Abstract
Background:
C-reactive protein (CRP) and white blood cell (WBC) are proinflammatory markers. They are major pathophysiological for the development of metabolic syndrome (MetS). This study aimed to address the independent associations between MetS and WBC counts and serum CRP levels and evaluation of their magnitude in relation to the MetS, based on the sex in the Iranian adults.
Materials and Methods:
In this cross-sectional study, subjects who met the MetS criteria, based on the Adult Treatment Panel III were selected from the Isfahan Healthy Heart Program database. A questionnaire containing the demographic data, weight, height, waist, and hip circumference of the respondents was completed for each person. Blood pressure was measured and the anthropometric measurements were done, and fasting blood samples were taken for 2 h postload plasma glucose (2 hpp). Serum [total, high-density lipoprotein (HDL), and low-density lipoprotein] levels of cholesterol, triglyceride, and CRP as well as WBC counts were determined. The univariate analyses were carried out to assess the relation between the CRP levels, WBC counts with the MetS in both sexes the.
Results:
In men with the abdominal obesity, the higher levels of WBC count, high serum triglyceride and blood glucose levels, a low serum HDL level, and raised systolic and diastolic blood pressure were observed. However, the higher serum CRP levels were only observed in those with the low serum HDL-cholesterol levels. The mean values of the WBC counts were statistically different between the men with and without MetS, but the mean values of the CRP levels were similar between the two groups. In women, the mean values of WBC count and CRP levels were statistically different in the subjects with and without a MetS components (except for the low serum HDL levels and high diastolic blood pressure for the WBC measures and abdominal obesity for the CRP measures) and for those with and without MetS. The age and smoking adjusted changes in the CRP levels and WBC counts correlated with the number of Mets components in the women.
Conclusion:
The findings of this study suggest substantial implications for the prevention and management of the MetS and atherosclerotic diseases, as these involve the suppression of inflammatory conditions rather than the incitement of anti-inflammatory conditions.
Keywords: C-reactive protein level, metabolic syndrome, white blood cell count
INTRODUCTION
Metabolic syndrome (MetS) is conceptualized as a clustering of risk factors, including insulin resistance, dyslipidemia, central adiposity, and high blood pressure that increase the risk of cardiovascular disease and type 2 diabetes mellitus. The combination of these findings defines the MetS.[1,2] There is global agreement that this risk factors gathering increase the risk of cardiovascular disease, and metabolic diseases, such as diabetes and thus has made it a serious public health problem.[3] In fact, numerous studies have shown people with the MetS are more likely to die prematurely and that they are at the greater risk of developing diabetes mellitus and cardiovascular disease.[4,5]
Inflammation is a major pathophysiological factor for the MetS development. Some evidences are available concerning the association between the appearance of MetS and chronic inflammatory response, characterized by the abnormal cytokine production and the activations of inflammatory signaling pathways.[6,7] Furthermore, some inflammatory biomarkers, such as C-reactive protein (CRP) and interleukin-6 are in associated with the MetS and its components in different settings.[6,7,8,9,10,11,12,13] Moreover, there is a proven association between the increased white blood cell (WBC) count as a biological marker of systemic and the components of the MetS.[14,15]
Nevertheless, there are few studies examining sex-based associations between the CRP level and WBC count as pro-inflammatory markers and the MetS, especially in our population. Indeed, other published findings achieved from small size populations. Therefore, this study aimed to investigate the independent associations between the MetS and WBC count and serum CRP levels in both sexes and evaluation of their magnitude in relation to the MetS in the Iranian adults.
MATERIALS AND METHODS
Study population
The Isfahan Healthy Heart Program is a comprehensive integrated community-based action-oriented study with a reference community has been conducted by the Isfahan Cardiovascular Research Institute since 2000 and completed in 2007 in Isfahan.[16,17] A random independent sample of adults was selected by the multistage cluster sampling. The effect of confounding was addressed by using the random, stratified household sampling, based on age and sex groups. The participants were more than 19 years old. Finally, 4719 subjects with MetS entered in our study. The samples underwent a 30-min interview by well-trained examiners to complete the validated questionnaires containing questions on demography, socioeconomic status, smoking behavior, physical activity, nutritional habits, and other risk profiles. Informed consent was obtained from all subjects prior to their participation in this study. This study was approved by the Ethical Committee of the Isfahan University of Medical Sciences. Isfahan Healthy Heart Program (IHHP) was covered under the institutional review board protocol FW A00008578.
