Abstract
Background
Circumcision can be performed for a variety of techniques, including conventional dissection surgery or a Plastibell device, and has religious, ritual, or medical roots. In countries like Iran, circumcision is done purely on religious grounds. In this study, we outline 390 cases in our practice and describe the epidemiology, indications, surgical technique used, and the early complications.
Materials and methods
In this retrospective study, the charts for 390 circumcision cases were analyzed for the period March 2005 to August 2010. We reviewed all cases, noting age, indication, type of anesthesia used, technique, cosmetic appearance, and any potential early complications. All cases were followed up 1–4 weeks postoperatively and their notes were evaluated.
Results
The age of children who underwent circumcision ranged from 3 weeks to 14 years, with a mean age of 4.25 years. The most common age for circumcision was 4–5 years (14.6%), and the least common age was 11–12 years (1.5%). In 372 cases (95%), the parents had opted for the procedure for religious reasons, and in 18 cases (5%), there was a medical indication, including phimosis (11 cases, 3%), urinary tract infection (5 cases, 1.2%), and balanoposthitis (2 cases, 0.8%). No major early complications were found in our series. Cosmetic appearance was satisfactory in all cases by 4 weeks after the operation.
Conclusion
Circumcision was performed for religious reasons in our cases, although medical indications sometimes modified the timing of the procedure. Conventional dissection surgery for circumcision was safe, effective, and without any major complications.
Keywords: male circumcision, conventional dissection surgery, neonatal, infant, complication, religious, ritual, meatus, phimosis
Introduction
Circumcision is the most common surgical procedure performed in boys living in Islamic communities.1 According to Christian texts, Jesus Christ, being a Jew, was circumcised on the eighth day after his birth, and this day was celebrated as the “Day of Circumcision” by the Catholic Church until 1960.2 Historically, circumcision is one of the oldest operations performed (Egyptian mummies from the third millennium BC have been found to be circumcised), and has been practiced for thousands of years by Moslems, Jews, and different peoples in Africa, the US, and Australia.3,4 One-sixth of the total male population of the world is estimated to have undergone circumcision.5 From a religious point of view, it is obligatory for a Muslim male to undergo the procedure if at all possible. It is recommended that circumcision be performed during the first 7 days of life. However, if someone is unable to undergo this operation due to fear of injury or because of medical advice given by an expert physician, then the religious obligation to be circumcised is waived.
Parents throughout the world may choose to have their child circumcised for social, medical, or religious reasons. The procedure can be performed by a number of types of health care professionals, and most children have a good to excellent functional and cosmetic outcome.6 On occasion, the results are unsatisfactory to the parents or primary care physician. Neglecting hygiene and incorrect methods of circumcision can lead to dangerous early and late complications. Early complications include bleeding, infection, urinary retention, hematoma, and necrosis of the glans, occasionally requiring amputation of the glans penis.7–9 We report here our experience of over 390 consecutive cases of circumcision, including an evaluation of epidemiology, complications, and surgical technique.
Materials and methods
We reviewed the charts of 390 consecutive children, infants, and neonates who underwent circumcision over a 5-year period from March 2005 to August 2010. All were Muslims, and among them, 343 cases (88%) were Iranians. The remaining 47 cases (12%) were immigrants from neighboring countries. Circumcision was performed for males up to 3–4 years of age using local anesthesia, and for older children was performed under general anesthesia. All circumcisions were carried out in the operating room of Kamkar Hospital. The selection of type of anesthesia was made by the operating urologist. The procedure was performed by a skilled nurse in local anesthesia cases and by the urologist in general anesthesia cases. In the case of local anesthesia, a pre-emptive dorsal penile nerve block was used, whereby a penile ring block was applied, with 5 mg/kg of 2% lidocaine injected using a 24-gauge needle. Circumcision was performed by conventional dissection surgery in all cases. A dorsal incision in the prepuce was made to allow full retraction of the foreskin using artery forceps. The foreskin was cut sharply over the clamp with a surgical blade, and tincture of benzoate gauze was applied as a temporary dressing. The tips of the foreskin were sutured with 4-0 plain catgut sutures. After the procedure, all cases were observed for 6–12 hours and discharged if no complications were noted. Oral antibiotics were prescribed for 3 days in all cases, and parents were instructed to apply antibiotic ointment at each diaper exchange for 1 week in infants and younger children. For older children, topical ointment was to be applied twice daily, with permission for bathing after 48 hours, returning to school in 5 days, and resuming full activity within 2 weeks. Parents were instructed to attend a first follow-up visit at 1 week and a second at 4 weeks after the procedure.
