Abstract
Orbital solitary fibrous tumor (SFT) is a rare tumor and orbits are a very uncommon site. It is mostly noted to arise from mesenchymal structures like pleura and peritoneum. The diagnosis of orbital SFT cannot be made with certainty on clinical or radiological evaluation alone and requires immunohistochemical studies for confirmation. Orbital SFT's usually show an indolent clinical course and a complete cure can usually be achieved with complete resection. We describe clinical presentations, radiological and operative findings, and pathological features of a patient with orbital SFT along with a brief review of literature.
Keywords: BCL-2, CD34, hemangiopericytoma, solitary fibrous tumor, orbit
INTRODUCTION
Solitary fibrous tumors (SFT) are uncommon spindle cell tumors of mesenchymal origin that most often arises from the pleura but may also occur infrequently in various other sites including lungs, peritoneum, pericardium, kidneys, liver and rarely in the orbit.[1] Mesothelial differentiation as a probable source of its histogenesis has been questioned and replaced by a hypothesis of a fibroblastic differentiation instead.[2] Westra et al.,[3] described the characteristic immunohistochemical features of orbital SFT and found that it shows a strong and diffuse immunoreactivity to CD34. Orbital SFT typically causes slowly progressive and painless proptosis, mostly in the fourth decade (age range, 9-76 years).[4,5,6] The usual clinical course is indolent and complete resection is usually adequate to prevent any recurrences.[7]
CASE REPORT
A 31-year-old man presented at a tertiary care eye hospital in India with complaints of painless but slowly progressive protrusion of the right eyeball with fullness above the lids since the past 6 months. The best corrected visual acuity was 20/20, N6. Hertels at a base of 104 mm showed a proptosis of 4 mm. Ocular movements revealed restricted upgaze in the right eye. Palpation of the superior orbit revealed a well-defined mass that was non-tender, compressible and non-pulsatile in nature. Computed tomography CT scan showed a heterogenous but well defined mass in the right superior orbit with a moderate but progressively increasing contrast enhancement [Figure 1a and b]. The globe, bony orbit and other orbital soft tissues were found to be within normal limits.
Figure 1.
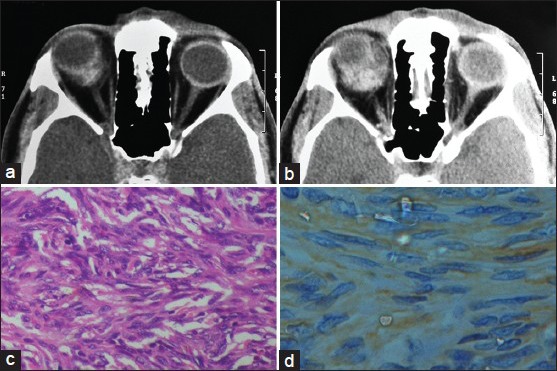
Computed tomography (CT) axial view, showing a small lobulated lesion in the superior orbit (a), which shows an irregular, moderate but progressive enhancement on contrast CT (b), Microphotograph of the tumor showing bundles of spindle cells with vascular channels and interspersed collagen (H and E, ×100) (c), Immunohistochemistry showing a CD99 positivity (d)
A provisional diagnosis of a well-defined, moderate flow vascular lesion was made and a plan to surgically excise the lesion was made. A Benedict's incision was used to approach the superior orbit. The lesion was found to have a capsule around it but was not adherent to the surrounding orbital soft-tissues and thus a cryotherapy assisted complete excision was carried out without much difficulty. The post-operative period was uneventful. Hertel's exophthalmometry confirmed absence of a proptosis and the surgical wound healed well. Last examination was 1-year post-operatively without any evidence of recurrence and the patient is on a follow-up.
Histopathology
Gross examination showed a pinkish mass whose cut section was pinkish-grey with multiple areas of hemorrhage. Microscopic examination showed an encapsulated tumor with cellular and cystic areas. Spindle shaped tumor cells arranged in whorls with minimal atypia, moderate nuclear pleomorphism and inconspicuous nucleoli were noted [Figure 1c]. The tumor showed vessels of varying caliber, dilated to compressed, lined by flattened endothelium [Figure 1c]. However, stag horn channels and giant cells were not noted. Immunohistochemistry showed tumor cells showing a positive staining with CD99 [Figure 1d], strongly positive for CD34 and BCL-2 [Figure 2a] and background positivity for vimentin [Figure 2b]. However, reticulin staining [Figure 2c] and smooth muscle actin (SMA) were negative [Figure 2d]. The morphological and immunohistochemical features were consistent with a diagnosis of orbital SFT.