Data collection
Information on the sociodemographic factors and self-reported medical history were obtained by interview. Anthropometric measurements, including height, weight, and waist and hip circumferences were taken with the subjects wearing light clothing by well-trained examiners. Waist circumference was measured to the nearest 0.1 cm in the horizontal plane at the high point of the iliac crest during minimal respiration.[17] Blood pressure was measured with a mercury sphygmomanometer using right arms, in a sitting position, after a 5-min rest. Systolic and diastolic blood pressures were recorded twice and the averages were used for the data analysis. Blood samples were drawn from anantecubital vein after an 8-12 h overnight fast. Samples were stored at −20°C until required for the biochemical assays. Fasting venous blood samples were obtained from the antecubital vein between 08:00 and 09:30 am. Blood samples were centrifuged for 10 min at 906 g within 30 min of collection. Sera were analyzed for the total cholesterol (TC), high-density lipoprotein (HDL), triglycerides (TG), and fasting blood glucose (FBG). Low-density lipoprotein-cholesterol (LDL) was calculated by Friedwald equation when TG was less than 400 mg/dL.[18] TC was measured using enzymatic colorimetric methods. HDL-C was determined after dextran sulphate-magnesium chloride precipitation of HDL. The serum CRP levels were measured with the same autoanalyzer. The assay (Pars Azmoun) had a limit of detection 0.05 mg/L and an upper limit of 160 mg/L. WBC count was determined using the sysmex.[16,17] All the tests were performed in the Central Laboratory of the Isfahan Cardiovascular Research Center using the autoanalyzer ELAN (Ependorf 2000). For quality-control measures, this laboratory meets the criteria of the national standard laboratory (a WHO collaborating centre in Tehran).
MetS definition
The ATPIII definition of MetS was met when three or more of the following criteria were present: Waist circumference ≥102 in cm the men and 88 cm in the women; HDL ≤40 mg/dL in the men and 50 mg/dL in the women or specific treatment for this lipid abnormality; TG ≥150 mg/dL or specific treatment for this lipid abnormality; systolic blood pressure ≥130 mm Hg or diastolic blood pressure ≥85 mm Hg or treatment of previously diagnosed hypertension; and fasting glucose ≥100 mg/dL.[14]
Statistical analyses
Results were reported as mean ± standard deviation for the quantitative variables and percentages for the categorical variables. The groups were compared using the t-test for the continuous variables and the Chi-square test for the categorical variables. P values of 0.05 or less were considered significant. All the statistical analyses were performed using SPSS version 16.0 (SPSS Inc., Chicago, IL, USA) for Windows.
The associations between the serum CRP levels and WBC count with the MetS components were examined with the logistic regression analysis. The significance level was set at P > 0.05.
RESULTS
The personal and clinical characteristics of the study subjects are presented in Table 1. Systolic and diastolic blood pressures were significantly higher in the men than in the women. Serum CRP and blood sugar levels were similar between the two genders. Levels of triglyceride and WBC counts were higher in the men compared with the women. Conversely, LDL cholesterol levels were higher in the women. Totally, the overall prevalence of the MetS was significantly higher in the women.
Table 1.
