Abstract
[Purpose] Cerebral palsy is a sensorimotor disorder that affects the control of posture and movement. The Nintendo® Wii Fit offers an inexpensive, enjoyable, suitable alternative to more complex systems for children with cerebral palsy. The aim of this study was to investigate the efficacacy of Wii-based balance therapy for children with ambulatory cerebral palsy. [Subjects] This pilot study design included fourteen ambulatory patients with cerebral palsy (11 males, 3 females; mean age 12.07 ± 3.36 years). [Methods] Balance functions before and after treatment were evaluated using one leg standing, the functional reach test, the timed up and go test, and the 6-minute walking test. The physiotherapist prescribed the Wii Fit activities,and supervised and supported the patients during the therapy sessions. Exercises were performed in a standardized program 2 times a week for 12 weeks. [Results] Balance ability of every patient improved. Statistically significant improvements were found in all outcome measures after 12 weeks. [Conclusion] The results suggest that the Nintendo® Wii Fit provides a safe, enjoyable, suitable and effective method that can be added to conventional treatments to improve the static balance of patients with cerebral palsy; however, further work is required.
Key words: Cerebral palsy, Balance, Nintendo® Wii Fit
INTRODUCTION
Cerebral palsy (CP) is a neurologic disorder that results from a defect or insult to the immature brain, and it is one of the most common causes of motor disability in childhood. CP describes a group of disorders of movement and posture, causing activity limitation and is attributed to non-progressive disturbances occurring in the developing fetal or infant brain1). Children with CP suffer from motor and cognitive disabilities, which usually require a multi-faceted treatment strategy over many years involving a number of different health professionals2). CP includes the following components: aberrant control of movement and/or posture, early onset, and no recognizable underlying progressive pathology. Disorders of movement and posture are caused by damage to the motor cortex. The consequences of chronic muscle imbalance and the resultant deformities can cause increasing disability with age3, 5). One of the most significant problems for children with CP is defective postural control. Maintaining postural control, required for the performance of activities of daily living, is often a major challenge for children with CP6). Children with CP show affected motor control with an associated pathological gait pattern due to injury to the central nervous system in the developing brain. Poor balance control is known to be an important causative element of the gait problems in these children7, 8). The Nintendo Wii Fit (“Wii Fit”) is a software/hardware game package for the Nintendo® Wii, designed to improve balance and fitness, while providing entertainment9). The Nintendo Wii system has been postulated to be effective at improving functional performance by enhancing flexibility, balance, strength and coordination training. The additional advantage of the Nintendo Wii system is the visual feedback that the participant receives during the training session. This visual feedback aids the participants improv balance, while the game simulation creates a perception that they can perform high level activities10). The Nintendo Wii offers a simple and affordable mode of virtual reality therapy that is being increasingly used to treat children with cerebral palsy, but to date few studies of its efficacy have been published. Therefore the aim of the current study was to investigate the effects of Wii-based balance therapy on balance and walking function of patients with CP.
