Introduction
The interface between HIV and substance use is inextricably intertwined and is complicated by interactions with the criminal justice system (CJS).1,2 Approximately one in six of the estimated 1.1 million HIV-infected individuals in the United States passes through the CJS annually. Most pass through jails where there is routine health assessment.3 As such, jails represent an important opportunity not only to detect and treat HIV infection,4 but also to screen for substance use disorders (SUDs). Evidence-based treatments are now routinely available for the treatment of both conditions,2 yet the availability of treatment for SUDs within criminal justice settings remains limited and the lack of treatment results in significant morbidity and mortality and recidivism to CJS.5–9
The CJS bears a considerable burden of individuals with SUDs, with up to 65% of prison inmates meeting DSM-IV criteria for drug or alcohol abuse or dependence.10,11 Drug use profiles by people entering prison have not appreciably changed since 1997.11 SUDs have a profoundly negative impact on the health of people living with HIV/AIDS (PLWHA).2 Not only are drug users less likely to be prescribed antiretroviral therapy (ART), but also, when they are, they are more likely to do so with advanced HIV infection and achieve less favorable treatment outcomes compared to non-drug users.12,13
In community settings, HIV-infected persons who actively use drugs and are not receiving drug treatment have poor engagement in HIV care and adherence to ART,14 including released prisoners.7,15 Alcohol use disorders similarly are associated with poor HIV treatment outcomes16 especially for those within the CJS.17 Provision of evidence-based treatment for SUDs, however, markedly improves HIV treatment outcomes.18–20 Less than one-fifth of all PLWHA in the U.S. have achieved viral suppression, far lower than the estimated 60% needed to reduce the ~56,000 new HIV infections annually – a number that has not changed appreciably in the past 15 years.21 Understanding the types and severity of SUDs among PLWHA who enter jails provides insight into developing necessary strategies in order to better improve access to HIV care, prescription of ART and improve ART adherence, all of which are prerequisite to achieving viral suppression.
We therefore examined the correlates of three major components of the HIV treatment engagement cascade that are requisite for achieving HIV viral suppression in the largest sample of recruited HIV-infected jail detainees: 1) having a HIV care provider; 2) receiving ART; and 3) achieving high levels of ART adherence (≥95%) among those prescribed it in the 30 days prior to incarceration. Moreover, because SUDs are chronic and relapsing conditions that figure prominently into comorbidity among jail detainees, we sought to describe the types of drugs used and their severity in order to provide insight into post-release interventions necessary for this population.
Methods
Data for this cross-sectional study is from the baseline assessment of the EnhanceLink initiative that enrolled HIV-infected adults aged 18 or older from 10 diverse jail settings in the U.S.
Study Settings
The 10 study sites in 9 states (CT, GA, IL, MA, NY, OH, PA, RI, SC) and entry criteria for each site22 as well as the post-release substance abuse treatment outcomes23 have previously been described elsewhere. Subjects were enrolled if they were HIV-infected and provided written consent for study participation. Subjects in New York City (NYC) who received case management for a serious DSM-IV mental disorder were excluded and only women were recruited in Chicago. Out of total 1270, baseline assessments for the 1,166 (91.8%) subjects who knew their HIV diagnosis before incarceration were included in the analysis; 80 of the 1,270 total subjects who reported to be diagnosed with HIV during their index incarceration as well as 24 individuals with incomplete baseline data were excluded.
Dependent Variables
To assess the extent to which detainees engaged in HIV care and treatment, we defined three dependent variables as the primary outcomes of interest: 1) Having an HIV care provider in the 30 days prior to incarceration; 2) Being prescribed ART in the 7 days prior to the index incarceration; and 3) Being highly adherent (defined by self-report of having taken ≥ 95% of prescribed ART) for the subset who received ART in the 7 days prior to incarceration.
Independent Variables and Behavioral Model for Vulnerable Populations
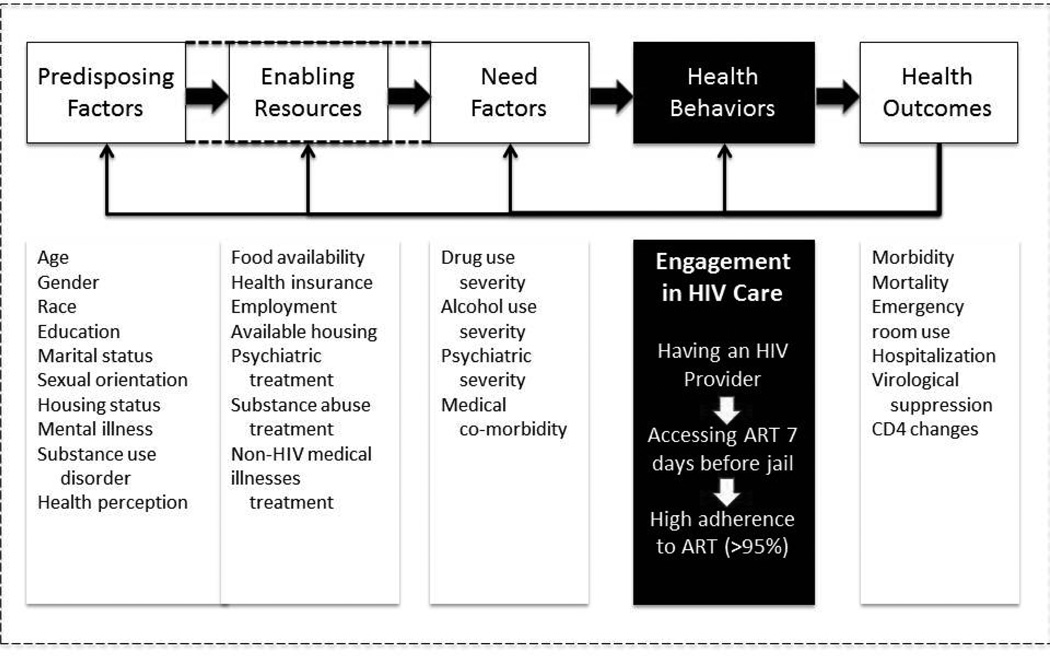
Independent variables were selected in accordance with the Behavioral Model for Vulnerable Populations. This model of health care utilization includes predisposing factors, enabling resources, and need factors as critical elements that influence health care utilization. In Figure 1, we adapt this model for this population as has been previously described for vulnerable populations24 and HIV-infected jail detainees.25
Figure 1.
