Abstract
Background
Despite growing concerns about non-medical prescription drug use and prescription drug use disorders, whether vulnerability for these conditions is drug-specific or occurs through a shared liability and common risk factors is unknown.
Methods
Exploratory and confirmatory factor analysis of Wave 1 of the National Epidemiologic Survey on Alcohol and Related Conditions were used to examine the latent structure of non-medical prescription drug use and prescription drug use disorders. Multiple indicators multiple causes (MIMIC) analysis was used to examine whether the effect of sociodemographic and psychiatric covariates occurred through the latent factor, directly on each drug class or both.
Results
A one-factor model described well the structure of both non-medical prescription drug use and prescription drug use disorders. Younger age, being White, having more intense pain or one of several psychiatric disorders increased the risk of non-medical prescription drug use through the latent factor. The same covariates, except for anxiety disorders also significantly increased the risk of prescription drug use disorders through the latent factor. Older age directly increased the risk of non-medical use of sedatives, and alcohol use disorders decreased the risk of non-medical tranquilizer use. No covariates had direct effects on the risk of any prescription drug use disorders beyond their effect through the latent factor.
Conclusion
The risk for non-medical prescription drug use and prescription drug use disorders occurs through a shared liability. Treatment, prevention and policy approaches directed at these drugs as a group maybe more effective than those focused on individual classes of drugs.
Keywords: Non-medical prescription drug use, Prescription Drug Use Disorders, Latent Structure, NESARC
1. INTRODUCTION
Prescription drugs such as opioid analgesics, sedatives, tranquilizers and stimulants are essential medications for the treatment of pain, insomnia, anxiety, attention-deficit hyperactivity disorder (ADHD), and other psychiatric disorders (Olfson et al., 2013, in Press; Resnik and Rehm, 2001). However, management of these medications is complicated by their liability to lead to abuse or dependence (Blanco et al., 2007; Compton and Volkow, 2006; Martins et al., 2012). Prescription drugs can also increase the risk of psychiatric and other medical disorders (Compton and Volkow, 2006; McCabe et al., 2005; Simoni-Wastila and Strickler, 2004; Swanson and Volkow, 2008), particularly when not used as directed by a physician. Between 1991-1992 and 2001-2002 the prevalence of non-medical use of prescription drugs increased by 53%, and the prevalence of prescription drug use disorder increased 67%, calling attention to the need to balance access for appropriate use of those medications with the need to curtail their non-medical use (Blanco et al., 2007).
Non-medical use of prescription drugs is often defined as using a psychotropic medication without a prescription, in greater amounts, more often, or longer than prescribed, or for a reason other than a doctor said you should use them (Blanco et al., 2013a; Martins et al., 2012). In the US, approximately 2.7% of the population (7 million persons) aged 12 years or older report non-medical prescription drug use at some point in their lives (SAMHSA, 2011), making it the second most used group of drugs, only after cannabis (Grant et al., 2004a). The number of individuals with past-year prescription drug use disorders is also considerable, ranging in 2009 from 160,000 individuals with sedative use disorder to close to two million people with prescription opioid use disorders (SAMHSA, 2011).
Non-medical use of prescription drugs has been associated with adverse health effects (Simoni-Wastila and Strickler, 2004), including respiratory depression, gastrointestinal dysmotility, central nervous system depression, cardiac dysrhythmia, hypertension, tachycardia, seizures, incoordination (Hernandez and Nelson, 2010), overdose (Bohnert et al., 2010, 2011) and premature mortality (Hall et al., 2008; Paulozzi et al., 2006). Non-medical prescription use and prescription drug use disorders are also associated with increased prevalence of substance use, mood and anxiety disorders (Kaloyanides et al., 2007; McCabe et al., 2006; Schepis and Hakes, 2011). Hence, their study has important implications for developing effective prevention and intervention strategies (McCabe et al., 2008) that may improve the population’s health. Despite growing concern about these issues, to date, no study has examined whether the association of non-medical prescription use and prescription drug use disorders with their correlates occurs independently for each individual drug or through a common liability that underlying vulnerability to all drugs. This information is important because disorder-specific influences may require disorder-specific interventions, whereas influences at the latent variable level may be more amenable to interventions with broader impact.
In order to address those gaps in knowledge, the present study builds on prior knowledge to examine in a national representative sample of the U.S. general population: 1) the latent structure of non-medical prescription use of stimulants, tranquilizers, opioids and sedatives; 2) the latent structure of prescription drug use disorders due to those medications; and, 3) sociodemographic and psychiatric characteristics that may be related to each of the subtypes of drugs and of the group as a whole. Prior to our analysis, we hypothesized based on the published literature indicating high rates of comorbidity between substance use disorders and other psychiatric disorders (Agrawal et al., 2006; Fenton et al., 2010; Fischer et al., 2012; Poulin, 2007) that: 1) all psychiatric disorders and level of pain would be associated with increased prevalence of all past-year prescription drug use disorders; and 2) level of pain and some psychiatric disorders would differentially be associated with certain prescription drugs. Specifically, level of pain would be associated with increased prevalence of prescription opioid use disorder due to their analgesic properties, anxiety and alcohol use disorders would be associated with increased prevalence of sedative and tranquilizer use disorders due to their action on benzodiazepine receptors, and mood disorders would be associated with stimulant use disorders due to their mood elevating properties.
