Abstract
Background:
Child and adolescent psychiatry has benefited from the application of self-report questionnaires because it is short, less costly and easy to apply. So we select the Strengths and Difficulties Questionnaire (SDQ) and evaluate the agreement between the self-report and parent report form.
Materials and Methods:
Subjects were 1934 Adolescents, 11-18 years old. After obtaining the samples consent, SDQ parent rated form and self-rated form were filled. The collected data were analyzed using the STATA statistical package version 9.
Results:
The adolescents obtained higher total difficulty scores than their parents, but it was not significant (P = 0.203). Boys had higher total difficulty scores than girls by parent informant (P = 0.001), but by self-report girls had higher total difficulty scores than boys (P = 0.42). 11-14 years had higher total difficulty scores by parent report than self-report (P = 0.42), but 15-18 years had higher total difficulty scores by self-report than parent report (P = 0.36).
Conclusion:
SDQ self-rating from adolescents may contribute better to the diagnostic process in the clinical setting.
Keywords: Adolescent, parent, Strengths and Difficulties Questionnaire
INTRODUCTION
Various studies have shown that a considerable percentage of children and adolescents meet the criteria for the emotional or the behavioral disorders.[1,2] Although their problems can create much distress for daily life and well-being, many adolescents with psychiatric disorders receive no professional help, in addition early intervention can prevent the persistence of the disorder into adulthood period.[3]
Evaluation of child psychiatric disturbances is mainly based on the clinical interviews with parents and teachers, assessment of misbehavior with various questionnaires and also on the observation of behavior in a diagnostic setting. For a comprehensive evaluation of such disturbances, it is necessary to draw information from the child or adolescent themselves as a valuable source for describing the patient's feelings, moods and subjective experiences.[4]
For this purpose, structured interviews such as the Kiddie-schedule for affective disorders and schizophrenia interview[5] or National Institute for Mental Health Diagnostic Interview Schedule for Children[6] can be employed. In these assessment instruments, the interview questions are standardized, and thus increase the reliability and allow a better comparison between patients and studies.
Due to the considerable amount of time required as well as the necessary degree of clinical expertise of the interviewer, the structured interviews are of limited importance for primary health- care in a clinical setting.[7] With regard to these problems and limitations, child and adolescent psychiatry has benefited from the development and application of screening questionnaires, which are shorter, less costly and easier to apply.[8]
The Strengths and Difficulties Questionnaire (SDQ) is a brief behavioral screening instrument for these purposes, developed by Goodman.[9,10,11,12] It contains 25 attributes, which concern both positive and negative behavioral traits. The SDQ has the following advantages: It fits easily on one page so it is very short; it is applicable to children and adolescents ranging from 4 to 16 years; the same version can be completed by parents and teachers; a similar version is available for self-report; both strengths and difficulties are well-represented; and there is an equal number of items on each relevant dimension, namely, conduct problems, emotional symptoms, hyperactivity, peer relationships and prosocial behaviors.[9,10]
These properties may enhance the acceptability for respondents and consequently, the response rate and accuracy of the answers.[13]
The SDQ has been translated into more than 40 languages in recent years; therefore, the psychometric properties of the SDQ need to be examined extensively.
The self-report version of the SDQ, like its parent- and teacher-rated counterparts only comprises 25 items and addresses a well-balanced number of positive and negative behavioral aspects. Although the SDQ has been used as a diagnostic instrument since 1997, studies from several countries have already reported psychometric properties of its self-rated version.[14] For the present investigation, we examined the Persian version of SDQ with different informants (parent-report and self-report). The present study comprehensively evaluates how well the information from children and adolescents matches with the judgments by their parents.
MATERIALS AND METHODS
This is a cross-sectional study carried out in Isfahan, Iran in 2011. The population studied comprised children and adolescents aged 11-18 years. The sampling was a random multistage cluster. The sample size was 1293 (644 [50%] boys and 641 [49.9%] girls), 8 were dropped out.
The address of the samples was selected from the family files that are in the Isfahan health center. These addresses were selected from 50 different regions of the city randomly.
The examiner team was composed of two members from the clinical psychologist (one male and one female) who had been trained how to fill in SDQ questionnaire by a child and adolescent psychiatrist. Inter-rater reliability was confirmed after completing questionnaires by the presence of child and adolescent psychiatrist in three consecutive sessions. Sampling protocol and cluster location details were taught to the examiner team members.
