Abstract
Ectopic pancreas in the mediastinum is extremely rare. We are reporting on a case of a twenty two year old woman who presented to our clinic with a large cervical mass. The CT scan revealed a cystic lesion in the anterior mediastinum. The patient underwent surgical resection by cervical approach. A Cystic mass with pseudocysts, cysts and complete pancreatic tissue were found in pathology. There were no signs of pancreatitis or malignancy. No recurrence was observed after a follow up of four years. We reviewed the case reports describing this rare condition in the medical literature.
We conclude that the possibility of ectopic pancreatic tissue should be included in the differential diagnosis of anterior mediastinal cystic mass, though as a remote possibility. Surgery is probably needed for the diagnosis and treatment. Posterior mediastinal pseudocyst is a different entity associated with acute pancreatitis. In those cases surgery is not recommended. Our third conclusion is that pancreatic tissue should be actively sought, if a structure resembling a pseudocyst is found in an unexpected location.
Virtual slides
The virtual slide(s) for this article can be found here: http://www.diagnosticpathology.diagnomx.eu/vs/1849369005957671
Keywords: Ectopic pancreas, Mediastinum, Computed tomography, Pseudocyst, Cyst
Background
Congenital ectopic pancreas is a known phenomena found in the gastrointestinal tract in about 2% of autopsies [1]. An ectopic pancreas arising from the anterior mediastinum is extremely rare. To the best of our knowledge, only a few cases [2-19] have been reported in the literature, all of them arising from the anterior mediastinum. A different phenomenon are the pseudocysts arising from the posterior mediastinum as a result of acute pancreatitis [20-26]. Ectopic tissue arising from the mediastinum might contain other organs like spleen and endometrium.
The first reported case was published in 1957 by Shillitoe and Wilson [2]. Herein we describe a case report of asymptomatic ectopic pancreas in the anterior mediastinum. In our case report pseudocysts and cysts were the main pathologic findings. We reviewed the cases published in the literature and distinguished between ectopic pancreas arising from the anterior mediastinum and ectopic pancreas arising from the posterior mediastinum.
Case presentation
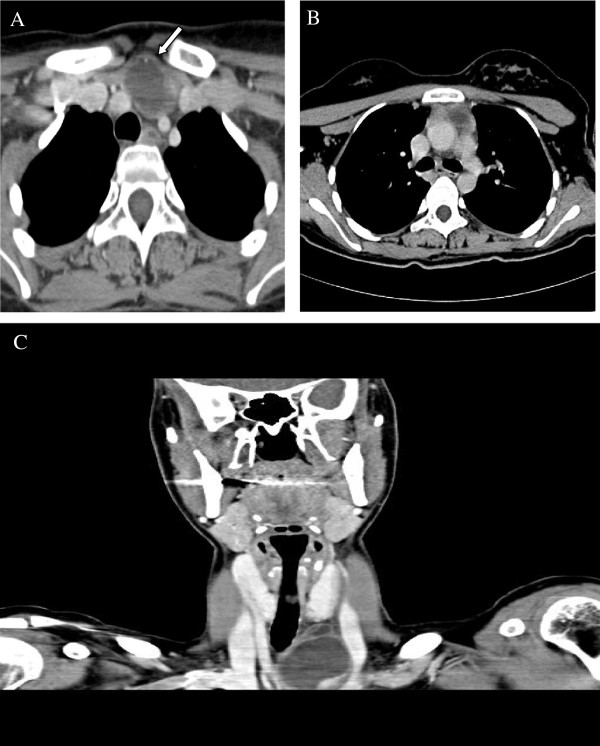
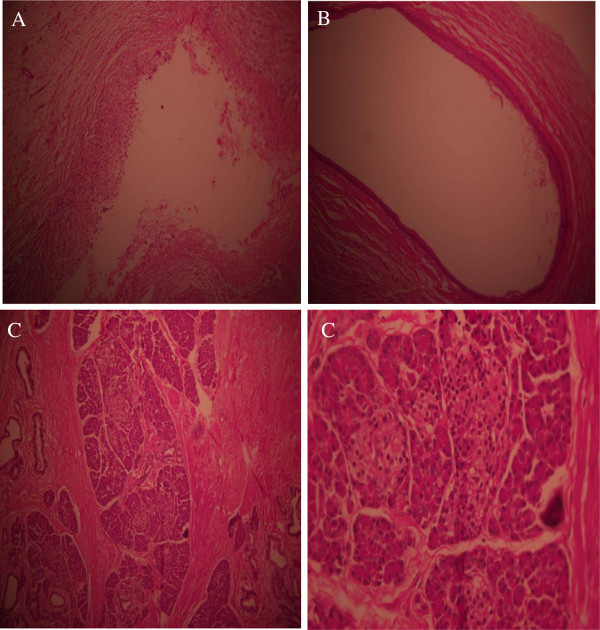
An otherwise healthy twenty two year old woman was sent to our hospital because of a left cervical mass. The mass was soft without tenderness and with no symptoms like chest pain, dyspnea or cough. The physical examination was unremarkable except the cervical mass. Blood tests including complete blood count, electrolytes and thyroid function tests were within the normal range. Cervical ultrasound revealed a left supraclvicular hypoechogenic lesion (2.4×3.8 cm). Chest computed tomography demonstrated a cystic mass in the anterior mediastinum protruding to the left cervical region, close to the left common carotid artery (Figure 1). Fine needle aspiration showed inflammatory cells without specific diagnosis and no signs of malignancy. Surgical resection was carried out by cervical approach. Pathology examination showed cystic masses along with pseudo cysts and a complete pancreatic tissue (including endocrine and exocrine tissue). There were no signs of malignancy (Figure 2). Surgical follow-up was uneventful. Four years after the operation the patient feels well with no signs of recurrence.