2. METHOD
2.1 Sample and procedures
The National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) (Grant et al., 2009, 2004b) was the source of data. The NESARC target population at Wave 1, collected in 2001-2002, was the civilian non-institutionalized population 18 years and older residing in households and group quarters. The overall survey response rate was 81%. Blacks, Hispanics, and young adults (aged 18-24 years) were oversampled, with data adjusted for over-sampling, household- and person-level non-response. The weighted data were then adjusted to represent the U.S. civilian population based on the 2000 Census. Interviews were conducted with 43,093 participants by experienced lay interviewers (Grant et al., 2009, 2004b). All procedures, including informed consent, received full human subjects review and approval from the US Census Bureau and the US Office of Management and Budget.
2.2 Assessment
The Alcohol Use Disorder and Associated Disabilities Interview Schedule-DSM-IV Version (AUDADIS-IV; Grant et al., 2003, 1995; Ruan et al., 2008), a fully structured diagnostic interview, includes computer algorithms and was used to generate 12-month DSM-IV diagnoses. The group of prescription drugs is comprised by sedatives (e.g., barbiturates), tranquilizers (e.g., benzodiazepines), opioids, and stimulants (e.g., amphetamines). Consistent with prior reports (Blanco et al., 2007, 2013c; Martins et al., 2012) non-medical use of a prescription drug was defined to respondents as using in the 12-months preceding the interview a prescription drug “without a prescription, in greater amounts, more often, or longer than prescribed, or for a reason other than a doctor said you should use them.”
To maximize statistical power and increase the stability of the estimates, we collapsed psychiatric disorders into broad groups. Axis I disorders included in the analyses were alcohol and drug use disorders (abuse and or dependence, excluding prescription drug use disorders), mood disorders (major depressive disorder, dysthymia, bipolar I and bipolar II disorders) and anxiety disorders (panic disorder, social anxiety disorder, specific phobia and generalized anxiety disorder disorders). Axis II disorders examined included cluster A (paranoid and schizoid), B (antisocial and histrionic) and C personality disorders (avoidant, dependent, and obsessive-compulsive). The test-retest reliabilities for AUDADIS-IV diagnoses are fair to good for mood, anxiety, and personality disorders (κ= 0.40-0.62) and excellent for substance use disorders (κ= 0.70-0.91; Grant et al., 2009; Hasin et al., 2007). Pain in the four weeks prior to the interview was assessed with an item from the Short Form 12, version 2 (SF-12; Ware et al., 2002) ranging from 1 (“not at all”) to 5 (“extreme”). We also included sex, age, race/ethnicity as covariates in our analyses because they have been shown in previous analyses to influence the risk for substance use disorders (Hernandez and Nelson, 2010; Martins et al., 2009).
2.3 Statistical analyses
Weighted percentages and corresponding standard errors were calculated to provide descriptive information about the relationship between sociodemographic and psychopathological correlates of non-medical use of prescription drugs and prescription drug use disorder. Because individuals often engage in non-medical use of more than one drug, the groups presented in the results overlap and those cannot be directly compared using standard bivariate tests such as chi-squares or odds ratios (the same is true in the case of prescription drug use disorders). However, their degree of association can be examined by looking at their tetrachoric correlations. Furthermore, the differential association between each predictor and non-medical use of each drug (and each prescription drug use disorder) can be examined using a Multiple Indicator Multiple Causes (MIMIC) approach, as explained below.
To examine the latent structure of non-medical use of prescription drugs and prescription drug use disorders, two separate exploratory factor analyses (EFA) using geomin oblique rotation were fit in the full sample, one using the four types of the past-year nonmedical prescription drugs use as the indicators, and the other one using as indicators the four types of the past-year prescription drug use disorder. We decided to use factor analysis rather than other latent variable techniques such as latent class analysis based on current conceptualizations of psychiatric disorders as continuous rather than discrete entities (Blanco et al., 2013b; Krueger, 1999), as well as empirical results indicating that externalizing disorders, including substance use disorders, are best described by models that assume continuous underlying latent variable (Markon and Krueger, 2005). The number of underlying factors in each analysis was determined based on the eigenvalues of the tetrachoric correlation matrices, and the goodness of fit measures, including by the likelihood chi-square test, comparative fit index (CFI), Tucker-Lewis index (TLI), root mean squared error of approximation (RMSEA) and standardized root mean square residual (SRMR). Hu and Bentler recommended CFI and TLI values above 0.95, and RMSEA values below 0.06, as representing good model fit (Hu et al., 1992). Factor analysis with dichotomous outcomes is a well-developed technique (Joreskog and Moustaki, 2001; Wirth and Edwards, 2007) utilizing probit regression of outcomes on the latent factor estimated with weighted least squares such that standardized factor loadings represent increases on the probit scale of each outcome associated with one standard deviation increases in the continuous latent factor. After the number of factors were determined for non-medical prescription drug use and prescription drug use disorder, a Multiple Indicators Multiple Causes (MIMIC) approach (Kim et al., 2011) was used to assess effects of covariates on the latent factors. Age, sex, race, level of pain, anxiety disorders, mood disorders, AUD, DUD, and clusters A, B and C personality disorders were used as covariates. The MIMIC approach allows simultaneous examination of several covariates. It provides an alternative to multiple group testing, which requires the creation of mutually exclusive groups (e.g., males versus females) and can be cumbersome when multiple covariates are examined. Standardized estimates of the direct relationship between covariates and the latent factors indicate how many standard deviations higher (or lower) the mean of the latent factor is expected to be for each level of the categorical covariates or for a one standard deviation increase in the continuous covariate (age) while holding all other covariates constant. A critical value of 0.05 was used to determine statistical significance of these covariate effects on factors.
