Abstract
Objective
Women delay seeking care for symptoms of Acute Coronary Syndromes (ACS) because of atypical symptoms, perceptions of invulnerability, or keeping symptoms to themselves. The purpose of this study was to explore how women recognized and interpreted their symptoms and subsequently decided whether to seek treatment within the context of their lives.
Method
Grounded theory was used to provide the methodological basis for data generation and analysis. Data were collected using in-depth interviews with 9 women with ACS.
Results
All participants went through a basic social process of searching for the meaning of their symptoms which informed their decisions about seeking care. Stages in the process included noticing symptoms, forming a symptom pattern, using a frame of reference, finding relief, and assigning causality. The evolving MI group (n=5) experienced uncertainty about bodily cues, continued life as usual, until others moved them towards care. The immediately recognizable MI group (n=4) labeled their condition quickly, yet delayed, as they prepared themselves and others for their departure.
Conclusions
All women delayed, regardless of their ability to correctly label their symptoms. Education aimed at symptom recognition/interpretation addresses only part of the problem. Women also should be educated about the potential danger of overestimating the time they have to seek medical attention.
INTRODUCTION
Every 34 seconds an American has an acute coronary event and approximately half of these events result in death.1 Treatments for acute coronary ischemia are time dependent. In fact, prehospital delay is one of the best predictors of in-hospital complications, including recurrent ischemia, re-infarction, ventricular arrhythmias, and cardiac death.2 Yet despite the clear advantage of timely treatment, many do not seek treatment within the optimal time period.
Three phases of prehospital treatment-seeking phases have been identified in the literature.3 These phases include (1) the time from symptom onset to the decision to seek medical treatment, (2) the time from decision to seek medication attention to the arrival of the first medical contact, and (3) the time from the first medical contact to hospital arrival (transport time). The first time interval, the time of symptom onset to the time a decision is made to seek treatment, is uniquely dependent on individual decision making by the woman experiencing symptoms. Proportionally, this time period accounts for three-quarters of the total prehospital time interval.4
The majority of studies have found that women delay seeking care for cardiac symptoms longer than men.5-11 Data from the National Registry of Myocardial Infarction which included 482,327 subjects (33.2 % women) reported an average delay for women of 21.6 – 36.6 minutes longer than the delay for men over the course of 10 year.6 Older age, African American or Hispanic ethnicity, low socioeconomic status, and lower educational level have been found to be predictors of increased delay,3 in addition to clinical factors such as diabetes, hypertension, high cholesterol, a history of heart failure or angina, and tobacco use.3 While knowledge of these factors is helpful in determining who is at highest risk for prehospital delay, many of these factors are not modifiable. Thus, new approaches are needed to identify causes of prehospital delay that are amenable to change.12-14
Symptom Recognition and Interpretation
Symptom recognition begins with awareness of a physical change, and this is followed by a process of symptom assessment, evaluation, and interpretation.3 During this process the individual considers potential causes of the symptoms and assesses the potential impact of the symptoms. Researchers have traditionally viewed difficulty in evaluating symptoms and assessing personal risk primarily as a knowledge deficit and/or Rpression of the meaning of symptoms as a health threat.15 Women viewing symptoms as insignificant has been considered by some researchers to reflect women’s need to maintain control of their situation.16
A major issue for women, however, is that the symptom experience is highly variable. Women are more likely than men to experience atypical symptoms,17-19 increasing the likelihood that they will attribute symptoms to non-cardiac etiologies, which in turn is associated with treatment delay.3,16,20-23 Women are also more likely to experience symptoms that do not match their expectations of a myocardial infarction,3, 16 to perceive themselves at low risk for heart disease,18,21,24 and to worry about troubling others with their symptoms;25-27; thus they may dismiss or minimize symptoms until these symptoms prevent continuation of their usual activities.16,28
However, to date, the reasons why women attend to personal and social obligations instead of attending to their emerging symptoms has not been explained fully. Sociocontextual issues have been treated largely as secondary or extenuating factors and have not been the targets of study or intervention.14 Editorials by thought leaders in the field have recognized a need to tie theory to findings in the current literature related to prehospital delay.3,13,14 Thus innovative approaches are needed to seek out underlying psychosocial causes of prehospital delay (beyond knowledge deficits) that are amendable to change.12-14 Therefore, the purpose of this study was to explore how women with symptoms of acute coronary syndrome (ACS) recognized and interpreted their symptoms and subsequently decided whether to seek treatment within the context of their lives.
METHODS
Design
A qualitative research approach was chosen to explore thoughts and behaviors of women related to how they recognize, interpret, and act upon acute cardiac symptoms, allowing for contextual, historical and situational variation.29 Grounded theory was used to examine the process women used to make meaning of their symptoms/situation within their larger social context.30 The study was approved by the institutional review board (IRB) at the university where the study was conducted, and all participants signed a consent form prior to being interviewed by the first author.
Participants and Settings
Participants included women age 35 years and older who had been hospitalized with a definitive diagnosis of ACS. The term ACS describes patients who present with either unstable angina (UA) or an acute MI (inclusive of those with and without ST segment elevation) because these conditions share common pathophysiological mechanisms related to plaque instability, rupture, with or without total occlusion.1 For this study ACS was defined as having symptoms of acute cardiac ischemia and at least one of the following: positive cardiac enzyme levels, electrocardiographic changes showing evidence of ACS, and/or significant cardiac disease as noted by a cardiac catheterization during the index hospitalization. Women were excluded if they were experiencing hemodynamic instability or were unable to understand spoken English.
