Abstract
Background
Diet modification is an important part of self-management for patients with diabetes and/or heart disease (including coronary artery disease, heart failure, and atrial fibrillation). Many health care providers and community-based programs advise lifestyle and diet modification as part of care for people with these conditions. This report synthesizes qualitative information on how patients respond differently to the challenges of diet modification. Qualitative and descriptive evidence can illuminate challenges that may affect the success and equitable impact of dietary modification interventions.
Objectives
To (a) examine the diet modification challenges faced by diabetes and/or heart disease patients; and (b) compare and contrast the challenges faced by patients who are members of vulnerable and nonvulnerable groups as they change their diet in response to clinical recommendations.
Data Sources
This report synthesizes 65 primary qualitative studies on the topic of dietary modification challenges encountered by patients with diabetes and/or heart disease. Included papers were published between 2002 and 2012 and studied adult patients in North America, Europe, and Australia/New Zealand.
Review Methods
Qualitative meta-synthesis was used to integrate findings across primary research studies.
Results
Analysis identified 5 types of challenges that are common to both vulnerable and nonvulnerable patients: self-discipline, knowledge, coping with everyday stress, negotiating with family members, and managing the social significance of food. Vulnerable patients may experience additional barriers, many of which can magnify or exacerbate those common challenges.
Limitations
While qualitative insights are robust and often enlightening for understanding experiences and planning services in other settings, they are not intended to be generalizable. The findings of the studies reviewed here—and of this synthesis—do not strictly generalize to the Ontario (or any specific) population. This evidence must be interpreted and applied carefully, in light of expertise and the experiences of the relevant community.
Conclusions
Diet modification is not simply a matter of knowing what to eat and making the rational choice to change dietary practices. Rather, diet and eating practices should be considered as part of the situated lives of patients, requiring an individualized approach that is responsive to the conditions in which each patient is attempting to make a change. Common challenges include self-discipline, knowledge, coping with everyday stress, negotiating with family members, and managing the social significance of food. An individualized approach is particularly important when working with patients who have vulnerabilities.
Plain Language Summary
Health care providers often encourage people with diabetes and/or heart disease to change their diet. They advise people with diabetes to eat less sugar, starch, and fat. They advise people with heart disease to eat less fat and salt. However, many patients find it difficult to change what they eat. This report examines the challenges people may face when making such changes. It also examines the special challenges faced by people who are vulnerable due to other factors, such as poverty, lack of education, and difficulty speaking English. Five themes were common to all people who make diet changes: self-discipline, knowledge, coping with stress, negotiating with family members, and managing the social aspect of food. Members of vulnerable groups also reported other challenges, such as affording fresh fruit and vegetables or understanding English instructions. This report may help health care providers work with patients more effectively to make diet changes.
Background
In July 2011, the Evidence Development and Standards (EDS) branch of Health Quality Ontario (HQO) began developing an evidentiary framework for avoidable hospitalizations. The focus was on adults with at least 1 of the following high-burden chronic conditions: chronic obstructive pulmonary disease (COPD), coronary artery disease (CAD), atrial fibrillation, heart failure, stroke, diabetes, and chronic wounds. This project emerged from a request by the Ministry of Health and Long-Term Care for an evidentiary platform on strategies to reduce avoidable hospitalizations.
After an initial review of research on chronic disease management and hospitalization rates, consultation with experts, and presentation to the Ontario Health Technology Advisory Committee (OHTAC), the review was refocused on optimizing chronic disease management in the outpatient (community) setting to reflect the reality that much of chronic disease management occurs in the community. Inadequate or ineffective care in the outpatient setting is an important factor in adverse outcomes (including hospitalizations) for these populations. While this did not substantially alter the scope or topics for the review, it did focus the reviews on outpatient care. HQO identified the following topics for analysis: discharge planning, in-home care, continuity of care, advanced access scheduling, screening for depression/anxiety, self-management support interventions, specialized nursing practice, and electronic tools for health information exchange. Evidence-based analyses were prepared for each of these topics. In addition, this synthesis incorporates previous EDS work, including Aging in the Community (2008) and a review of recent (within the previous 5 years) EDS health technology assessments, to identify technologies that can improve chronic disease management.
HQO partnered with the Programs for Assessment of Technology in Health (PATH) Research Institute and the Toronto Health Economics and Technology Assessment (THETA) Collaborative to evaluate the cost-effectiveness of the selected interventions in Ontario populations with at least 1 of the identified chronic conditions. The economic models used administrative data to identify disease cohorts, incorporate the effect of each intervention, and estimate costs and savings where costing data were available and estimates of effect were significant. For more information on the economic analysis, please contact either Murray Krahn at murray.krahn@theta.utoronto.ca or Ron Goeree at goereer@mcmaster.ca.
HQO also partnered with the Centre for Health Economics and Policy Analysis (CHEPA) to conduct a series of reviews of the qualitative literature on “patient centredness” and “vulnerability” as these concepts relate to the included chronic conditions and interventions under review. For more information on the qualitative reviews, please contact Mita Giacomini at giacomin@mcmaster.ca.
The Optimizing Chronic Disease Management in the Outpatient (Community) Setting mega-analysis series is made up of the following reports, which can be publicly accessed at http://www.hqontario.ca/evidence/publications-and-ohtac-recommendations/ohtas-reports-and-ohtac-recommendations.
Optimizing Chronic Disease Management in the Outpatient (Community) Setting: An Evidentiary Framework
Discharge Planning in Chronic Conditions: An Evidence-Based Analysis
In-Home Care for Optimizing Chronic Disease Management in the Community: An Evidence-Based Analysis
Continuity of Care: An Evidence-Based Analysis
Advanced (Open) Access Scheduling for Patients With Chronic Diseases: An Evidence-Based Analysis
Screening and Management of Depression for Adults With Chronic Diseases: An Evidence-Based Analysis
Self-Management Support Interventions for Persons With Chronic Diseases: An Evidence-Based Analysis
Specialized Nursing Practice for Chronic Disease Management in the Primary Care Setting: An Evidence-Based Analysis
Electronic Tools for Health Information Exchange: An Evidence-Based Analysis
Health Technologies for the Improvement of Chronic Disease Management: A Review of the Medical Advisory Secretariat Evidence-Based Analyses Between 2006 and 2011
Optimizing Chronic Disease Management Mega-Analysis: Economic Evaluation
How Diet Modification Challenges Are Magnified in Vulnerable or Marginalized People With Diabetes and Heart Disease: A Systematic Review and Qualitative Meta-Synthesis
Chronic Disease Patients’ Experiences With Accessing Health Care in Rural and Remote Areas: A Systematic Review and Qualitative Meta-Synthesis
Patient Experiences of Depression and Anxiety With Chronic Disease: A Systematic Review and Qualitative Meta-Synthesis
Experiences of Patient-Centredness With Specialized Community-Based Care: A Systematic Review and Qualitative Meta-Synthesis
Objective of Analysis
To (a) examine the diet modification challenges faced by heart disease and/or diabetes patients; and (b) compare and contrast the challenges faced by patients who are members of vulnerable and nonvulnerable groups as they change their diet in response to clinical recommendations.
Clinical Need and Target Population
Diabetes
Diabetes is a metabolic condition characterized by a deficiency in either insulin production or uptake. It is a chronic disease associated with multiple complications, including cardiovascular disease, stroke, blindness, kidney damage/failure, nerve damage, and amputations. (1) More than 90% of people with diabetes have type 2 diabetes, a form that is associated with increased age, body weight, and family history. (1) The number of Canadians with diabetes has increased dramatically over the last decade: in 2008/2009, almost 2.4 million people were living with the disease. (1)
Heart Disease
Heart disease is a term that encompasses multiple cardiovascular conditions, including coronary artery disease (CAD), heart failure, and atrial fibrillation. CAD is a narrowing of the blood vessels that supply blood and oxygen to the heart. Over 1.3 million Canadians self-reported CAD, which is the leading cause of death for men and women in Canada. (2) Heart failure is a complex set of symptoms indicating a weakened heart muscle and may follow CAD. The estimated prevalence of heart disease in Canadians over age 45 ranges from 2.2% (3) to 12%. (4) Atrial fibrillation is characterized by an irregular heart rate and may also coincide with CAD or other conditions of abnormal heart muscle function. Canadian prevalence figures are not available, but in the United States, 1 in 200 people aged 50 to 60 years has atrial fibrillation, rising to 1 in 10 people over the age of 80 years. (5)
Vulnerability
Development and Use
Following a review of the literature on vulnerability, a theoretical definition was created to sort the literature related to dietary modification. Paying attention to vulnerability is congruent with the Ontario Ministry of Health and Long-Term Care’s focus on health equity as a way of reducing the incidence of costly and preventable illnesses; addressing inequitable access to high-quality care can lead to a better understanding of the specific needs of health-disadvantaged populations. (6)
The definition was derived from a narrative review of the relevant literature; it informed understanding of vulnerability and highlighted groups that could be conceptualized as vulnerable to adverse health outcomes stemming from diabetes and/or heart disease. The definition was used to categorize papers according to whether they included a vulnerable or a nonvulnerable population.
Definition
While there is no clear definition of what constitutes “vulnerable populations,” they may be understood as social groups with an increased relative risk of or susceptibility to adverse health outcomes. This differential risk (or vulnerability) is evidenced by increased comparative morbidity, premature mortality, and diminished quality of life. The fundamental causes of increased susceptibility to disease are low social and economic status and lack of environmental resources. Groups recognized as vulnerable are the poor; those who are subjected to discrimination, intolerance, subordination, and stigma; and those who are politically marginalized, disenfranchised, and denied human rights. Vulnerable groups typically include women and children, visible minorities, immigrants, gay men and lesbians, the homeless, and the elderly. (7, 8)
The concept of vulnerability is linked to the idea of risk as a result of exposure to contingencies and stress, and difficulty coping with such exposures. (9, 10) There are 2 sides to vulnerability: an external side of susceptibility to risks, shocks, and stress; and an internal side, which is a lack of capacity or means to cope without damaging loss. (9, 10) Vulnerability is situational and viewed as a dynamic continuum: a person’s vulnerability can change, increasing during life transitions and major life changes. It is seen as an attribute of the total interaction between the person and his/her external environment. (10, 11)
Technique
Diet modification is part of the treatment and self-management recommendations for patients with diabetes and/or heart disease. (12, 13) For people with diabetes, sustained diet modification is an essential part of maintaining glycemic control, (14) and it is recommended as a preventative measure for people who may be at risk of developing type 2 diabetes. (12) Diet modification is also an important factor in the prevention and treatment of heart disease; (13) excess body weight and high cholesterol and sodium levels may exacerbate heart dysfunction.
