Abstract
Background:
The association of gastro-esophageal reflux (GER) with a wide variety of pulmonary disorders was recognized. We aimed to evaluate the effect of GER-induced esophagitis on airway hyper-reactivity (AHR) in patients and the response to treatment.
Materials and Methods:
In this cohort study, 30 patients attending the gastrointestinal clinic of a university hospital with acid reflux symptoms were included. All patients were evaluated endoscopically and divided into case group with esophagitis and control group without any evidence of esophagitis. Spirometry and methacholine test were done in all patients before and after treatment of GER with pantoprazole 40 mg daily for six months.
Results:
There was a significant difference in the rate of positive methacholine test between the cases (40%) and the controls (6.7%) prior to anti-acid therapy (P < 0.0001). After six months of treatment, the frequency of positive methacholine test diminished from 40 to 13.3% in the case group (P < 0.05) but did not change in the controls (P = 0.15).
Conclusion:
The presence of esophagitis due to GER would increase the AHR and treatment with pantoperazole would decrease AHR in patients with proved esophagitis and no previous history of asthma after six months.
Keywords: Airway hyper-reactivity, gastroesophageal reflux, methacholine test, spirometry
INTRODUCTION
Gastro-esophageal reflux (GER) disease is a common disorder and up to 40% of the Iranian population suffers from its classical symptoms.[1,2] The association of GER with a wide variety of pulmonary disorders was recognized as early as 1887. Mendelson[3] described pulmonary aspirations producing an acute asthma-like syndrome with wheezing in some patients. Researchers have suggested that GER is one of the etiologic factors in the development of pulmonary disorders,[4] upper respiratory symptoms such as cough, hoarseness, and throat complaints[5] as well as an aggravating factor for the symptoms of asthma.[6,7,8,9] Potential mechanisms underlying GER-induced airway symptomatology are thought to be microaspiration of acid into the airways with subsequent induction of an inflammatory response and bronchoconstriction, or stimulation of acid-sensitive receptors in the esophageal wall. The latter may either cause bronchoconstriction mediated by a direct vagal reflex or increase airway hyper-responsiveness through vagally-mediated pathways.[10,11] Several studies have been done to assess the association of GER and pulmonary disorders but most of these studies evaluated the effect of GER in asthmatics.[12,13,14,15] Bagnato et al., studied 30 patients suffering from GER without any evidence of asthma and 30 normal people using methacholine test. They concluded that subjects with GER had a greater increase in airway reactivity when inhaling methacholine compared to disease-free normal subjects.[16] In the present study we aimed to approach an asymptomatic respiratory disorder i.e., airway hyper-reactivity (AHR) via gastroenterologic abnormalities (GER symptoms and esophagitis). In addition, we tried to detect AHR in patients with esophagitis, and then the effect of six-month anti-reflux medical treatment on methacholine test and respiratory symptoms was assessed.
MATERIALS AND METHODS
In this controlled cohort study 30 patients with complaints of acid reflux symptoms and without respiratory symptoms attending a gastrointestinal clinic from November 2009 to May 2010 were included through convenience sampling. A checklist regarding gastrointestinal symptoms of GER was filled for each patient. All subjects with proven cardiovascular disease, pulmonary symptoms, active pulmonary disease like asthma, prior gastric surgery, pregnant women, active smokers, and patients with scleroderma were excluded. None of the subjects had used H2-blockers or proton pomp inhibitors during the three months preceding the study. All patients were evaluated endoscopically and the patients with esophageal, gastric and duodenal ulcers, patients with gastrointestinal malignancies were excluded. After upper gastrointestinal endoscopy, 15 patients were found to have reflux with esophagitis and another 15 had reflux without any evidence of distal esophagitis. They were organized as case and control groups respectively. The cases and the controls were matched for age and sex. Then all the patients underwent spirometry and methacholine test with asthograph. Asthograph is an apparatus that determines the resistance and conductivity of airways following inspiration of measured methacholine doses. Methacholine test was considered positive with constant doubled resistance or 35-40% decrease in conductivity.[17] After a six-month period of oral anti-acid therapy (40 mg pantoprazole daily, Adibi Pharmacy Co, Tehran, Iran), patients were evaluated with another spirometry and methacholine test. Relief from acid reflux symptoms was assessed at the sixth month of treatment. The definition of relief was patient-based judgment. There is no consensus indication for Helicobacter pylori eradication in patients without gastric and duodenal ulcers.[18] Since patients with gastric and duodenal ulcers were excluded, consequently all patients just receive proton pomp inhibitor treatment and Helicobacter pylori eradication was not indicated.
