Abstract
Objective
The goal of this study was to examine the clinical utility of nibbling behavior, defined as eating in an unplanned and repetitious manner between meals and snacks without a sense of loss of control, in obese patients with binge eating disorder (BED).
Methods
Two-hundred seventeen (N=217) consecutive, treatment-seeking, obese patients with BED were assessed with the Eating Disorder Examination (EDE). Nibbling frequency was examined in relation to current weight, eating disorder psychopathology and eating patterns.
Results
Results found that nibbling/picking was not related to body mass index, objective bulimic, subjective bulimic, or overeating episodes, food avoidance, sensitivity to weight gain, or any subscales of the EDE. However, nibbling/picking was significantly related to frequency of morning and afternoon snacking (r = .21, p = .002; r = .27, p < .001).
Discussion
The assessment of nibbling/picking behaviors among individuals with BED might not provide clinically significant information.
Keywords: Nibbling, Picking, Binge Eating Disorder, Eating Behaviors
1. Introduction
Binge Eating Disorder (BED) is characterized by recurrent binge eating, defined as eating an unusually large amount of food while experiencing a subjective sense of loss of control, marked distress, and not engaging in compensatory behaviors characteristic of bulimia nervosa (APA, 1994). It is recognized as an important clinical problem associated with high levels of eating disorder psychopathology, psychological distress and medical comorbidity, (Hudson et al., 2007; Allison et al., 2005) and is especially common among obese persons who seek weight loss treatment. Eating disorders, including BED, are frequently assessed using the Eating Disorder Examination (EDE), (Fairburn et al., 2008) a semi-structured interview that ascertains information about eating pathology and eating disorder diagnoses.
The most recent version of the EDE (v. 16) includes the addition of an item to assess nibbling (or picking). Based on the EDE definition, nibbling episodes are characterized by eating in an unplanned, repetitious manner between meals and snacks without feeling a loss of control. Nibbling/picking in this paper is distinguished from a related term known as “grazing.” Carter and Jansen (2012) define grazing as “the repeated consumption of smaller amounts of food over an extended period of time,” but point out that researchers have differed in whether grazing includes feelings of loss of control. It remains unclear whether nibbling is a problematic eating behavior and if its assessment provides useful clinical information. One study by de Zwaan and colleagues (2010) found that among 59 morbidly obese patients receiving gastric bypass surgery, 32% reported nibbling, but no relationship between nibbling and the presence of eating disorders prior to surgery or between nibbling and post-surgery weight loss was detected. In addition, Reas et al., (2012) examined nibbling behaviors among a normative sample of 58 adult young adult women. While they found that the majority of the sample reported engaging in some nibbling in the 28 days prior to the interview (91%), this behavior was not associated with BMI, frequency of meal or snack consumption, objective bulimic episodes, compensatory behaviors or any of the four EDE subscales. The study did reveal that engaging in more frequent nibbling was related to less avoidance of specific foods and less sensitivity to weight gain over a period of one week.
Given the paucity of research on nibbling, despite its inclusion in the EDE v. 16, the present study aimed to build on existing work by examining the frequency and relationship of nibbling to BMI, objective and subjective bulimic episodes, meal and snack patterns, and eating disorder psychopathology among obese, treatment-seeking individuals with BED.
2. Material and Methods
2.1. Participants
Participants were 217 consecutively evaluated, treatment-seeking obese individuals who met full DSM-IV research diagnostic criteria for BED. Individuals were recruited via newspaper advertisements seeking obese men and women who binge eat for treatment studies at a medical school-based specialty clinic. Participants were aged 21 to 65 years (M = 47.5, SD = 8.5), 72.8% (n = 158) were female, 78.8% (n = 171) were Caucasian, 14.7% (n = 32) were Black/African-American, 3.2% (n = 7) were Hispanic, and 3.2% (n = 7) self-described as “Other.” Mean BMI was 39.5 (SD = 6.3) kg/m2 and ranged from 29.0 to 55.5 kg/m2. Educationally, 81.1% (n = 176) reported at least some college.
2.2 Assessment
The study received full review and approval by the Yale institutional review board and all participants provided informed-written consents. Assessment procedures were performed by trained doctoral-level research-clinicians. BED diagnosis was based on the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I/P) (First et al., 1996) and confirmed with the Eating Disorder Examination interview (EDE) (Fairburn et al., 2008). Participants’ ages were obtained and heights and weights were measured at the initial assessment appointment. A frequency distribution and correlation analysis was performed using SPSS 19. Given the large number of statistical tests performed, a Bonferroni corrected alpha level of 0.003 was used as the threshold for statistical significance for correlations between nibbling/picking and relevant clinical variables. All tests were two-tailed.
