Abstract
Web-based videoconferencing can improve access to substance abuse treatment by allowing patients to receive counseling services in their homes. This randomized clinical trial evaluates the feasibility and acceptability of web-based videoconferencing in community opioid treatment program (OTP) participants. Participants that reported computer and Internet access (n = 85) were randomly assigned to receive 12 weeks of weekly individual counseling in-person or via eGetgoing, a web-based videoconferencing platform. Fifty-nine of these participants completed the study (eGetgoing=24; In-person=35), with most study withdrawal occurring among eGetgoing participants. Participants exposed to the study conditions had similar rates of counseling attendance and drug-positive urinalysis results, and reported similar and strong ratings of treatment satisfaction and therapeutic alliance. These results support the feasibility and acceptability of web-based counseling as a good method to extend access to individual substance abuse counseling when compared to in-person counseling for patients that are able to maintain a computer and Internet connection for reliable communication.
Keywords: Web-based videoconferencing, substance abuse treatment, therapeutic alliance, methadone maintenance, treatment satisfaction
1.0 Introduction
Web-based technologies hold promising opportunities for improving access to a wide range of therapeutic and educational interventions (Cucciare et al., 2009; Godleski et al., 2012). There is a growing literature on the efficacy and effectiveness of web-based strategies for treating substance use disorders, most prominently tobacco and alcohol (Alcohol Research Group & Vernon, 2011; Chen et al., 2012). Most of these studies, however, have been descriptive in design, and few of the emerging web-based interventions have targeted individuals with persistent and severe opioid dependence disorder (Backhaus et al., 2012; Kiluk et al., 2011).
Opioid-agonist treatment programs (OTPs) appear to be good settings for incorporating the use of web-based interventions. There are well over 1,200 OTPs in the United States alone, serving more than 300,000 patients on any given day (SAMHSA, 2012). Opioid-dependent patients enrolled in OTPs often have additional substance use problems and other health concerns that require concurrent treatment services (Brooner et al., 1997), problems that could be addressed partly through web-based counseling services. In addition, opioid-agonist treatment is often a long-term intervention that can require years of treatment. The use of web-based interventions can improve the convenience of treatment for some patients and potentially increase retention across extended periods of time (Ball & Ross, 1991; McKay, 2005; McLellan et al., 2000; Steel et al., 2011).
Prior studies of web-based interventions for substance use problems have often evaluated computer-administered pre-programmed treatment and education modules rather than the delivery of “real time” counseling services (Alcohol Research Group & Vernon, 2011; Chen et al., 2012; Kiluk et al., 2011; Sinadinovic et al., 2012). Pre-packaged interventions may not be particularly compatible with the routine course of opioid dependence over extended periods of time, with symptoms that fluctuate in scope and severity (Ball & Ross, 1991; McKay, 2005; McLellan et al., 2000). In contrast, web-based videoconferencing platforms can be integrated within a continuum of services for stable patients and used to intensify treatment for symptomatic patients that require more intensive care (King et al., 2009). A meta-analysis by Spek et al. (2007) found that web-based interventions were better attended and more effective when accompanied by direct therapist involvement, findings that dovetail with other studies reporting strong associations between counseling attendance and improved substance abuse outcomes (King & Brooner, 2008; McLellan et al., 1993). Studies focusing on psychiatric and other clinical populations have reported at least comparable outcomes in web-based versus traditional in-person service delivery (Backhaus et al., 2012; Deen et al., 2012; Koch, 2012; Olden et al., 2010; Shore, 2013).
Very few published randomized trials have evaluated the effectiveness of web-based videoconferencing interventions, though several new studies are currently underway (e.g., Strachan et al., 2012; Thorp et al., 2012). In addition, available studies have not explored potential unintended negative effects of web-based delivery of routine counseling that might compromise acceptability in and transportability to community-based programs. These effects include the impact of web-based care on patient-therapist relationships, and technological obstacles that might interfere with the expected convenience of the intervention (e.g., Sucala et al., 2012; Thorp et al., 2012; Deen et al., 2013; Shore, 2013).
A small randomized and controlled trial conducted at our community-based OTP (King et al., 2009) yielded encouraging results on the feasibility and acceptability of eGetgoing™ (CRC Health Group, Inc.), a web-based videoconferencing substance abuse treatment service delivery platform that can deliver “real time” group counseling services. Participants submitting drug-positive urine specimens (n = 37) were assigned to a more intensive counseling schedule for 6 weeks that included 1-hour, twice-weekly cognitive-behavioral group therapy sessions. Participants received either eGetgoing web-based group counseling (n = 20) or routine on-site and in-person group counseling (n = 17). The results showed a trend such that eGetgoing participants attended a higher percent of scheduled group counseling sessions than those assigned to the control condition (eGetgoing: 92% vs. On-site: 76%, p = .07), though both conditions had similar rates of drug-positive urine tests (eGetgoing: 37% vs. On-site: 42%, p = ns). eGetgoing participants also reported a strong preference for web-based service delivery.