All subjects were completely informed about the study and gave their written informed consent prior to their inclusion in the study. The results were analyzed by Chi-square and independent t-test in SPSS Version 13. P value under 0.05 was considered statistically significant.
RESULTS
Demographic characteristics and spirometric values are shown in Table 1. According to the normal body mass index value (<25), 66.7% of cases and 60% of controls were normal (P = 0.30).
Table 1.
Demographic characteristics and mean spirometric values and their statistical analysis before and after methacholine test
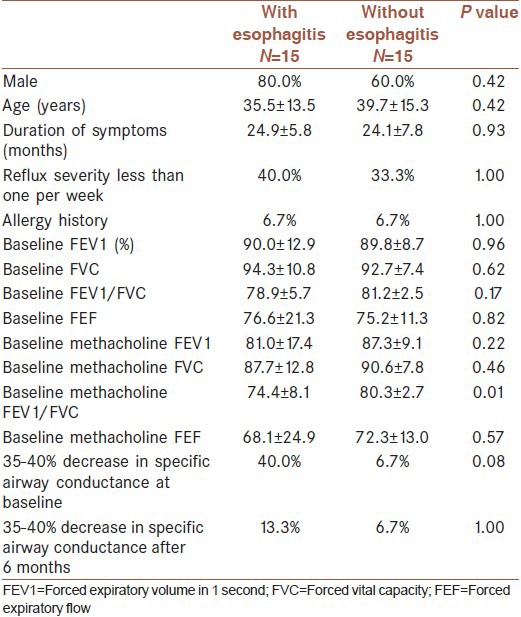
The mean period of symptomatic acid reflux was 24.9 ± 7.5 months in the case group and 24.1 ± 5.8 months in the control group (P = 0.93) and its severity was classified as follows; Class 1-less than once a week, Class 2-once a week, Class 3-two to four times a week, and Class 4-daily. All the patients underwent gastric mucosal biopsy for detection of Helicobacter pylori and it was found that 53.3% of cases and 33.3% of controls were infected (P = 0.04).
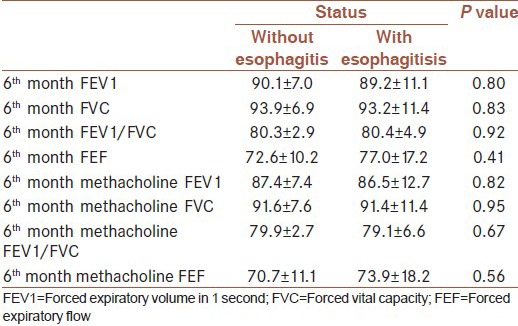
Acid reflux symptoms were relieved in 20% of the case group and 80% of the control group patients after anti-acid therapy with a significant difference (P < 0.0001). There was a significant difference in the rate of positive methacholine test between cases (40%) and controls (6.7%) prior to anti-acid therapy (P < 0.0001). After six months of anti-acid therapy, the rate of positive methacholine test diminished from 40 to 13.3% in the case group (P < 0.05) but did not change in the controls (P = 0.15). Mean spirometric values and their statistical analysis before and after methacholine test at the sixth month showed no difference between patients with and without esophagitis [Table 2].
Table 2.
