Abstract
Background:
Seborrheic dermatitis (SD) is a common, chronic inflammatory disease. Inflammatory reaction and oxidative stress are thought to be effective in the pathogenesis of SD. Based on anti-inflammatory and anti-oxidant properties of emu oil, this study was designed to evaluate effects of emu oil on patients suffering from SD, and to compare it with routine treatments of SD with topical steroids and antifungal agents.
Materials and Methods:
This clinical trial was conducted on126 patients who were randomly allocated to 2 groups: 62 in the clotrimazole vs. emu oil (group-1) and 64 in the hydrocortisone vs. emu oil (group-2). The right side of the face in both groups was treated with topical emu oil. The left side was treated with topical clotrimazole in the first group and with topical hydrocortisone in the second group. One month after the treatment, pre and post treatment symptom severity scores of pruritus, erythema and scales were compared.
Results:
All 3 medications significantly improved pruritus, erythema and scales (P < 0. 01). However, topical clotrimazole and hydrocortisone were significantly more effective than emu oil in improving scales (P < 0.01), and hydrocortisone was significantly more effective than emu oil in reducing pruritus (P < 0. 01). Comparing with topical clotrimazole, emu oil resulted in significantly more improvement of erythema (p:0.01).
Conclusion:
Emu oil is a potentially useful agent that significantly improves itching, erythema and scales associated with SD; however, it was less effective than hydrocortisone and clotrimazole which are routinely prescribed to treat SD.
Keywords: Emu oil, seborrehic dermatitis, therapy
INTRODUCTION
Seborrheic dermatitis (SD) is a common, chronic inflammatory disease that affects areas with increased density of sebaceous glands including face, scalp, upper trunk, and flexures of about 3-5% of the general population at any age.[1,15,10,26,31]
Although, the exact cause of SD remains unclear, it is believed that many factors may contribute to its development. For instance, inflammatory reaction to colonization of Malassezia yeasts and increased oxidative stress are thought to play an important role in the pathogenesis of SD.[7,18] Topical glucocorticoids have been considered as the mainstay of treatment of SD.[12,14] However, because chronic use of moderate to potent topical steroids may cause many adverse effects including, atrophy, telangiectasia, glaucoma, adrenal suppression, and also diminishing effectiveness, many other therapeutic options have been emerged, and a variety of topical therapies such as antifungals, zinc pyrithione, metronidazole, lithium salts, calcineurin inhibitors, coal tar shampoos, and selenium sulfide have been used to treat SD[8,16,19,20,21,25] Although effective medications are available for SD, need for long-term treatment necessitates use of treatment options with fewer side-effects and more patient's compliance. For this reason, there is a growing interest in the use of natural remedies.[6,27,33]
Emu oil has been recently demonstrated to have potent anti-inflammatory activity associated with decreased levels of the proinflammatory cytokines in the tissue.[13,14,15,16,17,18,19,20,21,22,23] Topical application of Emu oil has been shown to promote wound healing, and improve recovery of damaged skin.[3,7] Lagniel, Politis and Dmytrowich demonstrated that anti-inflammatory properties of transdermal application of Emu oil have been reported to be as effective as orally administered Ibuprofen.[2] In addition, Emu oil contains variable levels of several compounds with antioxidant properties.[22,4]
Due to the underlying well-known mechanism of oxidative stress and inflammation in the pathogenesis of Seborrheic dermatitis (SD), we tried to compare the efficacy of Emu oil with the routine SD treatments.
MATERIALS AND METHODS
This was a randomized controlled clinical trial, which was performed in dermatology out-patient clinics of the Isfahan University of Medical Sciences (IUMS), between August 2011 and September 2012. The sampling method used was simple random sampling.
Patients aged between 14 years and 60 years[34] with skin types II-V reference for Fitzpatrick is essential who had bilateral facial involvement with SD entered the study. The diagnosis of SD was carried out by an expert dermatologist in all the patients.
Subjects were excluded if they had previous history of medical therapy in 4 weeks apart of the investigation.[33]
After describing the goal of the study for all participants and describing the confidentiality of the information, all participants were assigned the consent form.
This research is approved by IUMS with the research project number 290279.