The MIMIC model was further used to identify whether there was any additional association between covariates and specific prescription drugs (or disorders) that were not captured by the latent factor (Muthen and Muthen, 2006). Following conventions for testing these additional direct paths leading from the covariate to the specific drugs (Kim et al., 2011; Stark et al., 2006), we used a conventional modification index cutoff of 10 corresponding to a chi-square difference test with 1 degree of freedom and a p-value of <0.01 for a large sample size.
All analyses where conducted in Mplus Version 7.1 (Muthen and Muthen, 2006), which takes into account the NESARC sampling weights and design effects in all analyses. The default estimator for the analysis was weighted least squares using a diagonal weight matrix (WLSMV) accompanied by standard errors and mean- and variance-adjusted chi-square test statistic that use a full weight matrix. The WLSMV is a robust estimator which does not assume normally distributed variables and provides the best option for modeling categorical or ordered data. The full Wave 1 sample was used to fit all the models in the study.
3. RESULTS
The 12-month prevalence of non-medical use ranged from 0.49% for stimulants to 1.81% for prescription opioids. Individuals with non-medical use of prescription drugs were on average in their third or fourth decade of life, with the majority male and White. For all groups, the common co-occurring disorders were alcohol use disorders. The average level of pain ranged from 1.90 (stimulants) to 2.01 (opiates). Among personality disorders, Cluster B was the most common across all drug groups (Table 1).
Table 1.
Past-year nonmedical prescription drug use and prescription use disorders in the NESARC Wave 1 (n= 43,093).
| Nonmedical prescription drug use (n= 1218) % or mean (S.E.) |
Nonmedical prescription drug use disorders (n= 235) % or mean (S.E.) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Sedatives (n=490, 1.24%) |
Opioids (n=686, 1.81%) |
Tranquilizers (n=345, 0.93%) |
Stimulants (n=186, 0.49%) |
Sedatives (n=62, 0.16%) |
Opioids (n=130, 0.35%) |
Tranquilizers (n=51, 0.13%) |
Stimulants (n=61, 0.16%) |
|
| Age (mean) | 37.61 (0.97) | 34.21 (0.68) | 34.19 (1.06) | 29.61 (0.99) | 35.33 (2.01) | 34.77 (1.50) | 31.48 (2.06) | 31.00 (2.04) |
| Gender | ||||||||
| Female | 45.55 (2.93) | 43.75 (2.65) | 38.17 (3.28) | 43.78 (4.45) | 48.03 (7.05) | 35.19 (4.72) | 33.37 (6.77) | 48.94 (7.81) |
| Male | 54.45 (2.93) | 56.25 (2.65) | 61.83 (3.28) | 56.22 (4.45) | 51.97 (7.05) | 64.81 (4.72) | 66.63 (6.77) | 51.06 (7.81) |
| Ethnicity | 0.00 (0.00) | |||||||
| White | 77.35 (2.72) | 75.18 (2.24) | 81.97 (2.79) | 78.12 (3.84) | 70.65 (6.30) | 71.27 (4.63) | 79.96 (5.86) | 77.85 (6.49) |
| No-White | 22.65 (2.72) | 24.82 (2.24) | 18.03 (2.79) | 21.88 (3.84) | 29.35 (6.30) | 28.73 (4.63) | 20.04 (5.86) | 22.15 (6.49) |
| Pain scale (mean) | 1.94 (0.07) | 2.01 (0.06) | 1.98 (0.07) | 1.90 (0.11) | 2.11 (0.19) | 2.32 (0.16) | 2.00 (0.22) | 1.86 (0.18) |
| Past-year psychiatric disorders | ||||||||
| Anxiety disorders | 26.32 (2.35) | 24.72 (2.09) | 28.02 (2.92) | 28.14 (3.98) | 38.56 (7.27) | 31.79 (5.90) | 50.15 (8.35) | 35.43 (7.77) |
| Mood disorders | 25.82 (2.14) | 22.78 (1.92) | 27.03 (2.75) | 36.11 (4.11) | 54.38 (7.13) | 40.05 (5.04) | 48.90 (7.64) | 38.21 (7.79) |
| Alcohol use disorders | 37.21 (2.93) | 44.46 (2.42) | 41.68 (3.16) | 56.98 (3.96) | 39.79 (7.03) | 57.53 (4.76) | 57.49 (8.35) | 62.84 (7.59) |
| Drug use disorders a | 18.29 (2.40) | 21.36 (1.89) | 29.00 (3.37) | 40.57 (4.26) | 34.86 (7.33) | 37.20 (5.37) | 53.77 (8.22) | 49.59 (7.80) |
| Personality disorders | ||||||||
| Cluster A | 27.58 (2.70) | 26.64 (1.98) | 29.73 (3.39) | 41.14 (4.39) | 49.28 (7.79) | 41.01 (5.40) | 55.30 (8.43) | 59.08 (7.07) |
| Cluster B | 42.94 (2.86) | 40.91 (2.23) | 49.76 (3.55) | 55.13 (4.39) | 63.27 (7.32) | 56.46 (5.04) | 75.44 (6.82) | 56.81 (8.22) |
| Cluster C | 20.24 (2.12) | 21.05 (1.86) | 22.29 (2.60) | 27.77 (4.00) | 35.32 (6.77) | 29.22 (5.06) | 27.55 (7.27) | 36.70 (7.67) |
Other than nonmedical prescription drug use disorders.