Results
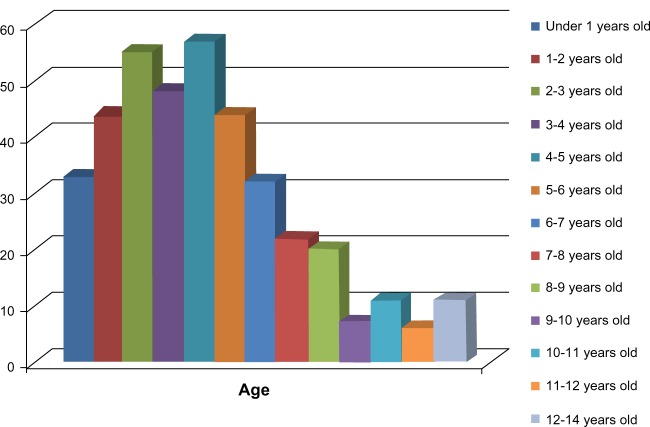
Children undergoing circumcision ranged in age from 3 weeks to 14 years, with a mean age of 4.25 years. The most common age of circumcision in our cases was 4–5 years (14.6%), and the least common age was 11–12 years (1.5%), as shown in Figure 1. The procedure was performed in 281 cases (72%) under local anesthesia and in the remaining 109 cases (28%) under general anesthesia (Figure 2). Circumcision was done for religious reasons in 372 cases (95%), because of phimosis in 11 cases (3%), urinary tract infection in five cases (1.2%), and balanophostitis in two cases (0.8%), as shown in Table 1. Conventional dissection surgery was the procedure used, and all patients were examined for early postoperative complications 1 week and 4 weeks later. Of the 390 male circumcisions performed, some early complications were seen, ie, hemorrhage (occurring in one patient [0.25%] 6 hours after the procedure and controlled by resuturing without any need for transfusion) and moderate to severe pain necessitating additional medication (two cases [0.5%]). No cases of penile swelling or glans injury were documented (Table 2). All patients had a satisfactory cosmetic outcome at 4 weeks after the operation.
Figure 1.
The age distribution of our circumcised cases.
Figure 2.
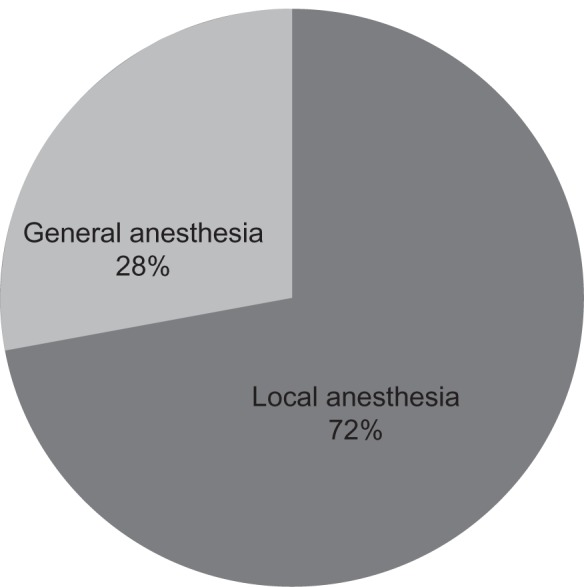
The distribution of type of anesthesia in our cases.
Table 1.