The present 12-week study builds on these findings by using a randomized and controlled design to evaluate the feasibility and acceptability of the eGetgoing videoconferencing platform to deliver individual counseling sessions routinely offered in OTPs. The eGetgoing condition was compared to a usual care condition that offered the same schedule of on-site and in-person individual counseling services. The primary outcomes were counseling attendance and treatment satisfaction, while secondary outcomes included rates of drug-positive urine samples and the quality of therapeutic alliance. In addition, the relative reinforcement value of the eGetgoing intervention was assessed using a novel Multiple Choice Procedure (Kidorf et al., 1995) to provide data on the potential for web-based videoconferencing formats to motivate changes in drug use or other treatment behaviors. Based on data from our first study (King et al., 2009), we expected the eGetgoing condition to be associated with higher rates of counseling utilization and greater treatment satisfaction.
2.0 Materials and methods
2.1 Participants
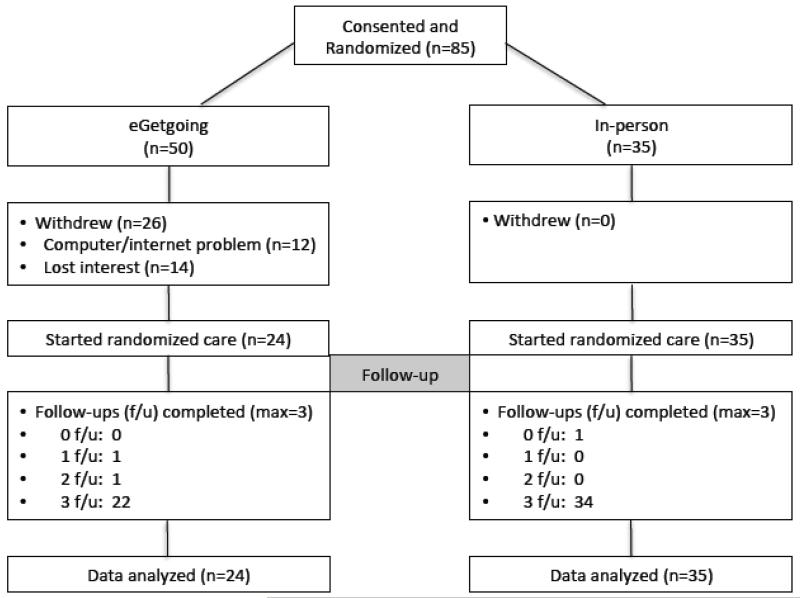
Eighty-five outpatients receiving opioid dependence treatment and comprehensive substance abuse care at Addiction Treatment Services at Johns Hopkins Bayview Medical Center (ATS) were enrolled in the study and randomized to study condition. Only 59 of these participants ultimately began randomized treatment and formed the study sample: 26 subjects withdrew from the eGetgoing condition due to problems with computer or Internet function (n = 12) or lost interest in the study (n = 14) prior to starting their randomized condition (see CONSORT diagram Figure 1). ATS had a mean census of approximately 475 patients at the time of the study. Patients were eligible for the study if they: 1) were drug abstinent and counseling adherent for the previous 30 days; 2) stated that they had a functioning computer with Internet connection; 3) were interested in receiving standard individual counseling via web-based videoconferencing and agreed to register with eGetgoing within 8 weeks of study enrollment; and 4) agreed to randomized assignment to study condition. We chose to target those with at least a short period of drug abstinence and counseling adherence because of their potential willingness to attend routine and intensified counseling schedules (in-person or via videoconferencing) over the short time frame of the study. These patients may also be more appreciative of videoconferencing formats because their abstinence affords more time towards work and family responsibilities and other recovery-oriented activities that might interfere with routine clinic counseling schedules. In addition, active drug users may be less likely to budget for non-essential household items such as computers with Internet connection.
Figure 1.
. CONSORT diagram.
Participants were recruited by use of IRB approved poster notices placed in conspicuous areas of the treatment clinic. In addition, research assistants reviewed counselor caseloads with clinical staff at least monthly to identify potentially eligible participants. Counseling and/or research staff members approached potential participants, informed them about the study, and scheduled appointments for those interested in study participation. Participants were enrolled from December 2009 to May 2012 and were followed for 12 weeks. All participants provided written informed consent to participate in the study, and the Johns Hopkins Institutional Review Board (IRB) approved the project.
2.2 Study design
After completing baseline assessments, participants were randomly assigned to one of two 12-week service delivery conditions: 1) standard in-person individual counseling delivery (In-person), or 2) web-based individual counseling delivery using the eGetgoing videoconferencing platform (eGetgoing). All other aspects of routine treatment in the clinic remained unchanged (see section 2.3). The only difference between study conditions was the availability of web-based videoconferencing for individual counseling delivery in the eGetgoing condition. Due to concern that those assigned to the eGetgoing condition might not have a working computer and Internet connection suitable for the study, the first 38 participants were randomized using a 2 (eGetgoing) to 1 (In-person) ratio to ensure an adequate numbers of participants starting the eGetgoing condition. The remaining 47 participants were randomized using a 1:1 ratio.