SUBJECTS AND METHODS
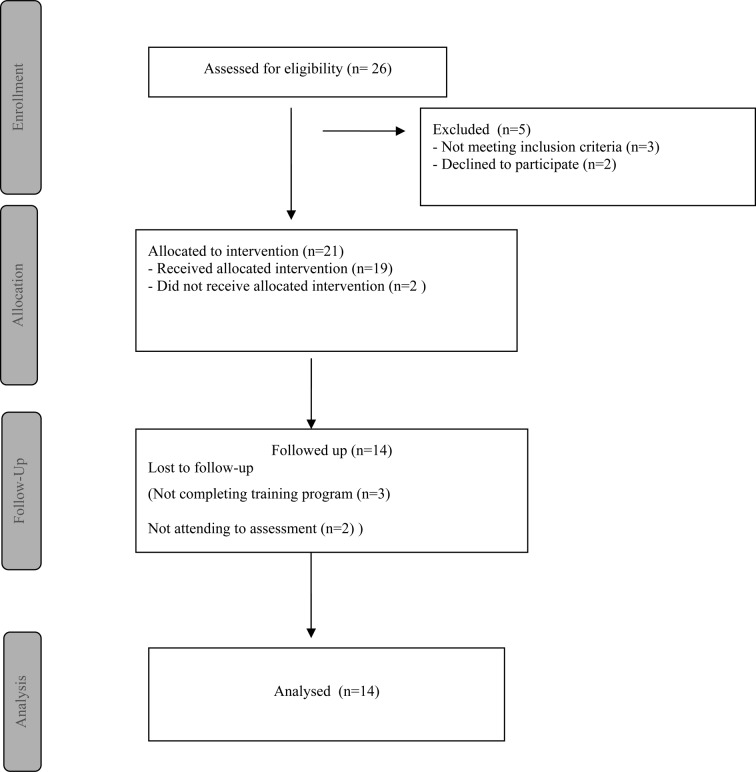
Fourteen patients with CP (3 girls, 11 boys) with an age range of 5–17 participated in this study (Fig. 1). The enrollment period was between December 2011 and June 2012. The patients were recruited from the pediatric neurology outpatient clinic of the Department of Pediatric Neurology, Faculty of Medicine, Istanbul University, and were diagnosed with CP. Participants had normal or mild level intellectual disability according to their health records. Exclusion criteria were the presence of epilepsy, Gross Motor Function Classification System Expanded and Revised (GMFMCS-ER) level 4 or 5, spasticity of 3 or more according to Modified Ashworth Scale in the lower extremities, and inability to cooperate with exercise or measurement. All patients and their parents were informed about the study, and written informed consent was obtained from the parents of the patients. The study was approved by the Ethics Committee of Istanbul University and was conducted in accordance with the Decleration of Helsinki. A demographic data form was filled in by a physiotherapist. Patients' weight and height were measured and body mass index (BMI) was calculated as the weight divided by the square of the height. Clinical features such as disease duration, and the subtype of CP were assessed by a pediatric neurologist.
Fig. 1.
Progress of study participants
The Gross Motor Function Classification for CP (GMFCS) is a five-level classification. In short, class 1 means that the child is freely ambulatory, class 2 means inability to run or jump, class 3 means dependency on devices for walking, and classes 4 and 5 mean non-ambulatory CP11). The GMFMCS-ER was developed using the 12-to18 year age band, on the basis of the concept that performance of gross motor function is influenced by physical, social, and attitudinal environment and personal factors such as preferences, interests, and motivation in 200712). The gross motor level of children with CP was assessed using the GMFMCS-ER in our present study.
The one leg standing test is a commonly used balance assessment of postural stability among physiotherapist and occupational therapists. Patients are given specific instructions to stand on one leg for as long as possible in one of two conditions, with the eyes open or eyes closed. Times are then recorded for the duration that the position was held13, 14). The one leg standing test is considered to be potentially useful for predicting functional decline, and has been shown to be sensitive to clinical interventions15). We used only the one leg standing with eyes open in present study. The Timed Up and Go test (TUG) was designed to measure speed during functional tasks that potentially threaten balance16). Balance in basic mobility manoeuvres is tested with the TUG. The participants sat on a standard armchair and were instructed to get up and walk at a comfortable and safe pace to a line on the floor 3 metres away, turn around, return to the chair and sit down again. The time required to complete the task was recorded. One practice session was performed once before the actual test.
The functional reach test (FRT) was developed as a measure of the margin of stability. The FRT has been used to describe and monitor an individual's balance and to screen for or predict an individual who is at risk of falling. The FRT is an easily administered performance-based measure. The test consists of measuring the distance that an individual can reach forward without moving his or her feet. The score is the distance that the person can reach. Variations of the test, having individuals reach in different directions, have been suggested17).
The 6-minute walking test has been used as a measure of the functional status of patients. The test was performed on an 8-meter track in a straight corridor as described in the literature. Patients were instructed to cover the largest possible distance in 6 minutes at a self-chosen walking speed. Turns were made on both ends of the 8-meter track. The distance walked was recorded with a lap counter. Each time the patient returned to the starting line, the lap counter was clicked once. Every minute the patients were encouraged in a standardized way, and time, recorded with a stopwatch, was called every minute18).