Indications for circumcision in Qom, Iran, from March 2005 to August 2010
| Religious ritual | 372 cases (95%) |
| Phimosis | 11 cases (3%) |
| Urinary tract infection | 5 cases (1.2%) |
| Balanoposthitis | 2 cases (0.8%) |
Table 2.
Early complications in our circumcised cases
| Bleeding | 1 case (0.25%) |
| Wound infection | 0 |
| Glans injury | 0 |
| Moderate to severe pain | 2 cases (0.50%) |
| Penile swelling | 0 |
| Unsatisfactory cosmetic appearance | 0 |
Discussion
Circumcision in Iran has a religious basis. In South Africa, neonatal circumcision is performed most commonly for religious and/or cultural reasons, followed by concern for hygiene, and more recently as a means of protection against human immunodeficiency virus/acquired immune deficiency syndrome.10 About 60% of male neonates in the US are circumcised.11 In different countries, eg, Angola, the Philippines, and the US, the procedure is considered to be a social norm, and most men are circumcised for nonreligious reasons, with rates of 99% in Angola, 90% in the Philippines, and 75% in the US, according to a Joint United Nations Programme on HIV/AIDS report in 2007.12 Figures on the health risks of circumcision in neonates vary, but most experts suggest that it is much safer in adults, with a complication rate below 1%. In the US, complication rates for neonatal circumcision have consistently been reported at 0.2%–0.4%.13 Complications, including bleeding and swelling, were reported to occur in approximately 1.5% of all circumcisions carried out by medical professionals in infants from 12 countries.13 However, for cultural and religious reasons, almost all parents in Iran elect to have their infants circumcised. Qom province is located in the center of Iran, with a population of 1,000,000, and all boys in the region have been circumcised by the time they reach puberty.
Circumcision may also be performed for a number of therapeutic and nontherapeutic reasons. Medical reasons cited for circumcision include phimosis and balanitis. Social and religious pressures are the most common reasons for nontherapeutic circumcision. The prepuce covering the glans is removed during the circumcision procedure to a point near the coronal sulcus.14 Despite the large number of specialists who perform this procedure, the results are rarely unsatisfactory.15
In a recent policy statement, the American Academy of Pediatrics stated that existing scientific data demonstrate the potential medical benefits of newborn male circumcision, but that these data are not sufficient to recommend routine newborn circumcision.6
Complications have an incidence of 0.2%–5.0%, and usually occur soon after circumcision, for reasons ranging from inadequate skin removal to neonatal death secondary to sepsis.16–18 Complications of circumcision may be addressed in acute and late categories. Acute problems include some major complications, ie, serious bleeding causing hemorrhagic shock and amputation, and late complications include skin loss, skin bridge, or urethrocutaneous fistula. Skin bridge is the most common cutaneous complication of newborn circumcision.18 The most common early complications tend to be minor and treatable, ie, pain, bleeding, swelling, or inadequate skin removal. However, serious complications can occur during the procedure, including death from excess bleeding, as well as amputation of the glans penis if the glans is not shielded during the procedure.19–21 We did not have any major complications like glans injury, sepsis, severe bleeding, or death in our series.
When circumcision is performed by an experienced surgeon, it is considered to be a routine and safe surgical procedure. However, despite its advantages, circumcision may have detrimental consequences if performed by an unskilled person. Moreover, when performed in greater numbers of people, the risk of complications increases.22–24 The late complications of circumcision include concealed penis, meatal stenosis,7,25,26 inclusion cysts, secondary chordee, urethrocutaneous fistula, phimosis, glandulopenile adhesions, and lymphedema.13,20,23,27,28 The reported overall complication rate of circumcision varies between 0.03% and 10%,29 and in our study was 0.75%, indicating that circumcision performed by qualified experts using conventional dissection surgery has the best outcomes.30 Hemorrhage, reported as one of the most common complications (0.1%–35%),31 was seen in 0.26% of the cases reported by Simforoosh et al32 and in 0.25% of our cases.