Conceptual model of health behaviors among the HIV-infected persons during the pre-incarceration period – adapted from Chen N, et al. 2011 with permission.
According to the model, predisposing factors are the individuals’ intrinsic characteristics that impact health care utilization. Represented in our study, they include age, gender, race, education, relationship status, sexual orientation, perception of health status, and the presence of a number of psychiatric and substance use disorders. Individual’s perception of their health status was dichotomized (good, very good, and excellent versus fair or poor). Enabling resources are those factors available to the individual by their community to facilitate access and health care utilization. They include having self-reported health insurance; food insecurity, defined as not having anything to eat for two days or more in the past 30 days; and housing status with homelessness defined as self-identifying as homeless or having spent at least one night in public venues over the past month. Need factors assess the extent to which a person may need care and is often determined by the severity of the diseases, the individual’s perceptions of their health and their priorities and needs for receiving care. These often include extent to which a person has multiple medical comorbidities, severity of drug or alcohol use, and severity of their psychiatric illnesses.
Types of drug use in the 30 days pre-incarceration was ascertained using the Addiction Severity Index (ASI)26 that includes opioids (heroin, other opioids / analgesics / painkillers), cocaine, cannabis, and amphetamines. Polysubstance use was defined if subjects used two or more substances per day (including alcohol). Pre-incarceration drug treatment was also reported from the ASI. Severity of substance use was determined by ASI Composite Scores26 The ASI composite scores were reported two ways: 1) continuous variables, ranging from 0–1; and 2) dichotomized composite scores using pre-specified cut-offs. Cut offs of 0.12, 0.15, and 0.22 for drug, alcohol, and psychiatric composite scores have been shown to confer high levels of sensitivity and specificity at (85%, 86%), (86%, 80%), and (90%, 71%), respectively, for DSM-IV diagnoses.25,27
Statistical Analysis
All independent variables that assessed predisposing factors, enabling resources, and need factors as described by Behavioral Model for Vulnerable Populations were assessed and the association between recent drug use and the aforementioned variables were studied. For continuous variables, the difference between the means was tested using independent-sample t-test. For the categorical variables, the Pearson’s chi-square test was used. Significance level was defined at 0.05.
Also, we used regression models to examine the correlations between the three major outcomes and drug use. We fitted univariate and multivariate regression models with unadjusted and adjusted odds ratio as the measures of strength. Age, gender, race, and ASI composite scores for drug, alcohol, and psychiatric illnesses plus any variable significant at the p≤0.10 in the univariate assessment were then entered into the multivariate logistic regression models to study their association with the three dependent outcomes while controlling for potential confounders. The significance of the overall model was evaluated using the log likelihood ratio test as well as Hosmer & Lemeshow goodness-of-fit test. Individual coefficients in the model were tested using Wald statistic for statistical significance. Multi-collinearity was evaluated between the covariates in the model using tolerance and Variance Inflation Factor (VIF). None of the covariates showed significant multi-collinearity. All the analyses were performed with SPSS statistical software V.16 (SPSS Inc., Chicago IL).
Results
Demographic and drug use characteristics of the sample are presented in Table 1. The mean age of the subjects was 42.8 years, mostly male (72.3%), people of color (80.4%) and heterosexual (78%). Recent drug use over the 30-day pre-incarceration period was reported for cocaine (53%), alcohol (51%), cannabis (31.4%), and heroin (26.8%). Lifetime use of drug treatment was high with 70.6% of all the detainees reported having received any treatment, while 55.7% were treated by drug detoxification only. Of note, 19.6% who received drug or alcohol treatment in the past 30 days reported concomitant recent substance use.
Table 1.