Nintendo Wii Fit balance evaluation and treatment were performed in a darkened room. Nintendo Wii Fit image projection was reflected on the wall. The patients' demographic information were recorded in the system, and the right and left foot as a percent of the total weight on the balance board was registered by the system. The time of one-leg standing was also recorded by the device. Then Wii Fit age was calculated by the device. If the Wii age of the person is greater than their actual age, it shows inability in exercise and balance.
A physiotherapist prescribed the Wii Fit activities, and supervised and supported the patients during the therapy sessions. Wii training was performed in a standardized program, 2 times a week for 12 weeks, with sessions lasting approximately 40 minutes. The exercise program included balance exercises on the Wii balance board. The training program was updated to higher levels of games every 4 weeks. In each session, the patients played the four games of the system. A brief explanation of the purpose of each one of these games can be found in Table 1. All the participants were assessed before and after the training program by a physiotherapist.
Table 1. Outline of Wii-Fit exercise program.
| Parameter | Description |
| Ski Slalom | Ski Slalom elicits a lower limb balance strategy and improves loading of the lower extremities |
| Soccer heading | This game improves movements of the trunk and extremities in a large spectrum of balance perturbations that vary in both amplitude and location of the destabilizing force. |
| Tilt Table | Tilt table elicits control over the whole body through dynamic balance training on a virtual balance board. |
| Walking a tightrope | Walking on the tightrope improves dynamic balance and trunk control through right and left transfer of body weight. |
| Repetition | Each game was played 3 times in 1 set |
| Duration | 40 minute |
| Frequency | 2 days/week for 12 weeks |
The data were evaluated using the Statistical Package for Social Science (SPSS) v.17.0 software for Windows and by analysing descriptive statistics (frequency, mean, and standard deviation (SD). The Mann-Whitney U Test was used to determine the effects of the exercise program. A significance level of 0.05 was used.
RESULTS
A total of 26 eligible patients with CP were included in this study. Twelve patients left the study and 14 patients completed our study. The patient population comprised 7 diplegic type CP, 5 patients with hemiplegic type CP, and 2 patients with dyskinetic type CP. The demographic and clinical features of the patients are shown in Table 2. Their mean age was 12.07 years (SD 3.36, range 11–16 years) . The median score of the GMFMCS-ER was 2 (range 1–3). Table 3 shows the levels of the GMFMCS-ER and Modified Ashworth Scale scores of all the participants. The changes in outcome measures at the end of training program for one leg standing time, the timed up and go test, the functional reach test, the 6- minute walking test and Wii Fit parameters are shown in Table 4. At the end of training program the Wii game score changes are shown in Table 5. Statistically significant improvements (p<0.05) were found in all the outcome measures, Wii Fit parameters and Wii game scores of the participants after 12 weeks.
Table2. The demographic and clinical features of the patients.
| Age (years) (mean(SD)) | 12.07 (3.36) |
| BMI (kg/m2) (mean(SD)) | 18.58 (3.84) |
| Sex (F/M) (n) | 3/11 |
| CP subtype (n) | |
| diplegic CP | 7 |
| hemiplegic CP | 5 |
| dyskinetic CP | 2 |
| GMFMCS-ER (median score- range) | 2 (range 1–3) |
SD: standard deviation, BMI: body mass index, F: female, M: male, CP: cerebral palsy, GMFMCS-ER: Gross motor function classification system expanded and revised
Table 3. The level of GMFMCS-ER and Modified Ashworth Scale of all participants.
