Abstract
OBJECTIVE:
Describe the major discrepancies between the clinical and postmortem findings in critically ill cancer patients admitted to the medical intensive care unit (MICU).
MATERIALS AND METHODS:
Retrospectively review of the medical records of all cancer patients who were admitted to the MICU and underwent postmortem examination over 6 year period. The records were reviewed for demographics, Acute Physiology and Chronic Health Evaluation (APACHE) II score, clinical cause of death, and postmortem findings.
RESULTS:
There were 70 patients who had complete medical records. Mean age was 54.7 years (standard deviation (SD) ±14.8 years). Twenty-six patients had hematopoeitic stem cell transplantation (group I), 21 patients had hematological malignancies (group II), and 23 patients had solid malignancies (group III). The APACHE II score on admission to the MICU was 24.2 ± 8.0. Sixty-seven patients were mechanically ventilated, and the MICU stay was (mean ± SD) 9.0 ± 11.6 days. Major discrepancies between the clinical and postmortem diagnoses (Goldman classes I and II) were detected in 15 patients (21%). The most common missed diagnoses were aspergillosis, pulmonary embolism, and cancer recurrence. There were no differences between groups regarding the rate of major discrepancies.
CONCLUSION:
Despite the advances in the diagnosis and treatment of critically ill cancer patients, autopsies continue to show major discrepancies between the clinical and postmortem diagnoses. Autopsy is still useful in this patient population.
Keywords: Autopsy, cancer, critical care
INTRODUCTION
The advances in the management of cancer and the reported improved outcome of critically ill cancer patients have led to more patients being admitted to the intensive care units (ICUs).[1] The spectrum of illnesses that affect these critically ill patients is wide and is due to the underlying malignancy, its treatment, unrelated conditions, or a combination of the above. Also not infrequently many of these conditions have atypical presentations in these critically ill patients. In spite of the advance in diagnostic techniques, major diagnoses may be missed in the critically ill cancer patients. Autopsies have been shown to yield significant discrepancies between the clinical diagnosis and postmortem diagnosis in hospitalized patients in general and in the critically ill.[2–14] There are very few studies that specifically describe the value of autopsy in the critically ill cancer patients.[15–17] The aim of this study is to identify the major discrepancies between clinical and postmortem diagnoses in a cohort of critically ill cancer patients.
MATERIALS AND METHODS
This study was conducted at Wayne State University affiliated medical center in Detroit, Michigan. The medical center consists of tertiary care teaching hospitals and a comprehensive cancer center. The criteria for admission to and discharge from the medical ICU (MICU) follow the guidelines set by the American College of Critical Care Medicine and Society of Critical Care Medicine.[18] The MICU is managed by full-time faculty members of the Pulmonary and Critical Care Division. Medical oncologists also conducted daily rounds on oncology patients in the MICU. Permission for autopsy is usually sought in all MICU deaths. Autopsies are usually performed within 24 h of death.
The study was approved by the institutional review board (IRB). It consisted of a retrospective review of critically ill patients who died in the MICU, and had a primary diagnosis of malignancy, and underwent autopsy. The patients were identified by reviewing the Pathology Department autopsy records over 6 year period. The medical records of those patients who had malignancy as their primary underlying disease were reviewed in detail. The review included demographic data, underlying malignancy, Acute Physiology and Chronic Health Evaluation (APACHE) II score on admission to the ICU, the need for mechanical ventilation, and length of stay in the ICU. The patients were classified into three groups based on their underlying malignancy (group I had hematopoietic stem cell transplantation (HSCT), group II had hematological malignancy, and group III had solid cancer). The investigators extracted from the medical record the main clinical cause of death and also documented the major autopsy findings from the final autopsy report on each of these patients. The discrepancies between the premortem clinical and the post mortem autopsy diagnoses were classified according to the Goldman criteria.[19] For purposes of this study, we focused on the class I and class II major discrepancies. Class I is a major missed diagnosis with potential adverse impact on survival and that would have changed management. Class II is a major missed diagnosis with no potential impact on survival and that would have not changed therapy. Three of the investigators (all clinicians) independently determined the presence and degree of discrepancy between the clinical and postmortem diagnoses. A consensus was reached if there were differences between the investigators.
