Abstract
There is currently a lack of valid instruments to measure adolescent diabetes numeracy. The Diabetes Numeracy Test (DNT) was adapted for type 1 diabetes and administered to two samples of adolescents. Sample 1 was administered the 39-item version of the DNT (DNT-39) with measures of self-management, responsibility, reading, and glycemic control (A1C). Sample 2 was administered the 14-item version of the DNT (DNT-14) with measures of self-management, responsibility, problem solving, and A1C. Both versions of the DNT showed adequate internal reliability. In sample 1, the DNT-39 and DNT-14 were related (r=.87, p=.001), and both DNT versions were related to parent education (DNT-14 r=.31, p=.02; DNT-39 r=.29, p=.03) and reading (DNT-14 r=.36, p=.005; DNT-39 r=.40, p=.001). In sample 2, the DNT-14 was related to A1C (r=−.29, p=.001), reading skills (r=.36, p=.005), diabetes problem solving (r=.27, p=.02), adolescent age (r=.19, p=.03), and parent education (r=.31, p=.02). In combined analyses, 75% of items were answered correctly on the DNT-14 (Range 7-100), and performance was associated with age (r=.19, p=.03), pump use (r=.33 p=.001), and A1C (r=−.29, p=.001). The DNT-14 is a feasible, reliable, and valid numeracy assessment that indicated adolescents with T1D have numeracy deficits that may impact their glycemic control.
Literacy includes a variety of skills beyond reading and writing (print literacy), including: listening and speaking (oral literacy), and numeracy (Nielsen-Bohlman, Panzer, & Kindig, 2004). Nearly half of American adults have inadequate general literacy (Nielsen-Bohlman, L., et al., 2004): 32% of adults have only basic quantitative skills, and 26% of adults have below basic quantitative skills. Quantitative literacy, or numeracy, can be defined as “the ability to understand and use numbers in daily life” (Rothman, Montori, Cherrington, & Pignone, 2008). Numeracy involves a range of skills including one’s ability to perform basic math functions; understand time, money, measurement, graphs, and probability; and the ability to perform multi-step math. Numeracy also includes the ability to figure out what math skills to apply to a given situation (i.e., contextual or application oriented numeracy) (Golbeck, Ahlers-Schmidt, Paschal,, & Dismuke, 2005; Montori, & Rothman, 2005). Knowledge does not always result in appropriate action due to issues such as motivation and/or situational barriers to knowledge implementation. However, lower health related numeracy in adults has frequently been shown to impact patients’ understanding of disease and health outcomes (Dewalt, Berkman, Sheridan, Lohr, & Pignone, 2004; Rothman, et al., 2004; Williams, Baker, Parker, & Nurss, 1998).
Successful self-management of T1D requires use of math skills on a daily basis including carbohydrate counting, interpretation of food labels and portion sizes, understanding glucometer results, drawing up the correct amount of insulin into a syringe, dosing insulin according to the number of carbohydrates eaten and/or blood sugar level, and successfully treating hypoglycemia. All of these self-management tasks require numeracy-related skills. In adults with type 2 diabetes, poor numeracy is prevalent, and numeracy skills have been related to inadequate self-management and outcomes (Cavanaugh, et al., 2008; Cavanaugh, et al., 2009; Osborn, Cavanaugh, Wallston, White, & Rothman, 2009; Sarkar, et al., 2010).
Self-management autonomy becomes increasingly important as children move into adolescence, seek independence, and spend more time away from home. For some adolescents, critical numeracy skills may have been only recently (if at all) mastered by the time they are trying to function autonomously. Though glycemic control depends on many variables, including patient motivation and environment, knowledge of how to perform diabetes-related tasks is ultimately necessary for success. To date, little research has been conducted on health literacy and numeracy in adolescents. Previous research has resulted in validation of numeracy scales for adults with diabetes (Huizinga, et al., 2008), measures for adolescent functional health literacy (Chisolm, & Buchanan, 2007), and measures of literacy or numeracy for parents of children with diabetes (Sanders, Federico, Klass, Abrams, & Dreyer, 2009; Sanders, Rothman, Franco, Lopez, & Delamater, 2008). However, no numeracy scales have been validated for adolescents with diabetes. The goals of this research were to describe numeracy skills in adolescents with type 1 diabetes, and examine the construct and predictive validity of the Diabetes Numeracy Test (DNT) when used with adolescents. Identifying low numeracy in routine clinical practice may allow identification of adolescents who could benefit from educational intervention, supportive tools, and/or regimen simplification.