They referred to sample's address if the adolescent had a normal IQ according to the judgment of the examiner, after giving explanation to them about the research and obtaining the samples consent, SDQ parent-rated form and SDQ self-report form were filled. There were no exclusion criteria for this study.
SDQ questionnaire is a structured questionnaire to screen psychiatric problems of children and adolescents containing 25 questions and 5 subscales including emotional, hyper activity, peer relationship, conduct problems and prosocial behavior. There were 5 items for each subscale. Each item was given in a score of 0-2 (0 for “not true,” 1 for “somewhat true” and 2 for “certainly true”).[15] The total scores of each subscale were from 0 to 10, classified to three categories (normal-borderline and abnormal). The total difficultly score was calculated by adding the four first subscales ranking from 0 to 40. The cut-off point of SDQ is 17 for children and 20 for adolescents.[16,18,19]
The questionnaire contained three forms as parent-report, teacher-report and self-report. The latter is for children aged over 11 years old.[13] The 25 items cover the same attributes as the parent-rated SDQ. For most items, the only difference is a grammatical change from the 3rd person to the 1st person. The wording of some of the items of the self-report version was modified. The psychometric property of the Persian version of SDQ was made and the reliability and the validity of it were acceptable.[21] The internal reliability testing of the total SDQ showed a Cronbach's alpha of 0.73,[13,18,19] 0.82 (England[11]), 0.78 (Netherlands[19]) and 0.71 (Finland[18]). The internal reliability of the subscales were: (1) Prosocial subscale 0.70; (2) hyperactivity subscale 0.71; (3) emotional subscale 0.70; (4) conduct subscale 0.63; (5) peer problems subscale 0.009.[19,20]
Extended version of SDQ form used in the present study contained impact score, having items about the overall distress and social impairments.[20]
First, it was asked from the parent if the child had any problems in one or more domain of emotion, behavior, concentration and coping with others. Then, if the answer was positive, other questions about distress, social impairment, burden and chronicity were asked and scored within 0-2. If the answer of the 1st question was negative, the other questions would not be asked and the impact score was considered as zero. The scores of the questions on overall distress and social impairment were added up and the impact score was calculated (score of 2 or more was considered abnormal).[11]
The adolescents completed the questionnaire battery while a trained psychologist assisted when help was asked. The participants were informed that all questionnaire responses were confidential.
Statistical methods
Data were analyzed using the STATA statistical package version 9. Descriptive statistics were used to determine the demographic characteristics from the sample. The independent t-test was conducted to determine the statistical differences between mean SDQ score of parent-adolescent reporting behavioral problems. P value less than 0.05 were considered as statistically significant. The study protocol was approved by the Ethic Committee of Isfahan Medical University.
RESULTS
Demographic data was matched at the beginning of the study.
Table 1 shows the means and the standard deviations of the SDQ scores rated by adolescents and parents. These results indicate that the adolescents obtained higher total difficulty scores than their parents, but it was not significant (P = 0.203).
Table 1.
Summarized descriptive and initial analytic statistic of parent-self reporting behavioral problems
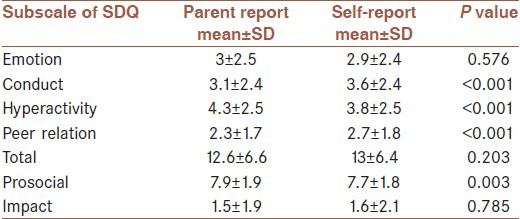
Table 2 shows the means and the standard deviations of the SDQ scores rated by adolescents and parents based on adolescent gender. This table indicates that boys had higher total difficulty scores than girls by parent informant, but by self-report girls had higher total difficulty scores than boys.
Table 2.