RESULTS
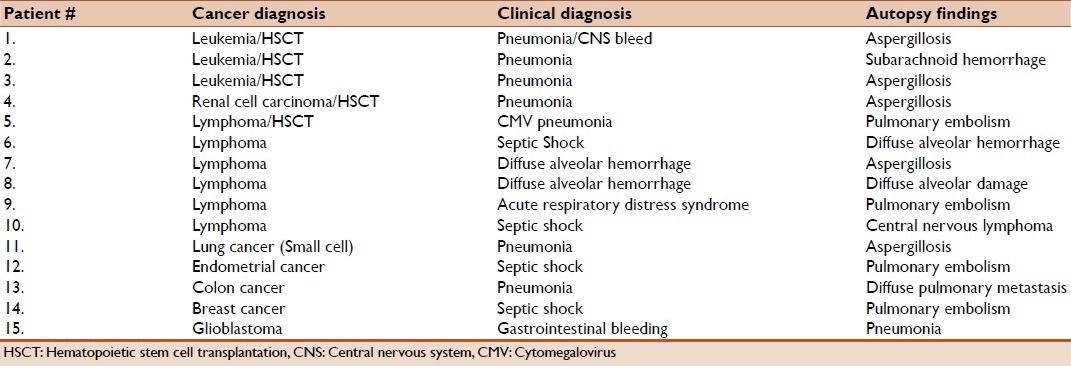
During the study period, there were 70 patients who had cancer as their primary diagnosis who died in the MICU and had autopsies and complete medical records (seven additional patients did not have complete medical records and were excluded from the study). The baseline clinical characteristics of these patients are summarized in Table 1. Twenty-six patients were HSCT recipients (all had allogeneic HSCT) (group I), 21 patients had hematological malignancies (group II), and 23 patients has solid tumors (group III). Fifteen patients had major discrepancies between the premortem and postmortem diagnoses: Goldman class I (nine patients) and class II (six patients). There were no significant differences between the different groups of cancer patients in the number of major discrepancies (six out of 26 in the HSCT group, four out of 21 in the hematological malignancy group, and five out of 23 in the solid tumors group. The major missed diagnoses are described in Table 2. The main missed diagnosis in these critically ill patients was invasive aspergillosis in five patients (three in HSCT recipients, one with hematological malignancy, and one with solid cancer). Pulmonary embolism was the second major missed diagnosis in these patients (four patients: One patient with HSCT, one patient with hematological malignancy, and two patients with solid cancer). Recurrence of cancer was the third major missed diagnosis in two patients (one patient with hematological malignancy and one patient with solid cancer). Table 3 details the primary clinical premortem diagnosis and the primary postmortem diagnosis in these patients who had major discrepancies.
Table 1.
Patient characteristics for different patient groups
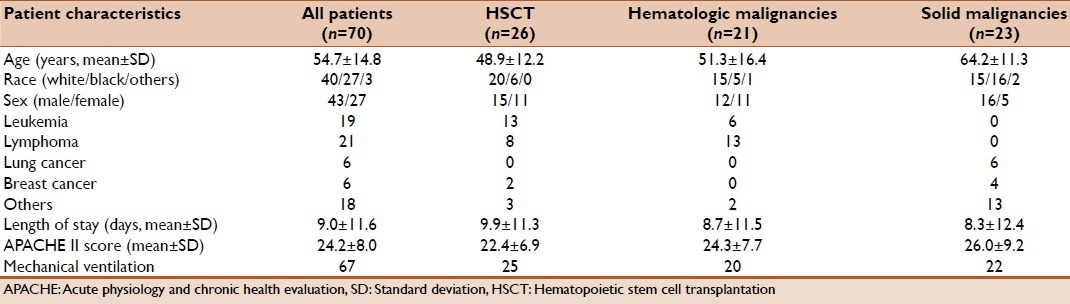
Table 2.
Goldman class I and II discrepancies in various subgroups
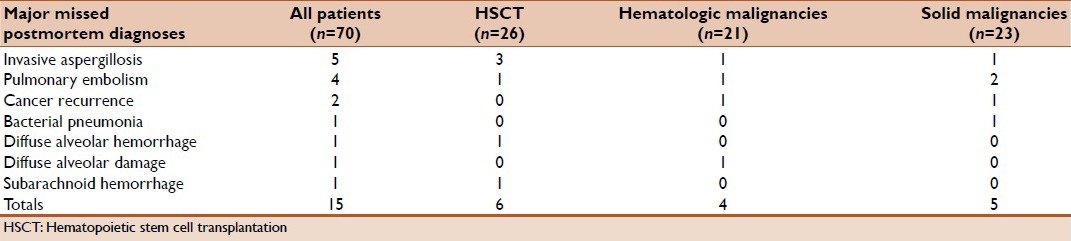
Table 3.