| Patients | GMFMCS-ER | MAS | |||||
| Level | (Hip Flex.R) | (Hip Flex L) | (HMS R) | (HMS L) | (GCS R) | (GCS L) | |
| 1 | II | 1+ | 1+ | 2 | 1+ | 1+ | 1+ |
| 2 | II | 1 | 1 | 1 | 1 | 1+ | 1+ |
| 3 | I | 1+ | 0 | 1 | 0 | 1+ | 0 |
| 4 | I | 1+ | 0 | 1+ | 0 | 1+ | 0 |
| 5 | I | 0 | 1 | 0 | 1 | 0 | 1 |
| 6 | II | 1+ | 1+ | 1+ | 1+ | 1+ | 1+ |
| 7 | II | 1+ | 1+ | 1+ | 1+ | 1+ | 1+ |
| 8 | II | 0 | 1+ | 0 | 2 | 0 | 1+ |
| 9 | II | 1+ | 1+ | 1+ | 1+ | 1+ | 1+ |
| 10 | II | 1+ | 1+ | 1+ | 1+ | 1+ | 1+ |
| 11 | II | 1 | 1 | 1 | 1 | 1 | 1 |
| 12 | I | 0 | 1 | 0 | 1 | 0 | 1+ |
| 13 | II | 1 | 1 | 1 | 1+ | 1 | 2 |
| 14 | III | 1 | 2 | 1 | 2 | 1 | 2 |
GMFMCS-ER: Gross motor function classification system expanded and revised., MAS: Modified Ashworth Scale, Flex: Flexion, R: Right, L: Left, HMS: Hamstring, GCS: Gastrocnemius
Table 4. The changes in outcome measures.
| Outcome measures | Pre-treatment Mean (SD) | Post-treatment Mean (SD) |
| One Leg Standing Test-R (sec) | 6.60 (8.95) | 7 (7.99)* |
| One Leg Standing Test-L (sec) | 5.41 (6.43) | 8.50 (9.36)* |
| Timed Up and Go Test (sec) | 18.26 (4.22) | 14.57 (5.39)* |
| Functional reach test (cm) | 20.78 (9.09) | 22.5 (10.75)* |
| 6-Minute Walking Test (m) | 312.71 (95.20) | 333.42 (89.66)* |
| Wii Fit parameters | ||
| One Leg Standing Test-L (sec) | 5.34 (4.59) | 10.37 (2.07)* |
| Left Foot Stability (score) | 5 (2.76) | 18.35 (12.32)* |
| Wii age | 44.64 (5.59) | 38.42 (14.65)* |
SD: Standard deviation, sec: second, cm: centimeter. *Significantly different from pre-treatment p<0.05
Table 5. The changes in Wii game scores.
| Outcome measures | Pre-treatment Mean (SD) | Post-treatment Mean (SD) |
| Ski Slalom (error score) | 11.21 (3.23) | 5.14 (3.48)* |
| Soccer heading (score) | 17.71 (9.60) | 55.07 (37.93)* |
| Tilt Table (score) | 11.42 (12.92) | 48.42 (29.29)* |
| Walking a tightrope (meter) | 2.30 (1.37) | 3.24 (1.49)* |
SD: Standard deviation, *Significantly different from pre-treatment to post-treatment p<0.05
DISCUSSION
The results of our study show that CP patients participating in a 12-week Wii Fit training program showed improved balance function and walking. Functional balance, which is an element of postural control, allows a child to perform activities of daily living (ADL), social activities, and recreational activities at home, school, and in the community. Motor disorders are often accompanied by poor balance control in patients with CP. Children with CP may have impaired postural balance that contributes to their gait abnormalities19). Therefore, the main focus of this study was to improved balance parameters and functional walking. Our study showed significant improvements in balance parameters of CP patients after the Wii-based balance therapy. Health care professionals have begun to use interactive gaming systems and technology to help rehabilitate patients with musculoskeletal and neurologic conditions. The growing popularity of interactive gaming is partially due to the belief that playing interactive video games during a rehabilitation session can direct a patient's focus away from the repetitive and mundane nature of rehabilitation exercises and toward the fun and competitive aspects of the video game20). The literature include some d studies of interactive games, especially Wii Fit games, in different neurological diseases and geriatrics21, 22). However in the literature, we found only a few trials demonstrating the benefits of Wii-based training for CP patients. Deutsch et al.23) demonstrated that Wii games improved visual perception, posture and functional mobility with Wii games in a case study with spastic diplegic CP. Unlike our study, Ramstrand et al.24) recruited eighteen children with hemiplegic or diplegic CP. The patients completed Wii fit training at home over five weeks. Their results suggest that use of a Nintendo Wii balance board and Wii Fit software for a minimum of thirty minutes per day in the patient's own home, over a five week period, is not effective as a balance training tool for children with CP. Jelsma et al.25) included 14 children with spastic hemiplegic cerebral palsy in their study. Nintendo Wii Fit training in lieu of regular physiotherapy was given for 3 weeks. Outcome measures included modified balance score running speed, and agility scales of the Bruininks-Oserestky test of Motor Performance, and the timed ascent and descent of stairs. Their study showed balance scores improved significantly but Nintendo Wii Fit training should not be used in place of conventional therapy, and further research is needed into its use as an adjunct to therapy. Nintendo Wii includes a lot of games. We aimed to improve the balance of children with CP in this study. For this reason, we used the ski slalom, soccer heading, tilt table and walking a tightrope games to attempt to improve their balance. Michalski et al.26) evaluated postural control strategies healthy individuals use to play Wii Fit videogames. Sixteen young adults played 10 trials of ski slalom and soccer heading respectively. Centre of pressure (COP) excursion and three-dimensional movement data were acquired to determine variability in medial–lateral COP sway and shoulder–pelvic movement. While there was no difference in medial–lateral COP variability between games during trial 1, there was a significant difference after 10 trials.
