Abstract
Background:
The Le7 acupoint had been known as an acupoint for reducing pain of appendicitis. However, no study on the effect of its acupressure on post-appendectomy pain is available. The objective of this study was to evaluate the effects of acupressure of Le7 acupoint on pain, nausea, and vomiting after appendectomy.
Materials and Methods:
A single-blind randomized controlled trial was conducted on 70 post-appendectomy patients in a general surgical ward. Patients with inclusion criteria were selected consecutively and were randomly assigned into two groups. The intervention group received acupressure to the Le7 acupoint and the second group was the control group. The severity of post-operative pain, nausea, and vomiting measured hourly till the seventh post-operative hour. T-test was used to compare the mean of pain and nausea severity of two groups. Paired t-test was used to compare the mean of pain intensity of each group before and total mean of pain at post-intervention hours. Chi-squared test and Fisher exact test were used for nominal data.
Results:
The mean of pain intensity in the intervention group was 5.10 ± 3.52 before intervention and decreased to 3.53 ± 0.75 in the post-operative hours (P = 0.018). The mean of pain intensity in the control group was 4.45 ± 3.16 before intervention and changed to 4.01 ± 0.92 in the post-operative hours (P = 0.32). However, the mean of pain intensity in the intervention group was less than the control group till 6th h after the surgery. No significant differences were observed between the two groups in terms of nausea and vomiting (P = 0.74).
Conclusion:
Acupressure on Le7 acupoint was effective on post-appendectomy pain but did not affect nausea and vomiting. Further investigations are suggested with starting acupressure at the onset of pain or nausea and vomiting.
Keywords: Acupressure, appendectomy, Ex-Le7 point, nausea, pain, vomiting
INTRODUCTION
Pain, nausea, and vomiting are common problems after the most of surgeries. Based on the previous researches 70% of post-surgical patients are facing with moderate to severe pain.[1] Post-operative nausea and vomiting (PONV) are also distressing with a prevalence of 20-30%, depending the type of surgery and patient-related factors. These problems are not only discomforting, but also may cause dehydration, electrolyte disturbances, delayed recovery, and delayed hospital discharge, if prolonged.[2]
Opioids and non-steroidal anti-inflammatory drugs remain the most common treatments for post-operative pain. However, many of these drugs are expensive, and all are associated with complications.[3] Side effects of drugs used for PONV are also a problem. Droperidol may cause drowsiness and extra-pyramidal symptoms. Metoclopramide has the same side effects in addition to headache and diarrhea. Ondansetron is associated with headache, diarrhea, and transient increase in hepatic transaminase level.[4,5] To avoid these side effects, alternative methods may be used rather than drug therapy.
Acupressure as a pain relieving method[2,6,7] has been noticed all over the world.[8] There are certain points in the body, which are known as pressure points and are capable to transmit the energy. By pressing these points, muscle spasm goes away, blood circulation and the body's vital energy improve, and calm the nerves.[7,8] Several studies have been conducted on the effects of acupressure on post-operative pain, nausea, and vomiting in variety of surgeries. Most of the studies have used the acupoints P6 and sp6.[4,8,9,10] Samad et al. (2003) in cholecystectomy patients and Lweis et al. (1991) in children undergoing strabismus correction, studied the effect of P6 acupressure on PONV. They reported that this method was ineffective.[8,9] However, Fan et al. has reported that this method reduced the severity of PONV.[4] Lee (2003) has also reported that sp6 acupressure could reduce labor pain.[11] Felhendler and Lisander (1996) have also reported that acupressure was effective for pain relief after arthroscopy.[12]
Lanwei acupoint also known as Le7 acupoint or the extra point33 is located below the right knee with a distance of 2 cun from the St. 36 (Zusanli) acupoint. This point had been known as a useful acupoint for reducing pain of acute and chronic appendicitis.[13] However, no study on the effect of Le7 acupressure on post-appendectomy pain is available. We assumed that acupressure on this point may be effective in reliving post-appendectomy pain, nausea, and vomiting. Therefore, the present study was conducted with the aim of assessing the effect of acupressure on Le7 acupoint on pain, nausea, and vomiting of patients after appendectomy which is the most common emergency abdominal surgery.[14] If effective, this method may be suggested as a complementary treatment to reduce post-appendectomy pain, nausea, and vomiting.