METHODS
Scale Development
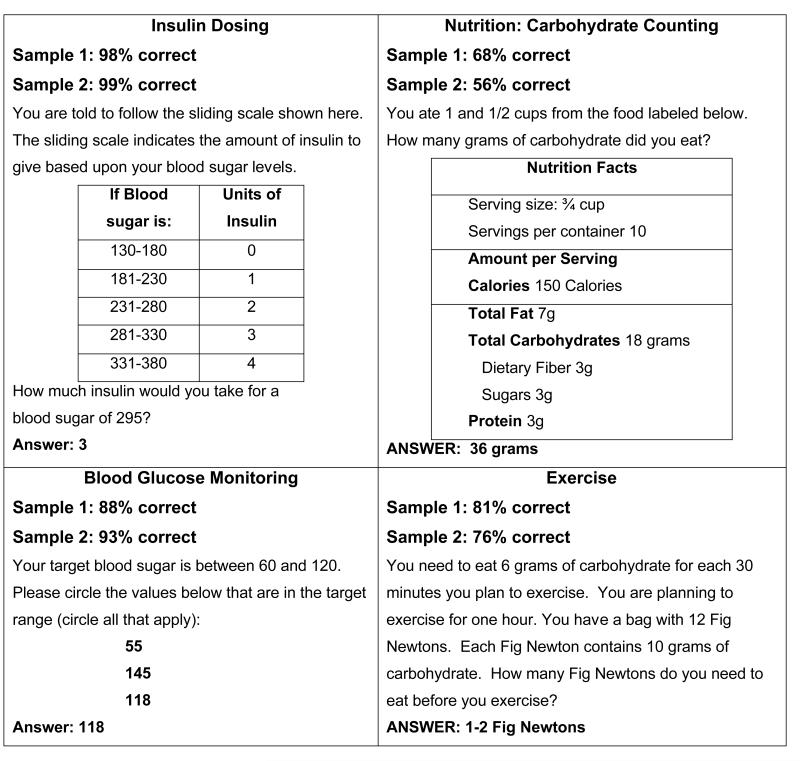
Our goal was to examine the Diabetes Numeracy Test (DNT), previously validated in adults with type 2 diabetes, for use in adolescents with T1D. The original DNT scale was developed by a team of experts in diabetes, literacy, and numeracy. A full description of the adult DNT development process is available elsewhere (Huizinga, et al., 2008). The original adult version of the DNT consisted of 43 items. To improve feasibility, a subset of 15 items from the full scale was also validated (DNT-15) (Cavanaugh et al., 2009; Huizinga et al., 2008). Item content on both versions of the DNT includes nutrition, exercise, blood glucose monitoring, and insulin administration. Figure 1 shows examples of items from each of the content domains. The items cover different types of math skills including: addition, subtraction, multiplication, division, fractions, multi-step mathematics, time, and numeration/counting. For the current research, the 43-item version was reduced to 39 items, and the 15-item version was reduced to 14 items by eliminating questions specific to type 2 diabetes (e.g. metformin dosing).
Figure 1.
Examples of DNT-14 items from each of the four content domains.
Recruitment and Settings
The study consisted of two independent samples. In sample 1, 61 adolescents were recruited. Data were collected from adolescents with Type 1 diabetes at the Vanderbilt Eskind Pediatric Diabetes Clinic or at the Tennessee Camp for Diabetic Children (TCDC) during 2004. Eligible patients were 12-17 years of age, fluent in English, and had a consenting guardian. Adolescents were excluded if they had >20/50 on the Rosenbaum pocket screen for visual acuity or a medical diagnosis involving cognitive deficits, psychosis, or blindness.