Maximum variation sampling was initially used to maximize diversity in race, ethnicity, social class, educational level, employment status, and past medical history. As the study progressed, theoretical variations were identified from the data from the initial participants and theoretical sampling was used.30 For example, women with comorbid conditions and recurrent ACS events were sampled purposively to explore the possible influences related to the differentiation of ACS symptoms from other bodily symptoms. Recruitment ceased when saturation was achieved. Saturation was determined after the primary investigator and senior researchers recognized repetition in the data collected. In qualitative research, it is through repetition and confirmation of previously collected data that determines completion of data collection, as opposed to a specific number of subjects.31 Furthermore, each interview concluded with the researcher summarizing the content to the woman interviewed to confirm that salient points were heard as a means to Rport truthfulness. One woman had a follow-up interview to reach a more complete degree of closure.
Data Collection
The first author conducted one-on-one audio recorded in-depth semi-structured interviews with all participants. The interviews began with a broad question to invite participants to tell their story. Follow-up and probing questions were then used to gather more information.32 Interviews were conducted either during the participant’s hospitalization or within 2 weeks of discharge in the participant’s home. They averaged 46 minutes in length (SD 9.4; range 33 to 66).
Data Analysis
Congruent with the tenets of grounded theory, data collection and analysis occurred simultaneously. Constant case comparison was used to systematically explore the process women used to make meaning of their symptoms, and memos were written as ideas were developed from the data analysis.30 Initial codes and categories were derived inductively from early interviews. Although themes and relationships between concepts/categories were initially tentative, they began to take shape as more data were generated.30 As new themes emerged, decision rules were modified, and all cases were reviewed to ascertain goodness of fit. The analysis was thus an evolving process.29, 33
Rigor of the Study
Trustworthiness of the research was optimized by taking measures to address credibility, dependability, and transferability of the findings. Credibility was maintained by asking participants open-ended questions, transcribing the data verbatim, and retaining audio recordings. Dependability (i.e., the tracking of processes and procedures to collect and interpret data)34 was addressed by engaging with senior researchers and methodological mentors to account for all major decisions related to data collection and data analysis. A log of definitions was used for coding and memos were used to track methodological and analytical decisions, this audit trail provided detailed and thorough explanations of how the data were generated and analyzed. Transferability (i.e,. the likelihood that the findings from this study will be useful in other settings)34 was addressed by using rich descriptions of the experience to present a realistic picture of the phenomenon.
RESULTS
The Sample
The sample included nine women who met the selection criteria and agreed to participate in the study. Six of the 9 participants had a confirmed MI, one of which was a ST segment elevation MI; the other 3 women had unstable angina. The women ranged in age from 49 to 74 years (mean 60.7; SD 9.0). Four were African American and five were Caucasian. Six were either married or living with a significant other; three were divorced or widowed. Most (n = 7) did not have any education beyond high school. Two-thirds (n = 6) of the women were on a fixed income (retired or on permanent disability); the remainder were hourly minimum wage workers. Household incomes were low, with over half below $ 40,000/year for 1-2 adults in the household. All participants, but one, were insured. All had known risk factors for heart disease; however, not all were being treated for the condition.
The Basic Social Process
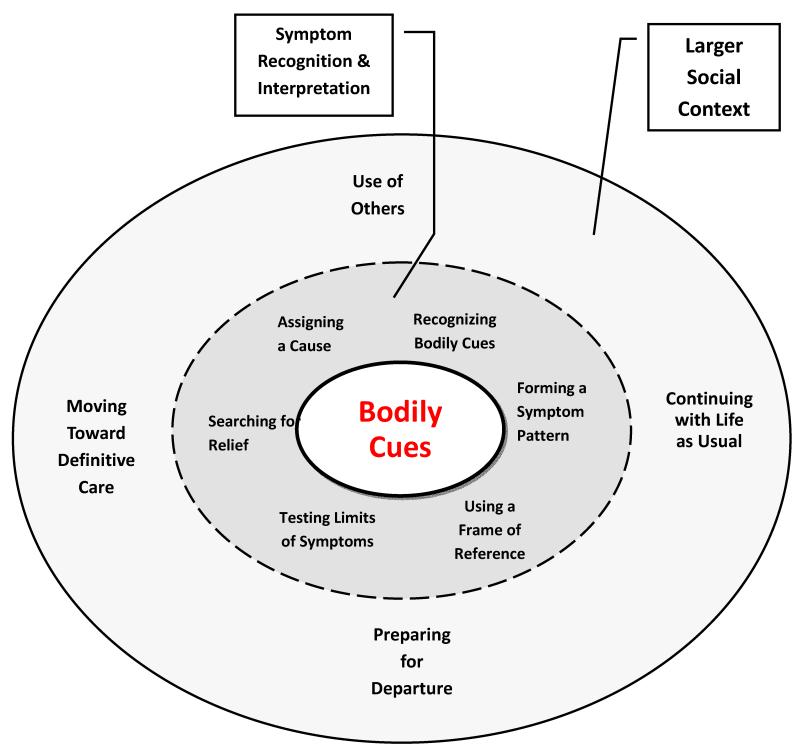
All of the women went through a basic social process of searching for the meaning of their symptoms, and this informed their decisions about seeking care. Within the basic process there were two core categories: (1) symptom recognition and interpretation, and (2) the larger social context (See Figure 1). Within the first core category, symptom recognition and interpretation began with the initial illness-related stimuli, bodily cues. The bodily cues, which accumulated over time for some, helped shape and reshape the meaning of the experience. However, the women’s search for meaning of their symptoms did not center on one piece of information. Having symptoms that were consistent enough to recognize relationships between symptoms allowed some women to form a united pattern, helping them label the situation. The women put great effort into classifying symptoms in a pattern that made sense. However, formulating a coherent symptom pattern for most of the women did not occur at a single point in time but, rather, was part of an unfolding process that required time, energy, and resources. Furthermore, the search for meaning was embedded in the second core category, the larger social context, as the women tried to interpret what was happening to them and to manage their relationships and social obligations. Key aspects of this process were described by the women in their interviews. However, not every woman went through each stage of the process; some went through the stages faster than others. How and when each stage was used for the women differed.
Figure 1.