Figure 1.
Computed tomography images. Axial Computed Tomography images at the level of the thoracic inlet, show two adjacent cystic lesions, one in the anterior lower neck (A) measuring 3.8×2.3×5.1 cm and one in the anterior mediastinum on the left (B), measuring 2.7×2.2×1.8 cm. On coronal reconstruction (C) the neck lesion is shown as a lobular cystic mass with smooth enhancing rim. There is a speck of calcification at the cyst's wall (A, arrow).
Figure 2.
Pathology slides. Pathology slides show pseudo cyst (A), cyst (B) and pancreatic tissue endocrine and exocrine pancreas (C).
Review of the literature
We performed a Pub med search in order to find all the published cases of ectopic pancreatic tissue in the Mediastinum. We reviewed the cases in order to describe this rare condition (Table 1).
Table 1.
Ectopic pancreas in the anterior mediastinum- clinical features of 22 cases
| Reference | Gender | Age | Size (Cm) | Clinical presentation | Pathology |
|---|---|---|---|---|---|
| Shillitoe
[2] 1957 |
Female |
15 |
5.5 |
Dyspnea, Night sweats |
Benign |
| Carr
[3] 1977 |
Female |
57 |
10 |
None |
Benign |
| Von Schweinitz
[4] 1990 |
Male |
5 |
5 × 5 × 5 |
Chronic Pneumonia |
Benign |
| Perez-Ordonez
[5] 1996 |
Female |
16 |
12 |
None |
Benign |
| Gong
[6] 1997 |
Female |
26 |
20 × 15 |
Chest pain, Cough |
Benign |
| Gong
[6] 1997 |
Female |
26 |
4.3 × 1.3 |
Chest pain |
Benign |
| Wu
[7] 1998 |
Female |
60 |
10 × 5 |
Chest pain |
Benign |
| Cagirici
[8] 2001 |
Female |
45 |
10 × 8 |
Chest pain, cough |
Benign |
| Sentis
[9] 2004 |
Male |
44 |
10 × 8 × 7.5 |
Chest pain, Dyspnea |
Benign |
| Tamura
[10] 2005 |
Male |
39 |
10 × 8 |
Chest pain |
Benign |
| Al-Salam
[11] 2006 |
Male |
40 |
8 × 6 × 6 |
Cervical swelling |
Benign |
| Wang
[12] 2007 |
Female |
17 |
12 × 12 × 4 |
Chest pain, Dyspnea |
Benign |
| Wang
[12] 2007 |
Female |
24 |
10 × 8 × 4 |
Chest pain, Dyspnea |
Benign |
| Ehricht
[13] 2009 |
Male |
25 |
15 × 15 |
Pneumonia |
Benign |
| Chen
[14] 2009 |
Female |
32 |
13 × 16 × 8 |
None |
Benign |
| Fayoumi
[15] 2010 |
Male |
51 |
10 × 7 × 5 |
Chest pain, cough |
Benign |
| Fayoumi
[15] 2010 |
Male |
42 |
10 × 5 |
Shoulder pain |
Benign |
| Romain
[16] 2011 |
Female |
66 |
11 × 9 |
Chest pain |
Malignant |
| Takemura
[17] 2011 |
Female |
21 |
3.5 × 3.5 |
Chest pain |
Benign |
| Szabados
[18] 2012 |
Male |
32 |
4 × 4 |
Chest pain, Hemoptysis |
Benign |
| Byun CS
[19] 2012 |
Female |
31 |
7 × 3 × 4 |
Chest pain, cough, Hemoptysis |
Benign |
| Rokach |
Female |
22 |
5.1 × 3.8 × 2.3 |
None (Asymptomatic cervical mass) |
Benign |
| Summery/Average |
F-14 |
34 |
3.5-20 |
Sympomatic-18 |
Benign-21 |
| M-8 | Asymptomatic-4 | Malignant-1 |
In addition to our patient we found twenty one case reports of ectopic pancreas in the mediastinum. Fifteen case reports were written in English three in Chinese, two in German and one in Spanish. Most of the cases were described in young adults; Average age was thirty four and ages ranged from 5 to 66. The prevalence was higher in females (64% females). The clinical presentation was usually nonspecific including, chest pain, shoulder pain, shortness of breath, fever, neck swelling, night sweats, heart murmur, fatigue, chronic pulmonary infiltrate and tamponade. Four patients were asymptomatic at presentation. All the cases showed