Sample 2 consisted of 72 adolescents with type 1 diabetes recruited from July to December 2009 as part of an adherence intervention study within the Vanderbilt Eskind Pediatric Diabetes Clinic. Inclusion criteria for sample 2 included a diagnosis of type 1 diabetes for at least 1 year, age 13-17, English speaking, and access to the Internet; as with sample 1, a consenting guardian was required. Adolescents were excluded if they had been diagnosed with intellectual, visual, or auditory disabilities.
Measures
Trained research assistants or a trained medical student administered the surveys to the adolescents and abstracted most recent A1C level from each medical record. The DNT 39-item version was administered to sample 1, and answers to the items in the DNT 14-item version were later analyzed separately. In addition to the DNT, demographic and clinical diabetes items, and the following measures were administered to sample 1 (N=61):
Summary of Diabetes Self-Care Activities-Revised (SSCA-R)
The SSCA-R is an 11-item validated scale that assesses the frequency of type 1 diabetes self-care task completion for the previous 7 days, including timing and dosing of insulin, general diet and snacks, exercise, blood glucose monitoring, foot care, and smoking (Schafer, Glasgow, Mccaul, & Dreher, 1983; Schilling, Grey, & Knafl, 2002).
Wide Range Achievement Test-3 (WRAT-3 Reading section) (Wilkinson, 1993)
The WRAT-3 Reading is a 36-item subtest of the WRAT-3 which assesses word recognition and reading skills. The WRAT-3 reading subtest has been related to general IQ as well as other intellectual skills assessed on the full WRAT-3, such as spelling and arithmetic (Strauss, Sherman, & Spreen, 2006).
Diabetes Family Responsibility Questionnaire (DFRQ) (Anderson, Auslander, Jung, Miller, & Santiago, 1990)
The DFRQ is a widely-used 17-item validated scale that assesses the extent of individual and shared responsibility related to completion of self-care tasks. For sample 1, adolescents were administered the child version of the DFRQ. In sample 2, parents were administered the DFRQ.
Sample 2 (N=72) was administered the DNT-14, demographic and clinical diabetes items, and the parent version of the DFRQ (Anderson et al., 1090). Sample 2 also completed the following two scales:
Diabetes Behavior Rating Scale (DBRS)
The DBRS is a 37-item validated scale that measures a range of self-care behaviors in adolescents related to the prevention of glycemic events, response to glycemic events, and maintenance behaviors (e.g. attending clinic appointments) in type 1 diabetes (Iannotti, et al., 2006).
Diabetes Problem Solving for Adolescents (Mulvaney, Wallston, Rothman, & Hartog, 2009)
The DPS-A is a new 27-item scale that is currently being validated in adolescents with type 1 diabetes. Items measure the ability to identify barriers to self-care and resolve them. The scale has adequate internal consistency (.89), and is related to HbA1c (−.32).
Ethics
Both studies received approval from the Vanderbilt Institutional Review Board. Parent consent and adolescent assent were obtained before completion of study measures.
Data Analysis
Patient characteristics were analyzed using means, medians, and percentages as appropriate. Performance on the numeracy scales was calculated as percent correct. Internal reliability of the scales was assessed using the Kuder-Richardson 20 reliability coefficient. Fourteen items from the DNT-39 were used for the DNT-14 (See Scale Development above). Construct validity was assessed through bivariate correlation between the DNT-39 and DNT-14 with other measures. All analyses relating the DNT to other measures used non-parametric Spearman Rho bivariate correlation. Within samples tests of significance were completed using F ratios and between samples using independent samples t-tests. In a combined analysis, performance on the DNT-14 was then compared to participant characteristics that were available in both participant samples. This included age, gender, diabetes duration, insulin pump status and A1C. All analyses were performed using SPSS v. 18.
RESULTS
Table 1 shows descriptive statistics for the two samples. The two samples were not significantly different on demographics, clinical characteristics, or mean DNT-14 score.
Table 1.