The 12-month prevalence of prescription drug use disorders ranged from 0.13% for tranquilizers to 0.35% for opioids. Individuals with prescription drug use disorders were on average also in their fourth decade of life and the majority was male and White. Level of pain was also numerically lowest among those with stimulant use disorder (1.86) and highest among those with prescription opioid use disorder (2.32). Alcohol use disorders were also the most common co-occurring axis I disorders for all drug groups, except for sedative use disorders, where mood disorders were more common. Cluster B remained the most common personality disorders among all drug groups, and were particularly prevalent among individuals with tranquilizer use disorders (75.44%).
3.1 Exploratory factor analyses
For both non-medical prescription drug use and prescription drug use disorders the tetrachoric correlations between the drugs were all above 0.6 (Table 2), and single-factor models provided an excellent fit to the data in the EFA (Table 3). For non-medical prescription drug use, only one eigenvalue was larger than one (3.1), with all others well below one (0.4, 0.3, and 0.2). The fit indices were CFI= 1.00, TLI= 1.00, RMSEA<0.001, and SRMR=0.07. For prescription drug use disorders, there was also only one eigenvalue above one (3.2), with all others below one (0.4, 0.3, and 0.1). The fit indices were CFI= 0.99, TLI= 0.99, RMSEA<0.01, and SRMR=0.02.
Table 2.
Tetrachoric correlations between nonmedical prescription drug use and use disorders. NESARC Wave 1 (n= 43093)
| Non-medical prescription drug use | Sedatives | Opioids | Tranquilizers | Stimulants |
|---|---|---|---|---|
| Sedatives | 1.00 | |||
| Opioids | 0.71 | 1.00 | ||
| Tranquilizers | 0.78 | 0.77 | 1.00 | |
| Stimulants | 0.65 | 0.69 | 0.66 | 1.00 |
|
| ||||
| Prescription drug use disorders | Sedatives | Opioids | Tranquilizers | Stimulants |
|
| ||||
| Sedatives | 1.00 | |||
| Opioids | 0.76 | 1.00 | ||
| Tranquilizers | 0.84 | 0.75 | 1.00 | |
| Stimulants | 0.73 | 0.71 | 0.64 | 1.00 |
Table 3.
Exploratory factor analyses of past-year non-medical use of prescription drugs and prescription drug use disorders. NESARC Wave 1.
| Non-Medical use of prescription drugs | Prescription drug use disorders | |
|---|---|---|
| Chi-square (df) p-value | 1.40(2) 0.50 | 2.80(2) 0.25 |
| CFI | 1.00 | 0.99 |
| TLI | 1.00 | 0.99 |
| RMSEA | <0.001 | <0.01 |
| SRMR | 0.07 | 0.02 |
|
| ||
| Prescription drugs | ||
|
| ||
| Loading | Loading | |
| Sedatives | 0.836 | 0.933 |
| Opioids | 0.861 | 0.830 |
| Tranquilizers | 0.892 | 0.921 |
| Stimulants | 0.794 | 0.791 |
df= degrees of freedom; CFI= comparative fit index; TLI= Tucker-Lewis index; RMSEA= root mean squared error of approximation; SRMR= standardized root mean square residual.
3.2 Multiple Indicators Multiple Causes
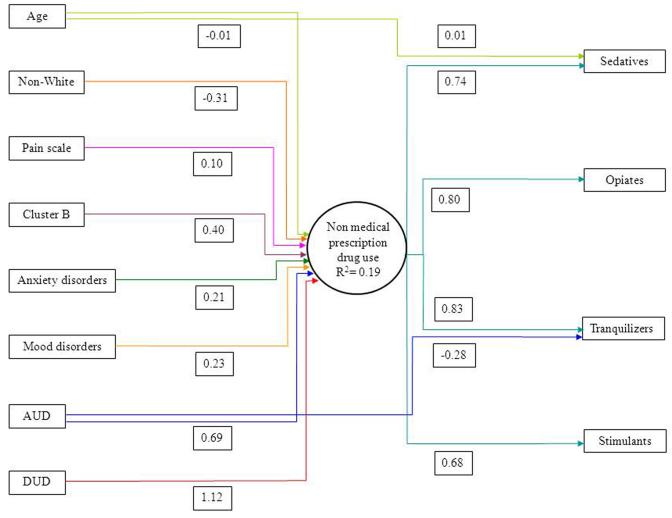
Younger age, being White, having more intense pain, and having Cluster B personality disorders, anxiety, mood, alcohol or drug use disorders were associated with significantly greater prevalence of non-medical prescription drug use through the latent factor (Figure 1). Furthermore, after adjusting for effect of the covariates on the factor, older age was associated with higher prevalence of non-medical use of sedatives, whereas having AUD associated with lower prevalence of non-medical tranquilizer use. Overall, 19% of the nonmedical prescription drug use was explained by all the covariates.