Fifty-seven participants received methadone maintenance treatment (M dose = 83 mg), one received buprenorphine/ naloxone maintenance, and one received naltrexone maintenance. Participants agreed to attend one weekly individual counseling session of 30 – 40 minutes duration as part of the study (and routine care) protocol. The primary counselor (BA or MA degree) provided the individual counseling and utilized supportive and problem-solving approaches (CSAT, 2005). Following the 12-week study, participants returned to treatment as usual (King & Brooner, 2008).
2.2.1 eGetgoing service delivery
Both the Joint Commission and the Commission on Accreditation of Rehabilitation Facilities (CARF) have accredited the eGetgoing web-based videoconferencing platform to deliver substance abuse treatment. The initial registration and computer set-up required access to a telephone as well as an Internet connection. Participants were also provided with a low-cost headset with microphone for their home computers to facilitate verbal communication between participant and provider. Participants assigned to this condition were required to contact an eGetgoing Information Technology (IT) technician to ensure that their computer had the required software, and to complete a structured tutorial given by the technician on navigating the eGetgoing platform. This process was often time consuming for participants with less computer experience, though the amount of preparation time to participate in a session went down over the course of the study. The participant’s assigned counselor also completed the same eGetgoing registration and online training procedures and continued to provide the individual counseling while the participant was in the study.
Each participant was assigned a unique log-on identification and password to ensure confidentiality. The IT technicians were notified of all scheduled counseling sessions and were available for technical support, if necessary. Participants were instructed to attend the session in a private setting, excluding family members, housemates, and friends. While sessions could be re-scheduled if participants or counselors were unable to attend the originally scheduled session, rescheduling was often logistically difficult due to the need to coordinate scheduling for the three different parties in a short period of time (participant, provider, e-Getgoing technician). In these situations, participants were offered the opportunity to meet with their counselor in the treatment clinic that week rather than miss the session.
There were higher rates of failed session attempts in the first half of the study, often due to problems with log-in names and passwords or audio communication. Counseling and research staff and eGetgoing IT staff became more adept at helping participants navigate the eGetgoing scheduling process and resolving technical issues in the latter half of the study, which improved the rate of completed web-based sessions.
2.2.2 Clinic-based in-person counseling
Participants assigned to this usual care service delivery condition were scheduled to attend one weekly 30 to 40 minute individual counseling session in the treatment program. The primary difference between the two study conditions was the setting used to deliver the counseling session (eGetgoing delivery vs. in-person usual care delivery).
2.3 Routine clinic care
ATS uses an adaptive stepped-care counseling model (Motivated Stepped Care- MSC) as routine care in which patients with partial and poor response to less intense counseling and monitoring schedules are systematically advanced to more intensive treatment schedules. Once the patient attends all scheduled counseling and submits drug negative urine specimens for a pre-determined period of time, the assigned counseling intensity is reduced (see Brooner et al., 2007 and King & Brooner, 2008 for a full description of the MSC model). Prior to study participation, all participants were required to meet with their individual counselor either weekly or monthly, depending on their response to treatment. However, all study participants agreed to attend one individual counseling session each week as part of the study protocol.
All participants submitted urine specimens for testing on a limited random schedule (Monday, Wednesday, Friday) with direct staff observation from an adjoining room (one-way mirror) to reduce submission of false or tampered specimens. Participants who had been drug-negative for at least 6 months prior to the study were permitted to leave one urine specimen per month; all other participants were required to leave weekly specimens. The alternative monthly urine collection schedule was used to avoid creating a disincentive to study participation in patients with longer periods of abstinence (i.e., avoid having to move from a monthly to a weekly urine collection schedule). No condition differences were observed for the percent of participants who were required to leave one urine specimen monthly versus weekly (monthly urine testing eGetgoing = 63% vs. In-person = 54%, χ2= 0.39, df = 1, p =0.531). Specimens were tested at an off-site certified clinical laboratory that uses an enzyme multiplied immunoassay technique (EMIT) to detect the presence of opioids, cocaine, benzodiazepines, amphetamine, and cannabis.
2.4 Study assessments
Participants completed baseline study assessments within the week prior to the 12-week randomized evaluation, and monthly assessments thereafter. The Client Satisfaction Questionnaire (CSQ; Larsen et al., 1979) is a self-administered 8-item questionnaire that uses a 4-point Likert scale rating to assess overall satisfaction with treatment across a number of dimensions. Items are averaged to yield a mean score (range 1-4; 4 is most satisfied). The Helping Alliance Questionnaire II (HAQ-II; Patient and therapist versions; Luborsky et al., 1996) is a 19-question self-administered instrument that measures the quality of the therapeutic alliance, and is completed separately by the patient and counselor. Each question is rated on a 6-point Likert scale, and items are averaged to yield a mean score (range 1-6; 6 is most satisfied).