Characteristics of sample 1, sample 2, and tests of mean differences.
| Variable | Sample 1 (N=61) | Sample 2 (N=72) | Difference (p value) |
|---|---|---|---|
| Mean (SD) or % | Mean (SD) or % | ||
| Age (years) | 13.92 (1.29) | 15.10 (1.41) | .19 |
| Gender (% Male) | 52.50 | 55.60 | .52 |
| Race / Ethnicity | |||
| White | 85.20 | 90.30 | .43 |
| Black | 11.50 | 6.90 | |
| Hispanic | 3.30 | 1.40 | |
| Asian | 0 | 1.40 | |
| Pump Use (% Yes) | 49.20 | 58.30 | .90 |
| Diabetes Duration (years) | 5.79 (3.32) | 6.30 (3.35) | .81 |
| Parent Education (years) | 12.47 (1.25) | NA | NA |
| Annual Household Income (Modal Range) |
$40 – 60,000 | NA | NA |
| HbA1c (%) | 8.78 (1.54) | 8.75 (1.71) | .62 |
| DNT-14 (% correct) | 73.77 (21.54) | 77.08 (22.39) | .33 |
| DNT-39 (% correct) | 69.25 (16.99) | NA | NA |
Sample 1 Analyses
For sample 1 (N=61) the DNT-39 mean was 69.25 (SD 16.99, 95% CI 64.90-73.60), median 74.36, range 21-97, and mode = 74. The DNT-14 mean was 73.77 (SD 21.54, 95% CI 68.25-79.29), median 76.92, range 7-100, and mode = 92. Internal reliability for the DNT-39 was .93, and .80 for the DNT-14. The two versions of the DNT were correlated .87 (p=.001). Table 2 shows the bivariate relationship of both versions of the DNT with relevant variables within sample 1. Pump users scored significantly higher on the DNT-39 (pump Mean 74.67, SD 13.28; non-pump Mean 64.01, SD 18.68, F 6.54, p=.01) and the DNT-14 (pump Mean 81.01, SD 15.87; non-pump Mean 66.76, SD 24.11, F 7.38, p=.01). Higher DNT score was also significant associated with parent education level (r=0.31, p=0.02). Males and females did not differ on either version of the test (39-item p=.76; 14-item p=.42). Neither the DNT-39 (r=−.22, p=.09) nor the 14 item version (r=−.14, p=.31) were significantly related to A1C in this sample.
Table 2.
Sample 1 bivariate correlations (rs) and obtained significance levels between the DNT and additional measures (N=61).
| Self- Management (SSCA-R) |
Diabetes Responsibility (adolescent) |
Parent Education |
WRAT3 | HbA1c | |
|---|---|---|---|---|---|
| DNT-39 | .12 (.350) | .09 (.506) | .29 (.028) | .40 (.001) | −.22 (.086) |
| DNT-14 | .11 (.382) | −.23 (.859) | .31 (.019) | .36 (.005) | −.13 (.310) |
Sample 2 Analyses
For sample 2 (N=72) mean performance on the DNT-14 in this sample was 77.08 (SD 22.39, 95% CI 71.82-82.34), median 85.71, range 14-100, and mode = 100. Internal reliability was .83 for the DNT 14. Table 3 shows the relationships between the DNT-14 and additional measures for sample 2. The DNT-14 was related to A1C and diabetes problem solving. Mean DNT-14 scores were not significantly different between male and female participants (p=.50). Insulin pump users (Mean 84.17, SD 20.00) scored significantly higher than non-pump users (Mean 71.19, SD 23.31; F 4.81, p=.01).
Table 3.
Sample 2 bivariate correlations (rs) and obtained significance levels between the DNT-14 and additional measures (N=72).
| Self- Management (DBMS) |
Diabetes Responsibility (parent) |
Diabetes Problem Solving |
HbA1c | |
|---|---|---|---|---|
| DNT-14 | .03 (.820) | −.29 (.022) | .27 (.023) | −.34 (.004) |
Combined Samples
The DNT-14 was available for analyses in both samples. In combined samples analyses, internal consistency reliability for the DNT-14 was .82 (N=133). The combined samples DNT-14 mean was 75.56 (SD 22.00, 95% CI 71.79-79.34), median 84.61, range 7.69-100, and mode = 100. The majority of scores were at the higher end of the score distribution (skewness −.91). Table 4 shows bivariate correlations between the DNT-14 and measures administered to both samples. The DNT-14 was related to age, pump use, and A1C. Gender (p=.36) was not related to numeracy scores. Adolescents using an insulin pump scored significantly higher (Mean 82.76, SD 18.20) than those who did not use an insulin pump (Mean 68.32, SD 23.36; F 8.01, p=.001).