Demographic characteristics and mean spirometric values and their statistical analysis before and after methacholine test at the 6th month
DISCUSSION
The prevalence of positive methacholine test in subjects with proven esophagitis was more than in patients with GER symptoms without evidence of esophagitis (40% vs. 6.7%), and it diminished after treatment with pantoprazole. There are several studies that have proved the high prevalence of GER in patients with asthma[19] but few ones have evaluated the effect of GER on bronchial hyper-reactivity in patients with no respiratory symptoms. Although the physiopathology and significance of asymptomatic bronchial hyper-reactivity are not definitively clarified, several investigations suggested that individuals with bronchial hyper-reactivity who have absolutely no symptoms may be in a latent phase of asthma that may become clinically active over the course of time.[20,21,22,23] Bagnato et al., in a study showed that subjects with GER and no clinical evidence of asthma had a greater increase in airway reactivity when inhaling methacholine compared to disease-free normal controls. They concluded that GER is associated with increased bronchial responsiveness following challenge with methacholine.[16] In a population-based birth cohort followed to age 26, Hancox et al., confirmed that there is a strong association between symptoms of GER and symptoms of asthma. Acid regurgitation tended to be a stronger predictor of respiratory symptoms than heartburn, but those with both heartburn and acid regurgitation had the highest risk of respiratory symptoms. The Hancox study provided longitudinal follow-up of asthma, wheeze and airway responsiveness since childhood, data on GER symptoms were not collected during childhood or adolescence and they were unable to establish the temporal sequence between respiratory symptoms, airway responsiveness and GER.[24] In another study by Demetrios et al., it was shown that patients with symptomatic GER and positive PH studies with no history of respiratory symptoms had significantly higher upper respiratory symptoms’ (laryngeal, nasal, sinus, pharyngeal and aural) scores than subjects with heartburn and negative PH probe studies. In their study, upper respiratory symptoms’ scores were proportional to the severity of GER expressed in numbers of reflux episodes recorded by 24-h monitoring. The proportional increase of scores with reflux episodes supports an association between GER and upper respiratory symptoms.[25]
Another aim of the present study was to determine whether acid-suppressive medical therapy would decrease AHR or not. Interestingly, after six-month anti-reflux treatment with pantoprazole, the rate of AHR decreased from 40% to 13.3% in the case group. In contrast, no change in AHR was observed after six-month treatment in the control group. This finding highlights the effect of GER and esophagitis in the pathogenesis of AHR, in which AHR responds to a proton pomp inhibitor with no direct medication for the respiratory system. Various studies have demonstrated controversial results about the effect of anti-reflux treatment with proton pomp inhibitors on asthma. Some studies revealed that treatment with proton pomp inhibitors had improved asthma symptoms and pulmonary function,[26,27] while Boeree et al., concluded that no clinical benefit of high-dose omeprazole could be established in asthma and chronic obstructive lung disease patients with severe airway hyper-responsiveness and increased GER.[28] In another study by Littner et al., it was shown that in patients with moderate to severe persistent asthma and symptoms of acid reflux, treatment with lansoprazole did not improve asthma symptoms or pulmonary function, or reduce albuterol use. It has been shown that lansoprazole could reduce asthma exacerbations and improve quality of life in patients with asthma.[29] However, in this study we focused on AHR patients without asthma and found a positive effect of acid-suppressive medical therapy on results of methacholine test.
The small sample size is a major limitation of our study. We did not perform esophageal biopsy and eosinophilic esophagitis although a rare disorder could not be ruled out.[30] Further studies with random selection and crossover design are recommended to improve both internal and external validity.
CONCLUSION
We concluded that the presence of esophagitis due to GER would increase the AHR, and a decrease in AHR in patients with proven esophagitis and no previous history of asthma receiving six months’ treatment with pantoprazole 40 mg daily was shown, as well.
ACKNOWLEDGMENT
This study was financially supported by the Baqiyatallah University of Medical Sciences, Tehran, Iran.
Footnotes
Source of Support: This study was financially supported by Baqiyatallah University of Medical Sciences, Tehran, Iran
Conflict of Interest: None declared.