Demographic characteristics, substance use pattern, substance use treatment history, and their associations with recent drug use - stratified based on any drug use in the 30 days pre-incarceration
| Total | Any Drug Use –30 days pre-incarceration** |
P-value | |||
|---|---|---|---|---|---|
| User N=841 |
Non-user N=322 |
||||
| Mean Age, years (S.D.) | 42.8 (8.8) | 42.4 (8.8) | 44.1 (8.7) | 0.004 | |
| Gender | Male | 842 (72.3%) | 585 (69.6%) | 256 (30.4%) | 0.008 |
| Female | 322 (27.7%) | 249 (77.3%) | 73 (22.7%) | ||
| Race/ethnicity | White | 159 (13.9%) | 118 (74.2%) | 41 (25.8%) | 0.779 |
| Hispanic | 292 (25.5%) | 213 (72.9%) | 79 (27.1%) | ||
| Black | 628 (54.9%) | 449 (71.6%) | 178 (28.4%) | ||
| Other | 65 (5.7%) | 43 (66.2%) | 22 (33.8%) | ||
| Education | < High school | 586 (50.6%) | 433 (74.0%) | 152 (26.0%) | 0.107 |
| ≥ High school diploma | 572 (49.4%) | 399 (69.8%) | 173 (30.2%) | ||
| Relationship Status | Married or in a relationship | 358 (30.7%) | 251 (70.3%) | 106 (29.7%) | 0.507 |
| Not in relationship | 807 (69.3%) | 582 (72.2%) | 224 (27.8%) | ||
| Sexual Orientation | Homo/bisexual | 255 (22.0%) | 183 (71.3%) | 72 (28.2%) | 0.944 |
| Heterosexual | 904 (78.0%) | 646 (71.5%) | 257 (28.5%) | ||
| Patient’s self-perception of his/her health status | Good | 634 (54.6%) | 439 (69.4%) | 194 (30.6%) | 0.056 |
| Poor | 528 (45.4%) | 393 (74.4%) | 135 (25.6%) | ||
| Health Insurance | Yes | 911 (78.7%) | 649 (71.3%) | 261 (28.7%) | 0.630 |
| No | 247 (21.3%) | 180 (72.9%) | 67 (27.1%) | ||
| Food Insecurity | Yes | 431 (37.2%) | 353 (81.9%) | 78 (18.1%) | <0.001 |
| No | 727 (62.8%) | 473 (65.2%) | 252 (34.8%) | ||
| Homelessness | Yes | 454 (39.2%) | 361 (79.5%) | 93 (20.5%) | <0.001 |
| No | 705 (60.8%) | 470 (66.9%) | 233 (33.1%) | ||
| Employment – Past 3 years | Employed | 246 (21.3%) | 165 (67.1%) | 81 (32.9%) | 0.058 |
| Unemployed | 911 (78.7%) | 666 (79.6%) | 244 (26.8%) | ||
| Paid Work –30 days pre-incarceration | Yes | 223 (19.6%) | 166 (74.4%) | 57 (25.6%) | 0.372 |
| No | 914 (80.4%) | 653 (71.4%) | 261 (28.6%) | ||
| Age at First Arrest | ≤13 yrs | 130 (11.6%) | 100 (76.9%) | 30 (23.1%) | 0.192 |
| >13 yrs | 988 (88.4%) | 706 (71.5%) | 282 (28.5%) | ||
| Mean age at first arrest, years (SD) | 19.8 (7.1) | 19.5 (6.8) | 20.6 (7.7) | 0.035 | |
| Medical Illnesses & Comorbidities | |||||
| Medical Comorbidities | Yes | 875 (75.6%) | 632 (72.2%) | 243 (27.8%) | 0.303 |
| No | 282 (24.4%) | 194 (69.0%) | 87 (31.0%) | ||
| Receiving treatment for a medical illness other than HIV | Yes | 834 (72.5%) | 593 (71.1%) | 241 (28.9%) | 0.321 |
| No | 317 (27.5%) | 243 (74.1%) | 82 (25.9%) | ||
| Mean number of times treated for Psychiatric illness (Inpatient) | 1.2 | 1.2 | 1.2 | 0.827 | |
| Mean number of times treated for Psychiatric illness (Outpatient) | 1.3 | 1.5 | 1.2 | 0.186 | |
| Substance Use Disorders – Last 30 days | |||||
| Alcohol | |||||
| Any Use | 51.0% | 59.5% | 29.0% | <0.001 | |
| To Intoxication | 27.8% | 33.7% | 12.7% | <0.001 | |
| Opioids | |||||
| Any Opioid | 31.8% | 44.1% | ---- | ---- | |
| Heroin | 26.8% | 37.1% | ---- | ---- | |
| Other | 9.2% | 12.7% | ---- | ---- | |
| Cocaine | 53.0% | 73.5% | ---- | ---- | |
| Cannabis | 31.4% | 43.7% | ---- | ---- | |
| Amphetamine | 1.7% | 2.4% | ---- | ---- | |
| Polysubstance Use* | 56.4% | 73.9% | ---- | ---- | |
| Drug Treatment | |||||
| Treated for “alcohol” or “drug” use –30 days pre-incarceration | 19.9% | 19.6% | 20.7% | 0.691 | |
| Treated for alcohol use -lifetime | 27.8% | 28.4% | 26.5% | 0.505 | |
| Treated for drug use - lifetime | 70.6% | 76.4 | 55.4% | <0.001 | |
| “Detox” only for alcohol -lifetime | 22.1% | 23.6% | 18.0% | 0.052 | |
| “Detox” only for drug -lifetime | 55.7% | 60% | 43.8% | <0.001 | |
| Addiction Severity Index (ASI)- Composite Scores – Continuous (Mean + SD) | |||||
| Drugs | 0.20 + 0.16 | 0.26 + 0.14 | 0.05 + 0.07 | <0.001 | |
| Alcohol | 0.18 + 0.25 | 0.22 + 0.27 | 0.10 + 0.19 | <0.001 | |
| Psychiatric | 0.28 + 0.26 | 0.29 + 0.26 | 0.25 + 0.25 | 0.021 | |
| Addiction Severity Index - Composite Scores – Dichotomous (using standard cut offs) | |||||
| Drugs (score ≥ 0.12) | 64.9% | 81.6% | 20.5% | <0.001 | |
| Alcohol (score ≥ 0.15) | 36.9% | 43.5% | 20.0% | <0.001 | |
| Psychiatric (score ≥ 0.22) | 52.3% | 54.2% | 47.5% | 0.042 | |
defined as using more than one type of drug in the same day during the 30-day period prior to index incarceration.
Numbers may not add up exactly to 100% due to missing data
Legend: ART: antiretroviral therapy; SD=standard deviation
Using documented ASI composite score cutoffs for high levels of severity, 64.9%, 36.9%, and 52.3% of subjects had ASI composite scores higher than the selected cut-offs for drug, alcohol, and psychiatric co-morbidity, respectively, indicating the group had the highest severity with underlying substance use and psychiatric illnesses.