Summarized descriptive and initial analytic statistic of parent-adolescent reporting behavioral problems based on child gender
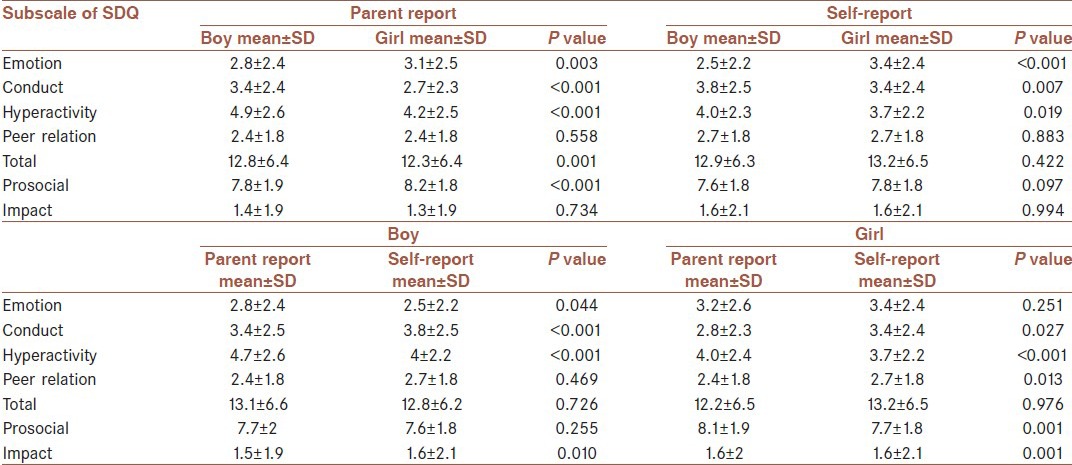
The most significant difference was on the hyperactivity scale for both girls and boys (P < 0.001). The data indicated for parent and self-reports higher means for both boys and girls on hyperactivity symptoms.
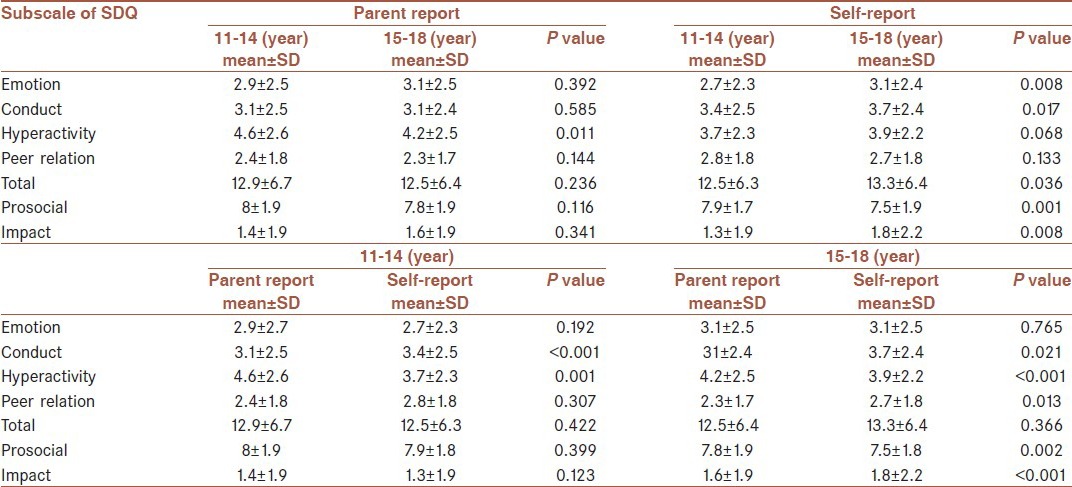
Table 3 shows the means and the standard deviation of the SDQ scores rated by adolescents and parents based on adolescent age. This table indicates that 11-14 years had higher total difficulty scores by parent report than self-report, but 15-18 years had higher total difficulty scores by self-report than parent report.
Table 3.
Summarized descriptive and initial analytic statistic of parent-child reporting behavioral problems based on adolescent age
DISCUSSION
This study confirmed that parents and adolescents provide similar information about adolescents’ mental health in both total difficulty score and the impact report that is the same as the results of other studies.[17,18,21] The mean total difficulty score was greater for adolescents than for parents, but it was not statistically significant (P = 0.203). This might reflect that adolescents may be more sensitive to minor disturbances and report them even if those disturbances are less visible for their parents. It was similar to the results of Goodman and Van Widen-Felt[11,12,13,17] but was higher than the Van Roy and Becker's study.[14]
Goodman's study was based on a population of adolescents aged 11-16 years while the Van Roy and Becker's study included 10-13 years. This supports the findings of other studies suggesting that in community samples, older children have a tendency to agree more with their parents.[22,23,24,27] The means of the SDQ total difficulty scores were somewhat higher in the present study than found in the British studies (boys 11.6, SD 5.4 and girls 11.2, SD 5.0).[9,11]
Although other studies have indicated higher agreement on externalizing problems (hyperactivity and conduct subscales) than on the emotional subscale,[25,26] this was not the case in the current study in which cross informant difference was significant for externalizing problems, but was not significant for emotional problems (similar to Becker's and Koskelainen's study).[14,15]
These findings support that for both externalizing and internalizing problems, characteristics of the behavioral items reported are more relevant in the prediction of parent-adolescent agreement than the type of disorder (e.g., low agreement on the stealing item in the conduct subscale versus higher agreement on the headaches item in the emotional subscale).