Table 4.
Combined samples bivariate correlations (rs) and obtained significance levels between DNT-14 and demographic and clinical measures (N=133).
| Child Age | Gender | Pump Use | Diabetes Duration |
HbA1c | |
|---|---|---|---|---|---|
| DNT-14 | .194 (.026) | .002 (.986) | .326 (.000) | −.005 (.951) | −.291 (.001) |
DISCUSSION
Both versions of the Diabetes Numeracy Test demonstrated internal consistency. The two versions showed relationships with glycemic control that were consistently in the appropriate direction. The 39-item version demonstrated construct validity in relation to reading skills. Results confirm predictive validity of the DNT 14-item version in relation to glycemic control, and construct validity in relation to diabetes problem solving (results from sample 2) and reading skills (results from sample 1). Scores on the DNT-14 increased as expected with increased grade level of the child and parent education. Pump users performed better on the DNT, likely because patients are required to demonstrate good control and reasonable hemoglobin A1c before being allowed to receive pump training at this center; in addition, patients receive intensive education prior to starting pump therapy, which in some cases may be the first time the adolescent participates in active education since their parents may have played a more central role at the time of diabetes diagnosis. Results are consistent with studies that used the DNT with adults suggesting relevancy for use with adolescents and adults (Chisolm & Buchanan, 2007).
Adolescents with T1D were able to correctly answer on average 75% of the items on the DNT-14, with a median of 85%. This performance is higher compared with adults with type 2 diabetes in previous studies (Cavanaugh, et al., 2009; Huizinga, et al., 2008). Adolescent performance on the DNT-14 revealed a wide range with a large standard deviation. This suggests that for some adolescents with diabetes low numeracy may be a real factor in successful self-management. Identifying patients with low diabetes-related numeracy may allow for targeting adolescents who need tailored educational programs and may inform decisions related to clinical recommendations.
Lower numeracy in this sample was associated with lower parent education, greater parent responsibility, and lower adolescent reading skills and diabetes problem-solving skills. Numeracy was significantly higher for insulin pump users in both samples. Self-management was not related to performance on the DNT, similar to studies in adults (Cavanaugh, et al., 2008). The lack of relationship between numeracy and adherence may be a result of the gap between self-management knowledge and action. Regardless of the level of numeracy skills, there are many factors that may influence the implementation of numeracy skills in everyday life. Adolescents report a variety of psychosocial barriers to self-management related to burn out, social support, and embarrassment (Mulvaney, et al., 2009). Difficulties in implementing knowledge and skills may also explain the mixed statistical findings for the relationship between the DNT and A1C in this study. Additionally, adherence rates are typically higher when assessed via self-report compared to more objective methods, and may be related to social desirability (Shiffman, Stone, & Hufford, 2008).
There are several limitations to the current study. The study includes adolescents from the same geographic region, but who were administered the test within different contexts. Although samples shared demographic and clinical variables, some measures, like the WRAT and Diabetes Problem Solving, were only administered to one sample. Sample 2 had limited socio-demographic data (e.g. no parent education), and so the two samples could not be compared directly on that variable. Finally, although the DNT in adolescents demonstrated associations similar to that observed in adults, no other measure of numeracy was used in this study for comparison.
An increased focus on adolescent health literacy and numeracy is needed to measure and document those skills, as well as to improve services and materials to support adolescents and parents in successful diabetes self-care management. The DNT-14 provides a more feasible option for the assessment of numeracy. However, to improve discrimination and assessment at the upper skill levels, difficulty of the DNT for adolescents with type 1 diabetes may need to be increased. Review of performance on the DNT can help providers identify areas where educational intervention is necessary. Studies have found relationships between parent literacy and numeracy and child outcomes (Hassan, & Heptulla, 2010; Ross, Frier, Kelnar, & Deary, 2001). Future research on the DNT should relate parent literacy and numeracy to those skills and outcomes in children.