Demographic and clinical characteristics of the study subjects by sex
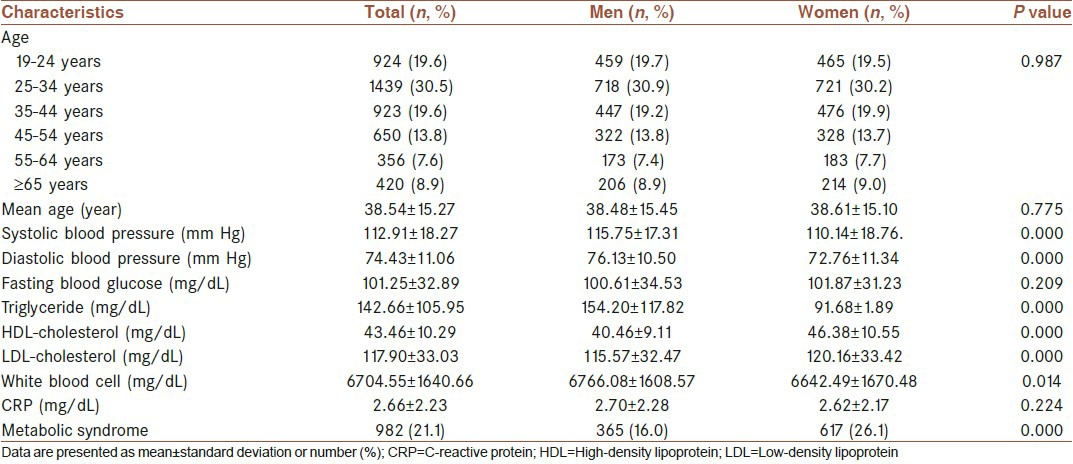
Table 2 shows the mean values of CRP levels and WBC counts, based on the presence and absence of each MetS components and according to the presence and absence of MetS in the men. In men, with the abdominal obesity a significantly higher level of WBC counts, high serum triglyceride and blood glucose levels and, low HDL-cholesterol levels, and raised systolic and diastolic blood pressures were observed. However, significantly higher serum CRP levels were only observed in those with the low HDL-cholesterol levels. The mean values of WBC counts were statistically different between the men with and without the MetS, but the mean values of CRP levels were similar between the two groups.
Table 2.
Metabolic syndrome components and mean value of white blood cell and C-reactive protein in both sexes
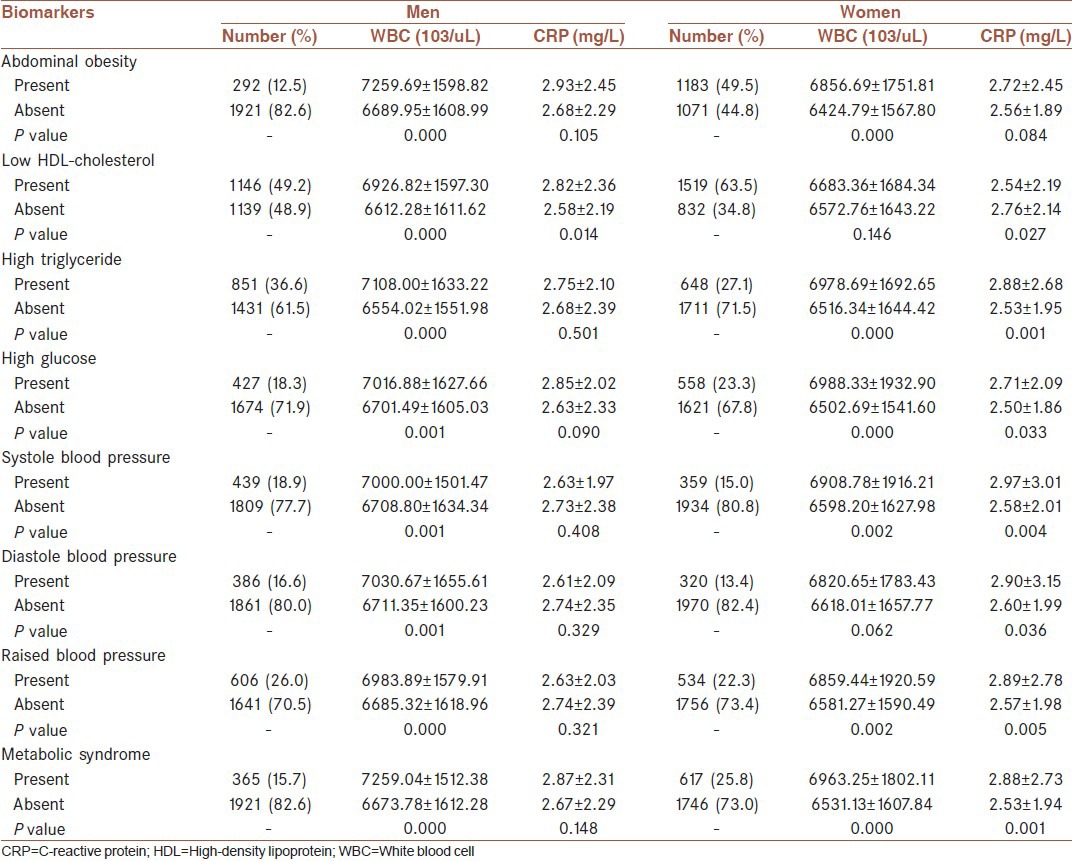
In women [Table 3], the mean values of WBC counts and CRP levels were statistically different in the subjects with and without a MetS component (except for the low HDL-cholesterol levels and high diastolic blood pressure for the WBC measures and abdominal obesity for the CRP measures) and for those with and without the MetS.
Table 3.
Univariate analyses with between white blood cell and C-reactive protein with number of metabolic syndrome components after adjusting by age and smoking