Finally, a Multiple Choice Procedure (MCP) questionnaire (Kidorf et al., 1995) was administered to eGetgoing participants to evaluate the monetary value associated with eGetgoing counseling and two other routine treatment services offered in most OTPs (i.e., access to a methadone take-home dose; in-person counseling sessions). The MCP consists of three service versus service comparisons (e.g., eGetgoing counseling vs. methadone take-home dose; methadone take-home vs. in-person counseling; eGetgoing counseling vs. in-person counseling), and 50 service versus money combinations (e.g., eGetgoing counseling vs. $1.00; eGetgoing counseling vs. $2.00, etc.). The maximum monetary value was $50.00, using increments of $1.00. This assessment measured the monetary value assigned by participants to each service, and provided an approximate monetary and reinforcement value of eGetgoing counseling, though participants did not receive any money based on their preferences. Participants were paid $30 for completing baseline assessments, $10 for each follow-up assessment at 1- and 2-months, and $15 for the 3-month follow-up (approximately $10 per hour).
2.5 Data analyses
A power analysis (alpha = .05, power = .80), using data from our previous study (King et al., 2009), indicated that 90 participants were required to detect condition differences on the primary outcomes of counseling attendance and treatment satisfaction. The study was ultimately under powered (n = 59) in part due to 26 participants withdrawing from the eGetgoing condition. Secondary outcomes included drug-positive urine samples and therapeutic alliance. T-tests and chi-square tests were used to compare study conditions on baseline demographic and drug use variables. T-tests were used to compare conditions on the mean number of counseling sessions attended and the mean percent of any drug-positive urine specimens submitted over the 12-week study period. Mixed models analyses were used to evaluate condition differences in follow-up CSQ and HAQ-II (therapist and patient versions) scores; we did not hypothesize or test within-subjects or interaction effects. Descriptive analyses were used to evaluate Multiple Choice Procedure values for eGetgoing participants.
3.0 Results
3.1 Participants
A substantial number of participants assigned to the eGetgoing condition (n = 26) failed to complete the required registration procedure with the eGetgoing Information Technology (IT) technician and withdrew from the study. Some of these participants lost interest in the study and did not attempt the registration procedure (n =14), while others reported problems with computer or Internet function during registration (n = 12). The 59 remaining participants (eGetgoing n = 24, In-person n = 35) were compared to those withdrawn from the study on demographic variables (age, gender, marital status, education, race, full time employment status) and relevant baseline treatment variables (number of weekly methadone take home doses, length of treatment episode prior to study consent); no significant differences were observed.
No significant condition differences were observed for any of the baseline demographic or treatment variables (see Table 1). The mean age of participants (n=59) was 41 years, 56% were female, 36% self-identified as a racial minority, 32% were married, mean education was 12 years, and 46% reported verified full-time employment. Job classifications for employed participants included: 17% in management, 14% in administration, 34% in service, 28% in construction, and 7% in transportation. Participants had responded well to treatment in the 12 weeks prior to the study: urine testing revealed an average of 6% drug-positive urine samples during that time with no significant difference between study conditions. Most participants submitted urine specimens on a monthly versus weekly schedule and received on average about 4 methadone take home doses each week. Mean length of treatment prior to study consent was several years for each condition.
Table 1.
Baseline Characteristics of Study Participants (n = 59)
| Variable | eGetgoing (n=24) |
In-person (n=35) |
p |
|---|---|---|---|
| M (SD) or % | M (SD) or % | ||
| Demographics | |||
| Female (%) | 54.2 | 57.1 | ns |
| Married (%) | 33.3 | 31.4 | ns |
| Age (yrs) | 40.5 (11.15) | 41.1 (10.50) | ns |
| Education (yrs) | 12.3 (2.39) | 11.9 (1.85) | ns |
| Minority (%) | 25.0 | 42.9 | ns |
| Full time employed (%) | 58.3 | 37.1 | ns |
| Treatment variables in 3 months prior to study consent | |||
| Urine tests positive for drug use (%) | 7.3 | 5.7 | ns |
| Submit monthly vs. weekly urine screens (%) | 62.5 | 54.3 | ns |
| Length of treatment prior to consent (days) | 2052 (1926) | 1242 (1555) | 0.080 |
| Number weekly methadone take-home doses | 4.3 (2.48) | 3.5 (1.74) | ns |
3.2 Counseling attendance
Over the 12-week study, eGetgoing participants (n=24) attended a mean of 5.4 (SD=2.54) eGetgoing counseling sessions; In-person participants (n=35) attended a mean of 6.1 (SD=3.30) counseling sessions (t = 0.91, df = 57, p = 0.367). However, 50% of eGetgoing participants attended at least one additional in-person counseling session due to problems with eGetgoing session scheduling. This often occurred due to last minute scheduling changes that precluded rescheduling the videoconferencing session that week, but sometimes occurred when technical difficulties prevented an eGetgoing session from occurring. Nevertheless, rates of overall counseling attendance for eGetgoing and In-person participants remained similar (eGetgoing: M = 7.3 (SD=2.49) sessions vs. In-person: M = 6.1 (SD=3.30) sessions; t = 1.39, df = 57, p = 0.169). Only one participant reported difficulty finding a private space in his home for conducting the videoconferencing sessions in some study weeks.