MATERIALS AND METHODS
Study design
A single-blind randomized controlled trial was undertaken to evaluate the effects of Le7 acupressure in relieving pain, nausea, and vomiting post appendectomy.
Sampling
The study was conducted on 70 post-appendectomy patients referred to a general surgical ward in a university hospital in the first half of 2012. Sample size was calculated based on data obtained from a pilot study on 14 patients (7 in each group). After 1 h acupressure on Le7 point and measuring the pain intensity, the difference between experimental and control groups was 0.44 (SD = 1.181). Based on the above parameters and selecting the significance level to be less than 0.05 and a power of 0.8, 34 subjects were estimated to be needed in each group. Then, we selected 35 patients in each group.
Samples were selected consecutively among the patients admitted for appendectomy and patients who entered the study were randomly assigned into the groups [Figure 1]. Sampling continued till we had two groups completed. Before the surgery, the overall design of the study (without specifying the allocated group) explained to the patients.
Figure 1.
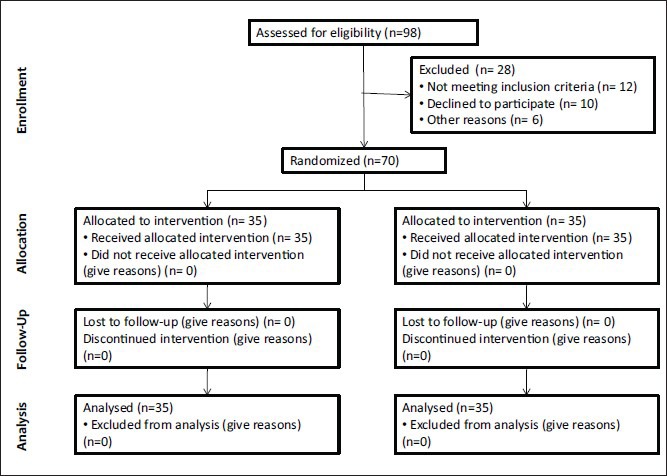
Design of the study
Inclusion and exclusion criteria
The criteria for inclusion of the participants were: The desire to participate in the research, no injury or lesion in the region of the acupoint of Le7, aged between 15 years and 70 years, being in the list of appendectomy surgery, and receiving general anesthesia. Those with the following conditions were not selected: A recent history of disorders associated with acute or chronic nausea and vomiting (such as gastrointestinal and ear disorders), experiencing nausea and vomiting during the last 24 h, the drug and alcohol addiction, a known neurological or psychiatric disease, and the previous use of acupressure or acupuncture techniques. The exclusion criteria were: Occurring unforeseen complications during surgery and anesthesia, prolonged surgical time (more than 2 h), receiving drugs outside anesthesia protocol for the routine appendectomy patients, and fever above 38°C.
Data collection instrument
Data collection instrument was prepared after a literature review and comprises three sections. The first section was the demographic data form and had six questions about the patient's age, gender, height, weight, level of education, and the study group the patient was belonged to. It also had two questions about the length of surgical incision (in millimeters) and the duration of anesthesia (in minutes). Second section was a visual analog scale (VAS) used for recording the severity of nausea. It consisted of a 100 mm calibrated line with a definite beginning and end. Descriptors were placed at each end of the line (0 = absence of nausea and vomiting and 100 = the worst condition). The observer asked the patient about the severity of nausea and marked an X on place that corresponded with severity of nausea. Nausea with a score of 70 was classified as severe, between 35 and 70 as moderate, and less than 35 as mild.[15] The frequency of vomiting was counted as a measure for the severity of vomiting. If there was retch or vomiting more than 5 times each hour, it was considered as severe vomiting, between 3 times and 5 times as the average and less than 3 times as mild.[16]
A VAS was also included in the third part for recording the severity of pain. It consisted of a 100 mm calibrated line with a definite beginning and end. Descriptors are placed at each end of the line (0 = no pain and 100 = the most unimaginable pain). Patients were asked to mark an X on place that corresponded with severity of pain.