The Core Process: Searching for the Meaning of Symptoms
Participants fell into two groups Group 1 (n=5), the evolving myocardial infarction (MI) group, experienced uncertainty about bodily cues. Symptoms were ever-changing and drawn out, and the women could not make sense of them, despite trying to label them (See Table 1). For this group, there was no clear differentiation between premonitory symptoms, prodromal symptoms, or acute symptoms of the ACS event. This lack of a clear transition to acute symptoms slowed the process of moving towards care. Unable to form a symptom pattern, they returned to their usual life, though they continued to monitor symptoms. Group 2 (n=4), the immediately recognizable MI group, had more prominent symptoms, formed a symptom pattern quickly, and labeled their condition early on (See Table 2). Initial symptoms for this group were very discrete, consistent with acute symptoms of an ACS event. In addition to differences in symptom interpretation, the two groups differed in their help-seeking behaviors. Notably, the groups did not however differ on type of ACS event (STEMI, nonSTEMI, versus unstable angina); each group was mixed.
Table 1. Symptom Characteristics for the Evolving MI Group.
| Characteristics | Descriptors | Illustrative Quotes |
|---|---|---|
| Main symptom(s) |
Initially low number of symptoms; vague; non- specific; lacking definition |
“I just kinda felt strange” “I have a lot of medical problems, a lot of pain and other issues. On an average day, nothing unusual, not really with my heart. Up until then, it was just funny that something wasn’t right…that day”. |
| Location | Initial location of symptoms | “The only thing that bothered me then was the burning in the throat.” “I had started coughing a lot.” |
| Onset | Gradual; hard to pinpoint exact time of onset. |
“It was not just all of a sudden – one thing.” “It probably started like a few months ago.” |
| Nature and duration |
Intermittent, inconsistent; spread over days or weeks. |
“It started in my lower part of my back and would creep up to my shoulders. Later on it was only down one arm.” |
| Intensity | Initially mild; gradually intensified in quality and quantity of symptoms. |
“My symptoms are kinda weird. I don’t have really strong symptoms. I just have this feeling.” “But see it wasn’t bad-bad.” |
Table 2. Stages Used by the Evolving MI Group to Recognize and Interpret Symptoms.
| Stage | Descriptors | Illustrative Quotes |
|---|---|---|
| Recognizing Bodily Cues |
Gradual recognition that something was different. |
“Well at the time, it really didn’t dawn on me that it was something new.” “I wasn’t really concerned with it … at the time”. |
| Forming Symptom Pattern |
Ambivalent about how to connect the symptoms into a meaningful whole. |
“The number of symptoms … weren’t really adding up to me. It’s (like) a big old jig saw puzzle-the whole symptom thing. It’s not right.” “I was kinda grasping for straws”. |
| Using Frame of Reference |
Reflecting on experiences of self or others to make sense of bodily cues; when symptoms were not an exact match held up assigning a label to them. |
“My momma and my grandma had a heart attack. I heard them say the same thing, burning down the throat. And burning down the arms too. So later (when arms started to burn/feel weak) I knew something was wrong. I said I was having a heart attack too.” |
| Testing the Limits of Symptom Course |
Noticing reduction in daily activities as a clue that something was wrong. |
“I did my usual sitting on the couch and lying in the bed – that’s all I could do. I was so tired that I really didn’t feel like fixing something to eat. So I skipped breakfast. I thought, I’ll get up and fix some lunch in a little bit. Lunch came,—and I didn’t… I couldn’t really do my usual because I couldn’t breathe. If I can’t get up and fix me something to eat, I mean something’s wrong.” |
| Searching for Relief and Assigning a Cause |
Used over-the-counter medication before prescription medication. Lack of effectiveness provided additional clues to causality. |
“It was like angina, but not like angina. I’m used to angina and having to take nitroglycerin. When I take nitroglycerin if I don’t get a massive headache I know something didn’t happen. I took nitro and none of that happened. I had no headache and it didn’t make me any better.” |
| Using Others to Make Sense of Symptoms |
Discussed with friends or family - often later in the symptom course when unable to figure things out on their own; sought affirmation. |
Consulting with friend on the phone the day of her heart attack: “This pain in my chest seems to be getting worse. And it’s going into my right side, which is strange. I’ve seen all these things (that) say don’t rule anything out on your own. Because it doesn’t mean that it’s not- just because it’s left side. Most people have their symptoms on their left side. Even though it’s in my right arm and shoulder and comes around, I’m not going to be silly enough to think it might not my heart.” |
| Continuing with Life as Usual |
Unable to interpret symptoms, continued with activities; yet continued to monitor symptoms |
“I kinda brushed it (off). I put it on the back burner. I got to feeling better, went back to work for a couple of days, then started feeling bad again while I was working”. |
| Moving Toward Definitive Care |
Someone or something else (incapacitating symptoms) made the decision for them to seek care |
“In the back of my mind I knew that this was something that really needed to be looked into. My body was saying, I’m not gonna do this anymore. Your body sometimes will take care of it for you. My body made my decision.” “My supervisor noticed me rubbing my arm. He asked, ‘are you ok? You look a little pale.’ I said, ‘I’ll be alright, I’ve just be working hard.’ He took my arm and said, ‘just wait a minute. I’m gonna have them check your blood pressure. Something’s not right.’ |
Evolving MI Group: Symptom Assessment and Interpretation
Noticing Bodily Cues Over Time
The first step in the process of forming a symptom pattern is recognition of bodily cues signaling that something in the body has changed. However, for most of the women in Evolving MI Group, symptoms were not immediately intense or prominent; they were not frequent, lasted little time, and were indistinguishable from usual bodily aches (Table 1). All five of the women in this group had symptom courses that were intermittent, ever-changing, and often spread out over days or weeks. The women noted that their symptoms were “peculiar”, but not initially a concern. Two women said that the early bodily cues were “not so unusual”. However, during the course of their interviews, the women began to recognize that their symptoms had actually started much earlier than they had initially thought.