The correlation between the alcohol and drug use was examined using the corresponding ASI composite scores. ASI drug and ASI alcohol composite scores were significantly correlated (p<0.001); however, the correlation was not strong (Pearson’s correlation coefficient r=0.22, and Spearman’s correlation coefficient r=0.17). Recent drug use was correlated with a number of demographic, social, and clinical factors. Independent correlates of recent drug use included being female (p=0.008), experiencing recent food insecurity (p<0.001), homelessness (p<0.001) and lower mean age at the time of first arrest compared to non-users (p=0.004).
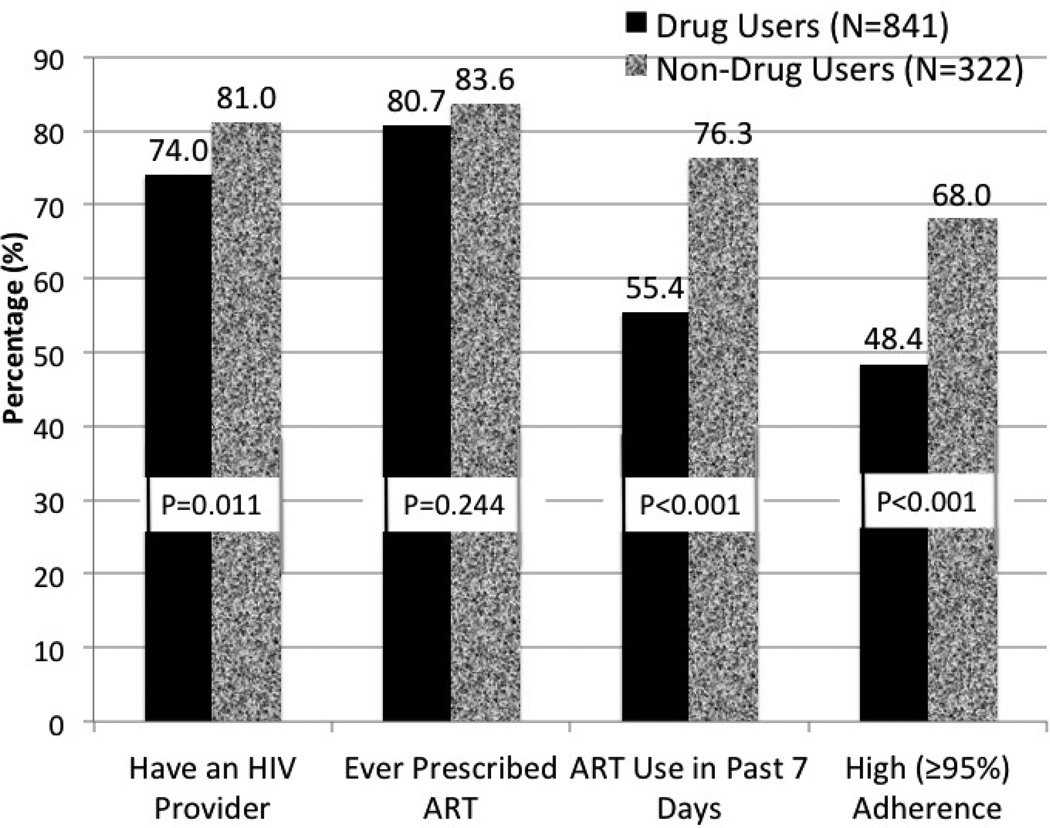
Figure 2 examines the recent engagement in HIV care among pre-incarceration drug users and non-users. Though over 80% of the sample had ever received ART, there was no significant difference between the two groups for this outcome. For the three primary outcomes of interest, pre-incarceration drug users were significantly less likely than non-users to have had a HIV doctor (74.0% versus 81.0%; p=0.011), received ART (55.4% versus 76.3%; p<0.001; N=950) or been adherent to it (48.4% versus 68.0%; p<0.001; N=581) in the time immediately preceding incarceration.
Figure 2.
Comparison of HIV Treatment Outcomes Among HIV-infected Drug Users Entering Jail (N=1166)
After controlling for potential covariates, lower drug use severity remained significant for all three primary outcomes. Table 2 presents the univariate and multivariate regression for correlates of having an HIV care provider in the last 30 days. Having health insurance, increased psychiatric severity and being seen by a physician for a non-HIV related condition were independently correlated with having a HIV provider, while increasing drug addiction severity, being female, black, homeless and having a self-perception of poor overall health status were associated with not having a HIV physician.
Table 2.