Figure 1.
Multiple Indicators Multiple Causes Model (MIMIC) among nonmedical prescription drug use. All effects shown are significant at p<0.05.
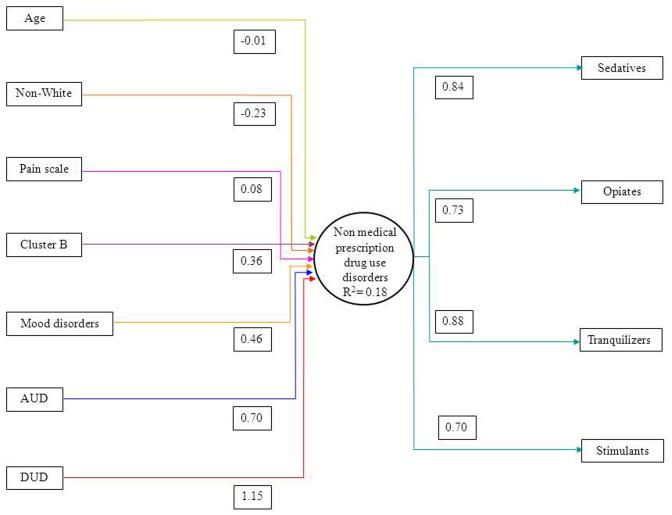
All covariates, except for anxiety disorders, that were significantly associated with non-medical use were also associated with prescription drug use disorders through common latent factor (Figure 2). There were no significant direct effects in the model, indicating that all the associations of the covariates on the risk of prescription drug use disorders occurred through the latent factor. Overall, 18% of the variance in prescription drug use disorders was explained by all the covariates. In both analyses, neither gender nor cluster A and C personality disorders were significantly associated with non-medical prescription use or prescription drug use disorders either through the factor or through direct effects.
Figure 2.
Multiple Indicators Multiple Causes Model (MIMIC) among nonmedical prescription drug use disorders. All effects shown are significant at p<0.05.
4. DISCUSSION
In a large national sample of US adults the latent structure of non-medical use of opioids, sedatives, tranquilizers and stimulants was well described by a single factor. The latent structure of prescription drug use disorders of those four drugs was also well described by a single underlying factor. Several correlates were associated with increased prevalence of both non-medical use and for prescription drug use disorder. In the case of prescription drug use disorder, the associations of the correlates occurred exclusively through the latent factor, whereas in the case of non-medical prescription drug use, some direct associations of the correlates with specific drugs were identified.
Despite the different and sometimes even opposite psychopharmacological effects of the different types of prescription drugs, we found that the latent structure of non-medical prescription drug use was well described by one factor. Consistent with our first hypothesis, all correlates were associated with greater prevalence of non-medical use of all drugs through the latent factor. Our findings are in accord with prior studies indicating that psychiatric disorders are strongly associated to non-medical prescription drugs (Blanco et al., 2007; Kaloyanides et al., 2007; McCabe et al., 2006, 2005; Simoni-Wastila and Strickler, 2004). In contrast, AUD was differentially associated with lower prevalence of non-medical use of tranquilizers, but our predictions of the differential association of other correlates with other specific drugs were not supported. Taken together, our results are generally not consistent with our second hypothesis and indicate that the association of psychiatric disorders with non-medical prescription drug use is mainly through their association with a common liability underlying the risk for non-medical prescription drug use.
The results of our analysis of prescription drug use disorders were even stronger. Paralleling our findings of the structure of non-medical use, the latent structure of prescription drug use disorder was also well described by a single factor. In line with our results regarding non-medical use, we found that all correlates (except anxiety disorders) were associated with greater prevalence of all prescription drug use disorders through the latent factor. Our findings are consistent with an extensive literature documenting the role of psychiatric disorders, including personality disorders in the etiology and persistence of substance use disorders (Blanco et al., 2013c; Compton et al., 2007; Hasin et al., 2011; Lopez-Quintero et al., 2011; Martins et al., 2012). Furthermore, we found no direct associations of any of the covariates with any of the prescription drug use disorders. Although the cross-sectional design of our study does not allow to draw causal inferences, this finding of lack of specificity between the association of psychiatric disorders with individual prescription drug use disorders argues against the self-medication hypothesis, in accord with recent analyses of the temporal relationship between anxiety disorders and alcohol and drug use (Robinson et al., 2011), or suggest that self-medication may not be inherently symptom/pharmacologic action specific. It is possible that specific psychiatric disorders may differentially influence initiation of non-medical use of certain substances, but once non-medical use is established, the role of psychiatric disorders on the risk of prescription drug use disorders development may be less drug-specific.