Procedure
The researcher had been trained on acupressure and using the acuband before the study. Acupressure was applied using a special band called acuband (PsiBand, American design, made in China). It has a push button for applying pressure on the desired points.
The technique was started after the full patient's consciousness (so that the patient is aware of the location, time, and person). All the patients were anesthetized using thiopental sodium (5 mg/kg), Atracurium (0.6 mg/kg), and Fentanyl (2 mcg/kg) and then the anesthesia continued using a gas mixture of O2 + N2O (each: 50%), Morphine (0.1 mg/kg) and Isofeluran (1 MAC [minimum alveolar concentration]). All the patients were transferred to the surgical ward by a specially trained team to eliminate the effect of patient movement and handling of pain, nausea, and vomiting.
Initially, the severity of pain, nausea, and vomiting were assessed and recorded. Then the acuband was fastened by the second researcher. In the experimental group the acuband was fastened on the right leg in such a way that the button located exactly on the Le7 acupoint. Then, the pulses below the point were checked to ensure that the acuband would not interfere with the blood flow. The patient's foot was also examined for the possibility of impaired venous return.
In order to keep the patients and the staff blind to the group the patient was belonged to, an acuband also used in the control group, but the band was fasten loosely and in a way that the button placed right in opposite side of the Le7 point (as sham point). The occurrence and the severity of pain, nausea, and vomiting were assessed and recorded in the two groups hourly and up to 7th h.
The acubands was preserved for 7 h. However, they were loosened for 10 min every 2 h and then tightened.
For patients who suffered from severe nausea and vomiting during this period, anti-emetic medication (Metoclopramid, 10 mg) was administered and the nausea was considered as severe one. An analgesic medication (Pethidine, 1 mg/kg) also administered if the pain score was six or higher.
Ethical considerations
This study was approved by the Research Council and the Research Ethics Committee in our University of Medical Sciences. The researchers also obtained the permission from the hospital authorities. All the subjects had been informed about voluntary participation in the research, non-disclosure of personal information, and offered a written informed consent form to be signed before entering the study. All subjects have been assured that they will receive all the necessary care and pain medications if the intervention had no effect. The researchers were mindful of the need to pay close attention to ethical considerations and the welfare of the participants. Ethical issues also were observed in accordance with the Helsinki Convention.
Data analysis
The SPSS software (Statistical Package for the Social Sciences) version 11.5 used for data analysis. Independent sample t-test was used to compare the mean of pain and nausea severity of two groups. The mean of pain intensity before the intervention was compared to the average of pain intensity in the next 7 h. Also the mean of the nausea intensity was compared with average of nausea intensity in the next 7 h. Paired t-test was used to compare the mean of pain intensity of each group before and total mean of pain at post intervention hours. Chi-squared test and Fisher exact test used for the nominal data. A P value of less than 0.05 was considered to be significant for all tests.
RESULTS
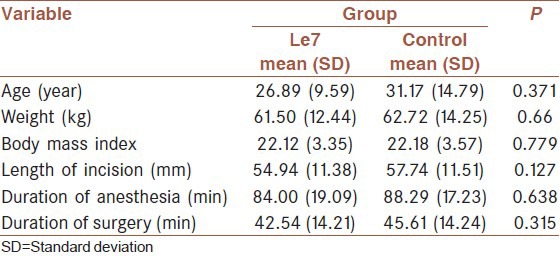
This study was undertaken on 70 patients in the age range 15-70 years. No significant difference was observed between the two groups in terms of age, body mass index, duration of anesthesia and the incision length [Table 1].
Table 1.
Demographic data of study groups
The mean of pain intensity in the Le7 group was less than the control group after the intervention (P = 0.02) [Table 2]. A significant deference was also observed between the mean pain severity of the Le7 group before the intervention and the total mean of pain severity in the seven post-operative hours (P = 0.018). However, such difference was not significant in the control group (P = 0.32). Figure 2 also shows that the mean of pain intensity was lower in Le7 group till the 6th h after the surgery.