Figure 2.
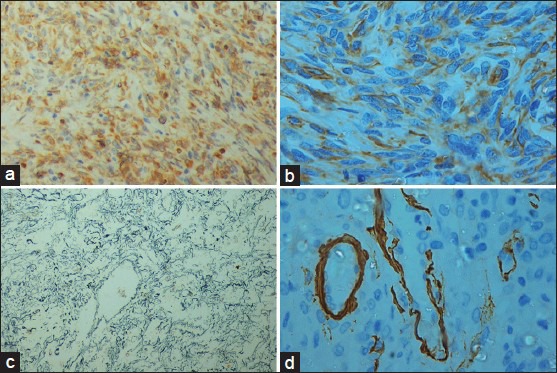
Immunohistochemistry microphotographs showing diffuse and strong positivity with BCL-2 (a), Vimentin positivity (b), Reticulin negativity (c), and smooth muscle actin negativity (d)
DISCUSSION
Orbital SFT most commonly present in middle-aged patients with gradual unilateral progressive proptosis and mass effect, predominantly in the superior part of the orbit, usually unassociated with features of pain or entrapment.[4,6,8] Atypical features reported in the literature include variable progression, visual disturbances, ocular motility restriction, or even a blepharoptosis.[4,6,9] Tumors that recur have been reported to invade surrounding tissues of the orbit as well as paranasal sinuses and intracranial space.[5,10] The major differential diagnosis include hemangioperictyoma, schwannoma, fibrous histiocytoma and optic nerve sheath meningioma.[4,5,6,7,8,9] SFT shares histologic features with other mesenchymal tumors, which is likely to contribute to its misdiagnosis. Imaging modalities are useful adjuncts in diagnosis.[11,12] Ultrasonography shows SFT to have low reflectivity with moderate sound attenuation.[11] A well circumscribed mild to moderate enhancing lesion as noted in our case is a typical CT scan finding.[12] T1-weighted magnetic resonance imaging reveals an intermediate intensity mass and T2 weighted images following gadolinium administration may show mild to moderate enhancement.[12]
A “patternless” growth pattern, where the spindle cells form a random arrangement is a characteristic feature. The cells are often densely arranged with numerous vascular channels that may occasionally form branching or stag horn-like channels.[3,4,5,6,13] The degree of collagen can range from very little to extensive keloid-like fibrosis.[6,13] Histologic features suggestive of aggressive behaviors include high mitotic rate of >4/10 high-power fields, necrosis, hypercellularity, nuclear pleomorphism and high MIB-1 labeling.[14] Advanced immunohistochemical techniques as described above have facilitated a clear distinction for the diagnosis of SFT. The tumor cells are found to have strong and diffuse positivity to CD34, vimentin and BCL-2, non-specific reactivity to CD99 and negativity to desmin, reticulin, cytokeratin, factor VIII related antigen, S-100, SMA and muscle specific actin.[3,4,5,6,7,8,9,10,11,12,13,14,15] In contrast to SFT, hemangiopericytomas which show weak positivity to CD34.[3,4,5,6,7,8,9,10,11,12,13,14,15] In one of the largest studies by Furusato et al.,[15] (n = 41) CD34 positivity was seen in all cases, CD99 in 67.5% and BCL-2 in 47.5% of the cases.