In this study, boys reported more problems than girls in all areas except emotional problems. The same pattern was observed in the parents’ reports (similar to Van Roy study[26] and Koskelainen study[15]).
In this study parents reported lower total difficulties with increasing the age of the adolescents conversely, older adolescents scored higher total difficulty by themselves. It means that self-evaluation will be better with increasing age and interview and evaluation of the adolescent separately is very important for diagnose and treatment.
CONCLUSION
The present results demonstrate that SDQ self-rating from adolescents represent a useful contribution to the diagnostic process in Iran the same as some other countries. It is an easily handled and economical instrument as a powerful and reliable tool for a multitude of clinical and research applications. The SDQ might be chosen, when the clinician or the researcher wants to assess the mental health risks in groups of children and adolescents with a brief and not too time-consuming questionnaire. In clinical settings, it might be a good screening instrument in the primary healthcare promoting early identification of a psychiatric disorder, e.g., for a general practitioner, a pediatrician or a nurse was taken to assess, which children are in need of mental health services.
ACKNOWLEDGMENT
This study was carried out as a research grant no 188077 of Research Deputy and ethical committee of Isfahan University of Medical Sciences with close cooperation of Isfahan Behavioral Science Center.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Fergusson DM, Horwood LJ, Lynskey MT. Prevalence and comorbidity of DSM-III-R diagnoses in a birth cohort of 15 year olds. J Am Acad Child Adolesc Psychiatry. 1993;32:1127–34. doi: 10.1097/00004583-199311000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Saunders SM, Resnick MD, Hoberman HM, Blum RW. Formal help-seeking behavior of adolescents identifying themselves as having mental health problems. J Am Acad Child Adolesc Psychiatry. 1994;33:718–28. doi: 10.1097/00004583-199406000-00013. [DOI] [PubMed] [Google Scholar]
- 3.Harrington R, Rutter M, Fombonne E. Developmental pathways in depression: Multiple meanings, antecedents, and endpoints. Devel Psycholopathol. 1996;8:601–16. [Google Scholar]
- 4.Zwaanswijk M, Van der Ende J, Verhaak PF, Bensing JM, Verhulst FC. Factors associated with adolescent mental health service need and utilization. J Am Acad Child Adolesc Psychiatry. 2003;42:692–700. doi: 10.1097/01.CHI.0000046862.56865.B7. [DOI] [PubMed] [Google Scholar]
- 5.Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, et al. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36:980–8. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- 6.Costello AJ, Edelbrock CS, Dulcan MK, Kalas R, Klaric SH. Washington: National Institute of Mental Health, D.C; 1984. Report on the NIMH diagnostic interview schedule for children (DISC) [Google Scholar]
- 7.Hodges K. Structured interviews for assessing children. J Child Psychol Psychiatry. 1993;34:49–68. doi: 10.1111/j.1469-7610.1993.tb00967.x. [DOI] [PubMed] [Google Scholar]
- 8.Fombonne E. The use of questionnaires in child psychiatry research: Measuring their performance and choosing an optimal cut-off. J Child Psychol Psychiatry. 1991;32:677–93. doi: 10.1111/j.1469-7610.1991.tb00343.x. [DOI] [PubMed] [Google Scholar]
- 9.Goodman R. The Strengths and Difficulties Questionnaire: A research note. J Child Psychol Psychiatry. 1997;38:581–6. doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- 10.Goodman R. The extended version of the Strengths and Difficulties Questionnaire as a guide to child psychiatric caseness and consequent burden. J Child Psychol Psychiatry. 1999;40:791–9. [PubMed] [Google Scholar]
- 11.Goodman R, Meltzer H, Bailey V. The Strengths and Difficulties Questionnaire: A pilot study on the validity of the self-report version. Eur Child Adolesc Psychiatry. 1998;7:125–30. doi: 10.1007/s007870050057. [DOI] [PubMed] [Google Scholar]