Participants were randomly allocated by random allocation to 2 treatment groups: Both groups were treated by Emu oil at the right side of the face and the left side had been treated by clotrimazole in the group 1 and with hydrocortisone in group 2 at the base line all the patients were visited by an expert dermatologist to assess the baseline severity score of seborrhoeic dermatitis symptoms (erythema, scaling, and pruritus) the erythema and scaling were evaluated due to 0-3 score in each side of the face: 0 = absent 1 = mild 2 = moderate 3 = severe, but the degree of pruritus was assessed by visual analog scaling (VAS) method. A 10 cm rule were demonstrated to the patient as VAS and the patients were asked to rate the severity of their pruritus over the previous 24 h by marking a point on the VAS line between 0 (no itching) and 10 (the most severe itching they have ever experienced).
The pure 20% Emu oil (Abian Ltd., Kashan, Iran) was used in the right side in both groups. The left side of the face in the group 1 was treated with topical clotrimazole 1% (Behvarzan co., Tehran, Iran) while in group 2, the topical hydrocortisone 1% (Behvarzan co., Tehran, Iran) All medications were prescribed twice daily for 30 days at the morning and evening on the cleaned skin.
Patients were asked to report any side-effect (contact dermatitis symptoms and so on) if there were any intolerable and sever symptoms the drug therapy was stopped and patients were treated by the routine SD treatment methods.
At the end of the study, all symptoms were reevaluated by the same dermatologist and the improvement in each one of the symptoms was assessed.
The mean difference in scores of erythema and scale and the pruritus were compared in both sides of the face and all the side-effects were reported was the clinical trial registered?
Since, both researcher and patient are informed of the treatment details, the study is not blinded.
Statistical analysis
Data were analyzed by SPSS 16.5 using independent t-test, Chi-square, and ANOVA. P values < 0.05 were considered statistically significant.
RESULTS
This randomized clinical trial has been performed on Seborhoeic dermatitis patients.
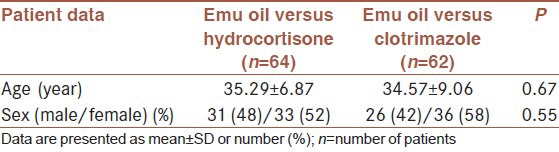
The samples consisted of 69 (55%) women and 57 (45%) men. There was no significant difference between 2 groups regarding baseline characteristics [Table 1].
Table 1.
Comparison of baseline characteristics between 2 groups
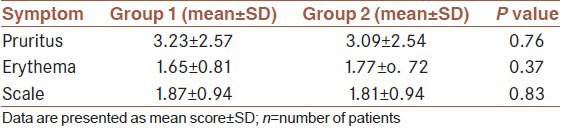
There was no significant difference between 2 groups regarding the baseline severity score of symptoms including pruritus, erythema, and scales [Table 2].
Table 2.
Comparison of baseline symptom severity score between 2 groups
All symptoms of SD (pruritus, scale, and erythema) were significantly differed at the end of the study in comparison to base line in all three treatment modalities (P value < 0.01).
The changing in pruritus score (due to VAS) was significantly different in hydrocortisone site in comparison to Emu oil [Table 3]. However, there were no difference between Emu oil and clotrimazole [Table 4].
Table 3.
Comparison of pre and post-treatment symptom severity score within and between treatment for group 2
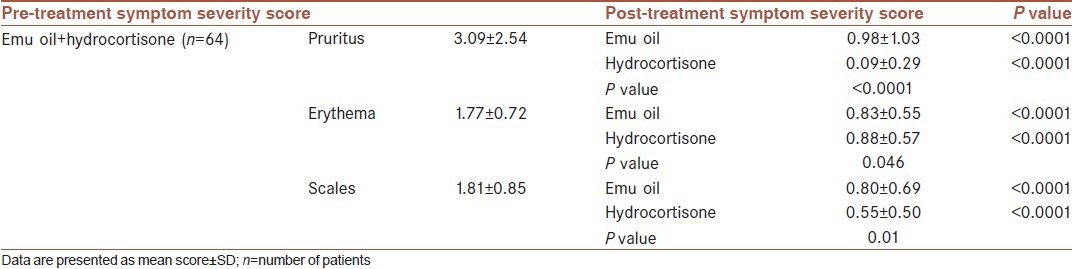
Table 4.