Recurrences and malignant transformation in orbital SFT are uncommon,[4,5,6,9] although Bernardini et al.,[5] reported a recurrence rate of 19% (n = 42). Complete surgical excision should be the goal in these cases although that may not always be possible. In such situations residual tumors may need further surgical excision since there is no conclusive evidence supporting any benefit of adjunctive radiotherapy or chemotherapy.[6,8,9,10] In view of all the above factors, a regular follow-up is ideal in these patients.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Brunnemann RB, Ro JY, Ordonez NG, Mooney J, El-Naggar AK, Ayala AG. Extrapleural solitary fibrous tumor: A clinicopathologic study of 24 cases. Mod Pathol. 1999;12:1034–42. [PubMed] [Google Scholar]
- 2.Hanau CA, Miettinen M. Solitary fibrous tumor: Histological and immunohistochemical spectrum of benign and malignant variants presenting at different sites. Hum Pathol. 1995;26:440–9. doi: 10.1016/0046-8177(95)90147-7. [DOI] [PubMed] [Google Scholar]
- 3.Westra WH, Gerald WL, Rosai J. Solitary fibrous tumor. Consistent CD34 immunoreactivity and occurrence in the orbit. Am J Surg Pathol. 1994;18:992–8. doi: 10.1097/00000478-199410000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Krishnakumar S, Subramanian N, Mohan ER, Mahesh L, Biswas J, Rao NA. Solitary fibrous tumor of the orbit: A clinicopathologic study of six cases with review of the literature. Surv Ophthalmol. 2003;48:544–54. doi: 10.1016/s0039-6257(03)00087-0. [DOI] [PubMed] [Google Scholar]
- 5.Bernardini FP, de Conciliis C, Schneider S, Kersten RC, Kulwin DR. Solitary fibrous tumor of the orbit: Is it rare? Report of a case series and review of the literature. Ophthalmology. 2003;110:1442–8. doi: 10.1016/S0161-6420(03)00459-7. [DOI] [PubMed] [Google Scholar]
- 6.Tam ES, Chen EC, Nijhawan N, Harvey JT, Howarth D, Oestreicher JH. Solitary fibrous tumor of the orbit: A case series. Orbit. 2008;27:426–31. doi: 10.1080/01676830802344508. [DOI] [PubMed] [Google Scholar]
- 7.Ha JK, Park BJ, Kim YH, Lim YJ. Orbital solitary fibrous tumor: A case report and diagnostic clues. J Korean Neurosurg Soc. 2009;46:77–80. doi: 10.3340/jkns.2009.46.1.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Polito E, Tosi GM, Toti P, Schürfeld K, Caporossi A. Orbital solitary fibrous tumor with aggressive behaviour. Three cases and review of the literature. Graefes Arch Clin Exp Ophthalmol. 2002;240:570–4. doi: 10.1007/s00417-002-0486-7. [DOI] [PubMed] [Google Scholar]
- 9.Dorfman DM, To K, Dickersin GR, Rosenberg AE, Pilch BZ. Solitary fibrous tumor of the orbit. Am J Surg Pathol. 1994;18:281–7. doi: 10.1097/00000478-199403000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Young TK, Hardy TG. Solitary fibrous tumor of the orbit with intracranial involvement. Ophthal Plast Reconstr Surg. 2011;27:e74–6. doi: 10.1097/IOP.0b013e3181ed3590. [DOI] [PubMed] [Google Scholar]
- 11.McElvanney AM, Noble JL, O’Donovan DG, Bonshek RE, Banerjee SS. Solitary fibrous tumour: An atypical presentation within the orbit. Eye (Lond) 1996;10:396–9. doi: 10.1038/eye.1996.81. [DOI] [PubMed] [Google Scholar]
- 12.Dalley RW. Fibrous histiocytoma and fibrous tissue tumors of the orbit. Radiol Clin North Am. 1999;37:185–94. doi: 10.1016/s0033-8389(05)70086-5. [DOI] [PubMed] [Google Scholar]
- 13.Char D, Weidner N, Ahn J. Solitary fibrous tumor of the orbit. Orbit. 1997;16:113–8. [Google Scholar]
- 14.Lucci LM, Anderson RL, Harrie RP, Mamalis N, Coffin C, Crandall DC. Solitary fibrous tumor of the orbit in a child. Ophthal Plast Reconstr Surg. 2001;17:369–73. doi: 10.1097/00002341-200109000-00012. [DOI] [PubMed] [Google Scholar]
- 15.Furusato E, Valenzuela IA, Fanburg-Smith JC, Auerbach A, Furusato B, Cameron JD, et al. Orbital solitary fibrous tumor: Encompassing terminology for hemangiopericytoma, giant cell angiofibroma, and fibrous histiocytoma of the orbit: Reappraisal of 41 cases. Hum Pathol. 2011;42:120–8. doi: 10.1016/j.humpath.2010.05.021. [DOI] [PubMed] [Google Scholar]