Given the significant number of dietary changes recommended for people with diabetes and/or heart disease, (12, 13), the scope of this report was not limited to any 1 type or method of dietary change. Instead, this meta-synthesis considered any reports of a patient’s attempt to change his/her diet, regardless of the type of intervention, education program, or health care provider involvement. Equally relevant were reports of successes, failures, and ongoing efforts related to dietary change. This broad scope reflected our interest in the patient’s experience of dietary modification, which may inform the design and implementation of a variety of self-management interventions or programs.
Evidence-Based Analysis
Research Questions
What are the diet modification challenges faced by diabetes and heart disease patients?
Do patients who are members of vulnerable and nonvulnerable groups experience different challenges as they change their diets in response to clinical recommendations? What challenges do they face, and how do those challenges change the experience of diet modification?
Research Methods
Literature Search
Search Strategy
A literature search was performed on May 3, 2012, using OVID MEDLINE and EBSCO Cumulative Index to Nursing and Allied Health Literature (CINAHL) and on May 4, 2012, using ISI Web of Science Social Sciences Citation Index (SSCI), for studies published from January 1, 2002, until May 2012. We developed a qualitative mega-filter by combining existing published qualitative filters. (15-17) The filters were compared and redundant search terms were deleted. We added exclusionary terms to the search filter that would be likely to identify quantitative research and reduce the number of false positives. We then applied the qualitative mega-filter to 9 condition-specific search filters (atrial fibrillation, chronic conditions, chronic obstructive pulmonary disease, chronic wounds, congestive heart failure, CAD, diabetes, multiple morbidities, and stroke). Appendix 1 provides details of the search strategy. Titles and abstracts were reviewed by 2 reviewers and, for those studies meeting the eligibility criteria, full-text articles were obtained.
Inclusion Criteria
English language full-reports
published between January 1, 2002, and May 2, 2012
primary qualitative empirical research (using any descriptive or interpretive qualitative methodology, including the qualitative component of mixed-methods studies) and secondary syntheses of primary qualitative empirical research
adult patients (> 18 years of age)
Canada, United States, Europe, Australia, and New Zealand
published research work (no theses)
studies addressing any aspect of the experience of dietary modification, nutrition, food, or meals (as indicated in the title or abstract)
participants were patients with diabetes or heart disease
Exclusion Criteria
studies addressing topics other than the experience of dietary modification, nutrition, food, or meals, or this topic was not sufficiently prominent to be mentioned in the title or abstract
studies that did not include patients with diabetes or heart disease
studies labelled “qualitative” but that did not use a qualitative descriptive or interpretive methodology (e.g., case studies, experiments, or observational analyses using qualitative categorical variables)
quantitative research (i.e., using statistical hypothesis testing, using primarily quantitative data or analyses, or expressing results in quantitative or statistical terms)
studies that did not pose an empirical research objective or question, or involve primary or secondary analysis of empirical data
Qualitative Analysis
We analyzed published qualitative research using techniques of integrative qualitative meta-synthesis. (18-21) Qualitative meta-synthesis, also known as qualitative research integration, is an integrative technique that summarizes research over a number of studies with the intent of combining findings from multiple papers. Qualitative meta-synthesis has 2 objectives: first, the aggregate of a result should reflect the range of findings while retaining the original meaning; second, by comparing and contrasting findings across studies, a new integrative interpretation should be produced. (22)
Predefined topic and research questions guided research collection, data extraction, and analysis. Topics were defined in stages as relevant literature was identified and corresponding evidence-based analyses proceeded. All qualitative research relevant to the conditions under analysis was retrieved. In consultation with Health Quality Ontario, a theoretical sensitivity to patient centredness and vulnerability was used to further refine the dataset. Finally, specific research questions were chosen and a final search performed to retrieve papers relevant to these questions. The current analysis included papers that addressed the issue of dietary modification challenges, patients with diabetes and heart disease, and both vulnerable and nonvulnerable groups.
Data extraction focused on—and was limited to—findings that were relevant to this research topic. Qualitative findings are the “data-driven and integrated discoveries, judgments, and/or pronouncements researchers offer about the phenomena, events, or cases under investigation.” (19) In addition to the researchers’ findings, original data excerpts (participant quotes, stories, or incidents) were also extracted to illustrate specific findings and, when useful, to facilitate communication of findings.
Through a staged coding process similar to that of grounded theory, (23, 24) findings were broken into their component parts (key themes, categories, concepts) and then regrouped across studies and related to each other thematically. This process allowed for organization and reflection on the full range of interpretative insights across the body of research. (19, 25) These categorical groupings provided the foundation from which interpretations of the social and personal phenomena relevant to diet modification were synthesized. A “constant comparative” and iterative approach was used, in which preliminary categories were repeatedly compared with the research findings, raw data excerpts, and coinvestigators’ interpretations of the studies, as well as with the original Ontario Health Technology Assessment Committee (OHTAC)-defined topic, emerging clinical evidence-based analyses of related technologies, (26) and feedback from OHTAC deliberations and expert panels on issues related to the topic.
Quality of Evidence
For valid epistemological reasons, the field of qualitative research lacks consensus on the importance of, and methods/standards for, critical appraisal. (27) Qualitative health researchers conventionally underreport procedural details, (20) and the quality of findings tends to rest more on the conceptual prowess of the researchers than on methodological processes. (27) Theoretically sophisticated findings are promoted as a marker of study quality for making valuable theoretical contributions to social science academic disciplines. (28) However, theoretical sophistication is not necessary to contribute potentially valuable information to a synthesis of multiple studies, or to inform questions posed by the interdisciplinary and interprofessional field of health technology assessment. Qualitative meta-synthesis researchers typically do not exclude qualitative research on the basis of independently appraised quality. This approach is common to multiple types of interpretive qualitative synthesis. (18, 19, 22, 28-32)
For this review, the academic peer review and publication process was used to eliminate scientifically unsound studies according to current standards. Beyond this, all topically relevant, accessible research using any qualitative interpretive or descriptive methodology was included. The value of the research findings was appraised solely in terms of their relevance to our research questions and the presence of data that supported the authors’ findings.
Results of Evidence-Based Analysis
The database search yielded 49,676 citations published between January 1, 2002, and May 2012 (with duplicates removed). Articles were excluded based on information in the title and abstract; 2 reviewers reviewed all titles and abstracts to confine the database to qualitative research relevant to any of the chronic diseases. Figure 1 shows the breakdown of when and for what reason citations were excluded from the analysis.
Figure 1: Citation Flow Chart.
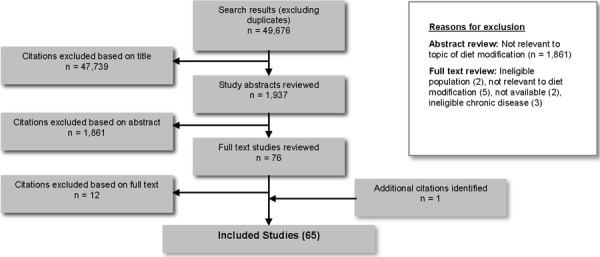
Sixty-four studies met the inclusion criteria. The reference lists of the included studies were hand-searched to identify any additional potentially relevant studies, and 1 additional citation was included, for a total of 65 studies. Of those studies, 41 included patients who were members of vulnerable populations and 24 included patients who were not identified as members of vulnerable populations. Fifty-four mainly addressed patients with diabetes, and 11 mainly addressed patients with heart disease.
For each included study (n = 65), the study design and location were identified and are summarized in Tables 1 and 2, respectively. For each included study about vulnerable populations (n = 41), types of vulnerabilities were identified and are summarized in Table 3.
Table 1: Body of Evidence Examined According to Study Design.
| Study Design | Number of Eligible Studies |
|---|---|
| Content analysis | 8 |
| Ethnographic analysis | 6 |
| Framework analysis | 4 |
| Grounded theory/constant comparative analysis | 11 |
| Other (case study, comparative, discourse analysis, narrative, participatory) | 10 |
| Phenomenological | 7 |
| Qualitative (otherwise unspecified) | 19 |
| Total | 65 |
Table 2: Body of Evidence Examined According to Study Location.
| Study Location | Number of Eligible Studies |
|---|---|
| Australia/New Zealand | 6 |
| Canada (not Ontario) | 4 |
| Europe | 19 |
| Ontario | 3 |
| United States | 33 |
| Total | 65 |
Table 3: Body of Evidence Examined According to Type of Vulnerability Identified.
| Type of Vulnerability Identified | Number of Eligible Studiesa |
|---|---|
| Minority ethnicity or culture | 36 |
| Aboriginal | 6 |
| Hispanic | 6 |
| Afro-Caribbean or Black | 9 |
| South Asian immigrants | 7 |
| Asian immigrants | 3 |
| African or Middle Eastern immigrants | 3 |
| “Minority” otherwise unspecified | 2 |
| Low socioeconomic status | 16 |
| Female | 5 |
| Rural dweller | 6 |
| Physical impairment | 1 |
| Total | 64 |
Many studies mentioned multiple vulnerabilities, so the total equals more than 41.
Context
Of the 41 papers describing vulnerable groups, 36 described patients with diabetes and 5 described patients with heart disease. An analysis of the issues faced by diabetes and heart disease patients when modifying their diet revealed that all patients encounter some common challenges, but that vulnerabilities tend to magnify experiences of common challenges and introduce additional ones. An individual’s particular challenges will reflect his or her unique set of circumstances and vulnerabilities.