Our study found improvements in the FRT, TUG, and the 6- minute walking test. The interventions chosen to improve gait were ski slalom, soccer heading, tilt table and walking a tightrope games. The games improved movements of the trunk and extremities through a large spectrum of balance perturbations that vary in both amplitude and location of the destabilizing force. At the same time these games improve dynamic balance and trunk control through right and left transfer of body weight. Therefore scores improved in FRT, TUG, and the 6-minute walking test.
There were two limitations to our study. First, we did not have homogeneous sub-groups of CP patients. Second, it was a small sample size from only one clinic. This study is important for the spread of Wii Fit use in the rehabilitation of cerebral palsy in our country. Therapists working in this area will provide a different perspective.
In conclusion, this study demonstrated that Wii based balance training has the potential to improve the balance and functional walking of patients with CP. This Wii-based training is more fun and provides motivation, and may be a preferable method of treatment for children with CP. Further research is needed to develop evidence-based guidelines for Wii-based balance therapy in CP.
REFERENCES
- 1.Bax M, Goldstein M, Rosenbaum P, et al. : Executive committee for the definition of cerebral palsy. Proposed definition and classification of cerebral palsy. Dev Med Child Neurol, 2005, 47: 571–576 [DOI] [PubMed] [Google Scholar]
- 2.Numthavaj P, Kliim-Due M, Rasmussen B, et al. : Individualized, home-based interactive training of cerebral palsy children delivered through the Internet. BMC Neurol, 2011, 11: 1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Taylor JR, Kopriva PG: Cerebral palsy. In. Medical, Psychosocial, and Vocational Aspects of Disability. Athens: Elliott Fitzpatrick Press, 2002, pp 387–400. [Google Scholar]
- 4.Benda W, McGibbon NH, Grant KL: Improvements in muscle symmetry in children with cerebral palsy after equine-assisted therapy (hippotherapy). J Altern Complement Med, 2003, 9: 817–825 [DOI] [PubMed] [Google Scholar]
- 5.Massion J, Alexandrov A, Frolov A: Why and how are posture and movement coordinated? Prog Brain Res, 2004, 143: 13–27 [DOI] [PubMed] [Google Scholar]
- 6.van der Heide JC, Begeer C, Fock JM, et al. : Postural control during reaching in preterm children with cerebral palsy. Dev Med Child Neurol, 2004, 46: 253–266 [DOI] [PubMed] [Google Scholar]
- 7.Dabney KW, Lipton GE, Miller F: Cerebral palsy. Curr Opin Pediatr, 1997, 9: 81–88 [DOI] [PubMed] [Google Scholar]
- 8.Woollacott MH, Shumway CA: Postural dysfunction during standing and walking in children with cerebral palsy: what are the underlying problems and what new therapies might improve balance? Neural Plast, 2005, 12: 211–219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Williams MA, Soiza LR, Jenkinson AM, et al. : Exercising with Computers in Later Life (EXCELL) − pilot and feasibility study of the acceptability of the Nintendo® Wii Fit in community-dwelling fallers. BMC Res Notes, 2010, 3: 238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kwok BC, Mamun K, Chandran M, et al. : Evaluation of the Frails' Fall Efficacy by Comparing Treatments (EFFECT) on reducing fall and fear of fall in, moderately frail older adults: study protocol for a randomised control trial. Trials, 2011, 12: 155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Palisano R, Rosenbaum P, Walter S, et al. : Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol, 1997, 39: 214–223 [DOI] [PubMed] [Google Scholar]
- 12.Can Child Centre for Childhood Disability Research: http://motorgrowth.canchild.ca/en/GMFCS/resources/GMFCS-ER.pdf (Accessed, 2007).