3.3 Urinalysis testing
As expected, participants in both conditions had low rates of drug-positive urinalysis results across the 12-week study period, with no between-group differences (eGetgoing (n=24): M = 11% (SD=0.27) vs. In-person (n=35): M = 9% (SD=0.16), t = .22, df = 57, p = 0.831).
3.4 Overall treatment satisfaction
Satisfaction was high in both conditions. Mean CSQ scores were high at both baseline (eGetgoing (n=24): M = 3.7 (SD=0.44) vs. In-person (n=35): M = 3.7 (SD=0.36)) and study end point (eGetgoing (n=22): M = 3.8 (SD=0.31) vs. In-person (n=34): M = 3.6 (SD=0.52)), and no condition effects were observed (F (1, 56) = 1.63, p = 0.207) for CSQ ratings for the 12-week follow-up period. Anecdotally, while some eGetgoing participants complained about technical problems when they occurred, most enjoyed the convenience of the service and the novelty of the experience.
3.5 Therapeutic alliance
No condition effects were observed for patient ratings of the therapeutic alliance (F (1, 56) = 0.01, p = 0.912). Mean patient-rated therapeutic alliance scores were very high at both baseline (eGetgoing (n=24): M = 5.2 (SD=0.68) vs. In-person (n=35): M = 5.4 (SD=0.52)) and study end point (eGetgoing (n=22): M = 5.4 (SD=0.70) vs. In-person (n=32): M = 5.4 (SD=0.48)). No condition effects (F (1, 56) = .47, p = 0.497) were observed for therapist ratings of the therapeutic alliance over the 12-week follow-up period. Mean therapist-rated therapeutic alliance scores were high at both baseline (eGetgoing (n=24): M = 5.1 (SD=0.49) vs. In-person (n=35): M = 5.0 (SD=0.40)) and study end point (eGetgoing (n=20): M = 5.2 (SD=0.50) vs. In-person (n=31): M = 5.1 (SD=0.40)).
3.6 Multiple Choice Procedure (MCP)
Descriptive analyses suggested a decrease in the percent of eGetgoing patients preferring web-based counseling to in-person counseling from baseline (91%) to week 12 (75%). The estimated value of an eGetgoing counseling session remained fairly stable from baseline (M = $16.77) to week 12 (M = $17.50), while the estimated value of an in-person counseling session appeared to increase from baseline (M = $8.77) to week 12 (M = $14.75). As a comparison, the mean MCP value of a take home dose of methadone was stable and relatively higher at baseline (M = $25.68) and week 12 (M = $26.75).
4.0 Discussion
The present study is the first known randomized and controlled trial evaluating web-based videoconferencing technology as a platform to provide individual counseling sessions in an OTP setting. Rates of counseling attendance were both good and comparable across service delivery conditions, contrary to our hypothesis and diverging from our first eGetgoing therapy study that found higher levels of group counseling utilization in eGetgoing versus in-person counseling conditions (King et al., 2009). These studies evaluated two different clinical situations. Participants in the first study were referred to more intensive substance abuse counseling due to illicit drug use, with clinic-based incentives used to motivate adherence in both conditions. In this context, more convenient access to treatment may have combined with behavioral reinforcement to motivate higher rates of attendance. The present sample was considerably more stable and required less intense levels of baseline treatment services; participants in both conditions were satisfied with attending approximately two counseling sessions each month and access to videoconferencing did not significantly affect the rates of counseling attendance.
That measures of overall treatment satisfaction (CSQ) remained high and not significantly different across both treatment conditions may be due to a ceiling effect; both conditions reported high satisfaction with treatment at baseline. In addition, the CSQ evaluates the overall treatment experience, not just satisfaction with videoconferencing. While participants’ initial enthusiasm for the eGetgoing technology moderated somewhat over the 12-week study period, three quarters of participants starting the eGetgoing condition ultimately favored access to this service delivery condition over routine in-person counseling by the end of the study. It should be noted that this favorable rating does not account for those withdrawing from the eGetgoing condition prior to experiencing the videoconferencing platform. Yet these findings are consistent with results from several studies showing that videoconferencing technology is well tolerated by patients receiving care in many areas of medicine and psychology, with outcomes comparable to usual care interventions (Koch, 2012; Olden at al., 2010; Steel et al., 2011).