Although some challenges may be characteristic of specific vulnerabilities, members of vulnerable groups do not share uniform experiences. Each patient is located in a particular social context, with a unique standpoint, situation, and access to or deprivation from certain resources. (33) This review identified a range of common issues, but the qualitative studies also found sufficient diversity and variation to preclude stereotypes. An individual’s context is shaped by many simultaneous pressures. For example, a program may serve 2 people with diabetes who are female, Bangladeshi immigrants, and senior citizens, but due to their particular social supports, financial resources, health care experiences, educational levels, time in Canada, and other factors, these women may have completely different experiences in adopting dietary modification guidelines. The aim of this report is to describe the issues that patients are likely to face; clinicians who counsel patients about dietary change must spend time exploring each individual’s particular challenges.
Themes
Five themes were identified as common to all patients making dietary modifications: self-discipline, knowledge, coping with everyday stress, negotiating with family members, and managing the social significance of food. Common challenges are outlined below; associated issues for people from vulnerable populations are also described, in relation to how they may exacerbate common challenges.
Self-Discipline
All studies reported that patients often described the challenge of trying to resist food they wanted to eat but knew wasn’t healthy, eat food they knew was healthy but didn’t enjoy, and reduce portion sizes.
Self-discipline is described as both an enabler of and a barrier to dietary change. Descriptions of control and self-discipline are common in diabetes, which often positions the patient as an agent with the power to exert control over his/her food consumption and therefore over his/her blood glucose levels. (34-41) However, this pervasive emphasis on self-discipline may also help explain why patients reported feelings of helplessness and frustration when they adhered to their diet but did not see corresponding improvements in their blood glucose readings. (42) Heart disease patients studied by Doyle (43) also described self-control as a major factor in their success, and a lack of willpower as one of the main causes of failure. Self-discipline was described as an enabler of change for patients who believed that dietary change was important: “regardless of challenges faced and lack of support, participants repeatedly expressed attitudes and beliefs that they could make the necessary changes to control diabetes.” (40) However, it was also understood as a barrier when patients described failure to resist food that was not diet-appropriate, (35-38) but that was enjoyable and brought satisfaction. (39, 41)
In many papers, participants admitted that they regularly succumbed to temptation and ate prohibited foods, because they desired a particular food for the pleasure it brought, (37, 44) as a means of coping with stress or emotion, (45-47) or because consumption of particular foods was linked to identity and belonging. (40, 48-52) Some papers suggested that stress might trigger consumption of unhealthy “comfort” foods. (53) When patients did not like recommended foods, the motivation for increased consumption of those foods was very low. (44, 54) Taste was mentioned frequently by patients from other culinary cultures; they perceived North American food to be bland and tasteless. (50, 53, 55-57) In some instances, the issue of culture can be dealt with by exploring culturally specific foods that are linked to taste (e.g., spices); some may be congruent with a diabetes- or heart-friendly diet. (50) Several authors suggested working with patients to create a diet that suited their palate.
Reducing portion sizes was described as a feasible task in multiple studies, (35, 36, 53, 57-62) and as a means of addressing the problem of limiting favourite unhealthy foods. (58) Many understood portion control to be a main component of dietary modification. However, implementing portion control was challenging. Many patients had difficulty understanding portion sizes and appropriate amounts of different food types. Some used general strategies such as avoiding second helpings (59) or preparing less food. (36, 53) Others spoke about the need to more precisely monitor the amount of food they consumed—”the diabetic diet consists of measuring and weighing every single thing you eat” (61)—but the extra effort required to measure portions was often described as cumbersome. (57, 60)
Another challenge related to portion control was feeling satisfied and overcoming feelings of hunger. (59) Patients who tried to decrease food portions and increase physical activity simultaneously found portion control very difficult. (41, 63) Others had difficulty understanding that not all food intake needed to be reduced; some understood dietary modification to mean that they should only eliminate unhealthy foods, not add healthy alternatives. (39) This finding was present among patients from both vulnerable and nonvulnerable groups, but communication between health care providers and patients from other cultural contexts may have exacerbated this misunderstanding, so that patients struggled with hunger. (39, 59) Lawton (50) described many anecdotes of deprivation and feelings of hunger resulting from misunderstandings about portion control. For example, some participants with diabetes described not being able to sleep because they were hungry, reporting that they would sit awake in bed with the light on, waiting for a blood glucose reading that was low enough to eat something. (50)
A third challenge to portion control was cultural understandings of health and etiology of disease. For Hmong people living in the United States, limiting food intake and feeling hungry is perceived to cause the body to fall out of balance, resulting in illness. The Hmong believe that someone who is ill should eat to satiety, (49) a cultural belief that is incompatible with the idea of portion control. Reducing intake of particular types of food may be problematic for those who believe that particular foods are necessary to keep the body in balance; for instance, traditional Chinese medicine holds that certain foods must be eaten in greater amounts to restore balance. As a result, patients with such beliefs may think that eliminating or reducing intake of certain foods will worsen their condition. (48, 64)
Knowledge
Various knowledge-related challenges were reported by patients: understanding what they should eat, understanding the link between their diet and blood glucose levels, and employing techniques they learned from health care professionals to count carbohydrates or monitor salt intake. These challenges were exacerbated for patients with low levels of health literacy, or with difficulty communicating effectively with health care provider due to language issues.
Knowledge deficits were widely reported in papers examining both vulnerable and nonvulnerable patients. Reported knowledge deficits included basic understanding of types of food that were diabetes- or heart-friendly; (54, 65) the relationship between diet and blood glucose levels; (61, 66, 67) the link between exercise, food, and blood glucose levels; (37, 42, 63, 65) the etiology and effects of diabetes; (68, 69) counting calories or carbohydrates; (38) and what foods were vegetables (versus carbohydrates). (70) Among heart disease patients, knowledge about dietary fibre was low, (71) which may explain other findings that fibre intake was seldom increased, even among those who were successful at making other dietary changes. (45)
Knowledge was generally seen as a wholly positive influence on dietary modification; for instance, it was described as empowering, increasing both motivation and feelings of self-efficacy. (34, 40, 72, 73) Doyle (43) referred to “poor recall of information” rather than lack of knowledge, drawing attention to the fact that it was difficult to evaluate whether a patient’s reported or demonstrated lack of knowledge meant a lack of opportunity to acquire knowledge or poor retention of knowledge that had been shared.
There were inconsistent reports about the level of knowledge needed for successful dietary modification. While most papers documented knowledge deficits, 2 emphasized that knowledge was not a barrier to dietary change. (45, 74) Clark and colleagues (45) studied Canadian heart disease patients of low socioeconomic status; participants demonstrated a high level of knowledge about the types of foods that increased cardiac risk and identified barriers other than knowledge to implementing dietary change. Greenhalgh and colleagues (74) emphasized that knowledge of dietary “facts” was not a main barrier to dietary change, even though significant knowledge deficits were prevalent among their sample of multiethnic British patients with diabetes. The authors stressed the importance of knowledge gained via “legitimate peripheral participation,” (74) rather than the acquisition of socially disembodied facts. By participating in their own self-management and interacting with peers and health care providers, patients were better able to develop socially and personally relevant knowledge and strategies for managing their diabetes. (74)
Read together, the papers by Greenhalgh (74) and Clark (45) provide a nuanced analysis of the relationship between knowledge and dietary change—one that may help explain and unite the more disparate findings in the literature. Knowledge that is applicable and useful may be most helpful to patients who are implementing self-management activities (including, but not limited to, dietary modification). Health care professionals should be encouraged to think of dietary counselling beyond the transfer of knowledge and skills, (75) and to help patients understand how to modify their diet in the unique context of their own life. For example, Aboriginal participants in Australia reported difficulty applying the knowledge they learned in a diabetes cooking course because of family/household preferences and the affordability of food. (76)
For immigrant patients whose first language was not English, language and communication barriers were cited as detrimental to the acquisition of knowledge. “We have a bit of a problem in English. In Punjabi, we can ask something in full. We can ask questions in full: What is this? What is that? What isn’t it? In English, we don’t always understand everything.” (71) Sometimes patients had to rely on friends or family to interpret information provided by the health care provider, which had the potential to upset customary parent/child roles, or result in crucial information being withheld (intentionally or unintentionally). (55) Participants who were able to communicate with a health care provider in their own language spoke positively about this opportunity and the cultural information that was shared, such as the implications of roti for cardiac health, (71) an issue that caused consternation for South Asian patients in another study. (50) The accessibility of patient education materials is also important. The use of pictures was suggested for people with low literacy levels, poor English skills, or lack of familiarity with North American food. (55, 60, 77) Translated patient education materials were helpful but did not alleviate the issue of English-only signage in stores and information on food labels. (60, 77)
Language is not the only communication barrier, however; cultural values related communication styles and preferences may also affect how information is understood and received. For example, Dussart (46) described people with diabetes from the Warlpiri Aboriginal group in Australia. For the Warlpiri, personal autonomy is a cultural value, and “advice” from health care professionals is often poorly received because “the imperative form and associated threats, so pervasive in bio-medical diagnosis and recommendations is an anathema to the Warlpiri people.” To ask a Warlpiri patient to refrain from eating a certain food would infringe on that person’s autonomy. (46)
Coping With Everyday Stress
All patients reported challenges related to routine events (such as co-ordinating family schedules); being forced to eat at particular times because of work; and avoiding convenience foods when busy. Patients who experienced higher levels of stress, or who had fewer resources to cope with stress, cited additional challenges that negatively affected attempts to modify their diet.