Our findings have implications for treatment, prevention and policy. From the treatment and prevention perspective, our findings of a latent variable underlying the four types of prescription drug use disorders examined in this study suggest that targeting disorders individually may be less efficient or successful than targeting their underlying shared liability. Our results may be particularly important for the pharmacological management of these disorders and for future medication development, as there are currently no medications that simultaneously target the receptors of all four types of prescription drugs. Our findings also highlight the potential utility of evidence-based non-pharmacological interventions that can target polysubstance use disorders, such as cognitive-behavioral therapy with relapse prevention. A better understanding of the biological and psychological factors underlying this shared liability may be useful in developing more effective treatments for prescription drug use disorders. A second implication of our findings is that, because the association of prescription drug use disorders and their correlates appear to occur mainly through a common factor, interventions directed at those correlates such as treatment of comorbid psychiatric disorders or effective approaches to pain reduction are likely to simultaneously reduce the liability for all prescription drug use disorders. Furthermore, our results suggest that those interventions could have a multiplicative effect if they also contribute to reduce the risk of non-medical drug use, and thus the probability of transition from non-medical drug use to prescription drug use disorder.
Our results have also policy implications. To date, most efforts at addressing prescription drug use disorders and non-medical use of prescription drugs have been targeted at controlling the prescription of opioid analgesics (Manchikanti, 2007; Wang and Christo, 2009). Although those approaches may yield some positive outcomes, our results suggest the need for a broader focus. At the population level, this may include educational campaigns that provide information about the potential adverse consequences of the non-medical use of prescription drugs (including the growing problem of prescription overdose death), as well as promoting restrictive social norms towards this use (Keyes et al., 2012). Most prescription opioids used for nonmedical purposes are obtained either directly or indirectly from physicians (SAMHSA, 2011). Thus, it may also benefit from the expansion of measures directed at curtailing doctor-shopping, such as the requiring the use of registries by treatment clinicians to ensure that patients are not receiving multiple prescriptions from different providers. For those already engaged in non-medical use of one drug, early brief interventions may decrease the probability of non-medical use of additional drugs, or the progression towards prescription drug use disorders (Blanco et al., 2013a; Martins et al., 2009).
This study should be interpreted in light of some limitations. First, information on non-medical prescription drug use was based on self-report and not confirmed via biological measures. Second, our sample is limited to adults. The structure of non-medical use and prescription drug use disorders may differ in adolescents, which are at increased risk of non-medical use of these drugs (McCabe et al., 2008). Third, the NESARC collected information on a broad group of prescriptions drugs. Thus, we were unable to examine individual medications, which may have differences in addiction liability. Fourth, data on ADHD were not collected in Wave 1 of the NESARC and thus, could not be included in these analyses.
In conclusion, the risk for non-medical prescription drug use and prescription drug use disorders appears to occur through a shared liability. The association of non-medical use and prescription drug use disorders with their correlates also appears to occur through this latent vulnerability. These results suggest that treatment, prevention and policy approaches directed at these drugs as a group may be more effective than those focused on individual classes of drugs.
Acknowledgments
Role of Funding Source: The National Epidemiologic Survey on Alcohol and Related Conditions was sponsored by the National Institute on Alcohol Abuse and Alcoholism with supplemental support from the National Institute on Drug Abuse. Work on this manuscript was supported by NIH grants DA019606, DA023200, DA023973, CA133050, MH076051 and MH082773 (Dr. Blanco), and the New York State Psychiatric Institute (Dr. Blanco). The sponsors had no additional role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
Dr. Blanco and Ms. Rafful designed the study and wrote the initial draft of the manuscript. Drs. Wall and Jin and Mr. Kerridge conducted the data analyses. Dr. Schwartz contributed to subsequent revisions of the manuscript. All authors contributed to and approved the final manuscript.
Conflict of interest
None.
REFERENCES
- Agrawal A, Lynskey MT, Madden PAF, Bucholz KK, Heath AC. A latent class analysis of illicit drug abuse/dependence: results from the National Epidemiological Survey on Alcohol and Related Conditions. Addiction. 2006;102:94–104. doi: 10.1111/j.1360-0443.2006.01630.x. [DOI] [PubMed] [Google Scholar]
- Blanco C, Alderson D, Ogburn E, Grant BF, Nunes EV, Hatzenbuehler ML, Hasin DS. Changes in the prevalence of non-medical prescription drug use and drug use disorders in the United States: 1991-1992 and 2001-2002. Drug Alcohol Depend. 2007;90:252–260. doi: 10.1016/j.drugalcdep.2007.04.005. [DOI] [PubMed] [Google Scholar]