cystic lesions located in the anterior mediastinum. Most of the lesions were large ranging from 3.5 cm to 20 cm in diameter. Large lesions encompassed adjacent structures such as the great vessels. Associated findings were pleural effusions and pericardial effusions. There were no specific findings on the CT scan that could distinguish ectopic pancreatic tissue from other diagnosis. The cyst wall and the solid portion of the lesions usually showed mild to moderate enhancement with contrast material. The radiological appearance could not be distinguished from Thymoma, Lymphoma or Teratoma. In all cases the diagnosis was done only after surgery. Twenty one cases were benign and fully recovered after the operation and in a single case pancreatic carcinoma arising from the mediastinum was found. In the benign cases no recurrence was reported. The only patient with pancreatic adenocarcinoma died 15 months after the operation. This case strengthens the importance of surgery.
Ectopic pancreas in the mediastinum is a very rare condition. There are two theories on the embryogenesis of this anomalous development [4,8]. The first theory involves pluripotent epithelial cells of the ventral primary foregut underwent abnormal differentiation that led to the formation of ectopic pancreatic tissue in the anterior mediastinum. The second theory involves migration of cells from the pancreatic bud to a different site. Ectopic pancreas can be found in other locations as well. The most common site is the gastrointestinal tract. Pancreatic tissue is found there in two percent of autopsies.
A different entity is a pseudocyst arising from the posterior mediastinum as a result of acute pancreatitis [20-26]. In those cases extension of pancreatic necrosis into the mediastinum was possible via the aorta or the esophageal hiatus, through the diaphragmatic crura, or through erosion in the diaphragm.
Ectopic tissue in the mediastinum is a rare phenomenon. The anomalous development of ectopic tissue may occur due to abnormal differentiation of pluripotent cells, migration of ectopic cells or malignant transformation. A few case reports described this rare phenomenon. Hong Li et al. described a rare liposarcoma in the superior mediastinum [27]. The origin of this rare tumor was the Para pharyngeal region. Monika Saini et al. described intrapulmonary Teratoma attaching the medial mediastinum [28]. Composite lymphoma in the anterior mediastinum, a rare lymphoma from two different origins, was described by Guohua Yu et al. [29]. These cases represent malignant transformation. In our cases there were no signs of malignancy and the origin of the ectopic tissue was probably from abnormal differentiation of pluripotent cells or migration of ectopic cells.
Conclusions
The first reported case of ectopic mediastinal pancreas was published in 1957 by Shillitoe and Wilson [2]. They described a fifteen year old female that had benign ectopic pancreatic tissue in the anterior mediastinum. Ectopic Pancreas in the anterior Mediastinum is extremely rare. Only twenty one case reports were described in the literature, all in young adults. The lesions were solid-cystic. The pathology and the clinical course were benign in twenty cases and malignant in one case. There were no signs of pancreatitis. Posterior mediastinal pseudocyst is a different entity associated with acute pancreatitis. In those cases surgery is not recommended.