Healthy eating habits were described as particularly difficult to maintain for patients under emotional stress. (35, 45-47) A diagnosis of diabetes or heart disease in itself may be a cause of stress and/or fear, and for patients who had already experienced negative side effects from their disease, fear was also a commonly reported stressful emotion. (43, 78) Patients may require more support from health care providers to manage stress. (79)
Emotional stress was also linked to increased fatigue and decreased ability to cope with other life events, (80) resulting in frustration. For some participants, the idea of prioritizing their own physical and emotional well-being over that of their family was very challenging. (80) Similarly, emotional stress was reported when patients were asked to prioritize their own needs in other ways, such as preparing meals that were diet-friendly but not enjoyed by other family members, (81) or diverting limited financial resources to pay for more expensive healthy food, medication, or medical supplies. (42, 81)
Everyday stressors, such as busy work schedules, family responsibilities, or the need to co-ordinate meals for multiple family members with different time requirements and dietary preferences were also cited as barriers. (51, 54, 60, 80-83) This may be particularly challenging for diabetes patients, who are often instructed to eat at regular times every day. If work schedule, childcare responsibilities, or a family member’s schedule disrupted regular mealtimes, patients found it difficult to manage these challenges and find alternative solutions. (84) Some talked about the importance of routine and scheduling, including the need to anticipate difficulties that might arise due to family and work schedules, and to plan food and meals accordingly. (35, 41, 85)
Stress may have more of an impact on vulnerable people, who may have additional everyday stressors and fewer resources to cope. Additional stress can come from intermediate factors such as financial insecurity or discrimination; this may lead to physiologic responses, and both may affect dietary practices. (86) The pervasive stress of poverty, including emotional pressures and fear about not being able to make recommended changes, may compound everyday stressors. (42, 45, 73, 87) People who are living in a new place, far away from their customary way of life and comforts, may also experience increased stress. (49, 51, 52, 57, 78, 79)
Negotiating With Family Members
Considering the influence of spouses and family members on meal planning and eating practices is important, since “food and eating form a large part of the ‘normal’ but essential activities of families, across cultures.” (88) Consequently, any type of dietary modification involves some degree of negotiation with other members of the household. Family members, especially spouses, can be a positive or negative influence on dietary change. It is important to consider the role of family members when planning dietary modification interventions; since meal planning and preparation is a shared activity, interventions aimed at the patient alone may mean that the one who receives dietary advice is not the one who does the cooking or serving. (83) A number of papers specifically addressed the spousal relationship and its effect on dietary modification. (72, 89-92) Others focused on the family relationship. (48, 55, 59, 80, 81, 88, 93, 94) The influence of spouses and family members is very important; the actions of family members may enable or inhibit dietary change (or neither), and this influence may change over time. (90)
Support at home is universally described as an essential component of successful dietary modification. Support (emotional understanding, respect for needs) is differentiated from help (instrumental assistance in chores, physical tasks, financial help, informational assistance); both types of assistance were seen as important, but support was described as essential by some participants. (80) Positive support (e.g., encouraging, reminders, emotional support, empowering patient to make change independently) was more successful than negative support (e.g., nagging, monitoring, restricting). (72, 80, 90)
Positive support at home helps patients make better food-related decisions while maintaining the interpersonal relationships that are essential for emotional understanding. Emotional support from family members was helpful in encouraging patients to keep working, and to help them realize that dietary change was an achievable goal. (36, 85) Instrumental help from family members, such as buying only healthy food, was also an important part of the positive value of relationships. (35) Family and friends were a key source of emotional support; those who were living well with diabetes or heart disease often acted as role models for successful change. (59, 82) Some patients reported that their own diagnosis of diabetes inspired concern for other family members and was a positive motivator for dietary change. (95) In other households, family members had high expectations for the patient, and such concern was cited as a motivating factor to comply with dietary modifications. (48) However, the concern of family members was also described as stressful, especially when it was focused on an issue that the patient could or would not change, (59) or when repeated reminders/help changed a spousal partnership to a parent-child dynamic. (92) Overzealous attention from family members can cause patients to take less responsibility and exhibit less self-control, letting family members make food-related choices and monitor/control food intake. (72)
Dietary change for a single patient has the potential to improve the diet of the whole family, (81, 82, 94) but can also be the cause of disagreements. (48, 55) Patients struggled to avoid tempting food when family members consumed it in their presence. (59) Family members were seldom inspired to alter their own diets to support patients, (94) and some participants spoke of trying to make dietary modifications that family members wouldn’t notice, such as switching to sweetener from sugar in baking, (93) or pouring skim milk into a whole milk jug. (59)
The links between food and family are complex, influenced by family and broader cultures, and by gender roles related to cooking, meal planning, and diet modification. Several papers discussed how dietary modification might be different for male and female patients. (48, 51, 53-55, 57, 61, 68, 72, 75, 81, 82, 86, 93, 96) The female patients in Beverley’s study (72) perceived that they received less support from their husbands than male patients received from their wives. Peel (96) found that female diabetes patients tended to describe dietary modification as an individual challenge, but male patients described dietary modification as a family matter. In many families, women have the main responsibility for food preparation, although not always the final say over the menu. (48, 55, 72, 81, 93) Control over dietary routines did not necessarily mean success in implementing dietary modification, due to the food preferences of other family members. (81) Astin (55) observed that in South Asian families, the adaptation of family members to the patient’s diet was linked to gender: if the patient was male, the whole family would typically adopt the modified diet; if the patient was female, she would typically prepare separate food for herself, not wanting to subject other family members to her dietary restriction. Due to the extra time and effort involved in preparing a separate, modified meal, female patients were more likely to lapse into an unmodified diet. (55)
Other considerations that affected family relations included balancing cultural understandings of how to care for an ill person with Western biomedical instructions. For Chinese spouses, restricting food during illness may be counterintuitive: instead, “special foods and disease-specific medicinal foods should appropriately be provided for patients as both a means of supporting health and demonstrating family solicitousness.” (48)
Family culture is a significant influence on food perceptions and eating practices, shaping understanding of the role of food in daily life. (81) Sometimes this influence is negative (emphasizing the consumption of food that is outside of the diet plan), but sometimes it is positive. One woman spoke of watching her mother adopt a diabetes-friendly diet and noticing how her health improved; this observation inspired the daughter to make more of an effort with respect to her own dietary change. (81) Sometimes, family culture and food are inextricable: for example, baking and sharing birthday cakes is a way of demonstrating caring. (88) Not being able to participate in these food-based family rituals is a challenge for patients and family members.
Managing the Social Significance of Food
Many studies emphasized patient reports that maintaining diet modification was especially difficult when visiting or hosting friends and family members, and during holiday or social occasions. Because of the central role of food in social gatherings, patients often felt left out or separated when they could not consume special foods.
Participants commented that it was especially difficult to exercise self-discipline and refuse favourite foods during social situations. (36, 48, 73, 87, 95) Difficulty in following disease-specific diets during social occasions meant that some patients chose not to attend these functions, leading to feelings of isolation and withdrawal. (48) Eating differently in social situations may also result in stigma; patients reported feeling distressed when their diabetes was a focus of attention at social events because they were not eating the same food as others. (48, 87) As a result, attempts at diet modification were more likely to fail during social occasions. (36) Sociocultural expectations related to good hosting are also often linked to the amount and type of food that is served. Patients developed strategies for socializing in a diet-friendly way in their own homes, but when visiting others, many talked about the social difficulties of maintaining restrictive diets but not refusing hospitality. (81, 93) The social stigma related to refusing food may be stronger in some cultures than others; for instance, Filipino patients discussed the centrality of food in their familial and social relationships. (97)
Food also plays a central role in religious practice, and dietary restrictions may cause patients to feel alienated from their spiritual community. Many religious holidays have associated food traditions that are not congruent with diabetes- or heart-friendly diets. Similar to social occasions, religious holidays were frequently cited as times when it was most difficult to maintain healthy eating habits. (48, 52) For patients with diabetes who observe periods of religious fasting, it may be a struggle to maintain stable blood glucose levels, and they may choose not to participate in the fast for the sake of their health. (57) Culturally appropriate diet counselling for patients who wish to fast may include recommendations about how or to what extent they may participate in fasting activities.
For some patients, particular foods have significant cultural meaning and are intrinsically linked with identity and belonging. Studies focusing on Asian and South Asian patients often mentioned rice as a symbolically important food, one that was particularly difficult to restrict or omit. (40, 48-51, 97) Other patients mentioned roti, (50, 71) ghee, (52) or corn tortillas (36, 53, 76, 79) as culturally significant foods. Patients often mentioned that no alternatives to these foods were suggested by health care providers, (50) or that the suggested alternatives were unsatisfactory: “patients and families were challenged by being asked to restrict rice and change from familiar white ‘fragrant’ rice to foreign ‘chewy’ and ‘tasteless’ brown, red, or black rice. These challenges were persistently noted by participants who felt called upon to cope with this change in communal meals.” (48)
The link between food and cultural identity is strong. For immigrants, food is often a link to their culture of origin. In the Chinese diet, for example, rice is a multifaceted and nuanced symbol of holistic health and well-being. (48) For Filipino-Americans, rice is “viewed as a symbol of strength, sustenance, sacrifice, wealth, and togetherness and may be eaten at every meal. Reducing or eliminating rice from one’s diet may be perceived as rejecting Filipino culture.” (97) For African-Americans, food has a rich symbolism and meaning, with slavery often mentioned as the originating site of the symbolism and meaning of food: “food became wealth in that it was available for them to share and enjoy when no other tangible resources were truly their own. Power over the production, consumption, and distribution of food likely served to affirm the personhood and identity of the slaves in an environment that relegated them to the status of property.” (75) The social and cultural meaning rooted in this history may still affect the way that food is understood, and the place and meaning of food in the lives of African-American people.
Summary
To assist in challenges with self-discipline, health care providers can work with patients to create a diabetes- or heart-friendly diet that suits and satisfies their palate. Challenges related to knowledge may be partially addressed by recognizing the need for health information that is applicable and useful to patients’ specific circumstances; this includes the provision of culturally specific dietary recommendations and informational or counselling materials available in other languages or pictorial forms. Providers may also wish to address the role of food, emotions, and stress to help patients develop strategies and coping techniques. Support for patients’ diet modification also requires taking into account their role in the family, in meal preparation, and in social and religious communities. Dietary counselling that attends to these dimensions can better help patients meet related challenges. Providers must be aware of the types of challenges that all patients face and how these may be magnified in vulnerable populations, but they should also continue to see their patients as individuals with unique experiences and circumstances.