Characteristics of patients in various sub groups with major discrepancies
DISCUSSION
The study describes that there are major discrepancies between the clinical diagnosis and postmortem diagnosis in 21% of critically ill cancer patients in whom autopsies were performed. Furthermore, the study indicates that the primary missed diagnoses were aspergillosis, pulmonary embolism, and recurrent cancer. There were no differences in the rates of major discrepancies between the patients whether they had HSCT or hematological malignancies or solid tumors.
The discrepancy rate in this study is within the range that was reported in autopsies performed on critically ill patients in general.[2–14] There were only few reports that describe the discrepancies between the clinical and postmortem diagnosis in critically ill cancer patients. In the study by Gerain et al., major discrepancies were found in 59% of patients.[15] The majority of these discrepancies were related to cancer itself or its treatment. In another study on critically ill HSCT recipients, the discrepancy rate was 36%.[16] A more recent study by Pastores et al., the major discrepancy rate in critically ill cancer patients was 26%.[17] The main missed diagnoses were opportunistic infections (15%), followed by cardiac complications (8%). The current study shows a similar discrepancy rate and emphasizes that aspergillosis and pulmonary embolism were the main missed diagnoses in this patient population. The relatively high rate of discrepancies reported in this study and other similar studies reflect the fact that these are critically ill cancer patients, including significant number of patients with HSCT or hematological malignancies. These patients have most complicated clinical course and pose a particular challenge to clinicians. Furthermore, coagulopathy and organ dysfunction that are typical of these patients limit the extent of diagnostic studies they can undergo. Change to palliative care in patients with advanced cancer may be another limiting factor to reaching a definitive diagnosis. Consequently, the discrepancy rate in these patients should not be taken as representative of all critically ill patients or suggestive of poor clinical judgment.
Invasive aspergillosis remains a major problem in critically ill cancer patients, especially those with HSCT, solid organ transplantation, or neutropenia. There are also recent reports that suggest an increased incidence of invasive aspergillosis in other critically ill patients without the classic risk factors.[20] In spite of the increased awareness about the importance of this opportunistic infection, it remains the main missed diagnosis in this study of critically ill cancer patients. This reflects the nonspecific presentation of this infection, and the difficulty in confirming the diagnosis in critically ill patients, which usually requires invasive procedures. Most of the patients reported in this study were before the introduction to clinical practice noninvasive diagnostic tests such as measuring galactomannan in the serum and other body fluids which has been shown to be an important tool in the diagnosis of invasive aspergillosis in HSCT recipients and patients with hematological malignancies.[21] Also some studies suggested that measuring galactomannan from bronchoalveolar lavage fluid correlated with the diagnosis of invasive pulmonary aspergillosis in critically ill patients.[22] The recent introduction of antifungal agents that are better tolerated have increased the use of these agents for prophylaxis and empiric therapy in critically ill patients at an increased risk of invasive aspergillosis. Further studies will be needed to know whether these factors may decrease the rate of missed invasive aspergillosis in the critically ill cancer patients.
The study also emphasizes the importance of thromboembolic disease in critically ill cancer patients. It accounted for 27% of major missed diagnoses. Cancer patients, especially those who are critically ill, are at an increased risk for thromboembolic disease and every effort should be made to maintain them on prophylactic measures. However, critically ill cancer patients are more likely to have conditions that may decrease the use of anticoagulant prophylactic measures such as thrombocytopenia, coagulopathy, and the concern about heparin induced thrombocytopenia. There is no evidence that prophylactic measures increase the risk of bleeding in patients with coagulopathy or thrombocytopenia. Newer anticoagulants such as low molecular dose heparin, fondaparinux and argatroban may be more effective and avoid some of the complications associated with prophylaxis against thromboembolic disease.[23] Also the routine incorporation of management bundles such as ventilator bundle and electronic medical records may improve compliance with patient safety measures including prophylaxis against thromboembolic disease.