2.3 Measures
Eating Disorder Examination (EDE 16.0D) (Fairburn et al., 2008). The EDE is a well-established and reliable investigator-based interview method for assessing eating disorder diagnoses and related symptomatology in BED. (Grilo et al., 2001; 2004). The EDE assesses different forms of overeating, including objective bulimic episodes (OBEs; binge eating defined as consuming unusually large quantities of food with a subjective sense of loss of control), objective overeating episodes (OOEs; unusually large quantities of food without a subjective sense of loss of control) and subjective bulimic episodes (SBEs; subjective sense of loss of control but a normal or small amount of food). In addition, the EDE assesses the frequency of nibbling/picking and meals and snacks consumed. The EDE also generates four subscales (dietary restraint (α = .60), eating concern (α = .63), weight concern (α = .59) and shape concern (α = .71)) and a global total score that reflect eating disorder psychopathology (α = .78).
The food avoidance and sensitivity to weight gain items on the EDE were also examined as outcomes, as was done in the Reas et al. (2012), study. The EDE food avoidance item states, “Over the past four weeks have you tried to avoid eating any foods which you like, whether or not you have succeeded?” and is rated on a frequency scale for the past 28 days. The sensitivity to weight gain item states, “Over the past four weeks what amount of weight gain, over a period of one week, would have definitely upset you?” and is rated on a 7-point severity scale.
3. Results
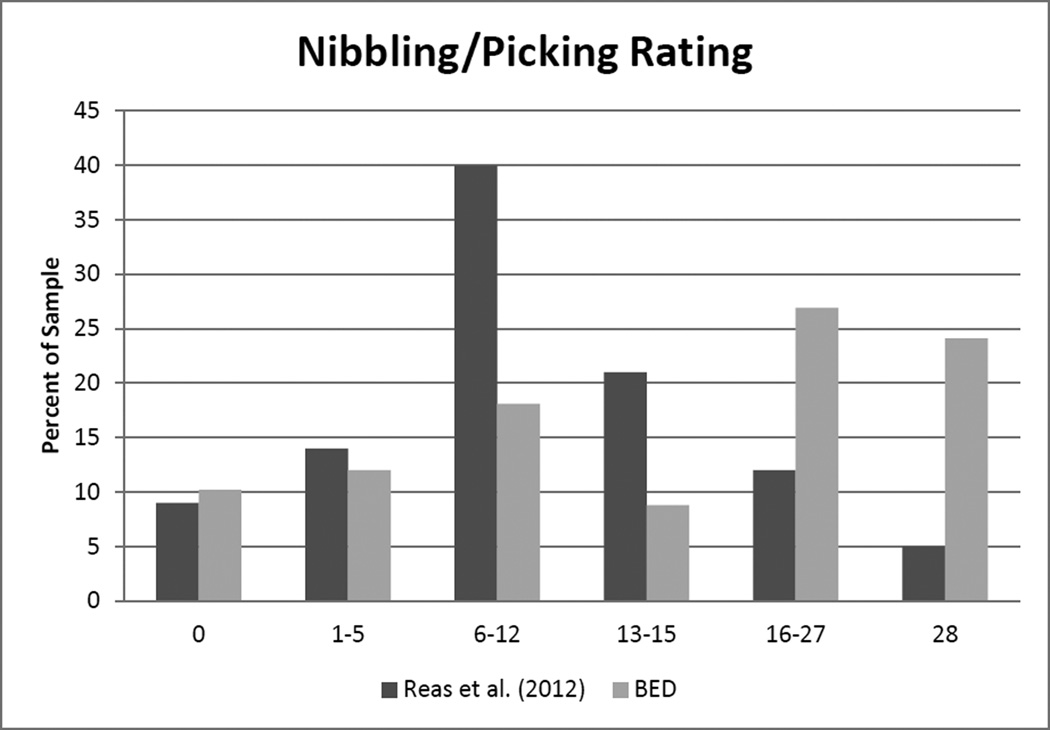
Daily nibbling/ picking was reported by 24.1%, and no nibbling/picking was reported by 10.2%, of the sample during the preceeding 28 days. 12% reported nibbling on 1 to 5 days, 18.1% on 6 to 12 days, 8.8% on 13 to 15 days, and 26.9 % on 16–27 days. Figure 1 depicts these percentages compared to those reported by Reas et al. (2012) in a sample of university women. As expected, the clinical sample of BED patients, reported more frequent nibbling episodes. A correlation analysis for nibbling/picking and relevant clinical variables is presented in Table 1. Nibbling/picking was not related to BMI; objective bulimic, subjective bulimic or overeating episodes, or; any subscales of the EDE. However, nibbling/picking was significantly related to morning and afternoon snacking (r = .21, p = .002; r = .27, p < .001). In contrast to Reas et al., no significant relationships were found between nibbling/picking and food avoidance (r = .05, p = .483) or sensitivity to weight gain (r = .01, p = .855). There was no significant relationship between nibbling/picking and age (r = .064, p = .350) or gender (F(1,214) = 1.215, p = .272).