Despite the overall encouraging levels of numeracy in this population, there was a significant minority of participants who exhibited lower diabetes-related numeracy. Intervention research designed to address numeracy in adolescents with type 1 diabetes should direct educational efforts toward the individuals who most need support. The relationship between adolescent numeracy and A1C needs to be examined in a larger sample, and the DNT should be validated in adolescents with type 2 diabetes.
Acknowledgments
The research was supported by DK070026 to Dr. Mulvaney, and K23 DK065294 and Vanderbilt Diabetes Research and Training Center Pilot and Feasibility Program grant DK020593 to Dr. Rothman. Dr. Cavanaugh is supported by K23 DK080952.
Contributor Information
SHELAGH A. MULVANEY, Vanderbilt University School of Nursing, and Division of Pediatric Endocrinology, Department of Pediatrics, and Department of Biomedical Informatics, Vanderbilt University Medical Center, Nashville, Tennessee, USA
JESSICA S. LILLEY, Division of Pediatric Endocrinology, Department of Pediatrics, Vanderbilt University Medical Center, Nashville, Tennessee, USA
KERRI L. CAVANAUGH, Division of Nephrology, Department of Medicine, and Center for Health Services Research, Institute for Medicine and Public Health, Department of Medicine, Vanderbilt University Medical Center, Nashville, Tennessee, USA
ERIC J. PITTEL, Eskind Pediatric Diabetes Clinic, Vanderbilt University Medical Center, Nashville, Tennessee, USA
RUSSELL L. ROTHMAN, Division of Pediatric Endocrinology, Department of Pediatrics, and Center for Health Services Research, Institute for Medicine and Public Health, Department of Medicine, Vanderbilt University Medical Center, Nashville, Tennessee, USA
REFERENCES
- Anderson BJ, Auslander WF, Jung KC, Miller JP, Santiago JV. Assessing family sharing of diabetes responsibilities. Journal of Pediatric Psychology. 1990;15(4):477–492. doi: 10.1093/jpepsy/15.4.477. [DOI] [PubMed] [Google Scholar]
- Cavanaugh K, Huizinga MM, Wallston KA, Gebretsadik T, Shintani A, Davis DA, et al. Association of numeracy and diabetes control. Annals of Internal Medicine. 2008;148(10):737. doi: 10.7326/0003-4819-148-10-200805200-00006. [DOI] [PubMed] [Google Scholar]
- Cavanaugh K, Wallston KA, Gebretsadik T, Shintani A, Huizinga MM, Davis DA, et al. Addressing literacy and numeracy to improve diabetes care. Diabetes Care. 2009;32(12):2149–2155. doi: 10.2337/dc09-0563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chisolm DJ, Buchanan L. Measuring adolescent functional health literacy: A pilot validation of the test of functional health literacy in adults. Journal of Adolescent Health. 2007;41(3):312–314. doi: 10.1016/j.jadohealth.2007.04.015. [DOI] [PubMed] [Google Scholar]
- DeWalt DA, Berkman ND, Sheridan S, Lohr KN, Pignone MP. Literacy and health outcomes: A systematic review of the literature. Journal of General Internal Medicine. 2004;19(12):1228–1239. doi: 10.1111/j.1525-1497.2004.40153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golbeck A, Ahlers-Schmidt C, Paschal A, Dismuke S. A definition and operational framework for health numeracy. American Journal of Preventive Medicine. 2005;29(4):375–376. doi: 10.1016/j.amepre.2005.06.012. [DOI] [PubMed] [Google Scholar]
- Hassan K, Heptulla RA. Glycemic control in pediatric type 1 diabetes: Role of caregiver literacy. Pediatrics. 2010;125(5):e1104–1108. doi: 10.1542/peds.2009-1486. [DOI] [PubMed] [Google Scholar]
- Huizinga M, Elasy T, Wallston K, Cavanaugh K, Davis D, Gregory R, et al. Development and validation of the diabetes numeracy test (dnt) BMC Health Services Research. 2008;8(1-8):96. doi: 10.1186/1472-6963-8-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iannotti RJ, Nansel TR, Schneider S, Haynie DL, Simons-Morton B, Sobel DO, et al. Assessing regimen adherence of adolescents with type 1 diabetes. Diabetes Care. 2006;29(10):2263–2267. doi: 10.2337/dc06-0685. [DOI] [PubMed] [Google Scholar]