REFERENCES
- 1.Ehsani MJ, Maleki I, Mohammadzadeh F, Mashayekh A. Epidemiology of gastroesophageal reflux disease in Tehran, Iran. J Gastroenterol Hepatol. 2007;22:1419–22. doi: 10.1111/j.1440-1746.2006.04616.x. [DOI] [PubMed] [Google Scholar]
- 2.Moghimi-Dehkordi B, Vahedi M, KhoshkroodMansoori B, Kasaeian A, Safaee A, Habibi M, et al. Economic burden of gastro-oesophageal reflux disease and dyspepsia: A community-based study. Arab J Gastroenterol. 2011;12:86–9. doi: 10.1016/j.ajg.2011.03.005. [DOI] [PubMed] [Google Scholar]
- 3.Mendelson CL. The aspiration of stomach contents into the lungs during obstetric anaesthesia. Am J Obstet Gynecl. 1946;52:191–201. doi: 10.1016/s0002-9378(16)39829-5. [DOI] [PubMed] [Google Scholar]
- 4.Pereira JC. [Lung diseases and gastro-oesophageal reflux disease] Rev Port Pneumol. 2009;15:899–921. doi: 10.1016/s0873-2159(15)30185-9. [DOI] [PubMed] [Google Scholar]
- 5.SaritasYuksel E, Vaezi MF. Extraesophageal manifestations of gastroesophagealb reflux disease: Cough, asthma, laryngitis, chest pain. Swiss Med Wkly. 2012;142:w13544. doi: 10.4414/smw.2012.13544. [DOI] [PubMed] [Google Scholar]
- 6.Onyekwere CA, Adeyeye OO, Ogbera AO, Duro-Emmanuel F. Prevalence of gastroesophageal reflux disease among patients with bronchial asthma. Trop Gastroenterol. 2010;31:195–8. [PubMed] [Google Scholar]
- 7.Saber H, Ghanei M. Extra-esophageal manifestations of gastroesophageal reflux disease: Controversies between epidemiology and clicnic. Open Respir Med J. 2012;6:121–6. doi: 10.2174/1874306401206010121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mureşan I, Picos A, Grad S, Dumitrascu DL. Respiratory involvement in thegastroesophageal reflux disesease. Rev Med ChirSoc Med Nat Iasi. 2011;115:662–71. [PubMed] [Google Scholar]
- 9.Gopal B, Singhal P, Gaur SN. Gastroesophageal reflux disease in bronchial asthma and the response to omeprazole. Asian Pac J Allergy Immunol. 2005;23:29–34. [PubMed] [Google Scholar]
- 10.Mansfield LE, Hameister HH, Spaulding HS, Smith NJ, Glab N. The role of the vagus nerve in airway narrowing caused by intraesophageal hydrochloric acid provocation and esophageal distention. Ann Allergy. 1981;47:431–4. [PubMed] [Google Scholar]
- 11.Jack CI, Calverley PM, Donnelly RJ, Tran J, Russell G, Hind CR, et al. Simultaneous tracheal and oesophageal pH measurements in asthmatic patients with gastro-oesophageal reflux. Thorax. 1995;50:201–4. doi: 10.1136/thx.50.2.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nagel RA, Brown P, Perks WH, Wilson RS, Kerr GD. Ambulatory pH monitoring of gastro-oesophageal reflux in “morning dipper” asthmatics. BMJ. 1988;297:1371–3. doi: 10.1136/bmj.297.6660.1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sontag SJ, O’Connell S, Khandelwal S, Miller T, Nemchausky B, Schnell TG, et al. Most asthmatics have gastroesophageal reflux with or without bronchodilator therapy. Gastroenterology. 1990;99:613–20. doi: 10.1016/0016-5085(90)90945-w. [DOI] [PubMed] [Google Scholar]
- 14.Vincent D, Cohen-Jonathan AM, Leport J, Merrouche M, Geronimi A, Pradalier A, et al. Gastro-oesophageal reflux prevalence and relationship with bronchial reactivity in asthma. Eur Respir J. 1997;10:2255–9. doi: 10.1183/09031936.97.10102255. [DOI] [PubMed] [Google Scholar]
- 15.Kiljander TO, Salomaa ER, Hietanen EK, Terho EO. Gastroesophageal reflux in asthmatics: A double-blind, placebo-controlled crossover study with omeprazole. Chest. 1999;116:1257–64. doi: 10.1378/chest.116.5.1257. [DOI] [PubMed] [Google Scholar]
- 16.Bagnato GF, Gulli S, Giacobbe O, De Pasquale R, Purello D’Ambrosio F. Bronchial hyperresponsiveness in subjects with gastroesophageal reflux. Respiration. 2000;67:507–9. doi: 10.1159/000067464. [DOI] [PubMed] [Google Scholar]