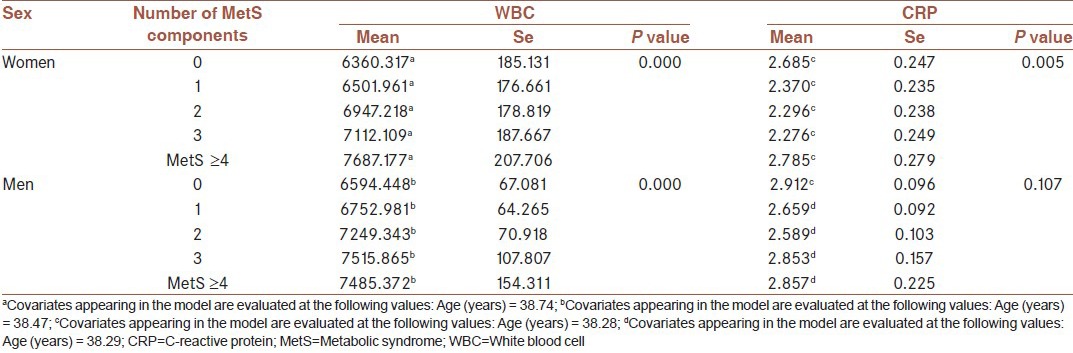
Furthermore, Table 3 hows the association between the CRP levels and WBC counts with the presence of the metabolic syndrome components. After adjustment for the age and smoking, significant relation was found between the number of the MetS components and WBC counts in both sexes. Association between the CRP levels and the number of the MetS components was insignificant.
DISCUSSION
This study aimed to identify the associations between the WBC counts and the serum CRP levels with the MetS in the adult Iranian population. The results showed that WBC counts were associated with the MetS in both men and women. However, the CRP levels were only associated with the MetS in the women. WBC counts were not significantly associated with the low HDL cholesterol levels as well as the increased diastolic blood pressure in the men, but this association was confirmed between different components of the MetS and WBC counts in the men. This result supports the findings of previous studies concerning a linear independent association between the WBC count and the risk of the MetS.[19,20] However, in other studies; finding was not specified in men or women. Overall, it seems that an increased WBC count may exacerbate insulin resistance and lead to the MetS and this pathway might be different in the two genders in various populations.