- Blanco C, Iza M, Schwartz RP, Rafful C, Wang S, Olfson M. Probability and predictors of treatment-seeking for prescription opioid use disorders: a national study. Drug Alcohol Depend. 2013a;131:143–148. doi: 10.1016/j.drugalcdep.2012.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanco C, Krueger RF, Hasin DS, Liu SM, Wang S, Kerridge BT, Saha T, Olfson M. Mapping common psychiatric disorders: structure and predictive validity in the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry. 2013b;70:199–208. doi: 10.1001/jamapsychiatry.2013.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanco C, Secades-Villa R, Garcia-Rodriguez O, Labrador-Mendez M, Wang S, Schwartz RP. Probability and predictors of remission from life-time prescription drug use disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J. Psychiatr. Res. 2013c;47:42–49. doi: 10.1016/j.jpsychires.2012.08.019. [DOI] [PubMed] [Google Scholar]
- Bohnert ASB, Fudalej S, Ilgen MA. Increasing poisoning mortality rates in the United States, 1999-2006. Public Health Rep. 2010;125:542–547. doi: 10.1177/003335491012500409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohnert ASB, Valenstein M, Bair MJ, Ganoczy D, McCarthy JF, Ilgen MA, Blow FC. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011;305:1315–1321. doi: 10.1001/jama.2011.370. [DOI] [PubMed] [Google Scholar]
- Compton WM, Thomas YF, Stinson FS, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch. Gen. Psychiatry. 2007;64:566–576. doi: 10.1001/archpsyc.64.5.566. [DOI] [PubMed] [Google Scholar]
- Compton WM, Volkow ND. Abuse of prescription drugs and the risk of addiction. Drug Alcohol Depend. 2006;83:S4–S7. doi: 10.1016/j.drugalcdep.2005.10.020. [DOI] [PubMed] [Google Scholar]
- Fenton MC, Keyes KM, Martins SS, Hasin DS. The role of a prescription in anxiety medication use, abuse, and dependence. Am. J. Psychiatry. 2010;167:1247–1253. doi: 10.1176/appi.ajp.2010.09081132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischer B, Lusted A, Roerecke M, Taylor B. The prevalence of mental health and pain symptoms in general population samples reporting nonmedical use of prescription opioids: a systematic review and meta-analysis. J. Pain. 2012;13:1029–1044. doi: 10.1016/j.jpain.2012.07.013. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend. 2003;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Goldstein RB, Chou SP, Huang B, Stinson FS, Dawson DA, Saha TD, Smith SM, Pulay AJ, Pickering RP. Sociodemographic and psychopathologic predictors of first incidence of DSM-IV substance use, mood and anxiety disorders: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Mol. Psychiatry. 2009;14:1051–1066. doi: 10.1038/mp.2008.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Harford TC, Dawson DA, Chou PS, Pickering RP. The Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS): reliability of alcohol and drug modules in a general population sample. Drug Alcohol Depend. 1995;39:37–44. doi: 10.1016/0376-8716(95)01134-k. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Pickering RP, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch. Gen. Psychiatry. 2004a;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Ruan W, Pickering RP. Co-occurrence of 12-month alcohol and drug use disorders and personality disorders in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch. Gen. Psychiatry. 2004b;61:361–368. doi: 10.1001/archpsyc.61.4.361. [DOI] [PubMed] [Google Scholar]
- Hall AJ, Logan JE, Toblin RL, Kaplan JA, Kraner JC, Bixler D, Crosby AE, Paulozzi LJ. Patterns of abuse among unintentional pharmaceutical overdose fatalities. JAMA. 2008;300:2613–2620. doi: 10.1001/jama.2008.802. [DOI] [PubMed] [Google Scholar]
- Hasin D, Fenton MC, Skodol A, Krueger R, Keyes K, Geier T, Greenstein E, Blanco C, Grant B. Personality disorders and the 3-year course of alcohol, drug, and nicotine use disorders. Arch. Gen. Psychiatry. 2011;68:1158–1167. doi: 10.1001/archgenpsychiatry.2011.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch. Gen. Psychiatry. 2007;64:830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- Hernandez SH, Nelson LS. Prescription drug abuse: insight into the epidemic. Clin. Pharmacol. Ther. 2010;88:307–317. doi: 10.1038/clpt.2010.154. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM, Kano Y. Can test statistics in covariance structure analysis be trusted? Psychol. Bull. 1992;112:351–362. doi: 10.1037/0033-2909.112.2.351. [DOI] [PubMed] [Google Scholar]
- Joreskog K, Moustaki I. Factor analysis of ordinal variables: a comparison of three approaches. Multivariate Behav. Res. 2001;36:347–387. doi: 10.1207/S15327906347-387. [DOI] [PubMed] [Google Scholar]
- Kaloyanides KB, McCabe SE, Cranford JA, Teter CJ. Prevalence of illicit use and abuse of prescription stimulants, alcohol, and other drugs among college students: relationship with age at initiation of prescription stimulants. Pharmacotherapy. 2007;27:666–674. doi: 10.1592/phco.27.5.666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Schulenberg JE, O’Malley PM, Johnston LD, Bachman JG, Li G, Hasin D. Birth cohort effects on adolescent alcohol use: the influence of social norms from 1976 to 2007. Arch. Gen. Psychiatry. 2012;69:1304–1313. doi: 10.1001/archgenpsychiatry.2012.787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim ES, Yoon M, Lee T. Testing measurement invariance using MIMIC: likelihood ratio test with a critical value adjustment. Educ. Psychol. Meas. 2011;72:469–492. [Google Scholar]