Significant correlates of having a HIV care provider within the 30-day period prior to incarceration
| Variable | Unadjusted OR [%95 CI] |
p-value | Adjusted OR [%95 CI] |
p-value | |
|---|---|---|---|---|---|
| Gender | Male | Referent | |||
| Female | 0.61 [0.46 – 0.81-] | 0.001 | 0.54 [0.38 –0.78] | 0.001 | |
| Age, years – continuous | 1.04 [1.03–1.06] | <0.001 | 1.02 [1.00–1.04] | 0.091 | |
| Race/ethnicity | White | Referent | |||
| Black | 0.58 [0.37–0.90] | 0.014 | 0.48 [0.27–0.86] | 0.013 | |
| Hispanic | 1.03 [0.63 – 1.71] | 0.898 | 0.65 [0.34 –1.24] | 0.190 | |
| Other | 0.58[0.29 –1.31] | 0.109 | 0.40 [0.17 – 0.94] | 0.035 | |
| Food Insecurity | No | Referent | |||
| Yes | 0.60 [0.46 – 0.79] | <0.001 | 0.80 [0.53–1.21] | 0.289 | |
| Homelessness | No | Referent | |||
| Yes | 0.35 [0.27 – 0.46] | <0.001 | 0.61 [0.41–0.92] | 0.017 | |
| Paid work in 30 days pre-incarceration | No | Referent | |||
| Yes | 0.71 [0.51 – 0.99] | 0.043 | 0.92 [0.60–1.40] | 0.688 | |
| Health Insurance | No | Referent | |||
| Yes | 7.49 [5.48 – 10.23] | <0.001 | 5.26 [3.58– 7.71] | <0.001 | |
| Medical Comorbidities | No | Referent | |||
| Yes | 1.96 [1.45 – 2.63] | <0.001 | 1.02 [0.66–1.52] | 0.955 | |
| Receiving treatment for medical illnesses other than HIV | No | Referent | |||
| Yes | 2.59 [1.94 – 3.45] | <0.001 | 2.28 [1.57–3.32] | <0.001 | |
| Patient’s self-perception of his/her health | Good | Referent | |||
| Poor | 0.73 [0.56–0.96] | 0.022 | 0.67 [0.47–0.95] | 0.024 | |
| Addiction Severity - Drug Composite Score (continuous) | 0.34 [0.14 – 0.82] | 0.017 | 0.28 [0.09–0.89] | 0.031 | |
| Addiction Severity - Alcohol Composite Score (continuous) | 0.51 [0.31–0.86] | 0.011 | 0.67 [0.34–1.31] | 0.238 | |
| Addiction Severity - Psychiatric Composite Score (continuous) | 1.27 [0.75 – 2.15] | 0.381 | 2.89 [1.36– 6.13] | 0.006 |
Legend: OR=Odds Ratio; CI=confidence interval
The following were not found to be significant correlates at p<0.10 on bivariate analysis and not included in the final model: education, relationship status, sexual orientation, employment (last 3 years), age at first arrest.
With regard to the second outcome, receipt of ART just before incarceration (Table 3), having health insurance, receiving treatment for a condition not related to HIV and increasing psychiatric severity portended a 3.67-, 2.98- and 2.65-fold increased likelihood of receiving ART, respectively, while being Black, female, having younger age, experiencing food insecurity, having self-perception of poor health status and having increasing levels of drug addiction severity was negatively associated with this outcome.
Table 3.
Significant correlates of receiving antiretroviral therapy (ART) in 7 days prior to incarceration
| Variable | Unadjusted OR [%95 CI] |
p-value | Adjusted OR [%95 CI] |
p-value | |
|---|---|---|---|---|---|
| Gender | Male | Referent | |||
| Female | 0.44 [0.33–0.59] | <0.001 | 0.46 [0.32– 0.67] | <0.001 | |
| Age – continuous | 1.04 [1.02–1.06] | <0.001 | 1.03 [1.01–1.05] | 0.003 | |
| Education | Less than High School Diploma | Referent | |||
| High School diploma or higher | 1.32 [1.02–1.72] | 0.038 | 1.19[0.86–1.65] | 0.304 | |
| Race/ethnicity | White | Referent | |||
| Black | 0.74 [0.50–1.11] | 0.148 | 0.54 [0.32–0.91] | 0.021 | |
| Hispanic | 1.15 [0.74–1.80] | 0.541 | 0.82 [0.46–1.46] | 0.494 | |
| Other | 0.78 [0.40– 1.52] | 0.468 | 0.49 [0.21– 1.14] | 0.097 | |
| Food Insecurity | No | Referent | |||
| Yes | 0.44 [0.34–0.58] | <0.001 | 0.58 [0.40–0.84] | 0.004 | |
| Homelessness | No | Referent | |||
| Yes | 0.43 [0.33–0.57] | <0.001 | 0.79[0.55–1.13] | 0.187 | |
| Health Insurance | No | Referent | |||
| Yes | 3.66 [2.57–5.19] | <0.001 | 2.58 [1.68– 3.94] | <0.001 | |
| Medical Comorbidities | No | Referent | |||
| Yes | 1.40 [1.03–1.91] | 0.033 | 1.03 [0.68–1.56] | 0.902 | |
| Receiving treatment for medical illnesses other than HIV | No | Referent | |||
| Yes | 2.69 [1.94–3.73] | <0.001 | 2.98 [2.00–4.44] | <0.001 | |
| Patient’s self-perception of his/her health | Good | Referent | |||
| Poor | 0.59 [0.45–0.77] | <0.001 | 0.55[0.40–0.76] | <0.001 | |
| Addiction Severity - Drug Composite Score (continuous) | 0.13 [0.05–0.31] | <0.001 | 0.12[0.04–0.35] | <0.001 | |
| Addiction Severity - Alcohol Composite Score (continuous) | 0.44 [0.26–0.75] | 0.003 | 0.63[0.33–1.22] | 0.170 | |
| Psychiatric Composite Score (continuous) | 0.73 [0.43–1.21] | 0.218 | 2.65 [1.33–5.28] | 0.006 |
Legend: OR=odds ratio; CI=confidence intervals
The following were not found to be significant correlates at p<0.10 on bivariate analysis and not included in the final model: relationship status, sexual orientation, employment (last 3 years), paid work (30 days pre-incarceration), age at first arrest.
Independent correlates for achieving optimal levels of ART adherence, however, yielded different results aside from increasing drug addiction severity being associated with an 82% reduced likelihood of achieving optimal adherence. For this outcome, none of the demographic, social or health utilization factors for other conditions were significant. Being employed and paid for work was associated with a two-fold increased likelihood of optimal adherence.