Limitations
Qualitative research provides theoretical and contextual insights into the experiences of limited numbers of people in specific settings. Qualitative research findings are not intended to generalize directly to populations, although meta-synthesis across a number of qualitative studies builds an increasingly robust understanding that is more likely to be transferable. While qualitative insights are robust and often enlightening for understanding experiences and planning services in other settings, the findings of the studies reviewed here—and of this synthesis—do not strictly generalize to the Ontario (or any specific) population. Findings are limited to the conditions included in the body of literature synthesized (i.e., diabetes and heart disease). The types of vulnerability discussed here reflect those seen in the literature; many other types of vulnerability may impact dietary modification, but may not have been studied, or may have been excluded as part of the search criteria (e.g. substance abuse, mental health issues). This evidence must be interpreted and applied carefully, in light of expertise and the experiences of the relevant community.
Conclusions
Diet modification is not simply a matter of knowing what to eat and making the rational choice to change dietary practices. Rather, diet and eating practices should be considered as part of the situated lives of patients, requiring an individualized approach that is responsive to the conditions in which each patient is attempting to make a change. Common challenges include self-discipline, knowledge, coping with everyday stress, negotiating with family members, and managing the social significance of food. An individualized approach is particularly important when working with patients who have vulnerabilities.
Acknowledgements
Editorial Staff
Pierre Lachaine
Jeanne McKane, CPE, ELS(D)
Amy Zierler, BA
Medical Information Services
Kaitryn Campbell, BA(H), BEd, MLIS
Kellee Kaulback, BA(H), MISt
Expert Panel for Health Quality Ontario: Optimizing Chronic Disease Management in the Community (Outpatient) Setting.
| Name | Title | Organization |
|---|---|---|
| Shirlee Sharkey (chair) | President & CEO | Saint Elizabeth Health Care |
| Theresa Agnew | Executive Director | Nurse Practitioners’ Association of Ontario |
| Onil Bhattacharrya | Clinician Scientist | Li Ka Shing Knowledge Institute, St. Michael’s Hospital, University of Toronto |
| Arlene Bierman | Ontario Women’s Health Council Chair in Women’s Health | Department of Medicine, Keenan Research Centre in the Li Ka Shing Knowledge Institute, St. Michael’s Hospital, University of Toronto |
| Susan Bronskill | Scientist | Institute for Clinical Evaluative Sciences |
| Catherine Demers | Associate Professor | Division of Cardiology, Department of Medicine, McMaster University |
| Alba Dicenso | Professor | School of Nursing, McMaster University |
| Mita Giacomini | Professor | Centre of Health Economics & Policy Analysis, Department of Clinical Epidemiology & Biostatistics |
| Ron Goeree | Director | Programs for Assessment of Technology in Health (PATH) Research Institute, St. Joseph’s Healthcare Hamilton |
| Nick Kates | Senior Medical Advisor | Health Quality Ontario – QI McMaster University Hamilton Family Health Team |
| Murray Krahn | Director | Toronto Health Economics and Technology Assessment (THETA) Collaborative, University of Toronto |
| Wendy Levinson | Sir John and Lady Eaton Professor and Chair | Department of Medicine, University of Toronto |
| Raymond Pong | Senior Research Fellow and Professor | Centre for Rural and Northern Health Research and Northern Ontario School of Medicine, Laurentian University |
| Michael Schull | Deputy CEO & Senior Scientist | Institute for Clinical Evaluative Sciences |
| Moira Stewart | Director | Centre for Studies in Family Medicine, University of Western Ontario |
| Walter Wodchis | Associate Professor | Institute of Health Management Policy and Evaluation, University of Toronto |
Appendices
Appendix 1: Literature Search Strategies
Mega Filter: OVID MEDLINE
Interviews+
(theme$ or thematic).mp.
qualitative.af.
Nursing Methodology Research/
questionnaire$.mp.
ethnological research.mp.
ethnograph$.mp.
ethnonursing.af.
phenomenol$.af.
(grounded adj (theor$ or study or studies or research or analys?s)).af.
(life stor$ or women* stor$).mp.
(emic or etic or hermeneutic$ or heuristic$ or semiotic$).af. or (data adj 1 saturat$).tw. or participant observ$.tw.
(social construct$ or (postmodern$ or post- structural$) or (post structural$ or poststructural$) or post modern$ or post-modern$ or feminis$ or interpret$).mp.
(action research or cooperative inquir$ or co operative inquir$ or co- operative inquir$).mp.
(humanistic or existential or experiential or paradigm$).mp.
(field adj (study or studies or research)).tw.
human science.tw.
biographical method.tw.
theoretical sampl$.af.
((purpos$ adj4 sampl$) or (focus adj group$)).af.
(account or accounts or unstructured or open-ended or open ended or text$ or narrative$).mp.
(life world or life-world or conversation analys?s or personal experience$ or theoretical saturation).mp
(lived or life adj experience$.mp
cluster sampl$.mp.
observational method$.af.
content analysis.af.
(constant adj (comparative or comparison)).af.
((discourse$ or discurs$) adj3 analys?s).tw.
narrative analys?s.af.
heidegger$.tw.
colaizzi$.tw.
spiegelberg$.tw.
(van adj manen$).tw.
(van adj kaam$).tw.
(merleau adj ponty$).tw
.husserl$.tw
foucault$.tw.
(corbin$ adj2 strauss$).tw
-
glaser$.tw.
NOT
p =.ti,ab.
p<.ti,ab.
p>.ti,ab.
p =.ti,ab.
p<.ti,ab.
p>.ti,ab.
p-value.ti,ab.
retrospective.ti,ab.
regression.ti,ab.
statistical.ti,ab.
Mega Filter: EBSCO Cumulative Index to Nursing & Allied Health Literature (CINAHL)
Interviews+
MH audiorecording
MH Grounded theory
MH Qualitative Studies
MH Research, Nursing
MH Questionnaires+
MH Focus Groups (12639)
MH Discourse Analysis (1176)
MH Content Analysis (11245)
MH Ethnographic Research (2958)
MH Ethnological Research (1901)
MH Ethnonursing Research (123)
MH Constant Comparative Method (3633)
MH Qualitative Validity+ (850)
MH Purposive Sample (10730)
MH Observational Methods+ (10164)
MH Field Studies (1151)
MH theoretical sample (861)
MH Phenomenology (1561)
MH Phenomenological Research (5751)
MH Life Experiences+ (8637)
MH Cluster Sample+ (1418)
Ethnonursing (179)
ethnograph* (4630)
phenomenol* (8164)
grounded N1 theor* (6532)
grounded N1 study (601)
grounded N1 studies (22)
grounded N1 research (117)
grounded N1 analys?s (131)
life stor* (349)
women’s stor* (90)
emic or etic or hermeneutic$ or heuristic$ or semiotic$ (2305)
data N1 saturat* (96)
participant observ* (3417)
social construct* or postmodern* or post-structural* or post structural* or poststructural* or post modern* or post-modern* or feminis* or interpret* (25187)
action research or cooperative inquir* or co operative inquir* or co-operative inquir* (2381)
humanistic or existential or experiential or paradigm* (11017)
field N1 stud* (1269)
field N1 research (306)
human science (132)
biographical method (4)
theoretical sampl* (983)
purpos* N4 sampl* (11299)
focus N1 group* (13775)
account or accounts or unstructured or open-ended or open ended or text* or narrative* (37137)
life world or life-world or conversation analys?s or personal experience* or theoretical saturation (2042)
lived experience* (2170)
life experience* (6236)
cluster sampl* (1411)
theme* or thematic (25504)
observational method* (6607)
questionnaire* (126686)
content analysis (12252)
discourse* N3 analys?s (1341)
discurs* N3 analys?s (35)
constant N1 comparative (3904)
constant N1 comparison (366)
narrative analys?s (312)
Heidegger* (387)
Colaizzi* (387)
Spiegelberg* (0)
van N1 manen* (261)
van N1 kaam* (34)
merleau N1 ponty* (78)
husserl* (106)
Foucault* (253)
Corbin* N2 strauss* (50)
strauss* N2 corbin* (88)
-
glaser* (302)
NOT
TI statistical OR AB statistical
TI regression OR AB regression
TI retrospective OR AB retrospective
TI p-value OR AB p-value
TI p< OR AB p<
TI p< OR AB p<
TI p= OR AB p=
Mega Filter: ISI Web of Science, Social Science Citation Index
TS=interview*
TS=(theme*)
TS=(thematic analysis)
TS=qualitative
TS=nursing research methodology
TS=questionnaire
TS=(ethnograph*)
TS= (ethnonursing)
TS=(ethnological research)
TS=(phenomenol*)
TS=(grounded theor*) OR TS=(grounded stud*) OR TS=(grounded research) OR TS=(grounded analys?s)
TS=(life stor*) OR TS=(women’s stor*)
TS=(emic) OR TS=(etic) OR TS=(hermeneutic) OR TS=(heuristic) OR TS=(semiotic) OR TS=(data saturat*) OR TS=(participant observ*)
TS=(social construct*) OR TS=(postmodern*) OR TS=(post structural*) OR TS=(feminis*) OR TS=(interpret*)
TS=(action research) OR TS=(co-operative inquir*)
TS=(humanistic) OR TS=(existential) OR TS=(experiential) OR TS=(paradigm*)
TS=(field stud*) OR TS=(field research)
TS=(human science)
TS=(biographical method*)
TS=(theoretical sampl*)
TS=(purposive sampl*)
TS=(open-ended account*) OR TS=(unstructured account) OR TS=(narrative*) OR TS=(text*)
TS=(life world) OR TS=(conversation analys?s) OR TS=(theoretical saturation)
TS=(lived experience*) OR TS=(life experience*)
TS=(cluster sampl*)
TS=observational method*
TS=(content analysis)
TS=(constant comparative)
TS=(discourse analys?s) or TS =(discurs* analys?s)
TS=(narrative analys?s)
TS=(heidegger*)
TS=(colaizzi*)
TS=(spiegelberg*)
TS=(van manen*)
TS=(van kaam*)
TS=(merleau ponty*)
TS=(husserl*)
TS=(foucault*)
TS=(corbin*)
TS=(strauss*)
-
TS=(glaser*)
NOT
TS=(p-value)
TS=(retrospective)
TS=(regression)
TS=(statistical)
Suggested Citation
This report should be cited as follows: Vanstone M, Giacomini M, Smith A, Brundisini F, DeJean D, Winsor S. How diet challenges are magnified in vulnerable or marginalized people with diabetes and heart disease: a systematic review and qualitative meta-synthesis. Ont Health Technol Assess Ser [Internet]. 2013 September;13(14):1-40. Available from: http://www.hqontario.ca/en/documents/eds/2013/full-report-OCDM-diet-challenges.pdf.