We conclude that ectopic pancreas should be considered in the differential diagnosis of anterior mediastinal lesions. Surgery is probably needed for the diagnosis and treatment. Pancreatic tissue should be actively sought, if a structure that looks like a pseudocyst is found in an unexpected location.
Consent
Written informed consent was obtained from the patient for the publication of this report and any accompanying images.
Contributor Information
Ariel Rokach, Email: rokach.ariel@gmail.com.
Gabriel Izbicki, Email: izbicki@szmc.org.il.
Maher Deeb, Email: deeb@szmc.org.il.
Naama Bogot, Email: bogotn@szmc.org.il.
Nissim Arish, Email: nissim.arish@gmail.com.
Irith Hadas-Halperen, Email: hadas@szmc.org.il.
Hava Azulai, Email: hava.az@gmail.com.
Abraham Bohadana, Email: abraham.bohadana@gmail.com.
Eli Golomb, Email: golomb@szmc.org.il.
References
- Lai EC, Tompkins RK. Heterotopic pancreas: review of a 26 year experience. Am J Surg. 1986;151:697–700. doi: 10.1016/0002-9610(86)90045-0. [DOI] [PubMed] [Google Scholar]
- Shillitoe AJ, Wilson JE. Enterogenous cyst of thorax with pancreatic tissue as a constituent. J Thorac Surg. 1957;34:810–814. [PubMed] [Google Scholar]
- Carr MJT, Deiraniya AK, Judd PA. Mediastinal cyst containing mural pancreatic tissue. Thorax. 1977;32:512–516. doi: 10.1136/thx.32.4.512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Von Schweinitz D, Wittekind C, Freihorst J. Mediastinaler sequester mit ektopem Pankreasgewebe [Mediastinal sequestration with ectopic pancreas] Z Kinderchir. 1990;45:249–250. [German] [PubMed] [Google Scholar]
- Perez-Ordonez B, Wesson DE, Smith CR. et al. A pancreatic cyst of the anterior mediastinum. Modern Pathol. 1996;9:210–214. [PubMed] [Google Scholar]
- Gong N, Fang G. Ectopic pancreas in within thorax: two case reports. Chin J Thorac Cardiovasc Surg. 1997;13:308. [Chinese] [Google Scholar]
- Wu J, Chen Y, Ni X. Ectopic pancreas in anterior mediastinal with pseudo-cyst: one case report. Chin J Thorac Cardiovasc Surg. 1998;14:214. doi: 10.1016/S1010-7940(98)00168-7. [Chinese] [DOI] [Google Scholar]
- Cagirici U, Ozbaran M, Veral A. et al. Ectopic mediastinal pancreas. Eur J Cardio-Thorac. 2001;19:514–515. doi: 10.1016/S1010-7940(01)00606-6. [DOI] [PubMed] [Google Scholar]
- Sentis MI, Sanchis JB, Garolera JMG. et al. Mediastinal enteric cyst: unusual clinical presentation and histopathology. Arch Bronconeumol. 2004;40:185–187. [Spanish] [PubMed] [Google Scholar]
- Tamura Y, Takahama M, Kushibe K. et al. Ectopic pancreas in the anterior mediastinum. Jpn J Thorac Cardiovasc Surg. 2005;53:498–501. doi: 10.1007/s11748-005-0095-6. [DOI] [PubMed] [Google Scholar]
- Al-Salam S, Al AM. Ectopic pancreatic tissue in the anterior mediastinum. Virchows Arch. 2006;448:661–663. doi: 10.1007/s00428-006-0159-8. [DOI] [PubMed] [Google Scholar]
- Wang W, Li KC, Qin W. et al. Ectopic pancreas in mediastinum report of 2 cases and review of the literature. J Thorac Imag. 2007;22:256–258. doi: 10.1097/01.rti.0000213587.44719.a7. [DOI] [PubMed] [Google Scholar]
- Ehricht A, Putzschler F, Weissmann K. et al. Ektopes Pankreasgewebe in einer Mediastinalzyste - eine seltene klinische Manifestation. [Ectopic pancreatic tissue within a mediastinal cyst—a rare clinical manifestation] Zentralbl Chir. 2009;134:178–181. doi: 10.1055/s-2008-1076882. [German] [DOI] [PubMed] [Google Scholar]