The secondary outcomes of drug-positive urinalysis results and measures of therapeutic alliance were also good and comparable across service delivery conditions. Counselors and participants rated the strength of the therapeutic alliance as high in both the eGetgoing and routine in-person conditions, a finding that dovetails with studies from other clinical areas showing that web-based interventions are associated with therapeutic interaction ratings that compare favorably to usual care interventions (Knaevelsrud & Maercker, 2007; Marziali et al., 2005; Sucala et al., 2012; Thorp et al., 2012). It should be noted that participants had a pre-existing counseling relationship established prior to study participation, which diverges from previous study designs (Knaevelsrud & Maercker, 2007; Spek et al., 2007; Thorp et al., 2012) and may have biased ratings of satisfaction and therapeutic alliance. Exclusive use of videoconferencing over longer periods of time might be experienced differently than in the present study. And, due to a variety of practical implementation issues, about half of those assigned to eGetgoing had at least one in-person session during the trial. Nevertheless, the strength of the therapeutic alliance did not deteriorate over the course of the study, supporting the view that this form of service delivery can be very acceptable in an OTP setting.
Results from the Multiple Choice Procedure showed that eGetgoing participants reported a preference for access to web-based counseling, and rated eGetgoing sessions ($17.50) as somewhat more valuable than usual care in-person sessions ($14.75). Neither means of counseling delivery was valued as highly as a methadone take home dose ($26.75). While both methadone take-homes and web-based videoconferencing might be conceptualized as clinic-based privileges that can reduce the considerable time demands of methadone treatment for patients that have achieved clinical stability, these data suggest that methadone take-homes have greater clinic-wide potential for prospectively reinforcing behavior change in drug use or other treatment behaviors. It remains possible that access to videoconferencing platforms may have greater reinforcement potential for those with busy work schedules or other time constraints, though the present study did not evaluate this hypothesis.
Perhaps the biggest challenge associated with the eGetgoing platform was adapting to the new technology. Participants were required to possess a reliable, updated computer with an Internet connection, and to register for the eGetgoing videoconferencing service. Initially, participants often experienced problems connecting to the eGetgoing platform, especially with the log-ins and passwords. Some counselors and participants had problems with the audio portion of the transmission and spent time in their sessions on the telephone and computer. The sources of these problems were manifold: participant inexperience with this technology, hardware and software problems, and negotiating the eGetgoing interface through the hospital computer security software. This platform was more convenient for attending sessions that were planned in advance, and much less so for attending sessions scheduled within short notice (1-2 days). As participants and counselors grew more comfortable with the technology, access to the eGetgoing platform considerably improved by the second half of the study. These problems are likely unavoidable when participants are responsible for their own computer equipment and Internet access. In fact, most studies on videoconferencing for psychotherapy or psychiatric evaluations have used dedicated videoconferencing equipment supplied by the clinics at two distant sites and did not rely on patients to supply their own equipment (Backhaus et al., 2012; Deen et al., 2012) or even supplied computers and Internet service to study participants (Marziali et al., 2005). In retrospect, it might have helped to offer on-site registration and tutorials to facilitate participant comfort with the technology in the clinic prior to using the technology at home. Other concerns, such as finding a private space to conduct the videoconferencing sessions at home, also interfered with the use of the technology at times.
Perhaps the biggest study limitation was the select sample. Only participants that had demonstrated clinical stability were recruited for the study. It is quite possible that individuals with higher rates of current drug use may have responded differently to the intervention, though our previous study using the eGetgoing platform to intensify treatment for those using illicit drugs yielded similar results (King et al, 2009). That the study was conducted during a severe economic recession when many clinic patients lost their jobs and could not afford upkeep on a computer and Internet connection may have further restricted the study sample.
In addition, a considerable number of individuals assigned to the eGetgoing condition withdrew prior to starting randomized care, thereby reducing statistical power to detect condition differences. While study withdrawal may have indicated a discrepancy between stated interest in using and accessing this technology, it seems possible that many of these participants may have remained in the study if they had the proper hardware and Internet access. Baseline demographic and treatment variables were similar for those participating in and those withdrawing from the study, though other factors not formally assessed may have differentiated these subgroups. Nevertheless, the primary outcomes supported previous work demonstrating comparability of web-based and in-person delivery platforms (Backhaus et al., 2012).
Taken together, these results make an important contribution to the field by studying a clinical population of opioid-dependent outpatients that had limited previous exposure to computerized or web-based interventions. The web-based and in-person conditions enjoyed similar rates of counseling adherence and drug-positive urine samples, with good continuing treatment satisfaction and strong therapeutic relationships without evidence of deterioration during the length of the study. Future research might target a more varied treatment population (e.g., those with more current substance use) across different phases of recovery. Evaluating alternative videoconferencing platforms that require fewer steps to prepare for transmission may be helpful for those interested in videoconferencing but reluctant to use a multi-step registration process. The findings suggest that web-based videoconferencing platforms in OTPs appear to be most optimally used to extend access to counseling for those who prefer the convenience of this technology and can maintain an adequate computer and Internet access for reliable communication.