Indexing
The Ontario Health Technology Assessment Series is currently indexed in MEDLINE/PubMed, Excerpta Medica/EMBASE, and the Centre for Reviews and Dissemination database.
Permission Requests
All inquiries regarding permission to reproduce any content in the Ontario Health Technology Assessment Series should be directed to: EvidenceInfo@hqontario.ca.
How to Obtain Issues in the Ontario Health Technology Assessment Series
All reports in the Ontario Health Technology Assessment Series are freely available in PDF format at the following URL: http://www.hqontario.ca/en/mas/mas_ohtas_mn.html.
Conflict of Interest Statement
All reports in the Ontario Health Technology Assessment Series are impartial. There are no competing interests or conflicts of interest to declare.
Peer Review
All reports in the Ontario Health Technology Assessment Series are subject to external expert peer review. Additionally, Health Quality Ontario posts draft reports and recommendations on its website for public comment prior to publication. For more information, please visit: http://www.hqontario.ca/en/mas/ohtac_public_engage_overview.html.
About Health Quality Ontario
Health Quality Ontario (HQO) is an arms-length agency of the Ontario government. It is a partner and leader in transforming Ontario’s health care system so that it can deliver a better experience of care, better outcomes for Ontarians and better value for money.
Health Quality Ontario strives to promote health care that is supported by the best available scientific evidence. HQO works with clinical experts, scientific collaborators and field evaluation partners to develop and publish research that evaluates the effectiveness and cost-effectiveness of health technologies and services in Ontario.
Based on the research conducted by HQO and its partners, the Ontario Health Technology Advisory Committee (OHTAC) — a standing advisory sub-committee of the HQO Board — makes recommendations about the uptake, diffusion, distribution or removal of health interventions to Ontario’s Ministry of Health and Long-Term Care, clinicians, health system leaders and policy-makers.
This research is published as part of Ontario Health Technology Assessment Series, which is indexed in CINAHL, EMBASE, MEDLINE, and the Centre for Reviews and Dissemination. Corresponding OHTAC recommendations and other associated reports are also published on the HQO website. Visit http://www.hqontario.ca for more information.
About the Ontario Health Technology Assessment Series
To conduct its comprehensive analyses, HQO and/or its research partners reviews the available scientific literature, making every effort to consider all relevant national and international research; collaborates with partners across relevant government branches; consults with clinical and other external experts and developers of new health technologies; and solicits any necessary supplemental information.
In addition, HQO collects and analyzes information about how a health intervention fits within current practice and existing treatment alternatives. Details about the diffusion of the intervention into current health care practices in Ontario add an important dimension to the review. Information concerning the health benefits; economic and human resources; and ethical, regulatory, social, and legal issues relating to the intervention assist in making timely and relevant decisions to optimize patient outcomes.
The public consultation process is available to individuals and organizations wishing to comment on reports and recommendations prior to publication. For more information, please visit: http://www.hqontario.ca/en/mas/ohtac_public_engage_overview.html.
Disclaimer
This report was prepared by HQO or one of its research partners for the Ontario Health Technology Advisory Committee and developed from analysis, interpretation, and comparison of scientific research. It also incorporates, when available, Ontario data and information provided by experts and applicants to HQO. It is possible that relevant scientific findings may have been reported since completion of the review. This report is current to the date of the literature review specified in the methods section, if available. This analysis may be superseded by an updated publication on the same topic. Please check the HQO website for a list of all publications: http://www.hqontario.ca/en/mas/mas_ohtas_mn.html.
Health Quality Ontario
130 Bloor Street West, 10th Floor
Toronto, Ontario
M5S 1N5
Tel: 416-323-6868
Toll Free: 1-866-623-6868
Fax: 416-323-9261
Email: EvidenceInfo@hqontario.ca
ISSN 1915-7398 (online)
ISBN 978-1-4606-1246-0 (PDF)
© Queen’s Printer for Ontario, 2013
List of Tables
List of Figures
| Figure 1: Citation Flow Chart |
List of Abbreviations
- CAD
Coronary artery disease
- OHTAC
Ontario Health Technology Advisory Committee
References
- 1.Public Health Agency of Canada. Diabetes in Canada: facts and figures from a public health perspective. Ottawa (ON): Public Health Agency of Canada. 2011. Jul 4, p. 123.
- 2.Public Health Agency of Canada. 2009 tracking heart disease and stroke in Canada. Ottawa (ON): Public Health Agency of Canada. 2009. Jun 10, [[cited 2013 April 9]]. p. 132. [Internet] Available from: http://www.phac-aspc.gc.ca/publicat/2009/cvd-avc/report-rapport-eng.php .
- 3.Redfield MM, Jacobsen SJ, Burnett JC, Mahoney DW, Bailey KR, Rodeheffer RJ, et al. Burden of systolic and diastolic ventricular dysfunction in the community: appreciating the scope of the heart failure epidemic. JAMA. 2003;289(2):194–202. doi: 10.1001/jama.289.2.194. [DOI] [PubMed] [Google Scholar]
- 4.Ammar KA, Jacobsen SJ, Mahoney DW, Kors JA, Redfield MM, Burnett JC, et al. Prevalence and prognostic significance of heart failure stages: application of the American College of Cardiology/American Heart Association heart failure staging criteria in the community. Circulation. 2007;115(12):1563–70. doi: 10.1161/CIRCULATIONAHA.106.666818. [DOI] [PubMed] [Google Scholar]
- 5.Nattel S, et al. New ideas about atrial fibrillation 50 years on. Nature. 2002;415(6868):219–26. doi: 10.1038/415219a. [DOI] [PubMed] [Google Scholar]
- 6.Ontario Ministry of Health and Long-Term Care. Health equity impact assessment workbook. Toronto(ON): Ontario Ministry of Health and Long-Term Care. Spring. 2012. p. 43. Report No.: HEIA Version 2.0.
- 7.Flaskerud JH, Winslow BJ, et al. Conceptualizing vulnerable populations health-related research. Nurs Res. 1998;47(2):69–78. doi: 10.1097/00006199-199803000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Ruof M, et al. Vulnerability, vulnerable populations and policy. Kennedy Inst Ethics J. 2004;14(4):411–25. doi: 10.1353/ken.2004.0044. [DOI] [PubMed] [Google Scholar]
- 9.Delor F, Hubert M, et al. Revisiting the concept of ‘vulnerability’. Soc Sci Med. 2000;50:1557–70. doi: 10.1016/s0277-9536(99)00465-7. [DOI] [PubMed] [Google Scholar]
- 10.Spiers J, et al. New perspectives on vulnerability using emic and etic approaches. J Adv Nurs. 2000;31(2):715–21. doi: 10.1046/j.1365-2648.2000.01328.x. [DOI] [PubMed] [Google Scholar]
- 11.Rogers A, et al. Vulnerability, health and health care. J Adv Nurs. 1997;26:65–72. doi: 10.1046/j.1365-2648.1997.1997026065.x. [DOI] [PubMed] [Google Scholar]
- 12.Canadian Diabetes Association. 2008 clinical practice guidelines for the prevention and management of diabetes in Canada. Can J Diabetes. 2008;32 Suppl(1):S1–S201. doi: 10.1016/j.jcjd.2013.01.009. [DOI] [PubMed] [Google Scholar]
- 13.Genest J, McPherson R, Frohlich J, Anderson T, Carpentier A, Couture P, et al. 2009 Canadian Cardiovascular Society Canadian guidelines for the diagnosis and treatment of dyslipidemia and prevention of cardiovascular disease in the adult-2009 recommendations. Can J Cardiol. 2009;25(10):567–79. doi: 10.1016/s0828-282x(09)70715-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM, et al. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care. 2002;25(7):1159–71. doi: 10.2337/diacare.25.7.1159. [DOI] [PubMed] [Google Scholar]
- 15.Wilczynski NL, Marks S, Haynes RB, et al. Search strategies for identifying qualitative studies in CINAHL. Qualitative health research. 2007;17:705–10. doi: 10.1177/1049732306294515. [DOI] [PubMed] [Google Scholar]
- 16.Shaw RL, Booth A, Sutton AJ, Miller T, Smith Ja, Young B, et al. Finding qualitative research: an evaluation of search strategies. BMC Med Res Methodol. 2004;(4):5. doi: 10.1186/1471-2288-4-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wong S, Wilczynski NL, Haynes RB, et al. Developing optimal search strategies for detecting clinically relevant qualitative studies in MEDLINE. Stud Health Technol Inform. 2004;107(1):311–6. [PubMed] [Google Scholar]
- 18.Sandelowski M, Barroso J, et al. Creating metasummaries of qualitative findings. Nurs Res. 2003;52(4):226–33. doi: 10.1097/00006199-200307000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Sandelowski M, Barroso J, et al. Toward a metasynthesis of qualitative findings on motherhood in HIV-positive women. Res Nurs Health. 2003;26(2):153–70. doi: 10.1002/nur.10072. [DOI] [PubMed] [Google Scholar]