Figure 1.
Percent of a clinical BED sample who reported days with nibbling/picking compared to a university women sample reported by Reas et al. 2012.
Table 1.
Correlation Table of Nibbling and Relevant Clinical Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Nibbling/Picking | 1.0 | ||||||||||||||||
| 2 | Body Mass Index | −0.1 | 1.0 | |||||||||||||||
| Monthly Meal & Snack Frequency (Days) | ||||||||||||||||||
| 3 | Breakfast | −0.01 | −0.08 | 1.0 | ||||||||||||||
| 4 | Mid-morning Snack | .21§ | 0.05 | 0.01 | 1.0 | |||||||||||||
| 5 | Lunch | 0.09 | −0.07 | .19** | .16* | 1.0 | ||||||||||||
| 6 | Mid-afternoon Snack | .27§ | −0.05 | 0.10 | .34** | 0.09 | 1.0 | |||||||||||
| 7 | Evening Meal | −0.02 | 0.07 | 0.04 | 0.00 | 0.08 | −0.05 | 1.0 | ||||||||||
| 8 | Evening Snack | 0.10 | −0.05 | −0.08 | 0.13 | 0.08 | .14* | 0.11 | 1.0 | |||||||||
| 9 | Nocturnal Eating | 0.16 | 0.07 | −0.06 | 0.11 | −0.1 | .15* | −0.02 | .21** | 1.0 | ||||||||
| Monthly Eating Episodes | ||||||||||||||||||
| 10 | Objective Bulimic Episodes | 0.16 | 0.03 | 0.13 | 0.02 | 0.02 | .16* | 0.02 | .15* | .29** | 1.0 | |||||||
| 11 | Subjective Bulimic Episodes | 0.1 | 0.04 | 0.02 | 0.11 | −.18** | 0.11 | 0.02 | 0.11 | .22** | 0.02 | 1.0 | ||||||
| Eating Disorder Examination Subscales | ||||||||||||||||||
| 12 | Eating Concern | 0.17 | 0.05 | 0.07 | .27** | 0.05 | .21** | −0.04 | 0.13 | 0.12 | 0.1 | .31** | 1.0 | |||||
| 13 | Weight Concern | 0.07 | 0.06 | 0.06 | 0.12 | −0.06 | 0.12 | −0.02 | 0.11 | .15* | 0.12 | .15* | .51** | 1.0 | ||||
| 14 | Shape Concern | 0.1 | 0.03 | 0.04 | 0.12 | −0.08 | .15* | 0.00 | 0.1 | .17* | .17* | .25** | .59** | .79** | 1.0 | |||
| 15 | Restraint | −0.02 | −0.1 | −0.02 | −0.03 | −0.08 | 0.02 | −0.03 | −0.01 | 0.05 | −0.03 | 0.10 | .19** | .31** | .28** | 1.0 | ||
| 16 | Food Avoidance | 0.05 | −.01 | −.05 | −.08 | −.08 | −.03 | −.06 | −.04 | −.03 | −.03 | 0.07 | .16* | .27** | .21** | .84** | 1 | |
| 17 | Sensitivity to Weight Gain | 0.01 | −.12 | −.06 | .07 | −.11 | .08 | −.04 | .01 | .05 | .04 | −.06 | .11 | .20** | .17* | .20** | .18* | 1 |
Correlation is significant at the 0.01 level (2-tailed).
Correlation is significant at the 0.05 level (2-tailed).