Conclusion
The most common reasons for circumcision in our region were religious and cultural. No major early complications were seen in our series. Due to the serious complications that can ensue, circumcision should be performed by trained nurses, surgeons, or urologists, and should be made illegal in unqualified hands. Circumcision by conventional dissection surgery is safe, without any major complications. If it is performed in secondary or tertiary care centers by experienced personnel, a high degree of parental satisfaction should be obtained. Our study was restricted to early complications, and follow-up studies are recommended to determine the late complications.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Aksz T, Erdoan B, Grrgti M, et al. Unusual complications of circumcision. Plast Reconstr Surg. 1998;101:1915–1918. doi: 10.1097/00006534-199806000-00021. [DOI] [PubMed] [Google Scholar]
- 2.Mattelaer JJ, Schipper RA, Das S. The circumcision of Jesus Christ. J Urol. 2007;178:31–34. doi: 10.1016/j.juro.2007.03.016. [DOI] [PubMed] [Google Scholar]
- 3.Parigi GB. Destiny of prepuce between Quran and DRG. Pediatr Med Chir. 2003;25:96–100. [PubMed] [Google Scholar]
- 4.Pust RA, Drost C, Willerding H, Bschleipfer T. Medieval scenes of ritual circumcision as a reflection of sociopolitical circumstances. Urologe A. 2005;44:277–281. doi: 10.1007/s00120-004-0761-9. German. [DOI] [PubMed] [Google Scholar]
- 5.Kazem MM, Mehdi AZ, Golrasteh KZ, Behzad FZ. Comparative evaluation of two techniques of hemostasis in neonatal circumcision using the Plastibell device. J Pediatr Urol. 2010;6:258–260. doi: 10.1016/j.jpurol.2009.08.007. [DOI] [PubMed] [Google Scholar]
- 6.American Academy of Pediatrics Task Force on Circumcision: Circumcision policy statement. Pediatrics. 1999;103:686–693. [PubMed] [Google Scholar]
- 7.Bazmamoun H, Ghorbanpour M, Mousavi-Bahar SH. Lubrication of circumcision site for prevention of meatal stenosis in children younger than 2 years old. Urol J. 2008;5:233–236. [PubMed] [Google Scholar]
- 8.Muula AS, Prozesky HW, Mataya RH, Ikechebelu JI. Prevalence of complications of male circumcision in Anglophone Africa: A systematic review. BMC Urol. 2007;7:4. doi: 10.1186/1471-2490-7-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Okeke LI, Asinobi AA, Ikuerowo OS. Epidemiology of complications of male circumcision in Ibadan, Nigeria. BMC Urol. 2006;6:21. doi: 10.1186/1471-2490-6-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Banieghbal B. Optimal time for neonatal circumcision: An observation-based study. J Pediatr Urol. 2009;5:359–362. doi: 10.1016/j.jpurol.2009.01.002. [DOI] [PubMed] [Google Scholar]
- 11.Niku S, Stock J, Kaplan G. Neonatal circumcision. Urol Clin North Am. 1995;22:57–65. [PubMed] [Google Scholar]
- 12.World Health Organization, Joint United Nations Programme on HIV/AIDS Male circumcision: Global trends and determinants of prevalence, safety and acceptability Available at: http://malecircumcision.org/media/documents/MC_Global_Trends_Determinants.pdfAccessed April 4, 2011
- 13.Weiss Ha, Larke N, Halperin D, Schenker I. Complications of circumcision in male neonates, infants, and children: A systematic review. BMC Urol. 2010;10:2. doi: 10.1186/1471-2490-10-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hirji H, Charlton R, Sarmah S. Male circumcision: A review of the evidence. J Mens Health Gend. 2005;2:21–30. [Google Scholar]