- 13.Atwater SW, Crowe TK, Deitz JC, et al. : Interrater and test-retest reliability of two pediatric balance tests. Phys Ther, 1990, 70: 79–87 [DOI] [PubMed] [Google Scholar]
- 14.Drusini AG, Eleazer GP, Caiazzo M, et al. : One-leg standing balance and functional status in an elderly community-dwelling population in northeast Italy. Aging Clin Exp Res, 2002, 14: 42–46 [DOI] [PubMed] [Google Scholar]
- 15.Shimada H, Uchiyama Y, Kakurai S: Specific effects of balance and gait exercises on physical function among the frail elderly. Clin Rehabil, 2003, 17: 472–479 [DOI] [PubMed] [Google Scholar]
- 16.Podsiadlo D, Richardson S: The Timed “Up & Go”: a test of basic functional mobility for the frail elderly persons. J Am Geriatr Soc, 1991, 39: 142–148 [DOI] [PubMed] [Google Scholar]
- 17.Katz-Leurer M, Rotem H, Keren O, et al. : Balance abilities and gait characteristics in post-traumatic brain injury, cerebral palsy and typically developed children. Dev Neurorehabil, 2009, 12: 100–105 [DOI] [PubMed] [Google Scholar]
- 18.ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories: ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med, 2002, 166: 111–117 [DOI] [PubMed] [Google Scholar]
- 19.Chen CL, Shen IH, Chen CY, et al. : Validity, responsiveness, minimal detectable change, and minimal clinically important change of Pediatric Balance Scale in children with cerebral palsy. Res Dev Disabil, 2013, 34: 916–922 [DOI] [PubMed] [Google Scholar]
- 20.González-Fernández M, Gil-Gómez JA, Alcañiz M, et al. : eBaViR, easy balance virtual rehabilitation system: a study with patients. Annu Rev Cybertherapy Telemed, 2010, 8: 49–53 [PubMed] [Google Scholar]
- 21.Franco JR, Jacobs K, Inzerillo C, et al. : The effect of the Nintendo Wii Fit and exercise in improving balance and quality of life in community dwelling elders. Technol Health Care, 2012, 20: 95–115 [DOI] [PubMed] [Google Scholar]
- 22.Pompeu JE, Mendes FA, Silva KG, et al. : Effect of Nintendo Wii™-based motor and cognitive training on activities of daily living in patients with Parkinson's disease: a randomised clinical trial. Physiotherapy, 2012, 98: 196–204 [DOI] [PubMed] [Google Scholar]
- 23.Deutsch JE, Borbely M, Filler J, et al. : Use of a low-cost, commercially available gaming console (Wii) for rehabilitation of an adolescent with cerebral palsy. Phys Ther, 2008, 88: 1196–1207 [DOI] [PubMed] [Google Scholar]
- 24.Ramstrand N, Lygnegård F: Can balance in children with cerebral palsy improve through use of an activity promoting computer game? Technol Health Care, 2012, 20: 501–510 [DOI] [PubMed] [Google Scholar]
- 25.Jelsma J, Pronk M, Ferguson G, et al. : The effect of the Nintendo Wii Fit on balance control and gross motor unction of children with spastic hemiplegic cerebral palsy. Dev Neurorehabil, 2013, 16: 27–37 [DOI] [PubMed] [Google Scholar]
- 26.Michalski A, Glazebrook CM, Martin AJ, et al. : Assessment of the postural control strategies used to play two Wii Fit™ videogames. Gait Posture, 2012, 36: 449–453 [DOI] [PubMed] [Google Scholar]