- Montori V, Rothman R. Weakness in numbers. The challenge of numeracy in health care. Journal of General Internal Medicine. 2005;20(11):1071–1072. doi: 10.1111/j.1525-1497.2005.051498.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulvaney SA, Wallston KA, Rothman RL, Hartog A. Modeling problem solving barriers to self-management: Pilot data from an internet intervention to adolescents with type 1 diabetes; Paper presented at the Proceedings from the American Diabetes Association Annual Meeting; 2009. [Google Scholar]
- Nielsen-Bohlman L, Panzer AM, Kindig DA. Health literacy: A prescription to end confusion. National Academies Press; Washington, D.C.: 2004. [PubMed] [Google Scholar]
- Osborn CY, Cavanaugh K, Wallston KA, White RO, Rothman RL. Diabetes numeracy: An overlooked factor in understanding racial disparities in glycemic control (original article: Epidemiology/health services research) Diabetes Care. 2009;32(9):1614–1619. doi: 10.2337/dc09-0425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross LA, Frier BM, Kelnar CJH, Deary IJ. Child and parental mental ability and glycaemic control in children with type 1 diabetes. Diabetic Medicine. 2001;18(5):364–369. doi: 10.1046/j.1464-5491.2001.00468.x. [DOI] [PubMed] [Google Scholar]
- Rothman R, DeWalt D, Malone R, Bryant B, Shintani A, Crigler B, et al. Influence of patient literacy on the effectiveness of a primary care-based diabetes disease management program. Journal of the American Medical Association. 2004;292(14):1711–1716. doi: 10.1001/jama.292.14.1711. [DOI] [PubMed] [Google Scholar]
- Rothman RL, Montori VM, Cherrington A, Pignone MP. Perspective: The role of numeracy in health care. [Article] Journal of Health Communication. 2008;13(6):583–595. doi: 10.1080/10810730802281791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanders LM, Federico S, Klass P, Abrams MA, Dreyer B. Literacy and child health: A systematic review. Archives of Pediatrics and Adolescent Medicine. 2009;163(2):131–140. doi: 10.1001/archpediatrics.2008.539. [DOI] [PubMed] [Google Scholar]
- Sanders LM, Rothman RL, Franco V, Lopez F, Delamater AM. Low parent health literacy is associated with poor glycemic control in children with type 1 diabetes mellitus; Paper presented at the Pediatric Academic Society Annual Meeting; 2008. [Google Scholar]
- Sarkar U, Karter A, Liu J, Moffet H, Adler N, Schillinger D. Hypoglycemia is more common among type 2 diabetes patients with limited health literacy: The diabetes study of northern california (distance) Journal of General Internal Medicine. 2010;25(9):962–968. doi: 10.1007/s11606-010-1389-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schafer LC, Glasgow RE, McCaul KD, Dreher M. Adherence to iddm regimens: Relationship to psychosocial variables and metabolic control. Diabetes Care. 1983;6(5):493–498. doi: 10.2337/diacare.6.5.493. [DOI] [PubMed] [Google Scholar]
- Schilling LS, Grey M, Knafl KA. A review of measures of self-management of type 1 diabetes by youth and their parents. Diabetes Educator. 2002;28(5):796–808. doi: 10.1177/014572170202800520. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Stone A, Hufford M. Ecological momentary assessment. Annual Review of Clinical Psychology. 2008;4:1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]
- Strauss E, Sherman EMS, Spreen O. A compendium of neuropsychological tests: Administration, norms, and commentary. Oxford University Press; New York, NY: 2006. [Google Scholar]
- Wilkinson G. The wide range achievement test - third edition (wrat-3) 3 ed. Wide Range; Wilmington, DE: 1993. [Google Scholar]
- Williams MV, Baker DW, Parker RM, Nurss JR. Relationship of functional health literacy to patients’ knowledge of their chronic disease: A study of patients with hypertension and diabetes. Archives of Internal Medicine. 1998;158(2):166–172. doi: 10.1001/archinte.158.2.166. [DOI] [PubMed] [Google Scholar]