Forming a Symptom Pattern
Eventually all of the women in Evolving MI Group noticed a change in their body. However, four of the five women were unable to initially form a symptom pattern, preventing them from assigning a label to what was happening to them. The women tried to interpret their bodily cues by linking symptoms together to identify a consistent symptom pattern and by comparing early symptoms with those of familiar bodily conditions, noting similarities and differences. As a result, they dismissed early symptoms as benign conditions, such as indigestion, a cold, the flu, a smoker’s cough, or pneumonia. Early monitoring then moved to a process of determining which bodily cues were present or absent. As symptoms began to occur more frequently and more intensely, the women monitored the symptoms more closely and recognized symptoms that seemed to be related, yet they were still unsure how to connect the “parts.” At that point many “knew” that their symptoms reflected more than a benign condition and they tried to form relationships among symptom features, based on starting location, the radiation of symptoms, and the quality, intensity, and duration of the symptoms. In time, most of the women in the Evolving MI Group could predict their duration when symptoms recurred. Although they could not assign a specific cause to the symptoms, they eventually labeled them as a sign of something bad. However, they remained perplexed about the meaning of the symptoms.
Using a Frame of Reference
Four of the five women in the Evolving MI Group used reflection on past experiences of self or others as a frame of reference in their search for a symptom pattern. However, because prior experiences did not exactly match current symptoms, the women had difficulty interpreting current symptoms. As time passed and symptoms evolved, the individuals called upon past references again and ultimately recognized features similar to a past heart condition. Then the women provisionally labeled their symptoms as cardiac.
Testing the Limits of the Symptom Course
As part of the process, the women in the Evolving MI Group examined the extent to which their symptoms intruded on usual daily activities. For example, one woman kept a mental record of what she could or could not do during the days her body started “giving me clues”, a few days before the heart attack. As symptoms progressed, she continued with as many of her usual activities as she could; however, she noticed that her tolerance for her activities such as walking was declining every day. Inability to keep up with “life as usual” helped the women in Group 1 gauge and interpret their symptoms as “something’s wrong” or a sign of sickness. However, they were still unable to fully interpret the symptoms.
Searching for Relief and Assigning a Cause
The women in the Evolving MI Group tried various home remedies, such as over-the-counter medications, to relieve their symptoms as they continued to collect clues about the meaning of the symptoms. As their symptoms continued, they began to use prescription medications, including nitroglycerin. The lack of effectiveness of these therapies provided additional clues to help form interpretations of their symptoms. Some women tried to assign causality to particular body systems while others hypothesized about specific things occurring in particular organs. One participant explained what went through her mind as she wrestled with interpreting her symptoms: “You start self-diagnosing in your mind. Maybe it’s not (your) heart, maybe it’s your lungs. Maybe it’s a lung collapsing with the right side (hurting) instead of the left side. I didn’t really know what to think.”
Evolving MI Group: The Larger Social Context
Use of Others
When unable to understand the cause of their symptoms, all but one of the women in the Evolving MI Group consulted with others. Some did so early in the symptom course, others much later. The women sought input from others for social comparison and advice and to validate their own thoughts about their symptoms. Despite having had a prior heart attack, one participant remained puzzled about the atypical location of her symptoms, which did not match those of the “average person”. Because one atypical feature got in the way of assigning a cause; she sought affirmation that she was not being unwise or inappropriate in thinking this “might” be her heart.
Continuing with Life As Usual
Unable to interpret what their symptoms meant, four of the five women in the Evolving MI Group put their bodily aches and pains on the “back burner” (as one woman phrased it) in order to continue with life as usual. One participant explained how she decided which symptoms could temporarily be put aside (vague, non-specific, less intense symptoms). Thus, the women in the Evolving MI Group 1 did not abandon their symptoms, but they put them in a place where they could still monitor them, while getting back to life as usual.
Moving Toward Definitive Care
The women in the Evolving MI Group eventually sought medical attention for their symptoms. However, for this group, someone or something else made the decision for them. For some of the women, trusted others witnessed their steady decline in bodily function and moved them towards care. Having others point out the need to seek medical attention gave them permission to leave their obligations – especially if they were engaged in activities that were not easily left. These women viewed seeking medical attention as a decision that was made for them, a situation that they viewed as giving up. However, they were relieved that the decision was made for them. This stage of the process for the Evolving MI Group went fairly quickly, as most of their prehospital time was spent trying to understand the symptoms themselves. Overall time of symptom onset to hospital arrival time for this group ranged from hours to days. Table 2 summarizes the stages in the process used by the Evolving MI Group to recognize and interpret their symptoms and to move towards definitive care.
The Immediately Recognizable MI Group: Symptom Assessment and Interpretation
Recognizing Symptoms Right Away
For the remaining four participants, in the Immediately Recognizable MI Group, the initial bodily cues were immediately recognizable (Table 3). Two of the women could pinpoint the exact date and time of the onset of symptoms. Three of the four women had a history of an MI; the fourth had a history of angina. Three of the four were retired nursing assistants, and thus may have also used professional knowledge to help with symptom interpretation. Three of the four women in this group knew almost instantly that the bodily cues were a sign of something very serious. For example, a 59 year old retired nursing aide knew within minutes that her bodily cues were a sign of sickness. Although her bodily cues were initially intermittent, the intensity and quality of symptoms were unmistakable. She identified with precision the moment when symptoms started and the moment when they resumed 25 minutes later.