- 12.Goodman R, Scott S. Comparing the Strengths and Difficulties Questionnaire and the child behavior checklist: Is small beautiful? J Abnorm Child Psychol. 1999;27:17–24. doi: 10.1023/a:1022658222914. [DOI] [PubMed] [Google Scholar]
- 13.Van Widenfelt BM, Goedhart AW, Treffers PD, Goodman R. Dutch version of the Strengths and Difficulties Questionnaire (SDQ) Eur Child Adolesc Psychiatry. 2003;12:281–9. doi: 10.1007/s00787-003-0341-3. [DOI] [PubMed] [Google Scholar]
- 14.Becker A, Hagenberg N, Roessner V, Woerner W, Rothenberger A. Evaluation of the self-reported SDQ in a clinical setting: Do self-reports tell us more than ratings by adult informants? Eur Child Adolesc Psychiatry. 2004;13(Suppl 2):II17–24. doi: 10.1007/s00787-004-2004-4. [DOI] [PubMed] [Google Scholar]
- 15.Koskelainen M, Sourander A, Kaljonen A. The Strengths and Difficulties Questionnaire among Finnish school-aged children and adolescents. Eur Child Adolesc Psychiatry. 2000;9:277–84. doi: 10.1007/s007870070031. [DOI] [PubMed] [Google Scholar]
- 16.Ganizadeh A, Izadpanah A, Abdollahi G. Scale validation of the SDQ in Iranian children. Iran J Psychiatry. 2007;2:65–71. [Google Scholar]
- 17.Goodman R. Psychometric properties of the SDQ. J Am Acad Child Adolesc Psychiatry. 2001;40:1137–45. doi: 10.1097/00004583-200111000-00015. [DOI] [PubMed] [Google Scholar]
- 18.Tehrani-doost M, Shahrivar Z, Pakbaz B, Rezaie A, Ahmadi F. Validity of Persian version of SDQ. Adv Cogn Sci. 2007;8:33–9. [Google Scholar]
- 19.Muris P, Meesters C, van den Berg F. The Strengths and Difficulties Questionnaire (SDQ) – Further evidence for its reliability and validity in a community sample of Dutch children and adolescents. Eur Child Adolesc Psychiatry. 2003;12:1–8. doi: 10.1007/s00787-003-0298-2. [DOI] [PubMed] [Google Scholar]
- 20.Arman S, Keypour M, Maracy MR, Attari A. Epidemiological study of youth mental health using Strengths and Difficulties Questionnaire (SDQ) Iran Red Crescent Med J. 2012;14:371–5. [PMC free article] [PubMed] [Google Scholar]
- 21.Klasen H, Woerner W, Wolke D, Meyer R, Overmeyer S, Kaschnitz W, et al. Comparing the German versions of the Strengths and Difficulties Questionnaire (SDQ-Deu) and the Child Behavior Checklist. Eur Child Adolesc Psychiatry. 2000;9:271–6. doi: 10.1007/s007870070030. [DOI] [PubMed] [Google Scholar]
- 22.Smedje H, Broman JE, Hetta J, von Knorring AL. Psychometric properties of a Swedish version of the “Strengths and Difficulties Questionnaire”. Eur Child Adolesc Psychiatry. 1999;8:63–70. doi: 10.1007/s007870050086. [DOI] [PubMed] [Google Scholar]
- 23.Seiffge-Krenke I, Kollmar F. Discrepancies between mothers’ and fathers’ perceptions of sons’ and daughters’ problem behaviour: A longitudinal analysis of parent-adolescent agreement on internalising and externalising problem behaviour. J Child Psychol Psychiatry. 1998;39:687–97. [PubMed] [Google Scholar]
- 24.Stanger C, Lewis M. Agreement among parents, teachers and children in internalizing and externalizing behaviore problems. J Clinic Child Psychiatry. 1993;33:107–15. [Google Scholar]
- 25.Verhulst FC, van der Ende J. Agreement between parents’ reports and adolescents’ self-reports of problem behavior. J Child Psychol Psychiatry. 1992;33:1011–23. doi: 10.1111/j.1469-7610.1992.tb00922.x. [DOI] [PubMed] [Google Scholar]
- 26.Van Roy B, Grøholt B, Heyerdahl S, Clench-Aas J. Self-reported strengths and difficulties in a large Norwegian population 10-19 years: Age and gender specific results of the extended SDQ-questionnaire. Eur Child Adolesc Psychiatry. 2006;15:189–98. doi: 10.1007/s00787-005-0521-4. [DOI] [PubMed] [Google Scholar]
- 27.Edelbrock C, Costello AJ, Dulcan MK, Conover NC, Kala R. Parent-child agreement on child psychiatric symptoms assessed via structured interview. J Child Psychol Psychiatry. 1986;27:181–90. [PubMed] [Google Scholar]