- 15.Brisson PA, Patel HI, Feins NR. Revision of circumcision in children: Report of 56 cases. J Pediatr Surg. 2002;37:1343–1346. doi: 10.1053/jpsu.2002.35005. [DOI] [PubMed] [Google Scholar]
- 16.Patel HI, Moriarty KP, Brisson PA, et al. Genitourinary injuries in the newborn. J Pediatr Surg. 2001;36:235–239. doi: 10.1053/jpsu.2001.20062. [DOI] [PubMed] [Google Scholar]
- 17.Breuer GS, Walfisch S. Circumcision complications and indications for ritual circumcisions – clinical experience and review of the literature. Isr J Med Sci. 1987;23:252–256. [PubMed] [Google Scholar]
- 18.Baskin LS, Canning DA, Snyder HM, et al. Treating complications of circumcision. Pediatr Emerg Care. 1996;12:62–68. doi: 10.1097/00006565-199602000-00018. [DOI] [PubMed] [Google Scholar]
- 19.Shenfeld OZ, Ad-El D. Penile reconstruction after complete glans amputation during ritual circumcision. Harefuah. 2000;139:352–354. Hebrew. [PubMed] [Google Scholar]
- 20.Ben Chaim J, Livne PM, Binyamini J, Hardak B, Ben-Meir D, Mor Y. Complications of circumcision in Israel: A one year multicenter survey. Isr Med Assoc J. 2005;7:368–370. [PubMed] [Google Scholar]
- 21.Schoen EJ, Colby CJ, To TT. Cost analysis of neonatal circumcision in a large health maintenance organization. J Urol. 2006;175(3 Pt 1):1111–1115. doi: 10.1016/S0022-5347(05)00399-X. [DOI] [PubMed] [Google Scholar]
- 22.Yegane RA, Kheirollahi AR, Salehi NA, Bashashati M, Khoshdel JA, Ahmadi M. Late complications of circumcision in Iran. Pediatr Surg Int. 2006;22:442–445. doi: 10.1007/s00383-006-1672-1. [DOI] [PubMed] [Google Scholar]
- 23.Williams N, Kapila L. Complications of circumcision. Br J Surg. 1993;80:1233–1236. doi: 10.1002/bjs.1800801005. [DOI] [PubMed] [Google Scholar]
- 24.Demirseren ME, Gokrem S. Circumcision in unqualified hands: A significant risk of complication. Plast Reconstr Surg. 2004;113:1090–1092. doi: 10.1097/01.prs.0000107735.19836.60. [DOI] [PubMed] [Google Scholar]
- 25.Joudi M, Fathi M, Hiradfar M. Incidence of asymptomatic meatal stenosis in children following neonatal circumcision. J Pediatr Urol. 2010 Sep 17; doi: 10.1016/j.jpurol.2010.08.005. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 26.Mahmoudi H. Evaluation of meatal stenosis following neonatal circumcision. Urol J. 2005;2:86–88. [PubMed] [Google Scholar]
- 27.Mousavi SA, Salehifar E. Circumcision complications associated with the Plastibell device and convention dissection surgery: A trial of 586 infants of ages up to 12 months. Adv Urol. 2008:606123. doi: 10.1155/2008/606123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Osifo OD, Oriaifo IA. Circumcision mishaps in Nigerian children. Ann Afr Med. 2009;8:266–270. doi: 10.4103/1596-3519.59583. [DOI] [PubMed] [Google Scholar]
- 29.Kaplan GW. Complications of circumcision. Urol Clin North Am. 1983;10:543–549. [PubMed] [Google Scholar]
- 30.Harel L, Staussbergr R, Jackson S, Amir J, Tiqwa P. Influence of circumcision technique on frequency of urinary tract infections in neonates. Pediatr Infect Dis J. 2002;21:879–880. doi: 10.1097/00006454-200209000-00020. [DOI] [PubMed] [Google Scholar]
- 31.Schoen EJ. Rebuttal: Should newborns be circumcised? YES. Can Fam Physician. 2008;54:22. [PMC free article] [PubMed] [Google Scholar]
- 32.Simforoosh N, Tabibi A, Khalil SAR, et al. Neonatal circumcision reduces the incidence of asymptomatic urinary tract infection: A large prospective study with long-term follow up using Plastibell. J Pediatr Urol. 2010 Nov 4; doi: 10.1016/j.jpurol.2010.10.008. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]