Abstract
Hospice is an underused service among people with Alzheimer disease. This study used the Hospice Use Model to examine community, care recipient, and caregiver characteristics associated with hospice use before death among 145 community-dwelling care recipients with Alzheimer disease and their caregivers. Secondary analysis using logistic regression modeling indicated that older age, male gender, black race, and better functional health of care recipients with Alzheimer disease were associated with a decreased likelihood of using hospice (model χ25 = 23.5, P = .0003). Moreover, care recipients recruited from an Alzheimer clinic were more likely to use hospice than those recruited from adult day-care centers. Caregiver factors were not independent predictors of hospice use. However, there was a significant interaction between hours of care provided each week and recruitment site. Among care recipients from the Alzheimer clinic, the probability of hospice use increased as caregiving intensity increased. This relationship was reversed in care recipients from day-care centers. Results suggest that adult day-care centers need to partner with hospice programs in the community. In conclusion, care recipient and community service factors influence hospice use in individuals with Alzheimer disease.
Keywords: adult day care, Alzheimer disease, caregivers, hospice, Hospice Use Model
A lzheimer disease (AD), the most common form of dementia1 that affects adults 65 years or older, was ranked the sixth leading cause of death in the United States in 2009.2 Alzheimer disease is incurable, progressive, and terminal.1 Terminal symptoms of AD such as loss of communicative abilities, loss of bodily functions, and becoming bed-bound,1 as well as family and friends’ lengthy ordeal in providing care, all reinforce the need for and appropriateness of hospice use among people with AD at the end of life.3 Benefits of hospice for care recipients include appropriate management of physical and emotional symptoms that cause pain, discomfort, and distress; nutritional management; and attention to social and spiritual needs; family/caregiver benefits include emotional support, respite, and grief counseling.3
The reported extent of hospice use among people with AD differs depending on the type of data reported and whether the data source is hospice organizations or Medicare claims files. Annual survey data on hospice admissions by primary diagnosis from the National Hospice and Palliative Care Organization indicated that the percentage of hospice admissions with dementia or AD has ranged from 9.8% in 2005 to 11.2% in 2009 and that dementia and AD were the third most common primary noncancer diagnoses in 2009.4 Alternatively, data on hospice use by diagnosis from Centers for Disease Control and Prevention death certificate records and Centers for Medicare & Medicaid Services hospice claims files for 2002 indicated that 41% of persons 65 years or older who died with a primary diagnosis of AD had used hospice care at some point during the year before their death.5 Furthermore, in both databases, AD was one of three causes of death with the highest hospice utilization rates in 2002 (malignancies = 65%; kidney disease and nephritis = 55%).5 Although both private and federal sources of data suggest that dementia and AD account for a substantial proportion of hospice use among older adults, hospice services are still underutilized in this population, with less than half of all dying patients using hospice.
Previous research has identified several factors associated with hospice use among community-dwelling care recipients regardless of terminal condition. For example, hospice use was more likely among care recipients who were white,5-8 female,5 and older5; had a diagnosis of cancer5,7,9,10; received home health services10; were married; had some college education; owned a home; made a living will; had high levels of social support; or had higher income.7
However, several studies have shown conflicting results regarding which care-recipient factors were associated with hospice use. One study found hospice use more likely among care recipients, unadjusted for type of diagnosis, who were relatively young (<54 years old) or male.7 Another study found hospice use more likely among care recipients, adjusted for cancer type and site, who were unmarried men.8 In brief, care-recipient factors age, gender, and marital status are associated with hospice use but not in a consistent manner.
Similarly, several studies have shown conflicting results about whether care-recipient age is a factor associated with hospice use among people with AD. In a previous study using secondary analysis, where national claims and mortality data were examined to determine differences in hospice utilization, results showed that for seven of the 11 cause-of-death categories, the hospice utilization rate was notably lower for the youngest age category (65-74 years) than for the oldest age categories (>74 years).5 For AD, however, hospice utilization decreased considerably with age (55% for 65- to 74-year-olds, 48% for 75- to 84-year-olds, and 36% for those ≥85 years),5 suggesting that older age is negatively associated with hospice use among people with AD.