This study and most of the previous studies were not able to provide variables that may predict the likelihood of missed major diagnoses in the critically ill cancer patients. Some studies on critically ill patients suggested that likelihood of missed diagnoses is higher with longer ICU stay.[4]
The rate of autopsies has steadily decreased in the last few decades. Some of the reasons that have been reported to explain the decrease in the rate of autopsy in general include the advances in diagnostic methods, the concern about medicolegal implications, increased work load for the pathologists, high cost and low reimbursement, and the perception of family members and physicians that the cause of death is usually related to the underlying malignancy and that autopsy is unlikely to lead to additional information. Also, patients who die in the ICU are likely to be cared for by the intensivist who is usually not the primary physician who had long-term relation with the patient and family.[17,24] This study shows that in spite of significant advances in the diagnosis and management of critically ill patients in general, there remains significantly high rate of major discrepancies between clinical and postmortem diagnoses. This underscores the significance of autopsy in the care of these patients. We recommend that intensivists continue to ask for autopsy in critically ill cancer patients since the information is likely to be useful in directing future care and planning in the ICU.
The study has limitations that include the retrospective nature of the analysis, the small number of patients who underwent autopsies, and the fact that the study was conducted in a single center; therefore the findings may not be applicable to other centers. Also the authors who reviewed these cases were clinicians and did not include a review by a pathologist, which may affect the accuracy of the autopsy findings. Further, there are no details on the status of underlying malignancy and details of treatment provided in the MICU. Although postmortem examination is sought in all MICU deaths, it is possible that clinicians may have been vigorous in pursuing autopsy in cases of clinical uncertainty, which in turn may have influenced the rate of major discrepancies reported in this study. It is also not clear whether the advanced malignancy in some patients may have limited the extent of diagnostic studies. Prospective multicenter studies are needed to address these limitations and confirm the findings of this study.
In conclusion, in the era modern diagnostic technology, major discrepancies between clinical and postmortem diagnoses in critically ill cancer patients remain. Invasive aspergillosis, pulmonary thromboembolism and cancer recurrence are the main missed diagnoses. There is benefit from performing autopsies on these patients. They provide pertinent information that may be useful for future ICU care.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Adam AK, Soubani AO. Outcome and prognostic factors of lung cancer patients admitted to the medical intensive care unit. Eur Respir J. 2008;31:47–53. doi: 10.1183/09031936.00031607. [DOI] [PubMed] [Google Scholar]
- 2.Fernandez-Segoviano P, Lazaro A, Esteban A, Rubio JM, Iruretagoyena JR. Autopsy as quality assurance in the intensive care unit. Crit Care Med. 1988;16:683–5. doi: 10.1097/00003246-198807000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Blosser SA, Zimmerman HE, Stauffer JL. Do autopsies of critically ill patients reveal important findings that were clinically undetected? Crit Care Med. 1998;26:1332–6. doi: 10.1097/00003246-199808000-00015. [DOI] [PubMed] [Google Scholar]
- 4.Berlot G, Dezzoni R, Viviani M, Silvestri L, Bussani R, Gullo A. Does the length of stay in the intensive care unit influence the diagnostic accuracy? A clinical-pathological study. Eur J Emerg Med. 1999;6:227–31. [PubMed] [Google Scholar]
- 5.Roosen J, Frans E, Wilmer A, Knockaert DC, Bobbaers H. Comparison of premortem clinical diagnoses in critically iII patients and subsequent autopsy findings. Mayo Clin Proc. 2000;75:562–7. doi: 10.4065/75.6.562. [DOI] [PubMed] [Google Scholar]
- 6.Tai DY, El-Bilbeisi H, Tewari S, Mascha EJ, Wiedemann HP, Arroliga AC. A study of consecutive autopsies in a medical ICU: A comparison of clinical cause of death and autopsy diagnosis. Chest. 2001;119:530–6. doi: 10.1378/chest.119.2.530. [DOI] [PubMed] [Google Scholar]