Discussion
Our findings illustrate that the prevalence of SUDs in the population of HIV-infected jail detainees is extremely high. Among all subjects, 72% had used drugs in the 30 days before incarceration and is similar to findings from Arrestee Drug Abuse Monitoring (ADAM II) project, where 66% reported any recent drug use, with the most commonly used substances being marijuana (35–58%), cocaine (12–33%), and heroin (3–22%).28,29 While most national surveys only measure recent use, our study extends this approach by also measuring addiction severity, which was particularly high within our sample with nearly two thirds of subjects having scores exceeding the threshold for having DSM-IV criteria for SUDs. Moreover, 37% and 52% of inmates had composite scores above the cut-offs for alcohol dependence, and psychiatric illnesses, respectively. These figures document the syndemic nature of HIV, substance abuse, mental illness and its intersection with the criminal justice system.
Unlike the findings among arrestees from ADAM-II, HIV-infected jail detainees were more likely to use cocaine, heroin and alcohol, rather than marijuana. At least for those with opioid dependence and alcohol use disorders, there are a number of evidence-based treatments, primarily medication-assisted therapies, that would greatly benefit these individuals.2 Specifically for opioid dependence, evidence-based treatments include methadone, buprenorphine and extended-release naltrexone (XR-NTX). In the case of alcohol dependence, naltrexone in either is oral or XR-NTX formulation is the preferred medication-assisted therapy, but acamprosate and disulfuram are also approved treatments.2 In the case of cocaine abuse, some behavioral interventions, specifically cognitive behavioral therapy, have been shown to be effective, but there is no FDA-approved effective medical therapy for cocaine use.2,17,30
Central to this study is the negative contribution of active drug use and the level of severity on each of the three designated HIV treatment outcomes. To our knowledge, this is the first time that drug use severity has been associated with all three negative health consequences along the HIV continuum of care cascade. It would be reasonable to extrapolate that the significantly lower rates of treatment engagement, and specifically suboptimal adherence, would result in lower levels of viral suppression as well. In the U.S., as few as 19% of all PLWHA are currently virally suppressed.21 With one sixth of all PLWHA transitioning through the CJS annually, it stands to reason that this population needs significantly better interventions to keep them fully engaged in care. Moreover, PLWHA who transition through the CJS have been documented to have high rates of HIV risk behaviors upon release31 and in the absence of effective HIV risk reduction strategies such as consistent evidence-based drug treatment, condom use or syringe exchange programs, interventions that target viral suppression would greatly contribute to HIV transmission and ultimately lower the ~56,000 new infections that have remained unchanged for the past decade.
The findings show that every 0.1 incremental increase in level of addiction severity translates into a 12% reduction in likelihood of having a HIV provider, a 19% reduction in likelihood of receiving ART, and a 16% reduction in achieving optimal ART adherence. Alcohol use severity, on the other hand, did not correlate with these outcomes aside from trending towards significance for ART adherence, but alcohol use disorders (AUD), per se, have been associated with a number of poor HIV treatment outcomes,16 especially with CJS populations.17 Unfortunately, only alcohol use severity and not the presence of an AUD was assessed in this study, but future jail-release programs should systematically assess them among PLWHA and link them with evidence-based alcohol relapse prevention treatments in order to improve retention in care and adherence with ART.32
Having health insurance was the strongest factor correlated with being engaged in HIV care and being prescribed ART. Similar findings have been found among the homeless.25,25 Similarly, being female and black were independently and negatively associated with these two outcomes. Therefore interventions that focus on PLWHA transitioning from jail should be culturally and gender appropriate in order to reap the greatest benefits. Two co-morbidities, individuals with high psychiatric severity and having been seen for a condition unrelated to HIV, were independently associated with having a HIV care provider and receiving ART. According to the Behavioral Model, these two factors would be consistent with need factors – having other conditions that require them to be engaged in care. Moreover, those with the highest psychiatric severity would also gain access to health insurance due to it being a disability and perhaps serve as a conduit to simultaneous HIV treatment.
Although this is the largest study of its size, a few limitations exist. First, the study is cross-sectional and only associations rather than causality can be inferred. Second, most data are self-reported and may introduce information biases, including reporting and recall bias. Third, using the 30-day pre-incarceration period may introduce bias in two directions. Those whose lives have become more chaotic and result in incarceration may over-represent the drug use information, while those who are on remanded while on probation or awaiting trial may reduce their drug use behaviors while trying avoiding jail. Moreover, though we used a number of psychometrically validated measures to assess the likelihood of being dependent on drugs or alcohol, we did not use standardized clinical screening measurements that would provide increased accuracy. Instead, we often relied on measures of drug and alcohol use severity. Notwithstanding these limitations, this is the largest sample of PLWHA who interface with jails and provide valuable insight into the healthcare disparities facing this vulnerable population during the period just prior to incarceration and give some insight into post-release needs.
Conclusions
Recent active drug use and addiction severity is extremely high among PLWHA as they enter jail, and is associated with a number of demographic and social instability characteristics, suggesting the need for multidisciplinary and gender-specific interventions for PLWHA. Although HIV-infected jail detainees had a number of community-based interactions with drug treatment services, most of them had been “detox” and may not have included many evidence-based treatments. The findings of increased drug use severity markedly reducing the engagement of PLWHA in the HIV treatment continuum of care suggests that evidence-based drug treatment interventions are urgently needed for this vulnerable and “challenging” population.
Table 4.