Table 2.
Mean (SD), estimated difference (95% confidence interval) and P values for pain intensity in the two groups before and after the intervention
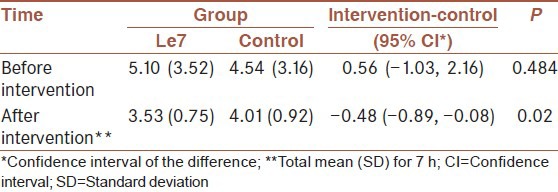
Figure 2.
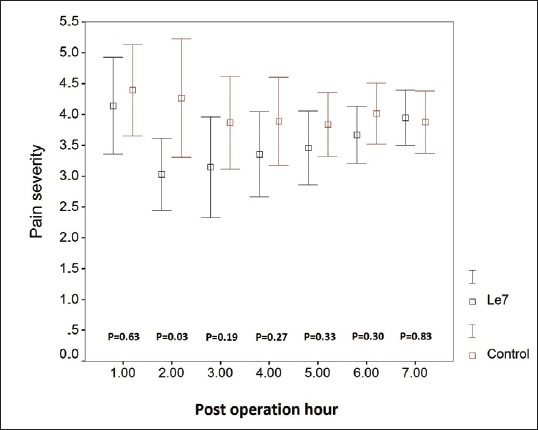
The mean and standard deviation of the pain severity in the seven post-operative hours
In total, 35 patients (18 in the Le7 group and 17 in the control group) experienced post-operative nausea. The incidence of nausea was not significantly different in the two groups. Also, no significant difference was observed between the means severity of post-operative nausea in the two groups [Table 3 and Figure 3].
Table 3.
Mean (SD), estimated difference (95% confidence interval) and P values for severity of nausea in the two groups before and after the intervention
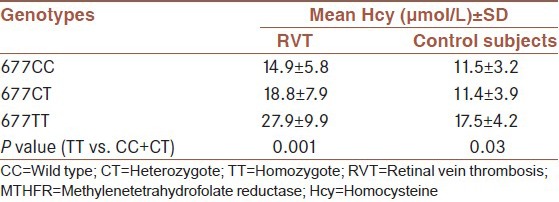
Figure 3.
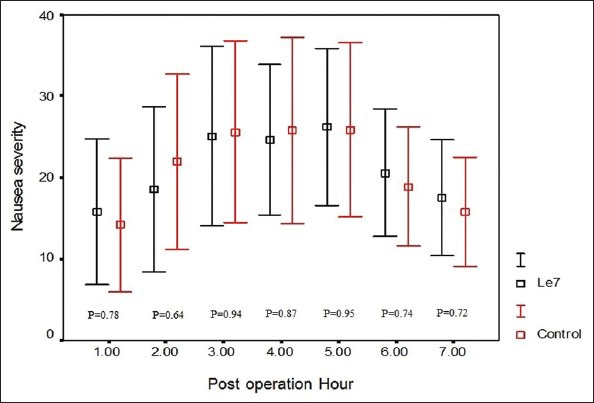
The mean and standard deviation of the nausea severity in the seven post-operative hours
Also 31 patients (16 in the Le7 group and 15 in the control group) experienced post-operative vomiting. From the total patients who experienced vomiting, four ones in the Le7 group and 7 patients in the control group had mild vomiting while the severity of vomiting was moderate in the other ones. None of the patients had severe vomiting.