Comparison of pre- and post-treatment symptom severity score within and between treatment for group 1
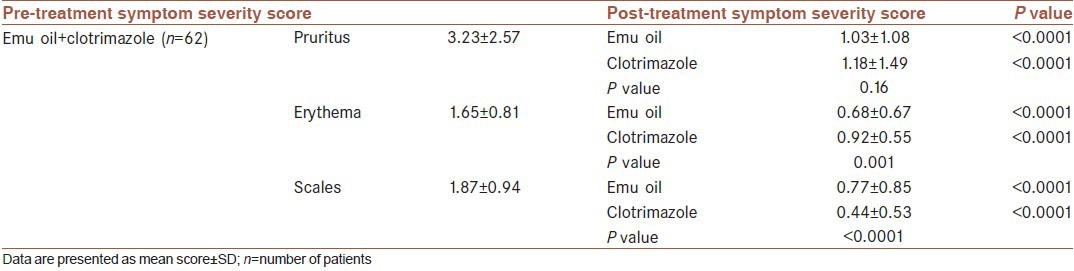
The changing in erythema score is significantly different in clotrimazole treated site in comparison to Emu oil [Table 3], but there was no difference between Emu oil and hydrocortisone [Table 3].
The score of scaling was changed more significantly by hydrocortisone and clotrimazole in comparison to Emu-oil [Tables 3–5].
Table 5.
Comparison of post-treatment severity of symptoms between three different treatment groups
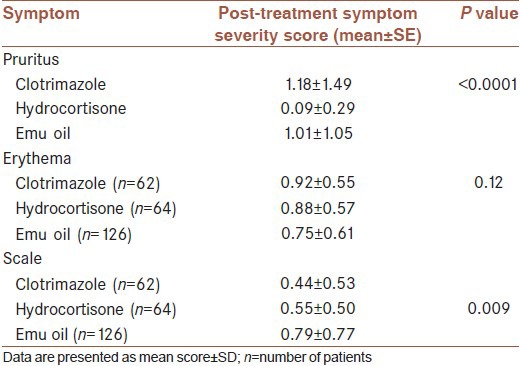
Due to ANOVA, the pruritus was significant differed in hydrocortisone group in comparison to Emu oil and clotrimazole (P<0.01).
The ANOVA defined that there were no difference between three groups in control of erythema (P > 0.01).
The scaling score for clotrimazole is significantly (P < 0.01) different from that of Emu oil according to ANOVA results.
The detailed ANOVA results are presented in Table 5. There were no serious reported adverse effects by the patients.
DISCUSSION
Recently, many studies have been designed to investigate effects of Emu oil with different concentrations and preparations on different dermatologic symptoms, such as ditching, erythema, and irritation associated with skin diseases such as dermatitis, eczema, and psoriasis.[4] In this study, we tried to investigate effects of Emu oil on SD symptoms, and compared it with routine SD treatments.
Due to our observation, all the treatment modalities can control all the main SD symptoms and the improvement is quite visible in three groups, but the effect of Emu oil was less effective than clotrimazol in controlling the scales and was weaker than hydrocortisone in controlling the pruritus. The potency of Emu oil in treating the erythema was similar to other routine treatment protocols Studies suggested that the effects of Emu oil on SD symptoms may be related to its antioxidation and anti-inflammatory properties.[29,22]
The inflammation is a well-known underlying mechanism in SD, so medications like corticosteroids have efficient clinical efficacy on SD due to their anti-inflammatory effects previous animal studies showed that topical application of Emu oil alleviates inflammation, and promotes healing process. Topical anti-inflammatory activity of Emu oil is possibly associated with decreased levels of the pro-inflammatory cytokines Tumor Necrozing Factor-α (TNF-α) and Interlukin-1α (IL-1α).[5,13,11,9]
It has been suggested that the n-3 and n-9 fatty acids in Emu oil may be responsible for its anti-inflammatory action.[9]
Moreover, antioxidant properties of Emu oil may play an important role in its therapeutic effects.[22,4] In addition to several fatty acids including oleic acid, linoleic acid, palmitic acid, and a-linolenic acid, Emu oil contains various compounds with anti-oxidant properties such as carotenoids, flavones, polyphenols, tocopherol, and phospholipids, which are considered as the probable source of therapeutic benefits.[2,4]
The role of oxidative stress has been demonstrated in the pathogenesis of more than 100 disorders such as allergic diseases, inflammatory skin disorders, acne vulgaris, vitiligo, atopic dermatitis, psoriasis, Behcet's disease, and skin cancers.[7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28]
Recently, a study by Emre et al. showed that SD may be associated with oxidative stress as well.[32] Given the anti-oxidant activity of Emu oil and role of oxidative stress in the pathogenesis of SD, it is not surprising to find Emu oil as an effective therapeutic agent for this clinical condition.