Significant correlates of high levels of adherence to antiretroviral therapy (≥ 95%) among subjects who received antiretroviral therapy in the 7 days prior to incarceration
| Variable | Unadjusted OR [%95 CI] |
p-value | Adjusted OR [%95 CI] |
p-value | |
|---|---|---|---|---|---|
| Gender | Male | Referent | |||
| Female | 1.04 [0.69–1.58] | 0.847 | 0.96[0.60–1.54] | 0.861 | |
| Age – continous | 1.00 [0.98–1.02] | 0.814 | 1.00 [0.98–1.02] | 0.969 | |
| Race/ethnicity | White | Referent | |||
| Black | 1.08 [0.66–1.76] | 0.771 | 1.02 [0.59–1.76] | 0.955 | |
| Hispanic | 1.06 [0.62–1.80] | 0.831 | 1.24 [0.68–2.26] | 0.485 | |
| Other | 0.86 [0.37–1.99] | 0.731 | 0.83 [0.34–2.05] | 0.686 | |
| Food Insecurity | No | Referent | |||
| Yes | 0.68 [0.47–0.98] | 0.039 | 0.97[0.62–1.54] | 0.908 | |
| Homelessness | No | Referent | |||
| Yes | 0.61 [0.42–0.87] | 0.007 | 0.72 [0.47–1.10] | 0.129 | |
| Paid work-30 days pre-incarceration | No | Referent | |||
| Yes | 2.03 [1.27–3.24] | 0.003 | 2.02 [1.21–3.36] | 0.007 | |
| Patient’s self-perception of his/her health | Good | Referent | |||
| Poor | 0.68 [0.49–0.96] | 0.026 | 0.70 [0.48–1.02] | 0.062 | |
| Addiction Severity - Drug Composite Score (continuous) | 0.14 [0.05–0.45] | 0.001 | 0.18 [0.05–0.62] | 0.007 | |
| Addiction Severity - Alcohol Composite Score (continuous) | 0.41 [0.20–0.85] | 0.017 | 0.49 [0.22–1.13] | 0.094 | |
| Psychiatric Composite Score (continuous) | 0.91 [0.47–1.76] | 0.784 | 1.45 [0.64–3.29] | 0.371 |
Legend: OR=odds ratio; CI=confidence interval
The following were not found to be significant correlates at p<0.10 on bivariate analysis and not included in the final model: education, relationship status, sexual orientation, health insurance, age at first arrest, medical comorbidities, receiving treatment for medical illnesses other than HIV.
Acknowledgments
Funding: Funding from this grant was provided by the Health Resources and Services Agency for the 10-site demonstration and by the National Institutes on Drug Abuse for career development (K24 DA017072) for Frederick L. Altice.
References
- 1.Springer SA, Altice FL. In: Improving the Care for HIV-Infected Prisoners: An Integrated Prison-Release Health Model Public Health Behind Bars. Greifinger RB, editor. New York: Springer; 2007. pp. 535–555. [Google Scholar]
- 2.Altice FL, Kamarulzaman A, Soriano VV, Schechter M, Friedland GH. Treatment of medical, psychiatric, and substance-use comorbidities in people infected with HIV who use drugs. Lancet. 2010 Jul 31;376(9738):367–387. doi: 10.1016/S0140-6736(10)60829-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Spaulding AC, Seals RM, Page MJ, Brzozowski AK, Rhodes W, Hammett TM. HIV/AIDS among inmates of and releasees from US correctional facilities2006: declining share of epidemic but persistent public health opportunity. PLoS One. 2009;4(11):e7558. doi: 10.1371/journal.pone.0007558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Flanigan TP, Zaller N, Beckwith CG, et al. Testing for HIV, sexually transmitted infections, and viral hepatitis in jails: still a missed opportunity for public health and HIV prevention. J Acquir Immune Defic Syndr. 2010 Dec;55(Suppl 2):S78–S83. doi: 10.1097/QAI.0b013e3181fbc94f. [DOI] [PubMed] [Google Scholar]
- 5.Bruce RD, Smith-Rohrberg D, Altice FL. In: Pharmacological Treatment of Substance Abuse in Correctional Facilities: Prospects and Barriers to Expanding Access to Evidence-Based Therapy Public Health Behind Bars. Greifinger RB, editor. New York: Springer; 2007. pp. 385–411. [Google Scholar]
- 6.Nunn A, Zaller N, Dickman S, Trimbur C, Nijhawan A, Rich JD. Methadone and buprenorphine prescribing and referral practices in US prison systems: results from a nationwide survey. Drug Alcohol Depend. 2009 Nov 1;105(1–2):83–88. doi: 10.1016/j.drugalcdep.2009.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Springer SA, Chen S, Altice FL. Improved HIV and substance abuse treatment outcomes for released HIV-infected prisoners: the impact of buprenorphine treatment. J Urban Health. 2010 Jul;87(4):592–602. doi: 10.1007/s11524-010-9438-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Oser CB, Knudsen HK, Staton-Tindall M, Taxman F, Leukefeld C. Organizational-level correlates of the provision of detoxification services and medication-based treatments for substance abuse in correctional institutions. Drug Alcohol Depend. 2009 Aug 1;103(Suppl 1):S73–S81. doi: 10.1016/j.drugalcdep.2008.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chandler RK, Fletcher BW, Volkow ND. Treating drug abuse and addiction in the criminal justice system: improving public health and safety. JAMA. 2009 Jan 14;301(2):183–190. doi: 10.1001/jama.2008.976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Abuse CoAaS. Behind Bars II: Substance Abuse and America’s Prison Population. New York: Columbia University; 2010. [Google Scholar]
- 11.Karberg JCMC. Drug use and dependence, state and federal prisoners. Bureau of Justice Statistics. 2006 http://bjs.ojp.usdoj.gov/content/pub/pdf/dudsfp04.pdf.