CRP is a sensitive marker of systemic inflammation which is produced by the liver.[14] Various studies have reported a linear association between the CRP levels and the metabolic disorders, including insulin resistance, the MetS, and the components of MetS.[21,22] In the Finnish Diabetes Prevention Study, CRP introduced as the best immunological predictor for the progression from impaired glucose tolerance to overt type 2 diabetes.[23] In our study, women participants with MetS were found to have significantly higher CRP levels than those without. On the contrary, we could not observe an independent association between the CRP level and MetS in the whole study population. In men, CRP did not increase significantly as a risk factor for the development of the MetS, while in the women; CRP was in association with the MetS. This finding was totally inconsistent with the study of Ryu et al.[23] To the best of our own knowledge, there is presently no study regarding the association between the inflammation and the MetS with sex. In this study, some baseline factors differed between the men and women, and it is likely that another set of factors related to inflammation influence this situation, such as cyclical hormonal changes associated with the menstrual cycle and subclinical autoimmune reactions.[23] Saltevo et al., showed that the levels of proinflammatory markers of CRP and interlukine-1, were significantly higher among the women with the MetS, rather than the men with the MetS, independently of the definition used International Diabetes Federation and National Cholesterol Education Program-Third Adult Treatment Panel. In contrast, another study showed that there was no difference between the men and the women without the MetS regarding the serum interlukine-1and CRP levels.[25] In this context, a recent meta-analysis has demonstrated that the high testosterone levels are associated with the high risk of type 2 diabetes in women, but with low risk in men.[26] High concentrations of sex hormone-binding-globulin are associated with the decreased risk of diabetes, particularly in the postmenopausal women.[27] Overall, although available data on the effects of gender relationships between the serum CRP levels and the MetS or atherosclerosis have been reported;[28] further prospective studies are required to confirm the contribution of CRP and other inflammatory markers to the development of the MetS. If this were confirmed, it would have substantial implications for the prevention and management of the MetS and atherosclerotic diseases, as these involve the suppression of inflammatory conditions rather than the incitement of anti-inflammatory conditions.
Limitation
The main limitation of this study was its cross-sectional design. In addition, this study could not show the temporal ordering of the association between the CRP levels, WBC counts and the MetS. Further longitudinal investigations are needed to confirm these associations.
ACKNOWLEDGMENT
The IHHP was conducted by the Isfahan Cardiovascular Research Center with the collaboration of Isfahan Provincial Health Office. It was supported by a grant (No. 31309304) from the Iranian Budget and Planning Organization, as well as the Deputy for Health of the Iranian Ministry of Health and Medical Education and the Iranian Heart Foundation. We are thankful to the team of ICRC and Isfahan Provincial Health Office as well as collaborators from Najaf-Abad Health Office and Arak University of Medical Sciences.
Footnotes
Source of Support: This program was supported by a grant (No. 31309304) from the Iranian Budget and Planning Organization, as well as the Deputy for Health of the Iranian Ministry of Health and Medical Education and Iranian Heart Foundation. It was conducted by Isfahan Cardiovascular Institute with the collaboration of Isfahan Provincial Health Center, both affiliated to Isfahan University of Medical Sciences
Conflict of Interest: None declared.