Table 3. Symptom Characteristics for the Immediately Recognizable MI Group.
| Characteristic | Descriptors | Illustrative Quotes |
|---|---|---|
| Main symptom(s) |
Chest pain with or without associated symptoms |
“It’s a tightening in my neck and … it takes, 45 seconds, a minute, before it goes into an actual pain. My shoulders tense up. I start sweating.” |
| Location | Able to pinpoint exact location at the time of onset. |
“I get real tightened up all in my chest and in my neck.” “It started hurting in my chest. My shoulder down to my elbow and up here in my chest. Pressure.” |
| Onset | Immediate and sudden onset; without warning. |
“All of a sudden, it just hit me. The sickness came out of nowhere.” “It all happens really fast.” “All of a sudden, look like bam (slapping hands together) it hits me and gives me a fit for a while.” |
| Nature and duration |
Steadily worse; intermittent for some. |
“My chest would just hurt bad…it finally went away. And then about 10 minutes later, it comes again. …Just wham. It was actually more intense.” |
| Intensity | Severe; often disabling. | “When the pain comes, it shows. It’s very domineering. I hurt so bad.” |
Forming a Symptom Pattern
Once a change from the usual status was noted, often suddenly and without warning, the women in the Immediately Recognizable MI Group began to tune into their bodily cues in an attempt to make sense of the information. Early monitoring of the symptoms included noting the quality, the location, the intensity, radiation, and duration of the symptoms. All of the women were able to relate symptom features to form a pattern and assign a high level of seriousness to the situation early on. Most of the women “knew” early on that the bodily cues were probably related to their heart.
The Immediately Recognizable MI Group: The Larger Social Context
Use of Others
The women in the Immediately Recognizable MI Group used others to confirm or validate their initial interpretation of symptoms. For example, a very independent woman, matriarch of her family, who only consulted with her husband about urgent matters, discussed the situation with her husband when her gut told her she might be having another heart attack. She did not want to jump to conclusions; she wanted to be sure. He immediately recognized the symptoms as cardiac, which confirmed her initial thoughts.
Preparing for Departure
The women in the Immediately Recognizable MI Group used their understanding of their symptom pattern and their past experience to decide on the timing for seeking care. The women did not question whether they needed to go to the hospital; instead for them it was a question of when to seek care. When they sought care depended on other aspects of their life. One important aspect of preparing for departure was deciding who they told about their symptoms. All of the women were selective, only telling significant others or direct Rervisors (if at work). One participant said, “You don’t want to tell people sometimes because they look at your strange; some don’t believe what you are saying.” When they disclosed their circumstances, three of the four women minimized symptoms, only partially revealing the extent of their pain and the seriousness of their situation. For example, one participant talked about “not making a big deal of it” in front of her children for fear of upsetting them. Another woman joked with her husband while preparing to go to the hospital to keep him calm and prevent him from calling other family members. Some women delayed telling others about symptoms because they felt a sense of responsibility or guilt for “bringing it on” (the words on one woman).
Another important aspect of preparing for departure was taking care of personal matters. Although one participant knew right away that she needed to make a move, she prolonged it as long as possible. All the women in this group initially prayed about their symptoms and slowed their pace in the hope that symptoms would cease and they would not need to go to the hospital. As symptoms continued, they felt obliged to do certain things prior to their departure (e.g., take a bath, change clothes, pack essential items). If symptoms intensified during these necessary activities, the women in this group did not abandon the activity. Instead, they took short cuts to finish, making sure nothing was left undone.
Another part of preparing for departure involved orchestrating role changes for others. For example, for women who were at work, requesting permission to leave or finding a replacement to take over their duties was a prerequisite to their departure. The women knew who to ask, to do what, in order to leave their obligations; however making these arrangements took time.
All of the women in this group made arrangements directly with family members to provide transportation to the hospital. All decided against using an ambulance, which slowed the process even more. They believed that their family members could get to the destination as quickly as an ambulance and they preferred to be with someone they knew when having heart symptoms in case something happened. As part of these arrangements, they considered how stable they were, using information from prior experiences, and made plans should things became unstable. For example, while having symptoms, one woman discussed with her husband by phone where she would wait for him, so she could be around others in case she got worse.
Another woman waited until there was a mutually convenient day for her daughter to drive her and for her husband to get off work to accompany her to the hospital. She felt she could wait because her symptoms were stable (defined by her as not needing a third nitroglycerin tablet when symptoms occurred). Both these women had plans to call 9-1-1 if symptoms got worse and became unstable.
The Immediately Recognizable MI Group: Moving Toward Definitive Care
Deciding where to go for treatment was the final part of the help-seeking process. All of the women in the Immediately Recognizable MI Group elected to bypass the closest emergency department or doctor’s office to go to a large medical center. The women in this group had been hospitalized before for cardiac symptoms and had been transferred to a larger medical center for definitive treatment. They viewed the larger medical center as a familiar place, with more resources to treat them, and as “one stop shopping” (i.e., avoiding a potential transfer later).
Eventually all of the women in the Immediately Recognizable MI Group moved towards care. The women in this group knew they needed to seek care, yet they needed to make arrangements through their social network to leave their obligations. They needed to take care of their own personal needs first, using a timeline they had estimated in their mind. This timeline was based on prior experiences, which informed their decisions related to seeking care. The women in this group took hours to seek care. However, 2 of the 4 women had intermittent symptoms over days, thus took longer overall to seek care. Table 4 summarizes the stages in the process that the women in the Immediately Recognizable MI Group used to recognize and interpret their symptoms and the approach they took to seeking care.
Table 4. Stages Used by the Immediately Recognizable MI Group to Recognize and Interpret Symptoms.