- 12.Wood E, Hogg RS, Harrigan PR, Montaner JS. When to initiate antiretroviral therapy in HIV-1-infected adults: a review for clinicians and patients. Lancet Infect Dis. 2005 Jul;5(7):407–414. doi: 10.1016/S1473-3099(05)70162-6. [DOI] [PubMed] [Google Scholar]
- 13.Porter K, Babiker A, Bhaskaran K, Darbyshire J, Pezzotti P, Walker AS. Determinants of survival following HIV-1 seroconversion after the introduction of HAART. Lancet. 2003 Oct 18;362(9392):1267–1274. doi: 10.1016/s0140-6736(03)14570-9. [DOI] [PubMed] [Google Scholar]
- 14.Lucas GM. Substance abuse, adherence with antiretroviral therapy, and clinical outcomes among HIV-infected individuals. Life Sci. 2011 May 23;88(21–22):948–952. doi: 10.1016/j.lfs.2010.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Springer SA, Pesanti E, Hodges J, Macura T, Doros G, Altice FL. Effectiveness of antiretroviral therapy among HIV-infected prisoners: Reincarceration and the lack of sustained benefit after release to the community. Clinical Infectious Diseases. 2004 Jun 15;38(12):1754–1760. doi: 10.1086/421392. 2004. [DOI] [PubMed] [Google Scholar]
- 16.Azar MM, Springer SA, Meyer JP, Altice FL. A systematic review of the impact of alcohol use disorders on HIV treatment outcomes, adherence to antiretroviral therapy and health care utilization. Drug Alcohol Depend. 2010 Dec 1;112(3):178–193. doi: 10.1016/j.drugalcdep.2010.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Springer SA, Azar MM, Altice FL. HIV, alcohol dependence, and the criminal justice system: a review and call for evidence-based treatment for released prisoners. Am J Drug Alcohol Abuse. 2011 Jan;37(1):12–21. doi: 10.3109/00952990.2010.540280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Altice FL, Bruce RD, Lucas GM, et al. HIV treatment outcomes among HIV-infected, opioid-dependent patients receiving buprenorphine/naloxone treatment within HIV clinical care settings: results from a multisite study. J Acquir Immune Defic Syndr. 2011;56(Suppl 1):S22–S32. doi: 10.1097/QAI.0b013e318209751e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lucas GM, Chaudhry A, Hsu J, et al. Clinic-based treatment of opioid-dependent HIV-infected patients versus referral to an opioid treatment program: A randomized trial. Ann Intern Med. 2010 Jun 1;152(11):704–711. doi: 10.1059/0003-4819-152-11-201006010-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Springer SA, Qiu J, Saber-Tehrani AS, Altice FL. Retention on buprenorphine is associated with high levels of maximal viral suppression among HIV-infected opioid dependent released prisoners. PLoS One. 2012;7(5):e38335. doi: 10.1371/journal.pone.0038335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gardner EM, McLees MP, Steiner JF, Del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011 Mar 15;52(6):793–800. doi: 10.1093/cid/ciq243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Draine J, Ahuja D, Altice FL, et al. Strategies to enhance linkages between care for HIV/AIDS in jail and community settings. AIDS Care. 2011 Mar;23(3):366–377. doi: 10.1080/09540121.2010.507738. [DOI] [PubMed] [Google Scholar]
- 23.Krishnan A, Wickersham J, Chitsaz E, et al. Post-release substance abuse outcomes among HIV-infected jail detainees: Results from a multisite study. AIDS and Behavior. 2012 Nov 01;2012:1–10. doi: 10.1007/s10461-012-0362-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gelberg L, Andersen RM, Leake BD. The Behavioral Model for Vulnerable Populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000 Feb;34(6):1273–1302. [PMC free article] [PubMed] [Google Scholar]
- 25.Chen NE, Meyer JP, Avery AK, et al. Adherence to HIV Treatment and Care Among Previously Homeless Jail Detainees. AIDS Behav. 2011 Nov 8; doi: 10.1007/s10461-011-0080-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McLellan AT, Kushner H, Metzger D, et al. The Fifth Edition of the Addiction Severity Index. J Subst Abuse Treat. 1992;9(3):199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- 27.Rikoon SH, Cacciola JS, Carise D, Alterman AI, McLellan AT. Predicting DSM-IV dependence diagnoses from Addiction Severity Index composite scores. J Subst Abuse Treat. 2006 Jul;31(1):17–24. doi: 10.1016/j.jsat.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 28.Office of National Drug Control Policy EOoTP. Arrestee Drug Abuse Monitoring Program. 2010 [Google Scholar]
- 29.Karberg JCJD. US Department of Justice, Bureau of Justice Statistics. Substance Dependence, Abuse, and Treatment of Jail Inmates 2002. 2005 http://bjs.ojp.usdoj.gov/content/pub/pdf/sdatji02.pdf.
- 30.National Institute on Drug Abuse (NIDA) Cocaine: Abuse and Addiction. 2010 https://www.drugabuse.gov/sites/default/files/rrcocaine.pdf.
- 31.Stephenson BL, Wohl DA, McKaig R, et al. Sexual behaviours of HIV-seropositive men and women following release from prison. Int J STD AIDS. 2006 Feb;17(2):103–108. doi: 10.1258/095646206775455775. [DOI] [PubMed] [Google Scholar]
- 32.Springer SA, Spaulding AC, Meyer JP, Altice FL. Public health implications for adequate transitional care for HIV-infected prisoners: five essential components. Clin Infect Dis. 2011 Sep;53(5):469–479. doi: 10.1093/cid/cir446. [DOI] [PMC free article] [PubMed] [Google Scholar]