- 7.Twigg SJ, McCrirrick A, Sanderson PM. A comparison of post mortem findings with post hoc estimated clinical diagnoses of patients who die in a United Kingdom intensive care unit. Intensive Care Med. 2001;27:706–10. doi: 10.1007/s001340100903. [DOI] [PubMed] [Google Scholar]
- 8.Ong AW, Cohn SM, Cohn KA, Jaramillo DH, Parbhu R, McKenney MG, et al. Unexpected findings in trauma patients dying in the intensive care unit: Results of 153 consecutive autopsies. J Am Coll Surg. 2002;194:401–6. doi: 10.1016/s1072-7515(02)01123-7. [DOI] [PubMed] [Google Scholar]
- 9.Nadrous HF, Afessa B, Pfeifer EA, Peters SG. The role of autopsy in the intensive care unit. Mayo Clin Proc. 2003;78:947–50. doi: 10.4065/78.8.947. [DOI] [PubMed] [Google Scholar]
- 10.Shojania KG, Burton EC, McDonald KM, Goldman L. Changes in rates of autopsy-detected diagnostic errors over time: A systematic review. JAMA. 2003;289:2849–56. doi: 10.1001/jama.289.21.2849. [DOI] [PubMed] [Google Scholar]
- 11.Combes A, Mokhtari M, Couvelard A, Trouillet JL, Baudot J, Hénin D, et al. Clinical and autopsy diagnoses in the intensive care unit: A prospective study. Arch Intern Med. 2004;164:389–92. doi: 10.1001/archinte.164.4.389. [DOI] [PubMed] [Google Scholar]
- 12.Silfvast T, Takkunen O, Kolho E, Andersson LC, Rosenberg P. Characteristics of discrepancies between clinical and autopsy diagnoses in the intensive care unit: A 5-year review. Intensive Care Med. 2003;29:321–4. doi: 10.1007/s00134-002-1576-z. [DOI] [PubMed] [Google Scholar]
- 13.Perkins GD, McAuley DF, Davies S, Gao F. Discrepancies between clinical and postmortem diagnoses in critically ill patients: An observational study. Crit Care. 2003;7:R129–32. doi: 10.1186/cc2359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dimopoulos G, Piagnerelli M, Berre J, Salmon I, Vincent JL. Post mortem examination in the intensive care unit: Still useful? Intensive Care Med. 2004;30:2080–5. doi: 10.1007/s00134-004-2448-5. [DOI] [PubMed] [Google Scholar]
- 15.Gerain J, Sculier JP, Malengreaux A, Rykaert C, Themelin L. Causes of deaths in an oncologic intensive care unit: A clinical and pathological study of 34 autopsies. Eur J Cancer. 1990;26:377–81. doi: 10.1016/0277-5379(90)90237-n. [DOI] [PubMed] [Google Scholar]
- 16.Al-Saidi F, Diaz-Granados N, Messner H, Herridge MS. Relationship between premortem and postmortem diagnosis in critically ill bone marrow transplantation patients. Crit Care Med. 2002;30:570–3. doi: 10.1097/00003246-200203000-00012. [DOI] [PubMed] [Google Scholar]
- 17.Pastores SM, Dulu A, Voigt L, Raoof N, Alicea M, Halpern NA. Premortem clinical diagnoses and postmortem autopsy findings: Discrepancies in critically ill cancer patients. Crit Care. 2007;11:R48. doi: 10.1186/cc5782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guidelines for intensive care unit admission, discharge, and triage. Task Force of the American College of Critical Care Medicine, Society of Critical Care Medicine. Crit Care Med. 1999;27:633–8. [PubMed] [Google Scholar]
- 19.Goldman L, Sayson R, Robbins S, Cohn LH, Bettmann M, Weisberg M. The value of the autopsy in three medical eras. N Engl J Med. 1983;308:1000–5. doi: 10.1056/NEJM198304283081704. [DOI] [PubMed] [Google Scholar]
- 20.Meersseman W, Vandecasteele SJ, Wilmer A, Verbeken E, Peetermans WE, Van Wijngaerden E. Invasive aspergillosis in critically ill patients without malignancy. Am J Respir Crit Care Med. 2004;170:621–5. doi: 10.1164/rccm.200401-093OC. [DOI] [PubMed] [Google Scholar]
- 21.Zmeili OS, Soubani AO. Pulmonary aspergillosis: A clinical update. QJM. 2007;100:317–34. doi: 10.1093/qjmed/hcm035. [DOI] [PubMed] [Google Scholar]
- 22.Meersseman W, Lagrou K, Maertens J, Wilmer A, Hermans G, Vanderschueren S, et al. Galactomannan in bronchoalveolar lavage fluid: A tool for diagnosing aspergillosis in intensive care unit patients. Am J Respir Crit Care Med. 2008;177:27–34. doi: 10.1164/rccm.200704-606OC. [DOI] [PubMed] [Google Scholar]
- 23.Linkins LA, Warkentin TE. The approach to heparin-induced thrombocytopenia. Semin Respir Crit Care Med. 2008;29:66–74. doi: 10.1055/s-2008-1047564. [DOI] [PubMed] [Google Scholar]
- 24.Esteban A, Fernandez-Segoviano P. Is autopsy dead in the ICU? Intensive Care Med. 2003;29:522–5. doi: 10.1007/s00134-002-1631-9. [DOI] [PubMed] [Google Scholar]