- 17.Hegewald MJ, Crapo RO. Pulmonary Function Testing. In: Murray JF, Nadel JA, editors. Textbook of Respiratory Medicine. Philadelphia PA: WB Saunders; 2010. p. 547. [Google Scholar]
- 18.Bazzoli F, Bianchi Porro G, Bianchi MG, Molteni M, Pazzato P, Zagari RM. Treatment of Helicobacter pylori infection. Indications and regimens: An update. Dig Liver Dis. 2002;34:70–83. doi: 10.1016/s1590-8658(02)80062-7. [DOI] [PubMed] [Google Scholar]
- 19.Larrain A, Carrasco E, Galleguillos F, Sepulveda R, Pope CE., 2nd Medical and surgical treatment of nonallergic asthma associated with gastroesophageal reflux. Chest. 1991;99:1330–5. doi: 10.1378/chest.99.6.1330. [DOI] [PubMed] [Google Scholar]
- 20.Carey VJ, Weiss ST, Tager IB, Leeder SR, Speizer FE. Airways responsiveness, wheeze onset, and recurrent asthma episodes in young adolescents. Am J Respir Crit Care Med. 1996;153:356–61. doi: 10.1164/ajrccm.153.1.8542143. [DOI] [PubMed] [Google Scholar]
- 21.Jones A. Asymptomatic bronchial hyperreactivity and the development of asthma and other respiratory tract illnesses in children. Thorax. 1994;49:757–61. doi: 10.1136/thx.49.8.757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Burrows B, Sears MR, Flannery EM, Herbison GP, Holdaway MD, Silva PA. Relation of the course of bronchial responsiveness from age 9 to age 15 to allergy. Am J Respir Crit Care Med. 1995;152(4 Pt 1):1302–8. doi: 10.1164/ajrccm.152.4.7551386. [DOI] [PubMed] [Google Scholar]
- 23.Hopp RJ, Townley RG, Biven RE, Bewtra AK, Nair NM. The presence of airway reactivity before the development of asthma. Am Rev Respir Dis. 1990;141:2–8. doi: 10.1164/ajrccm/141.1.2. [DOI] [PubMed] [Google Scholar]
- 24.Hancox RJ, Poulton R, Taylor DR, Greene JM, McLachlan CR, Cowan JO, et al. Associations between respiratory symptoms, lung function and gastro-oesophageal reflux symptoms in a population-based birth cohort. Respir Res. 2006;7:142. doi: 10.1186/1465-9921-7-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Theodoropoulos DS, Ledford DK, Lockey RF, Pecoraro DL, Rodriguez JA, Johnson MC, et al. Prevalence of upper respiratory symptoms in patients with symptomatic gastroesophageal reflux disease. Am J Respir Crit Care Med. 2001;164:72–6. doi: 10.1164/ajrccm.164.1.2006002. [DOI] [PubMed] [Google Scholar]
- 26.Shimizu Y, Dobashi K, Kobayashi S, Ohki I, Tokushima M, Kusano M, et al. A proton pump inhibitor, lansoprazole, ameliorates asthma symptoms in asthmatic patients with gastroesophageal reflux disease. Tohoku J Exp Med. 2006;209:181–9. doi: 10.1620/tjem.209.181. [DOI] [PubMed] [Google Scholar]
- 27.Sharma B, Sharma M, Daga MK, Sachdev GK, Bondi E. Effect of omeprazole and domperidone on adult asthmatics with gastroesophageal reflux. World J Gastroenterol. 2007;13:1706–10. doi: 10.3748/wjg.v13.i11.1706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Boeree MJ, Peters FT, Postma DS, Kleibeuker JH. No effects of high-dose omeprazole in patients with severe airway hyperresponsiveness and (a)symptomatic gastro-oesophageal reflux. Eur Respir J. 1998;11:1070–4. doi: 10.1183/09031936.98.11051070. [DOI] [PubMed] [Google Scholar]
- 29.Littner MR, Leung FW, Ballard ED, 2nd, Huang B, Samra NK Lansoprazole Asthma Study Group. Effects of 24 weeks of lansoprazole therapy on asthma symptoms, exacerbations, quality of life, and pulmonary function in adult asthmatic patients with acid reflux symptoms. Chest. 2005;128:1128–35. doi: 10.1378/chest.128.3.1128. [DOI] [PubMed] [Google Scholar]
- 30.Lucendo AJ. Eosinophilic diseases of the gastrointestinal tract. Scand J Gastroenterol. 2010;45:1013–21. doi: 10.3109/00365521003690251. [DOI] [PubMed] [Google Scholar]