- 20.Sandelowski M, Barroso J, et al. Handbook for synthesizing qualitative research. New York: Springer. 2006 [Google Scholar]
- 21.Thorne S, Jenson L, Kearney M, Noblit G, Sandelowski M, et al. Qualitative metasynthesis: reflections on methodological orientation and ideological agenda. Qual Health Res. 2004;14:1342–65. doi: 10.1177/1049732304269888. [DOI] [PubMed] [Google Scholar]
- 22.Saini M, Shlonsky A, et al. Systematic synthesis of qualitative research. Tripodi T, editor. New York: Oxford University Press. 2012 [Google Scholar]
- 23.Corbin JM, et al. Basics of qualitative research: techniques and procedures for developing grounded theory. 3rd ed. Strauss AL, editor. Los Angeles: Sage. 2008 [Google Scholar]
- 24.Charmaz K, et al. Constructing grounded theory: a practical guide through qualitative analysis. London: Sage. 2006 [Google Scholar]
- 25.Finfgeld DL, et al. Metasynthesis: The state of the art—so far. Qual Health Res. 2003;13(7):893–904. doi: 10.1177/1049732303253462. [DOI] [PubMed] [Google Scholar]
- 26.Health Quality Ontario. Specialized community-based care: an evidence-based analysis. Ont Health Technol Assess Ser [Internet] 2012 Nov;12(20):1–60. Available from: www.hqontario.ca/en/mas/tech/pdfs/2012/full-report-specialized-care.pdf . [PMC free article] [PubMed] [Google Scholar]
- 27.Melia KM, et al. Handbook of qualitative research. Bourgeault I, DeVries R, Dingwall R, editors. Thousand Oaks (CA): Sage; 2010. Recognizing quality in qualitative research. :559–74. [Google Scholar]
- 28.Sandelowski M, Barroso J, et al. Finding the findings in qualitative studies. J Nurs Scholarsh. 2002;34(3):213–9. doi: 10.1111/j.1547-5069.2002.00213.x. [DOI] [PubMed] [Google Scholar]
- 29.Noblit G, Hare RD, et al. Meta-ethnography: synthesizing qualitative studies. Newbury Park: Sage Publications. 1988 [Google Scholar]
- 30.Paterson B, et al. Coming out as ill: understanding self-disclosure in chronic illness from a meta-synthesis of qualitative research. Reviewing Res Evidence Nurs Pract. 2007:73–83. [Google Scholar]
- 31.Finfgeld-Connett D, et al. Meta-synthesis of presence in nursing. J Adv Nurs. 2006;55(6):708–14. doi: 10.1111/j.1365-2648.2006.03961.x. [DOI] [PubMed] [Google Scholar]
- 32.Barnett-Page E, Thomas J, et al. Methods for the synthesis of qualitative research: a critical review. BMC Med Res Methodol. 2009;9(1):59. doi: 10.1186/1471-2288-9-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Smith DE, et al. The everyday world as problematic: a feminist sociology. Boston: Northeastern University Press. 1987 [Google Scholar]
- 34.Broom D, Whittaker A, et al. Controlling diabetes, controlling diabetics: moral language in the management of diabetes type 2. Soc Sci Med. 2004;58(11):2371–82. doi: 10.1016/j.socscimed.2003.09.002. [DOI] [PubMed] [Google Scholar]
- 35.Gutschall M, Onega LL, Wright WK, et al. Patients’ perspectives about dietary maintenance in Type 2 diabetes. Top Clin Nutr. 2011;26(3):180–9. [Google Scholar]
- 36.Early KB, Shultz JA, Corbett C, et al. Assessing diabetes dietary goals and self-management based on in-depth interviews with Latino and Caucasian clients with type 2 diabetes. J Transcult Nurs. 2009;20(4):371–81. doi: 10.1177/1043659609334928. [DOI] [PubMed] [Google Scholar]
- 37.Gazmararian JA, Ziemer DC, Barnes C, et al. Perception of barriers to self-care management among diabetic patients. Diabetes Educ. 2009;35(5):778–88. doi: 10.1177/0145721709338527. [DOI] [PubMed] [Google Scholar]
- 38.Onwudiwe NC, Mullins CD, Winston RA, Shaya FT, Pradel FG, Laird A, et al. Barriers to self-management of diabetes: a qualitative study among low-income minority diabetics. Ethn Dis. 2011;21(1):27–32. [PubMed] [Google Scholar]
- 39.White S, Bissell P, Anderson C, et al. A qualitative study of cardiac rehabilitation patients’ perspectives on making dietary changes. J Hum Nutr Diet. 2011;24(2):122–7. doi: 10.1111/j.1365-277X.2010.01136.x. [DOI] [PubMed] [Google Scholar]
- 40.McCloskey J, Flenniken D, et al. Overcoming cultural barriers to diabetes control: a qualitative study of southwestern New Mexico Hispanics. J Cult Divers. 2010;17(3):110–5. [PubMed] [Google Scholar]
- 41.Balfe M, et al. Diets and discipline: the narratives of practice of university students with type 1 diabetes. Sociol Health Illn. 2007;29(1):136–53. doi: 10.1111/j.1467-9566.2007.00476.x. [DOI] [PubMed] [Google Scholar]
- 42.Nagelkerk J, Reick K, Meengs L, et al. Perceived barriers and effective strategies to diabetes self-management. J Adv Nurs. 2006;54(2):151–8. doi: 10.1111/j.1365-2648.2006.03799.x. [DOI] [PubMed] [Google Scholar]
- 43.Doyle B, Fitzsimons D, McKeown P, McAloon T, et al. Understanding dietary decision-making in patients attending a secondary prevention clinic following myocardial infarction. J Clin Nurs. 2012;21(1-2):32–41. doi: 10.1111/j.1365-2702.2010.03636.x. [DOI] [PubMed] [Google Scholar]
- 44.Heo S, Lennie TA, Moser DK, Okoli C, et al. Heart failure patients’ perceptions on nutrition and dietary adherence. Eur J Cardiovasc Nurs. 2009;8(5):323–8. doi: 10.1016/j.ejcnurse.2009.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Clark AM, Duncan AS, Trevoy JE, Heath S, Chan M, et al. Healthy diet in Canadians of low socioeconomic status with coronary heart disease: not just a matter of knowledge and choice. Heart Lung. 2011;40(2):156–63. doi: 10.1016/j.hrtlng.2010.01.007. [DOI] [PubMed] [Google Scholar]
- 46.Dussart F, et al. Diet, diabetes and relatedness in a central Australian Aboriginal settlement: some qualitative recommendations to facilitate the creation of culturally sensitive health promotion initiatives. Health Promot J Austr. 2009;20(3):202–7. doi: 10.1071/he09202. [DOI] [PubMed] [Google Scholar]
- 47.Jacobsson A, Pihl E, Martensson J, Fridlund B, et al. Emotions, the meaning of food and heart failure: a grounded theory study. J Adv Nurs. 2004;46(5):514–22. doi: 10.1111/j.1365-2648.2004.03025.x. [DOI] [PubMed] [Google Scholar]
- 48.Chesla CA, Chun KM, Kwan CML, et al. Cultural and family challenges to managing type 2 diabetes in immigrant Chinese Americans. Diabetes Care. 2009;32(10):1812–6. doi: 10.2337/dc09-0278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Culhane-Pera KA, Her C, Her B, et al. “We are out of balance here”: a Hmong cultural model of diabetes. J Immigr Minor Health. 2007;9(3):179–90. doi: 10.1007/s10903-006-9029-3. [DOI] [PubMed] [Google Scholar]
- 50.Lawton J, Ahmad N, Hanna L, Douglas M, Bains H, Hallowell N, et al. ‘We should change ourselves, but we can’t’: accounts of food and eating practices amongst British Pakistanis and Indians with type 2 diabetes. Ethn Health. 2008;13(4):305–19. doi: 10.1080/13557850701882910. [DOI] [PubMed] [Google Scholar]
- 51.Mellin-Olsen T, Wandel M, et al. Changes in food habits among Pakistani immigrant women in Oslo, Norway. Ethn Health. 2005;10(4):311–39. doi: 10.1080/13557850500145238. [DOI] [PubMed] [Google Scholar]
- 52.Mohan S, Wilkes L, Jackson D, et al. Lifestyle of Asian Indians with coronary heart disease: the Australian context. Collegian. 2008;15(3):115–21. doi: 10.1016/j.colegn.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 53.Benavides-Vaello S, Brown S, et al. Evaluating guiding questions for an ethnographic study of Mexican American women with diabetes. Hispanic Health Care Int. 2010;8(2):77–84. [Google Scholar]
- 54.Kieffer EC, Willis SK, Odoms-Young AM, Guzman JR, Allen AJ, Two Feathers J, et al. Reducing disparities in diabetes among African-American and Latino residents of Detroit: the essential role of community planning focus groups. Ethn Dis. 2004;14(3 Suppl 1) [PubMed] [Google Scholar]
- 55.Astin F, Atkin K, Darr A, et al. Family support and cardiac rehabilitation: a comparative study of the experiences of South Asian and White-European patients and their carer’s living in the United Kingdom. Eur J Cardiovasc Nurs. 2008;7(1):43–51. doi: 10.1016/j.ejcnurse.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 56.Burke NJ, et al. “...As soon as she stepped off the plane”: understanding and managing migration, chronic illness, and poverty in Albuquerque, New Mexico. Hum Organ. 2007;66(4):380–8. [Google Scholar]
- 57.Wallin AM, Lofvander M, Ahlstrom G, et al. Diabetes: a cross-cultural interview study of immigrants from Somalia. J Clin Nurs. 2007;16(11C):305–14. doi: 10.1111/j.1365-2702.2007.02099.x. [DOI] [PubMed] [Google Scholar]
- 58.Barton SS, Anderson N, Thommasen HV, et al. The diabetes experiences of Aboriginal people living in a rural Canadian community. Aust J Rural Health. 2005;13(4):242–6. doi: 10.1111/j.1440-1584.2005.00709.x. [DOI] [PubMed] [Google Scholar]
- 59.Lohri-Posey B, et al. Middle-aged Appalachians living with diabetes mellitus: a family affair. Fam Community Health. 2006;29(3):214–20. doi: 10.1097/00003727-200607000-00008. [DOI] [PubMed] [Google Scholar]
- 60.Mian SI, Brauer PM, et al. Dietary education tools for South Asians with diabetes. Can J Diet Pract Res. 2009;70(1):28–35. doi: 10.3148/70.1.2009.28. [DOI] [PubMed] [Google Scholar]
- 61.Skelly AH, Dougherty M, Gesler WM, Soward AC, Burns D, Arcury TA, et al. African American beliefs about diabetes. West J Nurs Res. 2006;28(1):9–29. doi: 10.1177/0193945905280298. [DOI] [PubMed] [Google Scholar]