| Stage | Descriptors | Illustrative Quotes |
|---|---|---|
| Recognition of Bodily Cues |
Immediate | “At 5 after 9, I felt a pain and it sort of passed over (me). And then about 9:30 it started up again. It didn’t ease up”. |
| Forming a Symptom Pattern |
Recognizable as cardiac even if initially intermittent; symptoms unmistakable. |
“When the first one left (I thought) well ok, that was only one. Maybe it’s gone. When the second one came, 10 minutes (later), it was more intense. Your gut is already thinking that it was your heart. It wasn’t a question was it your heart.” “I knew the instant I got it. Because I had had it before.” “When I have pains, angina, from the heart, my whole arm aches all up and down to my hand. And when it’s just acid reflux I have pains in my chest, but mostly down here (pointing down). But up here is where I get concerned (demonstrating top part of chest).” |
| Using Others | Using others to validate their initial thoughts about symptoms |
“I don’t call him unless it’s really some pain. I said, my chest in hurting, really hurting. He wanted me to point out where I was hurting. I said somewhere in the chest area (but) it don’t much feel like a heart attack. But something is going on. I had suspicion of it being a heart attack.” “My husband and I sit down and talk about it.” |
| Preparing for Departure |
Taking time to finish a task or activity prior to departing for the emergency room |
“I knew after 5 or 10 minutes I needed to go. I just wanted to prolong it as long as I could. I had to do some things I had to do before I went.” “I had some personal things I wanted to do for myself. I’m funny about me. People are gonna be taking off my clothes and checking me.” “I can see the worriation on my husband’s face, of being scared to death. My feelings when I am going through this actually is more focused on my husband … It’s not really about me.” |
| Moving Toward Definitive Care |
Making decisions about when and where to seek medical care; never a question about if they needed to seek care. |
“It’s never a question of if I was going to the hospital but it’s which hospital and when. Because I know I’m gonna have to go.” “The only question was do I go ahead and call an ambulance. But I wanted my husband to be there. He told me to stay around people while I was waiting on him and we decided when he got there.” “My husband and I talk about it. He knows what to do. If I get to 3 nitroglycerins that means there is a serious problem. If it don’t calm down (I) get to the ER quick as I can, call 9-1-1. I did not want that to happen.(That’s) the reason why my husband and I decided we would go (to the hospital).” |
DISCUSSION
This study explored the thoughts and behaviors of women who experienced symptoms of ACS and the decision making process which preceded seeking care. One group of women had evolving symptoms, which led to ambivalence about the nature of the symptoms; and another group of women had symptoms that were readily identified as a serious cardiac problem needing medical attention but chose to delay seeking care as long as they could. Thus both groups of women initially delayed in seeking treatment, but for different reasons.
Differences in initial symptoms for women with ACS symptoms have been previously reported; first in early research by McSweeney35 and recently in work by O’Donnell and Moser33 and a Swedish study of elderly women with first time MI.37 Like the slow-onset MI group in research by O’Donnell and Moser, the women in the Evolving MI Group had symptoms that were initially vague and non-specific, which were often confused with symptoms of other health conditions. However, our findings highlight an explanation for why vague symptoms influence symptom interpretation. Consistent, prominent symptoms are needed in order to form a coherent symptom pattern prior to seeking care. Thus, symptom severity was only one part of forming a symptom pattern. This finding is consistent with work by Fukuoka and colleagues38 that found severity of chest pain was not a reliable cue to enable women to recognize their symptoms as cardiac.
Moreover, this study found that a prior frame of reference was helpful, but not sufficient, to form a symptom pattern, especially if at least one symptom feature differed. Even one factor that did not match prior experience prevented some women from forming a symptom pattern, halting the process of symptom interpretation to label the event life-threatening. These findings help explain why some women with past MIs do not equate symptoms of ischemia with a cardiac etiology and thus, delay seeking care more than those with a first time event. Prior studies have attributed this additional delay to inaccuracies in perceived vulnerability. However, our study suggests that symptoms with one event are not always identical to those in subsequent events. In contrast, women in the Immediately Recognizable MI Group were able to correctly label symptoms as cardiac even if their prior frame of reference did not match up perfectly. Thus the ability to form a symptom pattern may also vary among individuals; some women may have a higher tolerance for ambiguity in matching a prior frame of reference.
The findings also help explain why some women appear to dismiss evolving symptoms and continue with life as usual. In this study, some women returned to social obligations and role responsibilities because of a lack of understanding of their symptoms. Women who could not form a symptom pattern moved their attention away from symptoms to other aspects of their lives, and entered treatment later than needed. This finding differs from Rosenfeld’s work that found some women simply ignore their symptoms until the pain intensifies.22
The women in the Immediately Recognizable MI Group tended to overestimate the amount of time they had to safely engage in activities that they believed essential to complete prior to their departure. Based on past experience, they assumed that they could predict the amount of time they had to complete these tasks. These findings are consistent with prior research that indicates some women continue with daily responsibilities that are tightly linked to their personal integrity despite having correctly recognizing and interpreting their symptoms.26, 27,37
A strength of this study is that it provides personal in-depth accounts of women with ACS which help to explain how women recognize, interpret, and act on bodily cues. These findings may provide some explanation of why symptom education alone is not fully successful in getting women to quickly seek medical attention for ACS. The limitations of the study are its small sample and the potential for recall bias, since the women were interviewed up to 2 weeks after experiencing ACS symptoms.
Implications for Future Research
More systematic study of a larger sample is needed to compare thought processing and treatment-seeking patterns of groups differentiated based on their ability to recognize and interpret symptoms. The noticeability of symptoms may be enhanced, for example, by identifying factors that influence the ability to detect symptoms. Research is also needed to identify other factors that help with recognition of symptoms, such as somatic awareness or cue sensitivity, which may influence a woman’s ability to recognize a change in their body. For example, Miller39 found that cue sensitivity influenced the decisions of women with heart disease to attend to bodily cues. Furthermore, Riegel and colleagues40 found that as individuals aged their ability to detect and interpret symptoms (e.g. shortness of breath) declines. In addition, some women’s efforts to recognize a symptom pattern in our study were halted when one particular symptom feature did not match up exactly to past events. Thus, a better understanding of which person-related qualities influence tolerance for not having an exact match would also be helpful. These are areas of inquiry that need further study.