Fortunately, similar to the previous studies, no serious adverse effect was found associated with topical use of Emu oil.[13,2] It is an important advantage for this medication in comparison with other pharmaceutical compounds like steroids.
Since, we have prescribed natural pure Emu oil for SD patients and found it effective, other modified preparations of Emu oil may even result in more clinical improvement.
As hydrocotison had more effect on pruritus than other two treatment modalities, it seems that the selection of hydrocrtison is logical when the main symptom of the patient is pruritus.
Because of an acceptable improvement in pruritus severity index in Emu oil group, we suggest that Emu oil could be added to hydrocortisone to relieve pruritus more significantly and reduce the side-effects or could be used solely in treatment of those patients and areas that we are frightened about corticostroid side-effects such as periocular and genital areas and infant and children.
The efficacy of clotrimazole on scaling was better than other treatments, but addition of Emu oil to clotrimazole could have a better influence on the scales because of the hydrating potency and emollient activities of Emu oil.
As we shown the erythema is quite well-controlled by all treatment modalities, so Emu oil could be a well choice with less side-effects in treating this symptom Emu oil is a potentially useful agent that significantly improves itching, erythema, and scales associated with SD; however, it was less effective than routine topical therapies.
The mechanisms responsible for aforementioned therapeutic effects of Emu oil remain to be ascertained, and further biochemical assessments are needed to determine how this agent affects SD symptoms.
Limitation of the study
Since both the researcher and patient are informed of the treatment details, the study is not blinded; it might be a limitation for the study.
ACKNOWLEDGMENT
The authors should appreciate Dr. Shahtalebi who prepared the topical samples and also Dr. J. Jouzdani for his cooperation in data analysis.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Schechtman RC, Midgley G, Hay RJ. HIV disease and Malassezia yeasts: A quantitative study of patients presenting with seborrhoeic dermatitis. Br J Dermatol. 1995;133:694–8. doi: 10.1111/j.1365-2133.1995.tb02740.x. [DOI] [PubMed] [Google Scholar]
- 2.Snowden JM, Whitehouse MW. Anti-inflammatory activity of emu oils in rats. Inflammopharmacology. 1997;5:127–32. doi: 10.1007/s10787-997-0021-x. [DOI] [PubMed] [Google Scholar]
- 3.Politis MJ, Dmytrowich A. Promotion of second intention wound healing by emu oil lotion: Comparative results with furasin, polysporin, and cortisone. Plast Reconstr Surg. 1998;102:2404–7. doi: 10.1097/00006534-199812000-00020. [DOI] [PubMed] [Google Scholar]
- 4.Whitehouse MW, Turner AG, Davis CK, Roberts MS. Emu oil (s): A source of non-toxic transdermal anti-inflammatory agents in aboriginal medicine. Inflammopharmacology. 1998;6:1–8. doi: 10.1007/s10787-998-0001-9. [DOI] [PubMed] [Google Scholar]
- 5.Bornhövd E, Burgdorf WH, Wollenberg A. Macrolactam immunomodulators for topical treatment of inflammatory skin diseases. J Am Acad Dermatol. 2001;45:736–43. doi: 10.1067/mjd.2001.117525. [DOI] [PubMed] [Google Scholar]
