. 2012;45:476–491. doi: 10.1002/eat.20977. [DOI] [PubMed] [Google Scholar]
- Sunday SR, Halmi KA. Taste perceptions and hedonics in eating disorders. Physiology & Behavior. 1990;48:587–594. doi: 10.1016/0031-9384(90)90196-b. [DOI] [PubMed] [Google Scholar]
- Taylor GJ, Parker JD, Bagby RM, Bourke MP. Relationships between alexithymia and psychological characteristics associated with eating disorders. J Psychosom Res. 1996;41(6):561–568. doi: 10.1016/s0022-3999(96)00224-3. [DOI] [PubMed] [Google Scholar]
- Wiens S. Interoception in emotional experience. Current Opinion in Neurology. 2005;18:442–447. doi: 10.1097/01.wco.0000168079.92106.99. [DOI] [PubMed] [Google Scholar]
- Zimmerli EJ, Walsh BT, Guss JL, Devlin MJ, Kissileff HR. Gastric compliance inbulimia nervosa. Physiology & Behavior. 2006;87:441–446. doi: 10.1016/j.physbeh.2005.11.010. [DOI] [PubMed] [Google Scholar]