Correlation for Nibbling/Picking is significant at the <0.003 level based on a Bonferroni corrected alpha level
4. Discussion
The results from this study revealed that the majority of individuals with BED (90%) in this treatment-seeking sample engaged in nibbling behavior. Furthermore, 24.1% of the patients in this study reported nibbling every day, while Reas and colleagues found that only 5% of a non-clinical, young adult sample reported daily nibbling. Although many of the participants with BED were engaging in frequent nibbling and increased nibbling was associated with more frequent consumption of morning and afternoon snacks, it was not associated with participants’ BMI, overeating or binge eating frequency or eating disorder psychopathology. These findings are consistent with a study that assessed nibbling among a community sample of 69 individuals who were classified as having BED based on the EDE self-report questionnaire, where no relationships between bulimic episodes or restraint scores and nibbling were detected (Masheb et al., 2011). Unlike the Reas et al. (2012) study, which found a small, negative relationship between nibbling/picking and food avoidance (r = −.273, p = .038) and sensitivity to weight gain (r = −.266, p = .044), no relationship was observed in this sample. It is plausible that normal weight individuals without eating disorders who have less sensitivity to weight gain and food avoidance would be more likely to engage in nibbling/picking episodes. In contrast, individuals with BED might infrequently engage in food avoidance behaviors, explaining the lack of a relationship with nibbling/picking.
Several limitations of this research must be considered. First, this study is limited by the exploratory nature of the analyses, which were undertaken as hypothesis generating, due to the dearth of research on nibbling. In addition, the association between nibbling behavior and other clinical indicators, including treatment response, were not examined thus, limiting the ability to draw conclusions about the clinical significance of nibbling. The EDE also relies on retrospective recall of eating behaviors over the last 28 days, which are subject to measurement error, especially given evidence that obese individuals underestimate food intake (Buhl et al., 1995; Lichtman et al., 1992). In addition, nibbling was only measured over a 28-day time period in the current study, but it is possible that longer-term patterns of nibbling might be clinically significant for individuals with BED. While the EDE does not distinguish between potentially problematic and non-problematic nibbling, the current EDE definition of nibbling/picking excludes episodes characterized by feelings of loss of control. However, there might be some eating occasions where people engage in unplanned, repetitious eating (“nibbling”), while experiencing a loss of control. Currently, these kinds of episodes would be classified by the EDE as subjective bulimic episodes (SBE), but there might be a distinction between an isolated SBE and repetitious eating (“nibbling/picking”) accompanied by a loss of control. This is an important area for future research given studies that have revealed that feelings of loss of control during eating episodes in general, are associated with greater psychopathology (Latner, Hildebrandt, Rosewall, Chisholm, & Hayashi, 2007; Colles, Dixon, & O’Brien, 2008; Mond et al., 2010; Jenkins, Conley, Rienecke Hoste, Meyer, & Blissett, 2012). The present study was also correlational in nature and did not include a non-BED comparison group. Finally, the sample was largely Caucasian and female and participants were treatment seeking. Therefore, the findings might not generalize well to non-treatment seeking individuals and more diverse groups.
Despite these limitations, the current study is strengthened by a large sample of obese, treatment-seeking individuals with BED who completed the EDE in person. The results from this study extend conclusions made by Reas et al., who argued that nibbling falls outside the realm of pathological eating behaviors. Although that study was based on a normative sample, the findings from the current study in combination with previous work suggest that the assessment of nibbling/picking behaviors might provide little clinical utility and its inclusion in standard eating disorder assessments might not be warranted. However, future research should examine patterns of nibbling/picking over a longer time period, evaluate its relationship to treatment outcome, and determine whether nibbling/picking episodes are ever accompanied by a loss of control, and if so, whether meaningful distinctions between SBE and nibbling/picking episodes can be made.
Highlights.
This study examined the clinical utility of nibbling behavior
Nibbling is eating in an unplanned, repetitious way between meals and snacks
Participants were 217 obese patients with binge eating disorder
Nibbling was not related to BMI or disordered eating behaviors or cognitions
Assessing nibbling among binge eaters might have little clinical utility
Acknowledgments
Role of Funding Sources:
This research was supported by grants from the National Institutes of Health (R01 DK49587 and R21 MH082629). The funding sponsors had no role in study design, collection, analysis, or interpretation of data, writing the manuscript, and the decision to submit the manuscript for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors:
Robin M. Masheb originated the study idea, conducted statistical analyses and contributed to the writing of the manuscript.
Christina A. Roberto assisted with interpretation of the data and the writing of the manuscript.
Marney A. White provided feedback on the study design and drafts of the manuscript.
All authors have contributed to and reviewed the final manuscript.
Conflict of Interest:
The authors have no conflicts of interest.