- 6.Satchell AC, Saurajen A, Bell C, Barnetson RS. Treatment of dandruff with 5% tea tree oil shampoo. J Am Acad Dermatol. 2002;47:852–5. doi: 10.1067/mjd.2002.122734. [DOI] [PubMed] [Google Scholar]
- 7.Baz K, Cimen MY, Kokturk A, Yazici AC, Eskandari G, Ikizoglu G, et al. Oxidant/antioxidant status in patients with psoriasis. Yonsei Med J. 2003;44:987–90. doi: 10.3349/ymj.2003.44.6.987. [DOI] [PubMed] [Google Scholar]
- 8.Dreno B, Chosidow O, Revuz J, Moyse D Study investigator group. Lithium gluconate 8% vs. ketoconazole 2% in the treatment of seborrhoeic dermatitis: A multicentre, randomized study. Br J Dermatol. 2003;148:1230–6. doi: 10.1046/j.1365-2133.2003.05328.x. [DOI] [PubMed] [Google Scholar]
- 9.Yoganathan S, Nicolosi R, Wilson T, Handelman G, Scollin P, Tao R, et al. Antagonism of croton oil inflammation by topical emu oil in CD-1 mice. Lipids. 2003;38:603–7. doi: 10.1007/s11745-003-1104-y. [DOI] [PubMed] [Google Scholar]
- 10.Gupta AK, Madzia SE, Batra R. Etiology and management of Seborrheic dermatitis. Dermatology. 2004;208:89–93. doi: 10.1159/000076478. [DOI] [PubMed] [Google Scholar]
- 11.Li ZQ, Wang JH, Ren JL, Yi ZH. Effects of topical emu oil on wound healing in scalded rats. Di Yi Jun Yi Da Xue Xue Bao. 2004;24:1255–6. [PubMed] [Google Scholar]
- 12.Rigopoulos D, Ioannides D, Kalogeromitros D, Gregoriou S, Katsambas A. Pimecrolimus cream 1% vs. betamethasone 17-valerate 0.1% cream in the treatment of seborrhoeic dermatitis. A randomized open-label clinical trial. Br J Dermatol. 2004;151:1071–5. doi: 10.1111/j.1365-2133.2004.06208.x. [DOI] [PubMed] [Google Scholar]
- 13.Qiu XW, Wang JH, Fang XW, Gong ZY, Li ZQ, Yi ZH. Anti-inflammatory activity and healing-promoting effects of topical application of emu oil on wound in scalded rats. Di Yi Jun Yi Da Xue Xue Bao. 2005;25:407–10. [PubMed] [Google Scholar]
- 14.Firooz A, Solhpour A, Gorouhi F, Daneshpazhooh M, Balighi K, Farsinejad K, et al. Pimecrolimus cream, 1%, vs. hydrocortisone acetate cream, 1%, in the treatment of facial seborrheic dermatitis: A randomized, investigator-blind, clinical trial. Arch Dermatol. 2006;142:1066–7. doi: 10.1001/archderm.142.8.1066. [DOI] [PubMed] [Google Scholar]
- 15.Schwartz RA, Janusz CA, Janniger CK. Seborrheic dermatitis: An overview. Am Fam Physician. 2006;74:125–30. [PubMed] [Google Scholar]
- 16.Elewski BE, Abramovits W, Kempers S, Schlessinger J, Rosen T, Gupta AK, et al. A novel foam formulation of ketoconazole 2% for the treatment of seborrheic dermatitis on multiple body regions. J Drugs Dermatol. 2007;6:1001–8. [PubMed] [Google Scholar]
- 17.Lagniel C, Torres AM. Consequences of burn injuries treatment with 100% pure emu oil. Burns. 2007;33:S148. [Google Scholar]
- 18.Manríquez JJ, Uribe P. Seborrhoeic dermatitis. Clin Evid. 2007;7:1713. [PMC free article] [PubMed] [Google Scholar]
- 19.Ozcan H, Seyhan M, Yologlu S. Is metronidazole 0.75% gel effective in the treatment of seborrhoeic dermatitis? A double-blind, placebo controlled study. Eur J Dermatol. 2007;17:313–6. doi: 10.1684/ejd.2007.0206. [DOI] [PubMed] [Google Scholar]