Acknowledgments
This study was supported by Challenge grant NIH 1RC1DA028189 from the National Institute on Drug Abuse (PI: Van L. King, MD). We also thank Kori Kindbom, Rachel Burns, Michael Sklar and others who work in the Clinical Research Assessment Unit for their outstanding assistance in the conduct of this study. We also thank the ATS clinical staff and patients who agreed to participate in this study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Alcohol Research Group. Vernon ML. A review of computer-based alcohol problem services designed for the general public. J Subst Abuse Treat. 2011;38(3):203–211. doi: 10.1016/j.jsat.2009.11.001. PMID: 20015607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Backhaus A, Agha Z, Maglione ML, Repp A, Ross B, Zuest D, Rice-Thorp NM, Lohr J, Thorp SR. Videoconferencing psychotherapy: a systematic review. Psychological Services. 2012;9(2):111–131. doi: 10.1037/a0027924. [DOI] [PubMed] [Google Scholar]
- Ball JC, Ross A. The effectiveness of methadone maintenance treatment. Springer- Verlag; New York: 1991. [Google Scholar]
- Brooner RK, King VL, Kidorf MS, Schmidt CW, Bigelow GE. Psychiatric and substance use comorbidity among treatment-seeking opioid abusers. Archives of General Psychiatry. 1997;54:71–80. doi: 10.1001/archpsyc.1997.01830130077015. [DOI] [PubMed] [Google Scholar]
- Center for Substance Abuse Treatment . Medication-Assisted Treatment for Opioid Addiction in Opioid Treatment Programs. TIP Series 43. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2005. DHHS Publication no. (SMA) 05-4048. [PubMed] [Google Scholar]
- Chen YF, Madan J, Welton N, Yahaya I, Bauld L, Wang D, Fry-Smith A, Munafo MR. Effectiveness and cost-effectiveness of computer and other electronic aids for smoking cessation: a systematic review and network meta-analysis. Health Technol Assess. 2012;16(38):1–125. doi: 10.3310/hta16380. PMID: 23046909. [DOI] [PubMed] [Google Scholar]
- Cucciare MA, Weingardt KR, Humphreys K. How Internet technology can improve the quality of care for substance use disorders. Curr Drug Abuse Rev. 2009;2(3):256–62. doi: 10.2174/1874473710902030256. [DOI] [PubMed] [Google Scholar]
- Deen TL, Fortney JC, Schroeder G. Patient acceptance of and initiation and engagement in telepsychotherapy in primary care. Psychiatric Services. 2013 doi: 10.1176/appi.ps.201200198. In Advance, Feb. 1, 2013; doi:10.1176/appi.ps.201200198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deen TL, Godleski L, Fortney JC. A description of telemental health services provided by the Veterans Health Administration in 2006-2010. Psychiatric Services. 2012 doi: 10.1176/appi.ps.201100458. doi: 10.1176/appi.201100458. [DOI] [PubMed] [Google Scholar]
- Germain V, Marchand A, Bouchard S, Guay S, Drouin MS. Assessment of the therapeutic alliance in face-to-face or videoconference treatment for posttraumatic stress disorder. Cyberpsychol Behav Soc Netw. 2010;13(1):29–35. doi: 10.1089/cyber.2009.0139. PMID: 20528290. [DOI] [PubMed] [Google Scholar]
- Godleski L, Darkins A, Peters J. Outcomes of 98,609 U.S. Department of Veterans Affairs patients enrolled in Telemental Health services, 2006-2010. Psychiatric Services. 2012;63(4):383–385. doi: 10.1176/appi.ps.201100206. [DOI] [PubMed] [Google Scholar]
- Kidorf M, Stitzer ML, Griffiths RR. Evaluating the reinforcement value of clinic-based privileges through a multiple choice procedure. Drug Alcohol Depend. 1995;39:167–172. doi: 10.1016/0376-8716(95)01136-7. PMID: 8556964. [DOI] [PubMed] [Google Scholar]
- Kiluk BD, Sugarman DE, Nich C, Gibbons CJ, Martino S, Rounsaville BJ, Carroll KM. A methodological analysis of randomized clinical trials of computer-assisted therapies for psychiatric disorders: toward improved standards for an emerging field. Am J Psychiatry. 2011;168:790–799. doi: 10.1176/appi.ajp.2011.10101443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King VL, Brooner RK. Improving treatment engagement in opioid-dependent outpatients with a motivated stepped-care adaptive treatment model. Joint Comm J Qual Patient Saf. 2008;34:209–213. doi: 10.1016/s1553-7250(08)34027-6. PMID: 18468359. [DOI] [PubMed] [Google Scholar]
- King VL, Stoller KB, Kidorf M, Kindbom K, Hursh S, Brady T, Brooner RK. Assessing the effectiveness of an Internet-based videoconferencing platform for delivering intensified substance abuse counseling. J Subst Abuse Treat. 2009;36:331–338. doi: 10.1016/j.jsat.2008.06.011. PMID: 18775625. [DOI] [PubMed] [Google Scholar]