Conclusion
These findings suggest that these women delayed seeking care, regardless of their ability to correctly label their symptoms. Education aimed at symptom recognition and interpretation addresses only part of the problem. Women also should be educated about the potential danger of overestimating the time they have to seek medical attention. Furthermore, health care providers should emphasize that symptoms from one event may differ in subsequent episodes.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Go AS, Mozaffarian D, Roger VL, et al. on behalf of the American Heart Association Statistics Committee and Stroke Statistics Subcommittee Heart disease and stroke statistics – 2013 Update: a report from the American Heart Association. Circulation. 2013;127:e6–e245. doi: 10.1161/CIR.0b013e31828124ad. DOI: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wu JR, Moser DK, Riegel B, McKinley S, Doering LV. Impact of prehospital delay in treatment seeking on in-hospital complications after acute myocardial infarction. J Cardiovasc Nurs. 2011;26(3):184–93. doi: 10.1097/JCN.0b013e3181efea66. doi: 10.1097/JCN.0b013e3181efea66. [DOI] [PubMed] [Google Scholar]
- 3.Moser K, Kimble LP, Alberts MJ, et al. Reducing delay in seeking treatment by patients with acute coronary syndrome and stroke: A scientific statement from the American Heart Association Council on Cardiovascular Nursing and Stroke Council. Circulation. 2006;114:168–182. doi: 10.1161/CIRCULATIONAHA.106.176040. [DOI] [PubMed] [Google Scholar]
- 4.Rassmsen CH, Munck A, Kragstrup J, Haghfelt T. Patient delay from onset of chest pain suggesting acute coronary syndrome to hospital admission. Scandanavian Cardiovascular Journal. 2003;37:183–186. doi: 10.1080/14017430310014920. [DOI] [PubMed] [Google Scholar]
- 5.McGin AP, Rosamond WD, Goff DC, et al. Trends in prehospital time and use of emergency medical services for acute myocardial infarction: Experience in 4 US communities from 1987-2000. Am Heart J. 2005;150:392–400. doi: 10.1016/j.ahj.2005.03.064. [DOI] [PubMed] [Google Scholar]
- 6.Ting HH, Bradley EH, Wang Y, et al. Factors associated with longer time from symptom onset to hospital presentation for patients with ST-elevation myocardial infarction. Arch Intern Med. 2008;168(9):959–968. doi: 10.1001/archinte.168.9.959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McGin AP, Rosamond WD, Goff DC, et al. Trends in prehospital time and use of emergency medical services for acute myocardial infarction: Experience in 4 US communities from 1987-2000. Am Heart J. 2005;150:392–400. doi: 10.1016/j.ahj.2005.03.064. [DOI] [PubMed] [Google Scholar]
- 8.Gible WB, Armstrong PW, Ohman EM, et al. for the Global Use of Strategies to Open Occluded Coronary Arteries (GUSTO) Investigators Persistence of delays in presentation and treatment for patients with acute myocardial infarction: the GUSTO-I and GUSTO-III experience. Ann Emerg Med. 2002;39(2):123–130. doi: 10.1067/mem.2002.121402. [DOI] [PubMed] [Google Scholar]
- 9.Goldbg RJ, Steg PG, Sadiq I, et al. Extent of, and factors associated with, delay to hospital presentation in patients with acute coronary disease (The GRACE Registry) Am J Cardiol. 2002;89:791–796. doi: 10.1016/s0002-9149(02)02186-0. [DOI] [PubMed] [Google Scholar]
- 10.Sheif SE, Rathore SS, Gersh BJ, et al. Time to presentation with acute myocardial infarction in the elderly: associations with race, sex, and socioeconomic characteristics. Circulation. 2000;102(14):1651–6. doi: 10.1161/01.cir.102.14.1651. [DOI] [PubMed] [Google Scholar]
- 11.Goldbg RJ, Gurwitz JH, Gore JM. Duration of, and temporal trends (1994-1997) in, prehospital delay in patients with acute myocardial infarction: The second National Registry of Myocardial Infarction. Arch Intern Med. 1999;159(18):2141–2147. doi: 10.1001/archinte.159.18.2141. [DOI] [PubMed] [Google Scholar]
- 12.Ting HH, Bradley EH. Patient education to reduce prehospital delay time in acute coronary syndrome: Necessary but not sufficient. Circulation: Cardiovascular Quality and Outcomes. 2009;2:522–523. doi: 10.1161/CIRCOUTCOMES.109.912188. DOI: 10.1161/CIRCOUTCOMES.109.912188. [DOI] [PubMed] [Google Scholar]
- 13.Dracu K. The challenge of reducing prehospital delay in patients with acute coronary syndrome. Circulation: Cardiovascular Quality and Outcomes. 2009;2:144–145. doi: 10.1161/CIRCOUTCOMES.109.855635. DOI: 10.1161/CIRCOUTCOMES.109.855635. [DOI] [PubMed] [Google Scholar]
- 14.Sullin MD, Ciechanowski PS, Russo JE, Soine LA, Jordan-Keith K, Ting HH, et al. Understanding why patients delay seeking care for acute coronary syndromes. Circulation: Cardiovascular Quality and Outcomes. 2009;2:148–154. doi: 10.1161/CIRCOUTCOMES.108.825471. DOI: 10.1161/CIRCOUTCOMES.108.825471. [DOI] [PubMed] [Google Scholar]
- 15.Dracu K, McKinley S, Riegel B, Mieschke H, Doering LV, Moser D. KA nursing intervention to reduce prehospital delay in acute coronary syndrome: A randomized clinical trial. Journal of Cardiovascular Nursing. 2006;21(3):186–193. doi: 10.1097/00005082-200605000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Demps SJ, Dracup K, Moser DK. Women’s decision to seek care for symptoms of acute myocardial infarction. Heart Lung. 1995;24:444–56. doi: 10.1016/s0147-9563(95)80022-0. [DOI] [PubMed] [Google Scholar]