- Krueger RF. The structure of common mental disorders. Arch. Gen. Psychiatry. 1999;56:921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- Lopez-Quintero C, Cobos JP, Hasin DS, Okuda M, Wang S, Grant BF, Blanco C. Probability and predictors of transition from first use to dependence on nicotine, alcohol, cannabis, and cocaine: results of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Drug Alcohol Depend. 2011;115:120–130. doi: 10.1016/j.drugalcdep.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manchikanti L. National drug control policy and prescription drug abuse: facts and fallacies. Pain Physician. 2007;10:399–424. [PubMed] [Google Scholar]
- Markon KE, Krueger RF. Categorical and continuous models of liability to externalizing disorders: a direct comparison in NESARC. Arch. Gen. Psychiatry. 2005;62:1352–1359. doi: 10.1001/archpsyc.62.12.1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins S, Fenton M, Keyes K, Blanco C, Zhu H, Storr C. Mood and anxiety disorders and their association with non-medical prescription opioid use and prescription opioid-use disorder: longitudinal evidence from the National Epidemiologic Study on Alcohol and Related Conditions. Psychol. Med. 2012;42:1261–1272. doi: 10.1017/S0033291711002145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins SS, Keyes KM, Storr CL, Zhu H, Chilcoat HD. Pathways between nonmedical opioid use/dependence and psychiatric disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Drug Alcohol Depend. 2009;103:16–24. doi: 10.1016/j.drugalcdep.2009.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Cranford JA, Boyd CJ. The relationship between past-year drinking behaviors and nonmedical use of prescription drugs: prevalence of co-occurrence in a national sample. Drug Alcohol Depend. 2006;84:281–288. doi: 10.1016/j.drugalcdep.2006.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Cranford JA, West BT. Trends in prescription drug abuse and dependence, co-occurrence with other substance use disorders, and treatment utilization: results from two national surveys. Addict. Behav. 2008;33:1297–1305. doi: 10.1016/j.addbeh.2008.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Teter CJ, Boyd CJ, Knight JR, Wechsler H. Nonmedical use of prescription opioids among US college students: prevalence and correlates from a national survey. Addict. Behav. 2005;30:789–805. doi: 10.1016/j.addbeh.2004.08.024. [DOI] [PubMed] [Google Scholar]
- Muthen LK, Muthen BO. Mplus version 4 User’s Guide. Muthen & Muthen; Los Angeles: 2006. [Google Scholar]
- Olfson M, Blanco C, Wang S, Greenhill LL. Trends in office-based treatment of adults with stimulants in the United States. J. Clin. Psychiatry. 2013;74:43–50. doi: 10.4088/JCP.12m07975. [DOI] [PubMed] [Google Scholar]
- Olfson M, Crystal S, Iza M, Wang S, Blanco C. National trends in office-based prescription of schedulle II opioids. J. Clin. Psychiatry. doi: 10.4088/JCP.13m08349. in Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulozzi LJ, Budnitz DS, Xi Y. Increasing deaths from opioid analgesics in the United States. Pharmacoepidemiol. Drug Saf. 2006;15:618–627. doi: 10.1002/pds.1276. [DOI] [PubMed] [Google Scholar]
- Poulin C. From attention-deficit/hyperactivity disorder to medical stimulant use to the diversion of prescribed stimulants to non-medical stimulant use: connecting the dots. Addiction. 2007;102:740–751. doi: 10.1111/j.1360-0443.2007.01758.x. [DOI] [PubMed] [Google Scholar]
- Resnik DB, Rehm M. The undertreatment of pain: scientific, clinical, cultural, and philosophical factors. Med. Health Care Philosoph. 2001;4:277–288. doi: 10.1023/a:1012057403159. [DOI] [PubMed] [Google Scholar]
- Robinson J, Sareen J, Cox BJ, Bolton JM. Role of self-medication in the development of comorbid anxiety and substance use disorders: a longitudinal investigation. Arch. Gen. Psychiatry. 2011;68:800–807. doi: 10.1001/archgenpsychiatry.2011.75. [DOI] [PubMed] [Google Scholar]
- Ruan W, Goldstein RB, Chou SP, Smith SM, Saha TD, Pickering RP, Dawson DA, Huang B, Stinson FS, Grant BF. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of new psychiatric diagnostic modules and risk factors in a general population sample. Drug Alcohol Depend. 2008;92:27–36. doi: 10.1016/j.drugalcdep.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAMHSA . Results from the 2010 National Survey on Drug Use and Health: Summary of National Findings. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2011. [Google Scholar]
- Schepis TS, Hakes JK. Non-medical prescription use increases the risk for the onset and recurrence of psychopathology: results from the National Epidemiological Survey on Alcohol and Related Conditions. Addiction. 2011;106:2146–2155. doi: 10.1111/j.1360-0443.2011.03520.x. [DOI] [PubMed] [Google Scholar]
- Simoni-Wastila L, Strickler G. Risk factors associated with problem use of prescription drugs. Am. J. Public Health. 2004;94:266–268. doi: 10.2105/ajph.94.2.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stark S, Chernyshenko OS, Drasgow F. Detecting differential item functioning with confirmatory factor analysis and item response theory: toward a unified strategy. J. Appl. Psychol. 2006;91:1292–1306. doi: 10.1037/0021-9010.91.6.1292. [DOI] [PubMed] [Google Scholar]
- Swanson JM, Volkow ND. Increasing use of stimulants warns of potential abuse. Nature. 2008;453:586–586. doi: 10.1038/453586a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J, Christo PJ. The influence of prescription monitoring programs on chronic pain management. Pain Physician. 2009;12:507–515. [PubMed] [Google Scholar]
- Ware J, Kosinski M, Turner-Bowker DM, Gandek B. SF-12v2: How to score version 2 of the SF-12 Health Survey. Quality Metric Incorporated Health Assessment Lab Boston; Massachusetts Lincoln, Rhode Island: 2002. [Google Scholar]
- Wirth RJ, Edwards MC. Item factor analysis: current approaches and future directions. Psychol. Methods. 2007;12:58–79. doi: 10.1037/1082-989X.12.1.58. [DOI] [PMC free article] [PubMed] [Google Scholar]