- Knaevelsrud C, Maercker A. Internet-based treatment for PTSD reduces distress and facilitates the development of a strong therapeutic alliance: a randomized controlled clinical trial. BMC Psychiatry. 2007;7:13. doi: 10.1186/1471-244X-7-13. doi:10.1186/1471-244X-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koch EF. The VA Maryland health care system’s Telemental Health Program. Psychological Services. 2012;9(2):203–205. doi: 10.1037/a0026144. [DOI] [PubMed] [Google Scholar]
- Larsen DL, Attkisson CC, Hargreaves WA, Nguyen TD. Assessment of client/patient satisfaction: development of a general scale. Eval Program Plann. 1979;2:197–207. doi: 10.1016/0149-7189(79)90094-6. PMID: 10245370. [DOI] [PubMed] [Google Scholar]
- Luborsky L, Barber JP, Siqueland L, Najavits LM, Frank A, Daley D. The revised Helping Alliance Questionnaire (HAq-II): psychometric properties. J Psychother Practice Research. 1996;5(3):260–271. http://jppr.psychiatryonline.org/cgi/content/abstract/5/3/260. [PMC free article] [PubMed] [Google Scholar]
- Marziali E, Donahue P, Crossin G. Caring for others: Internet health care support intervention for family caregivers of persons with Alzheimer’s, stroke, or Parkinson’s Disease. Families in Society. 2005;86:375–383. [Google Scholar]
- McKay JR. Is there a case for extended interventions for alcohol and drug use disorders? Addiction. 2005;100:1594–1610. doi: 10.1111/j.1360-0443.2005.01208.x. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Arndt IO, Metzger DS, Woody GE, O’Brien CP. The effect of psychosocial services in substance abuse treatment. JAMA. 1993;269:1953–1959. [PubMed] [Google Scholar]
- McLellan AT, Lewis DC, O’Brien CP, Kleber HD. Drug dependence, a chronic medical illness: Implications for treatment, insurance, and outcomes evaluation. JAMA. 2000;284:1689–1695. doi: 10.1001/jama.284.13.1689. PMID: 11015800. [DOI] [PubMed] [Google Scholar]
- Olden M, Cukor J, Rizzo A, Rothbaum B, Difede J. House calls revisited: leveraging technology to overcome obstacles to veteran psychiatric care and improve treatment outcomes. Ann N Y Acad Sci. 2010;1208:133–141. doi: 10.1111/j.1749-6632.2010.05756.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shore JH. Telepsychiatry: videoconferencing in the delivery of psychiatric care. Am J Psychiatry. 2013;170:256–262. doi: 10.1176/appi.ajp.2012.12081064. [DOI] [PubMed] [Google Scholar]
- Sinadinovic K, Wennberg P, Berman AH. Targeting problematic users of illicit drugs with Internet-based screening and brief intervention: a randomized controlled trial. Drug Alcohol Dependence. 2012;126:42–50. doi: 10.1016/j.drugalcdep.2012.04.016. [DOI] [PubMed] [Google Scholar]
- Spek V, Cuijpers P, Nyklicek I, Riper H, et al. Internet-based cognitive behaviour therapy for symptoms of depression and anxiety: a meta-analysis. Psychol Med. 2007;37:319–328. doi: 10.1017/S0033291706008944. PMID: 17112400. [DOI] [PubMed] [Google Scholar]
- Steel K, Cox D, Garry H. Therapeutic videoconferencing interventions for the treatment of long-term conditions. J Telemed Telecare. 2011;17(3):109–117. doi: 10.1258/jtt.2010.100318. [DOI] [PubMed] [Google Scholar]
- Strachan M, Gros DF, Yuen E, Ruggerio KJ, Foa EB, Acierno R. Home-based telehealth to deliver evidence-based psychotherapy in veterans with PTSD. Contemporary Clinical Trials. 2012;33:402–409. doi: 10.1016/j.cct.2011.11.007. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration . National Survey of Substance Abuse Treatment Services (N-SSATS): 2011. Data on Substance Abuse Treatment Facilities. BHSIS Series S-64. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2012. HHS Publication No. (SMA) 12-4730. [Google Scholar]
- Sucala M, Schnur JB, Constantino MJ, Miller SJ, Brackman EH, Montgomery GH. The therapeutic relationship in E-therapy for mental health: a systematic review. J Medical Internet Research. 2012;14(4):e110. doi: 10.2196/jmir.2084. PMCID: PMC3411180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorp SR, Fidler J, Moreno L, Floto E, Agha Z. Lessons learned from studies of psychotherapy for posttraumatic stress disorder via video teleconferencing. Psychological Services. 2012;9(2):197–199. doi: 10.1037/a0027057. [DOI] [PubMed] [Google Scholar]