- 17.Canto G, Shlipak MG, Rogers WJ, et al. Prevalence, clinical characteristics, and mortality among patients with myocardial infarction presenting without chest pain. J Am Med Assoc. 2000;283(24):3223–3229. doi: 10.1001/jama.283.24.3223. [DOI] [PubMed] [Google Scholar]
- 18.Higgion RW. omen’s help-seeking behaviour at the onset of myocardial infarction. Br J Nurs. 2008;17(1):10–14. doi: 10.12968/bjon.2008.17.1.28054. [DOI] [PubMed] [Google Scholar]
- 19.Shinn Y, Martin R, Suls J. Meta-analytic evaluation of gender differences and symptom measurement strategies in acute coronary syndromes. Heart & Lung. 2010;39(4):283–295. doi: 10.1016/j.hrtlng.2009.10.010. [DOI] [PubMed] [Google Scholar]
- 20.Foste S, Mallik MA. comparative study of differences in the referral behavior patterns of men and women who have experienced cardiac-related chest pain. Intensive Crit Care Nurs. 1998;14(4):192–202. doi: 10.1016/s0964-3397(98)80525-9. [DOI] [PubMed] [Google Scholar]
- 21.Finnen JR, Meischke H, Zapka JG, et al. Patient delay in seeking care for heart attack symptoms: Findings from focus groups conducted in five U.Sregions. Prev Med. 2000;31:205–213. doi: 10.1006/pmed.2000.0702. [DOI] [PubMed] [Google Scholar]
- 22.Rosenld AG, Lindauer Al, Darney BG. Understanding treatment seeking delay in women with acute myocardial infarction: Descriptions of decision-making patterns. Am J Crit Care. 2005;14:285–293. [PubMed] [Google Scholar]
- 23.Thureon M, Jarlov MB, Lindahl B, Svensson L, Zedigh C, Herlitz J. Thoughts, actions, and factors associated with prehospital delay in patients with acute coronary syndrome. Heart Lung. 2007;36:398–409. doi: 10.1016/j.hrtlng.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 24.Harraon TL. Factors influencing delay in seeking treatment for acute ischemic symptoms among lower income, urban women. Heart Lung. 2007;36:96–104. doi: 10.1016/j.hrtlng.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 25.Moser K, McKinley S, Dracup K, Chung ML. Gender differences in reasons patients delay in seeking treatment for acute myocardial infarction symptoms. Patient Educ and Counseling. 2005;56:45–54. doi: 10.1016/j.pec.2003.11.011. [DOI] [PubMed] [Google Scholar]
- 26.Turri SA, Johnson JL. Maintaining integrity: Women and treatment seeking for the symptoms of potential cardiac illness. Qualitative Health Research. 2008;18(11):1461–1476. doi: 10.1177/1049732308325824. [DOI] [PubMed] [Google Scholar]
- 27.Turri SA. Finamore SReducing delay for women seeking treatment in the emergency department for symptoms of potential cardiac illness. J Emerg Nurs. 2008;34:509–515. doi: 10.1016/j.jen.2007.09.016. [DOI] [PubMed] [Google Scholar]
- 28.Alonz AA. The impact of the family and lay others on care-seeking during life-threatening episodes of suspected coronary artery disease. Soc Sci Med. 1986;22(12):1297–1311. doi: 10.1016/0277-9536(86)90093-6. [DOI] [PubMed] [Google Scholar]
- 29.Corbi J, Strauss A. Basics of qualitative research. 3rd edition Sage Publications; Thousand Oaks, CA: 2008. [Google Scholar]
- 30.Charm K. Constructing grounded theory: A practical guide through qualitative analysis. Sage; Thousand Oaks, CA: 2006. [Google Scholar]
- 31.Streurt HJ, Carpenter DR. Qualitative research in nursing. 5th edition Lippincott, Williams, & Wilkins; Philadelphia, PA: 2011. [Google Scholar]
- 32.Kvale S, Brinkmann S. Interviews: Learning the craft of qualitative research interviewing. 2nd edition Sage; Thousand Oaks, CA: 2009. [Google Scholar]
- 33.Sandewski M. Focus on qualitative methods Qualitative analysis: What it is and how to begin. Research in Nursing and Health. 1995;18:371–375. doi: 10.1002/nur.4770180411. [DOI] [PubMed] [Google Scholar]
- 34.Bloomrg LD, Volpe M. Completing your qualitative dissertation: A Roadmap from beginning to end. Sage; Thousand Oaks, CA: 2008. [Google Scholar]
- 35.McSwey JC. Women’s narratives: evolving symptoms of myocardial infarction. Journal of Women & Aging. 1998;10(2):67–77. doi: 10.1300/J074v10n02_06. [DOI] [PubMed] [Google Scholar]
- 36.O’Donll S, Moser DK. Slow-onset myocardial infarction and its influences on help-seeking behaviors. Journal of Cardiovascular Nursing. 2012;27(4):334–344. doi: 10.1097/JCN.0b013e31822071f3. [DOI] [PubMed] [Google Scholar]
- 37.Isaksn RM, Brulin D, Eliasson M, Naslund U, ZIngmark K. Older women’s prehospital experiences of their first myocardial infarction. Journal of Cardiovascular Nursing. 2013;28(4):360–369. doi: 10.1097/JCN.0b013e31824bcebc. Doi: 10.1097/JCN.0b013e31824bcebc. [DOI] [PubMed] [Google Scholar]
- 38.Fukuo Y, Dracup K, Moser DK, et al. Is severity of chest pain a cue for women and men to recognize acute myocardial infarction symptoms as cardiac in origin? Prog Cardiovasc Nurs. 2007;22:132–137. doi: 10.1111/j.0889-7204.2007.88859.x. [DOI] [PubMed] [Google Scholar]
- 39.Mille C. Cue sensitivity in women with cardiac disease. Progress in Cardiovascular Nursing. 2000;15(3):82–89. doi: 10.1111/j.1751-7117.2000.tb00210.x. [DOI] [PubMed] [Google Scholar]
- 40.Reige B, Dickson VV, Cameron J, Johnson JC, Bunker S, Page K, Worrall-Carter L. Symptom recognition in elders with heart failure. Journal of Nursing Scholarship. 2010;41(1):92–100. doi: 10.1111/j.1547-5069.2010.01333.x. [DOI] [PubMed] [Google Scholar]