References
- Allison KC, Grilo CM, Masheb RM, Stunkard AJ. Binge eating disorder and night eating syndrome: a comparative study of disordered eating. Journal of Consulting and Clinical Psychology. 2005;73:1107–1115. doi: 10.1037/0022-006X.73.6.1107. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual - Text revision. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Buhl KM, Gallagher D, Hoy K, Matthews DE, Heymsfield S. Unexplained disturbance in body weight regulation: Diagnostic outcome assessed by doubly labeled water and body composition analyses in obese patients reporting low energy intakes. Journal of the American Dietetic Association. 1995;95:1393–1400. doi: 10.1016/S0002-8223(95)00367-3. [DOI] [PubMed] [Google Scholar]
- Carter FA, Jansen A. Improving psychological treatment for obesity. Which eating behaviours should we target? Appetite. 2012;58:1063–1069. doi: 10.1016/j.appet.2012.01.016. [DOI] [PubMed] [Google Scholar]
- Colles SL, Dixon JB, O’Brien PE. Loss of control is central to psychological disturbance associated with binge eating disorder. Obesity. 2008;16:608–614. doi: 10.1038/oby.2007.99. [DOI] [PubMed] [Google Scholar]
- de Zwaan M, Hilbert A, Swan-Kremeier L, Simonich H, Lancaster K, Howell LM, et al. Comprehensive interview assessment of eating behavior 18–35 months after gastric bypass surgery for morbid obesity. Surgery for Obesity and Related Diseases. 2010;6:79–85. doi: 10.1016/j.soard.2009.08.011. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z, O'Connor ME. Eating Disorders Examination (Edition 16.0D) In: Fairburn CG, editor. Cognitive behavior therapy and eating disorders. New York: Guilford Press; 2008. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV Axis I disorders - Patient version (SCID-I, Version 2.0) New York: New York State Psychiatric Institute; 1996. [Google Scholar]
- Grilo CM, Masheb RM, Lozano-Blanco C, Barry DT. Reliability of the Eating Disorder Examination in patients with binge eating disorder. International Journal of Eating Disorders. 2004;35(1):80–85. doi: 10.1002/eat.10238. [DOI] [PubMed] [Google Scholar]
- Grilo CM, Masheb RM, Wilson GT. A comparison of different methods for assessing the features of eating disorders in patients with binge eating disorder. Journal of Consulting and Clinical Psychology. 2001;69(2):317–322. doi: 10.1037//0022-006x.69.2.317. [DOI] [PubMed] [Google Scholar]
- Hudson JI, Hiripi E, Pope HG, Jr, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biological Psychiatry. 2007;61(3):348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenkins PE, Conley CS, Rienecke Hoste R, Meyer C, Blissett JM. Perception of control during episodes of eating:Relationships with quality of life and eating psychopathology. International Journal of Eating Disorders. 2012;45:115–119. doi: 10.1002/eat.20913. [DOI] [PubMed] [Google Scholar]
- Latner JD, Hildebrandt T, Rosewall JK, Chisholm AM, Hayashi K. Loss of control over eating reflects eating disturbances and general psychopathology. Behaviour Research and Therapy. 2007;45:2203–2211. doi: 10.1016/j.brat.2006.12.002. [DOI] [PubMed] [Google Scholar]
- Lichtman SW, Pisarska K, Berman ER, Pestone M, Dowling H, Offenbacher E, et al. Discrepancy between self-reported and actual caloric intake and exercise in obese subjects. New England Journal of Medicine. 1992;327:1893–1898. doi: 10.1056/NEJM199212313272701. [DOI] [PubMed] [Google Scholar]
- Masheb RM, Grilo CM, White MA. An examination of eating patterns in community women with bulimia nervosa and binge eating disorder. International Journal of Eating Disorders. 2011;44:618–624. doi: 10.1002/eat.20853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mond JM, Latner JD, Hay PH, Owen C, Rodgers B. Objective and subjective bulimic episodes in the classification of bulimic-type eating disorders: another nail in the coffin of a problematic distinction. Behaviour research and therapy. 2010;48(7):661–669. doi: 10.1016/j.brat.2010.03.020. [DOI] [PubMed] [Google Scholar]
- Reas DL, Wisting L, Kapstad H, Lask B. Nibbling: frequency and relationship to BMI, pattern of eating, and shape, weight and eating concerns among university women. Eating Behaviors. 2012;13:65–66. doi: 10.1016/j.eatbeh.2011.10.005. [DOI] [PubMed] [Google Scholar]