DISCUSSION
In the present study the intensity of post-operative pain was lower in Le7 group than the control groups. Studies have been conducted on the effects of acupressure on pain have reported different results. Lee reported that this treatment was effective on pain after child birth.[11] However, another study reported that the method was not successful on pain reduction after abdominal surgeries.[3]
It is noteworthy that in previous studies on the effect of acupressure on pain, researchers applied the method on points that were fully known to be effective in traditional Chinese medicine.[3,11] For example, Lee stimulated the sp6 point that painless labor is one of its applications in acupuncture.[11] In the present study we examined the effect of pressure on Le7 acupoint that had been reported to be effective in reducing pain of acute and chronic appendicitis[13] but, no study was available to assess its acupressure on post appendectomy patients. On the other hand, the effects observed in this study, may be due to the connections between the skin's dermatomes.[17]
In the present study, the incidence and the severity of post-operative nausea did not significantly differ in the two groups. Several studies have been conducted to evaluate the effects of acupressure on PONV (although not in post-appendectomy patients). Several studies have used the P6 acupoint[2,4,8,9,18,19,20] and conflicting results have been reported. Two studies have reported that this technique was not effective for nausea and vomiting after cholecystectomy[8] and strabismus correction.[9] However, some of the studies showed that this method has significantly reduced the severity of nausea and vomiting after adeno-tonsillectomy and laparoscopic surgeries.[2,4] while no study on the effects of acupressure on Le7 point is available, the studies that used P6 or other acupoints for PONV have not been reached to a definitive conclusion.
CONCLUSIONS
The present study showed that acupressure on Le7 acupoint was effective on post-appendectomy pain while its effect on PONV did not differ with the control group. It seems that nurses can be trained to use acupressure on Le7 acupoint as a remedy for post-appendectomy pain. However, further investigations are recommended to confirm the results of the present study. In the present study, acupressure was started when the patients recovered from anesthesia and findings showed a considerable reduction in the severity of post-operative pain. However we suggest further studies with starting acupressure at the onset of pain or nausea and vomiting. The results should be interpreted with considering some limitations. First, the number of patients in each group was small. Second, we assessed the patients’ pain, nausea and vomiting only for 7 h. Third, our study was single blinded. Therefore, it is recommended to repeat a larger, double-blind study with longer period of assessment of pain and PONV. Also amount of medication received in each group did not check in the present study. It is suggested that the amount of medication to be controlled in the future studies.
ACKNOWLEDGMENT
This study was part of a M. S. thesis and a research project funded and supported by Deputy of Research, Kashan University of Medical Sciences, Grant No: 9061. The study was also registered at Iranian Registry of Clinical Trials (IRCT) with registration number: IRCT201112118374N1. The authors would like to acknowledge all patients participated in this study. We also acknowledge the authorities in Alzahra Hospital for their supports.
Footnotes
Source of Support: This study is funded by Kashan University of Medical Sciences, Kashan, Iran. The grant number is: 9061
Conflict of Interest: None declared.
REFERENCES
- 1.Ung JW, Lui JC. Postoperative pain management: Study of patients’ level of pain and satisfaction with health care providers’ responsiveness to their reports of pain. Nurs Health Sci. 2003;5:13–21. doi: 10.1046/j.1442-2018.2003.00130.x. [DOI] [PubMed] [Google Scholar]
- 2.Sadri B, Nematollahi M, Shahrami R. The effect of acupressure on the reduction of PONV after adenotonsilectomy. Razi J Med Sci. 2007;13:119–25. [Google Scholar]