- 62.Minicucci S, Paisley J, Mori M, Madill J, et al. Development and focus group testing of a healthy snack pamphlet for people living with diabetes. Can J Diabetes. 2002;26(2):120–4. [Google Scholar]
- 63.Malpass A, Andrews R, Turner KM, et al. Patients with type 2 diabetes experiences of making multiple lifestyle changes: a qualitative study. Patient Educ Couns. 2009;74(2):258–63. doi: 10.1016/j.pec.2008.08.018. [DOI] [PubMed] [Google Scholar]
- 64.Chun KM, Chesla CA, et al. Cultural issues in disease management for Chinese Americans with type 2 diabetes. Psychol Health. 2004;19(6):767–85. [Google Scholar]
- 65.Choudhury SM, Brophy S, Williams R, et al. Understanding and beliefs of diabetes in the UK Bangladeshi population. Diabet Med. 2009;26(6):636–40. doi: 10.1111/j.1464-5491.2009.02741.x. [DOI] [PubMed] [Google Scholar]
- 66.Fritschi C, Quinn L, Penckofer S, Surdyk PM, et al. Continuous glucose monitoring: the experience of women with type 2 diabetes. Diabetes Educ. 2010;36(2):250–7. doi: 10.1177/0145721709355835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Holmstrom IM, Rosenqvist U, et al. Misunderstandings about illness and treatment among patients with type 2 diabetes. J Adv Nurs. 2005;49(2):146–54. doi: 10.1111/j.1365-2648.2004.03274.x. [DOI] [PubMed] [Google Scholar]
- 68.Rahim-Williams B, et al. Beliefs, behaviors, and modifications of type 2 diabetes self-management among African American women. J Natl Med Assoc. 2011;103(3):203–15. doi: 10.1016/s0027-9684(15)30300-x. [DOI] [PubMed] [Google Scholar]
- 69.Coronado G, Thompson B, Tejeda S, Godina R, et al. Attitudes and beliefs among mexican americans about Type 2 diabetes. J Health Care Poor Underserved. 2004;15:576–88. doi: 10.1353/hpu.2004.0057. [DOI] [PubMed] [Google Scholar]
- 70.Wood F, Jacobson S, et al. Employee perceptions of diabetes education needs: a focus group study. AAOHN J. 2005;53(10):443–9. [PubMed] [Google Scholar]
- 71.Galdas PM, Kang HBK, et al. Punjabi Sikh patients’ cardiac rehabilitation experiences following myocardial infarction: a qualitative analysis. J Clin Nurs. 2010;19(21-22):3134–42. doi: 10.1111/j.1365-2702.2010.03430.x. [DOI] [PubMed] [Google Scholar]
- 72.Beverly EA, Miller CK, Wray LA, et al. Spousal support and food-related behavior change in middle-aged and older adults living with type 2 diabetes. Health Educ Behav. 2008;35(5):707–20. doi: 10.1177/1090198107299787. [DOI] [PubMed] [Google Scholar]
- 73.Chlebowy DO, Hood S, LaJoie AS, et al. Facilitators and barriers to self-management of type 2 diabetes among urban African American adults: focus group findings. Diabetes Educ. 2010;36(6):897–905. doi: 10.1177/0145721710385579. [DOI] [PubMed] [Google Scholar]
- 74.Greenhalgh T, Collard A, Campbell-Richards D, Vijayaraghavan S, Malik F, Morris J, et al. Storylines of self-management: narratives of people with diabetes from a multiethnic inner city population. J Health Serv Res Policy. 2011;16(1):37–43. doi: 10.1258/jhsrp.2010.009160. [DOI] [PubMed] [Google Scholar]
- 75.Liburd LC, et al. Food, identity, and African-American women with type 2 diabetes: an anthropological perspective. Diabetes Spectrum. 2003;16(3):160–5. [Google Scholar]
- 76.Abbott P, Davison J, Moore L, Rubinstein R, et al. Barriers and enhancers to dietary behaviour change for Aboriginal people attending a diabetes cooking course. Health Promot J Austr. 2010;21(1):33–8. doi: 10.1071/he10033. [DOI] [PubMed] [Google Scholar]
- 77.Bird SM, Wiles JL, Okalik L, Kilabuk J, Egeland GM, et al. Living with diabetes on Baffin Island: Inuit storytellers share their experiences. Can J Public Health. 2008;99(1):17–21. doi: 10.1007/BF03403734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sulaiman ND, Furler JS, Hadj EJ, Corbett HM, Young DY, et al. Stress, culture and ‘home’: social context in Turkish and Arabic-speaking Australians’ views of diabetes prevention. Health Promot J Austr. 2007;18(1):63–8. doi: 10.1071/he07063. [DOI] [PubMed] [Google Scholar]
- 79.Vincent D, Clark L, Zimmer LM, Sanchez J, et al. Using focus groups to develop a culturally competent diabetes self-management program for Mexican Americans. Diabetes Educ. 2006;32(1):89–97. doi: 10.1177/0145721705284372. [DOI] [PubMed] [Google Scholar]
- 80.Carter-Edwards L, Skelly AH, Cagle CS, Appel SJ, et al. “They care but don’t understand”: family support of African American women with type 2 diabetes. Diabetes Educ. 2004;30(3):493–501. doi: 10.1177/014572170403000321. [DOI] [PubMed] [Google Scholar]
- 81.Denham SA, Manoogian MM, Schuster L, et al. Managing family support and dietary routines: type 2 diabetes in rural Appalachian families. Families Syst Health. 2007;25(1):36–52. [Google Scholar]
- 82.Parker S, Hunter T, Briley C, Miracle S, Hermann J, Van Delinder J, et al. Formative assessment using social marketing principles to identify health and nutrition perspectives of Native American women living within the Chickasaw Nation boundaries in Oklahoma. J Nutr Educ Behav. 2011;43(1):55–62. doi: 10.1016/j.jneb.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 83.Penn L, Moffatt SM, White M, et al. Participants’ perspective on maintaining behaviour change: a qualitative study within the European Diabetes Prevention Study. BMC Public Health. 2008;8(235) doi: 10.1186/1471-2458-8-235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Rankin D, Cooke DD, Clark M, Heller S, Elliott J, Lawton J, et al. How and why do patients with Type 1 diabetes sustain their use of flexible intensive insulin therapy? A qualitative longitudinal investigation of patients’ self-management practices following attendance at a Dose Adjustment for Normal Eating (DAFNE) course. Diabet Med. 2011;28(5):532–8. doi: 10.1111/j.1464-5491.2011.03243.x. [DOI] [PubMed] [Google Scholar]
- 85.Karner A, Tingstrom P, Abrandt-Dahlgren M, Bergdahl B, et al. Incentives for lifestyle changes in patients with coronary heart disease. J Adv Nurs. 2005;51(3):261–75. doi: 10.1111/j.1365-2648.2005.03467.x. [DOI] [PubMed] [Google Scholar]
- 86.Schulz AJ, Zenk S, Odoms-Young A, Hollis-Neely T, Nwankwo R, Lockett M, et al. Healthy eating and exercising to reduce diabetes: exploring the potential of social determinants of health frameworks within the context of community-based participatory diabetes prevention. Am J Public Health. 2005;95(4):645–51. doi: 10.2105/AJPH.2004.048256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Cavanaugh CL, Taylor CA, Keim KS, Clutter JE, Geraghty ME, et al. Cultural perceptions of health and diabetes among Native American men. J Health Care Poor Underserved. 2008;19(4):1029–43. doi: 10.1353/hpu.0.0083. [DOI] [PubMed] [Google Scholar]
- 88.Gregory S, Bostock Y, Backett-Milburn K, et al. Recovering from a heart attack: a qualitative study into lay experiences and the struggle to make lifestyle changes. Fam Pract. 2006;23(2):220–5. doi: 10.1093/fampra/cmi089. [DOI] [PubMed] [Google Scholar]
- 89.Miller D, Brown JL, et al. Marital interactions in the process of dietary change for type 2 diabetes. J Nutr Educ Behav. 2005;37(5):226–34. doi: 10.1016/s1499-4046(06)60276-5. [DOI] [PubMed] [Google Scholar]
- 90.Paisley J, Beanlands H, Goldman J, Evers S, Chappell J, et al. Dietary change: what are the responses and roles of significant others? J Nutr Educ Behav. 2008;40(2):80–8. doi: 10.1016/j.jneb.2007.04.374. [DOI] [PubMed] [Google Scholar]
- 91.Trief PM, Sandberg J, Greenberg RP, Graff K, Castronova N, Yoon M, et al. Describing support: a qualitative study of couples living with diabetes. Families Syst Health. 2003;21(1):57–67. [Google Scholar]
- 92.Goldsmith DJ, Lindholm KA, Bute JJ, et al. Dilemmas of talking about lifestyle changes among couples coping with a cardiac event. Soc Sci Med. 2006;63(8):2079–90. doi: 10.1016/j.socscimed.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 93.Guell C, et al. Diabetes management as a Turkish family affair: chronic illness as a social experience. Ann Hum Biol. 2011;38(4):438–44. doi: 10.3109/03014460.2011.579577. [DOI] [PubMed] [Google Scholar]
- 94.Laroche HH, Heisler M, Forman J, Anderson M, Davis MM, et al. When adults with diabetes attempt to drink less soda: resulting adult-child interactions and household changes. J Natl Med Assoc. 1004;100(9):1004–11. doi: 10.1016/s0027-9684(15)31436-x. [DOI] [PubMed] [Google Scholar]
- 95.Wellard SJ, Rennie S, King R, et al. Perceptions of people with type 2 diabetes about self-management and the efficacy of community based services. Contemp Nurse. 2008;29(2):218–26. doi: 10.5172/conu.673.29.2.218. [DOI] [PubMed] [Google Scholar]
- 96.Peel E, Parry O, Douglas M, Lawton J, et al. Taking the biscuit? A discursive approach to managing diet in type 2 diabetes. J Health Psychol. 2005;10(6):779–91. doi: 10.1177/1359105305057313. [DOI] [PubMed] [Google Scholar]
- 97.Finucane ML, McMullen CK, et al. Making diabetes self-management education culturally relevant for Filipino Americans in Hawaii. Diabetes Educ. 2008;34(5):841–53. doi: 10.1177/0145721708323098. [DOI] [PubMed] [Google Scholar]