REFERENCES
- 1.Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: An American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112:2735–52. doi: 10.1161/CIRCULATIONAHA.105.169404. [DOI] [PubMed] [Google Scholar]
- 2.Kahn R, Buse J, Ferrannini E, Stern M. The metabolic syndrome: Time for a critical appraisal: Joint statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2005;28:2289–304. doi: 10.2337/diacare.28.9.2289. [DOI] [PubMed] [Google Scholar]
- 3.Grundy SM, Howard B, Smith S, Jr, Eckel R, Redberg R, Bonow RO. Prevention Conference VI: Diabetes and cardiovascular disease: Executive summary: Conference proceeding for healthcare professionals from a special writing group of the American Heart Association. Circulation. 2002;105:2231–9. doi: 10.1161/01.cir.0000013952.86046.dd. [DOI] [PubMed] [Google Scholar]
- 4.Isomaa B, Almgren P, Tuomi T, Forsen B, Lahti K, Nissen M, et al. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care. 2001;24:683–9. doi: 10.2337/diacare.24.4.683. [DOI] [PubMed] [Google Scholar]
- 5.Guize L, Thomas F, Pannier B, Bean K, Danchin N, Bénétos A. Metabolic syndrome: Prevalence, risk factors and mortality in a French population of 62 000 subjects. Bull Acad Natl Med. 2006;190:685–97. [PubMed] [Google Scholar]
- 6.Wellen KE, Hotamisligil GS. Obesity-induced inflammatory changes in adipose tissue. J Clin Invest. 2003;112:1785–8. doi: 10.1172/JCI20514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rutter MK, Meigs JB, Sullivan LM, D’Agostino RB, Sr, Wilson PW. C-reactive protein, the metabolic syndrome, and prediction of cardiovascular events in the Framingham Offspring Study. Circulation. 2004;110:380–5. doi: 10.1161/01.CIR.0000136581.59584.0E. [DOI] [PubMed] [Google Scholar]
- 8.Heikkilä K, Ebrahim S, Lawlor DA. A systematic review of the association between circulating concentrations of C reactive protein and cancer. J Epidemiol Community Health. 2007;61:824–33. doi: 10.1136/jech.2006.051292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wannamethee SG, Lowe GD, Shaper AG, Rumley A, Lennon L, Whincup PH. The metabolic syndrome and insulin resistance: Relationship to haemostatic and inflammatory markers in older non-diabetic men. Atherosclerosis. 2005;181:101–8. doi: 10.1016/j.atherosclerosis.2004.12.031. [DOI] [PubMed] [Google Scholar]
- 10.Nakanishi N, Shiraishi T, Wada M. C-reactive protein concentration is more strongly related to metabolic syndrome in women than in men: The Minoh Study. Circ J. 2005;69:386–91. doi: 10.1253/circj.69.386. [DOI] [PubMed] [Google Scholar]
- 11.Pischon T, Hu FB, Rexrode KM, Girman CJ, Manson JE, Rimm EB. Inflammation, the metabolic syndrome, and risk of coronary heart disease in women and men. Atherosclerosis. 2008;197:392–9. doi: 10.1016/j.atherosclerosis.2007.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wannamethee SG, Whincup PH, Rumley A, Lowe GD. Inter-relationships of interleukin-6, cardiovascular risk factors and the metabolic syndrome among older men. J Thromb Haemost. 2007;5:1637–43. doi: 10.1111/j.1538-7836.2007.02643.x. [DOI] [PubMed] [Google Scholar]
- 13.Hamid YH, Rose CS, Urhammer SA, Glumer C, Nolsoe R, Kristiansen OP, et al. Variations of the interleukin-6 promoter are associated with features of the metabolic syndrome in Caucasian Danes. Diabetologia. 2005;48:251–60. doi: 10.1007/s00125-004-1623-0. [DOI] [PubMed] [Google Scholar]
- 14.Ford ES. The metabolic syndrome and Creactive protein, fibrinogen, and leukocyte count: Findings from the Third National Health and Nutrition Examination Survey. Atherosclerosis. 2003;168:351–8. doi: 10.1016/s0021-9150(03)00134-5. [DOI] [PubMed] [Google Scholar]
- 15.Desai MY, Dalal D, Santos RD, Carvalho JA, Nasir K, Blumenthal RS. Association of body mass index, metabolic syndrome, and leukocyte count. Am J Cardiol. 2006;97:835–8. doi: 10.1016/j.amjcard.2005.10.021. [DOI] [PubMed] [Google Scholar]