- 20.Seckin D, Gurbuz O, Akin O. Metronidazole 0.75% gel vs. ketoconazole 2% cream in the treatment of facial seborrheic dermatitis: A randomized, double-blind study. J Eur Acad Dermatol Venereol. 2007;21:345–50. doi: 10.1111/j.1468-3083.2006.01927.x. [DOI] [PubMed] [Google Scholar]
- 21.Warshaw EM, Wohlhuter RJ, Liu A, Zeller SA, Wenner RA, Bowers S, et al. Results of a randomized, double-blind, vehicle-controlled efficacy trial of pimecrolimus cream 1% for the treatment of moderate to severe facial seborrheic dermatitis. J Am Acad Dermatol. 2007;57:257–64. doi: 10.1016/j.jaad.2006.11.007. [DOI] [PubMed] [Google Scholar]
- 22.Bennett DC, Code WE, Godin DV. Comparison of the antioxidant properties of emu oil with other avian oils. Aust J Exp Agric. 2008;48:1345–50. [Google Scholar]
- 23.Cicek B, Bakers, Tagt D. Pimecrolimus 1% cream and methyl predniszolon acetonide 0.1% cream and metronidazol 0.75% gel in the treatment of seborrheic dermatosis: A randomized clinical study. J dermatol treat. 2009;20:344–9. doi: 10.3109/09546630802687349. [DOI] [PubMed] [Google Scholar]
- 24.Karaca S, Güder H. Antioxidant system in dermatology. Turkish J Dermatol. 2009;3:32–9. [Google Scholar]
- 25.Koc E, Arca E, Kose O, Akar A. An open, randomized, prospective, comparative study of topical pimecrolimus 1% cream and topical ketoconazole 2% cream in the treatment of seborrheic dermatitis. J Dermatolog Treat. 2009;20:4–9. doi: 10.1080/09546630802286993. [DOI] [PubMed] [Google Scholar]
- 26.Naldi L, Rebora A. Clinical practice. Seborrheic dermatitis. N Engl J Med. 2009;360:387–96. doi: 10.1056/NEJMcp0806464. [DOI] [PubMed] [Google Scholar]
- 27.Paghdal KV, Schwartz RA. Topical tar: Back to the future. J Am Acad Dermatol. 2009;61:294–302. doi: 10.1016/j.jaad.2008.11.024. [DOI] [PubMed] [Google Scholar]
- 28.Kadam DP, Suryakar AN, Ankush RD, Kadam CY, Deshpande KH. Role of oxidative stress in various stages of psoriasis. Indian J Clin Biochem. 2010;25:388–92. doi: 10.1007/s12291-010-0043-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lindsay RJ, Geier MS, Yazbeck R, Butler RN, Howarth GS. Orally administered emu oil decreases acute inflammation and alters selected small intestinal parameters in a rat model of mucositis. Br J Nutr. 2010;104:513–9. doi: 10.1017/S000711451000084X. [DOI] [PubMed] [Google Scholar]
- 30.Kutlubay Z, Kevser Uzunçakmak T, Engin B, Tüzün Y , Vitiligo and oxidative stress. J Turk Acad Dermatol. 2011;5:1154. [Google Scholar]
- 31.Sampaio AL, Mameri AC, Vargas TJ, Ramos-e-Silva M, Nunes AP, Carneiro SC. Seborrheic dermatitis. An Bras Dermatol. 2011;86:1061–71. doi: 10.1590/s0365-05962011000600002. [DOI] [PubMed] [Google Scholar]
- 32.Emre S, Metin A, Demirseren DD, Akoglu G, Oztekin A, Neselioglu S, et al. The association of oxidative stress and disease activity in seborrheic dermatitis. Arch Dermatol Res. 2012;304:683–7. doi: 10.1007/s00403-012-1254-0. [DOI] [PubMed] [Google Scholar]
- 33.Pazyar N, Yaghoobi R, Bagherani N, Kazerouni A. A review of applications of tea tree oil in dermatology. Int J Dermatol. 2012 doi: 10.1111/j.1365-4632.2012.05654.x. DOI: 10.1111/j. 1365-4632.2012.05654.x. [DOI] [PubMed] [Google Scholar]
- 34.Bolognia JL, Jorizzo JL, Schaffer JV. Dermatology. 3rd ed. Vol. 1. Elsevier; 2012. [Google Scholar]