- 3.Sakurai M, Suleman MI, Morioka N, Akça O, Sessler DI. Minute sphere acupressure does notreduce postoperative pain or morphine consumption. Anesth Analg. 2003;96:493–7. doi: 10.1097/00000539-200302000-00036. [DOI] [PubMed] [Google Scholar]
- 4.Fan CF, Tanhui E, Joshi S, Trivedi S, Hong Y, Shevde K. Acupressure treatment for prevention of postoperative nausea and vomiting. Anesth Analg. 1997;84:821–5. doi: 10.1097/00000539-199704000-00023. [DOI] [PubMed] [Google Scholar]
- 5.Abtahi D, Ashari A, Lotfi M. Acupressure treatment in postoperative nausea and vomiting prevention. Zahedan J Res Med Sci. 2005;7:205–12. persian. [Google Scholar]
- 6.Goel S. Acupressure guide. London: Diamond Books; 1999. The principles of acupressure techniqe; pp. 17–54. [Google Scholar]
- 7.Weiss-Farnan P. Acupressure. In: Snyder M, Lindquist R, editors. Complementary and alternative therapies in nursing. 6th ed. New York: Springer Publishing; 2010. pp. 287–305. [Google Scholar]
- 8.Samad K, Afshan G, Kamal R. Effect of acupressure on postoperative nausea and vomiting in laparoscopic cholecystectomy. J Pak Med Assoc. 2003;53:68–72. [PubMed] [Google Scholar]
- 9.Lewis IH, Pryn SJ, Reynolds PI, Pandit UA, Wilton NC. Effect of P6 acupressure on postoperative vomiting in children undergoing outpatient strabismus correction. Br J Anaesth. 1991;67:73–8. doi: 10.1093/bja/67.1.73. [DOI] [PubMed] [Google Scholar]
- 10.Alkassi A, Evertson K, Johnsson VA, Ofenbartl L, Kalman S. P6 acupressure may relieve nausea and vomiting after gynecological surgery: An effectiveness study in 410. Can J General Anesth. 2002;49:1034–39. doi: 10.1007/BF03017897. [DOI] [PubMed] [Google Scholar]
- 11.Lee MK, Chang SB, Kang DH. Effects of SP6 acupressure on labor pain and length of delivery time in women during labor. J Altern Complement Med. 2004;10:959–65. doi: 10.1089/acm.2004.10.959. [DOI] [PubMed] [Google Scholar]
- 12.Felhendler D, Lisander B. Pressure on acupoints decreases postoperative pain. Clin J Pain. 1996;12:326–9. doi: 10.1097/00002508-199612000-00012. [DOI] [PubMed] [Google Scholar]
- 13.Alt-Epping S, Ostermann T, Schmidt J, Zirngibl H. Diagnosis of appendicitis with particular consideration of the acupuncture point Lanwei: A prospective study. Forsch Komplementarmed Klass Naturheilkd. 2002;9:338–45. doi: 10.1159/000069233. [DOI] [PubMed] [Google Scholar]
- 14.Manning MV. Management of patients with intestinal and rectal disorders. In: Smeltzer S, Bare BG, Hinkle JL, Cheever KH, editors. Brunner and Suddarth's textbook of medical surgical nursing. 12th ed. Philadelphia: Lippincott; 2009. pp. 1028–1071. [Google Scholar]
- 15.Montazeri S, Pourmehdi Z, Latifi SM, Aghaie M. Evaluation acupressure effect on nausea and vomiting during and after cesarean section under spinal anesthesia in pregnant women referred to Razi hospital. Sci Med J Ahwaz Jundishapur Univ Med Sci. 2004;42:68–76. [Google Scholar]
- 16.Harmon D, Gardiner J, Harrison R, Kelly A. Acupressure and the prevention of nausea and vomiting after laparoscopy. Br J Anaesth. 1999;82:387–90. doi: 10.1093/bja/82.3.387. [DOI] [PubMed] [Google Scholar]
- 17.Cheville A, Caraceni A, Portenoy RK. Pain, definition and assessment. In: Massei MJ, editor. Pain, What psychiatrists to know? Washington DC: American Psychiatric Press Inc; 2000. pp. 1–20. [Google Scholar]
- 18.Wang SM, Kain ZN. P6 acupoint injections are as effective as droperidol in controlling early postoperative nausea and vomiting in children. Anesthesiology. 2002;97:359–66. doi: 10.1097/00000542-200208000-00012. [DOI] [PubMed] [Google Scholar]
- 19.Habib AS, Itchon-Ramos N, Phillips-Bute BG, Gan TJ Duke Women's Anesthesia (DWA) Research Group. Transcutaneous acupoint electrical stimulation with the Relief Band for the prevention of nausea and vomiting during and after cesarean delivery under spinal anesthesia. Anesth Analg. 2006;102:581–4. doi: 10.1213/01.ane.0000189217.19600.5c. [DOI] [PubMed] [Google Scholar]
- 20.Agarwal A, Bose N, Gaur A, Singh U, Gupta MK, Singh D. Acupressure and ondansetron for postoperative nausea and vomiting after laparoscopic cholecystectomy. Can J Anaesth. 2002;49:554–60. doi: 10.1007/BF03017380. [DOI] [PubMed] [Google Scholar]