- 16.Sarraf-Zadegan N, Sadri G, Menk Afzali H, Baghaei M, Mohammadi Fard N, Shahrokhi S, et al. Isfahan Healthy Heart Programme: A comprehensive integrated community-based programme for cardiovascular disease prevention and control. Design, methods and initial experience. Acta cardiol. 2003;58:309–20. doi: 10.2143/AC.58.4.2005288. [DOI] [PubMed] [Google Scholar]
- 17.Gharipour M, Sarrafzadegan N, Sadeghi M, Andalib E, Talaie M, Shafie D, Aghababaie E. Predictors of metabolic syndrome in the Iranian population: waist circumference, body mass index, or waist to hip ratio? Cholesterol 2013. 2013 doi: 10.1155/2013/198384. 198384. doi:10.1155/2013/198384. Epub 2013 Mar 24. PubMed PMID: 23634297; PubMed Central PMCID: PMC3619538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin chem. 1972;18:499–502. [PubMed] [Google Scholar]
- 19.Nakanishi N, Sato M, Shirai K, Nakajima K, Murakami S, Takatoeige T, et al. Associations between white blood cell count and features of the metabolic syndrome in Japanese men office workers. Ind Health. 2002;40:273–7. doi: 10.2486/indhealth.40.273. [DOI] [PubMed] [Google Scholar]
- 20.Lohsoonthorn V, Dhanamun B, Williams M. Prevalence of metabolic syndrome and its relationship to white blood cell count in a population of Thai men and women receiving routine health examinations. Am J Hypertens. 2006;19:339–45. doi: 10.1016/j.amjhyper.2005.10.008. [DOI] [PubMed] [Google Scholar]
- 21.Festa A, D Agostino R, Jr, Howard G, Mykkanen L, Tracy RP, Haffner SM. Chronic subclinical inflammation as part of the insulin resistance syndrome: The Insulin Resistance Atherosclerosis Study (IRAS) Circulation. 2000;102:42–7. doi: 10.1161/01.cir.102.1.42. [DOI] [PubMed] [Google Scholar]
- 22.Herder C, Peltonen M, Koenig W, Kraft I, Muller-Scholze S, Martin S, et al. Systemic immune mediators and lifestyle changes in the prevention of type 2 diabetes. Diabetes. 2006;55:2340–6. doi: 10.2337/db05-1320. [DOI] [PubMed] [Google Scholar]
- 23.Ryu SY, Kim KS, Park J, Kang MG, Han MA. The association between circulating inflammatory markers and metabolic syndrome in Korean rural adults. J Prev Med Public Health. 2008 Nov;41:413–8. doi: 10.3961/jpmph.2008.41.6.413. doi: 10.3961/jpmph.2008.41.6.413. PubMed PMID: 19037171. [DOI] [PubMed] [Google Scholar]
- 24.Saltevo J, Vanhala M, Kautiainen H, Kumpusalo E, Laakso M. Gender differences in C-reactive protein, interleukin-1receptor antagonist and adiponectin levels in the metabolic syndrome: A population-based study. Diabet Med. 2008;25:747–50. doi: 10.1111/j.1464-5491.2008.02440.x. [DOI] [PubMed] [Google Scholar]
- 25.Ding EL, Song Y, Malik VS, Liu S. Sex differences of endogenous sex hormones and risk of type 2 diabetes. A systematic review and meta analysis. JAMA. 2006;295:1288–99. doi: 10.1001/jama.295.11.1288. [DOI] [PubMed] [Google Scholar]
- 26.Crandall C, Palla S, Reboussin B, Hu P, Barrett-Connor E, Reuben D, et al. Cross-sectional association between markers of inflammation and serum sex steroid levels in postmenopausal estrogen/progestin interventions trial. J Womens Health. 2006;15:14–23. doi: 10.1089/jwh.2006.15.14. [DOI] [PubMed] [Google Scholar]
- 27.Jovelić A, Raden S, Hajduković Z, Canji T. The relationship between C-reactive protein and subclinical carotid arteriosclerosis in military pilots. Vojnosanit Pregl. 2009;66:465–71. doi: 10.2298/vsp0906465j. [DOI] [PubMed] [Google Scholar]
- 28.Wang TJ, Nam BH, Wilson PW, Wolf PA, Levy D, Polak JF, et al. Association of C reactive protein with caritid atherosclerosis in men and women: The Framingham Heart Study. Arterioscler Thromb Vasc Biol. 2002;22:1662–7. doi: 10.1161/01.atv.0000034543.78801.69. [DOI] [PubMed] [Google Scholar]