- Chen ZH, Yu RS, Dong F. et al. CT findings of an ectopic pancreas in the anterior mediastinum. Korean J Radiol. 2009;10:527–530. doi: 10.3348/kjr.2009.10.5.527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fayoumi S, Al-Husseini L, Jalil R. et al. Ectopic pancreatic tissue in the thoracic cavity: report of two cases. Ann Thorac Surg. 2010;90:25–27. doi: 10.1016/j.athoracsur.2010.05.059. [DOI] [PubMed] [Google Scholar]
- Romain PS, Muehlebach G, Damjanov I. et al. Adenocarcinoma arising in an ectopic mediastinal pancreas. Ann Diagn Pathol. 2012;16:494–497. doi: 10.1016/j.anndiagpath.2011.04.005. [DOI] [PubMed] [Google Scholar]
- Takemura M, Yoshida K, Morimura K. Thoracoscopic resection of thoracic esophageal duplication cyst containing ectopic pancreatic tissue in adult. J Cardiothorac Surg. 2011;6:118. doi: 10.1186/1749-8090-6-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szabados S, Lénárd L, Tornóczky T. et al. Ectopic pancreas tissue appearing in mediastinal cyst. J Cardiothorac Surg. 2012;7:22. doi: 10.1186/1749-8090-7-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byun CS, Park IK, Kim H. et al. Ectopic pancreas with hemorrhagic cystic change in the anterior mediastinum. Korean J Thorac Cardiovasc Surg. 2012;45:131–133. doi: 10.5090/kjtcs.2012.45.2.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirchner SG, Heller RM, Smith CW. Pancreatic pseudocyst of the mediastinum. Radiology. 1977;123:37–42. doi: 10.1148/123.1.37. [DOI] [PubMed] [Google Scholar]
- Owens GR, Arger PH, Mulhern CB. et al. CT evaluation of mediastinal pseudocyst. J Comput Assist Tomogr. 1980;4:256–259. doi: 10.1097/00004728-198004000-00028. [DOI] [PubMed] [Google Scholar]
- Maier W, Roscher R, Malfertheiner P. et al. Pancreatic pseudocyst of the mediastinum evaluated by CT. Eur J Radiol. 1986;6:70–72. [PubMed] [Google Scholar]
- Crombleholme TM, deLorimier AA, Adzick NS. et al. Mediastinal pancreatic pseudocysts in children. J Pediatr Surg. 1990;25:843–845. doi: 10.1016/0022-3468(90)90188-F. [DOI] [PubMed] [Google Scholar]
- Rose EA, Haider M, Yang SK, Telmos AJ. Mediastinal extension of a pancreatic pseudocyst. Gastroenterol. 2000;95:3638–3639. doi: 10.1111/j.1572-0241.2000.03387.x. [DOI] [PubMed] [Google Scholar]
- Winsett MZ, Amparo EG, Fagan CJ. et al. MR imaging of mediastinal pseudocyst. J Comput Assist Tomogr. 1988;12:320–322. doi: 10.1097/00004728-198803000-00024. [DOI] [PubMed] [Google Scholar]
- Karantanas AH, Sandris V, Tsikrika A. et al. Extension of Pancreatic Pseudocysts into the Neck: CT and MR Imaging Findings. AJR. 2003;180:843–845. doi: 10.2214/ajr.180.3.1800843. [DOI] [PubMed] [Google Scholar]
- Li H, Zhou X, Ran Q, Wang L. Parapharyngeal liposarcoma: a case report. Diagn Pathol. 2013;42:1596–1598. doi: 10.1186/1746-1596-8-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saini ML, Krishnamurthy S, Kumar RV. Intrapulmonary mature Teratoma. Diagn Pathol. 2006;1:38. doi: 10.1186/1746-1596-1-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guohua Y, Lingling K, Guimei Q. et al. Composite lymphoma in the anterior mediastinum: a case report and review of the literature. Diagn Pathol. 2011;6:60. doi: 10.1186/1746-1596-6-60. [DOI] [PMC free article] [PubMed] [Google Scholar]