Hospice use and duration thereof are associated with several caregiver factors. Caregivers who are daughters of the care recipients,10 and knowledgeable about hospice,11 were more likely to use hospice. Also, if the hospice user had an informal caregiver, hospice use was longer.10 However, caregivers who were protective of their caregiving role were less likely to use hospice.12 Interestingly, caregivers who had higher depression scores were less willing to even discuss home hospice.13
Although many studies of health services use employ a conceptual framework based on the Behavioral Model of Health Services Utilization (BMHSU),14 a comprehensive health services conceptual framework has not been used for the study of hospice. Without such a framework to provide context, it is difficult to replicate studies, to understand care recipient and caregiver factors associated with hospice use, or to interpret research findings.
To address the lack of a conceptual framework, the Behavioral Model of Hospice Use (BMHU) was developed to guide a study of factors associated with hospice use among terminally ill cancer and noncancer patients.6 However, the study was limited to terminally ill patients who had been referred to hospice. More importantly, the framework did not include caregiver factors.
Caregiver characteristics were included in the Revised Andersen’s Behavioral Model of Health Services Utilization (RAB) to identify caregiver and care-recipient factors associated with formal service utilization.15 However, the model focused on formal service utilization in the home, community, physician and hospital settings, and not primarily hospice. Moreover, the study population included only Hispanic Americans, limiting the external validity of the study findings. More work is therefore needed to determine if caregiver factors are associated with hospice use among terminally ill patients.
The primary purpose of this study was to determine if community characteristics and caregiver characteristics were associated with hospice use at the end of life among people 65 years or older with AD, after controlling for the effect of care-recipient characteristics. That is, we wanted to examine the additional influence of community characteristics and caregiver characteristics on hospice use after care-recipient characteristics were considered. To guide the study, we developed the Hospice Use Model, which incorporates important concepts and predictors of hospice use from previous research into a single health services use model.
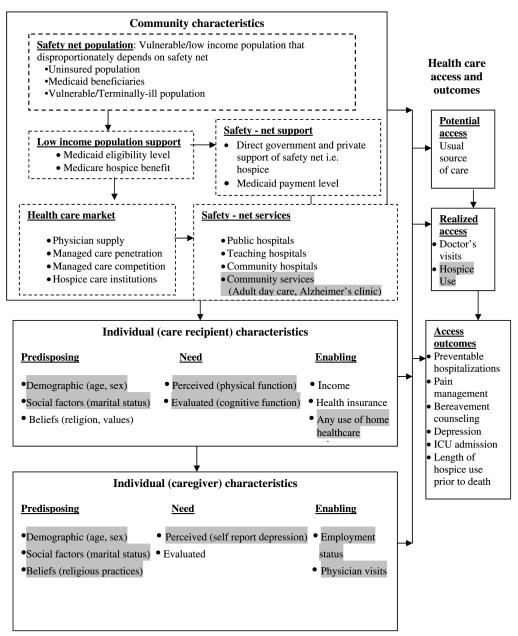
Conceptual Framework
The Hospice Use Model shown in Figure 1 incorporates concepts from three health services use models: BMHU,6 RAB,15 and the BMHSU.14 The BMHSU describes community characteristics (safety-net population, low-income population support, healthcare market, safety-net support, and safety-net services) and individual characteristics (predisposing, need, enabling factors) that influence the individual’s healthcare access and outcomes.14 Community characteristics in this model describe the effects of contextual variables (social, economic, structural, public policy) on healthcare access and outcomes.14 Individual characteristics are attributes of the person that influence whether he/she will seek care and the effects on healthcare access and outcomes.14
FIGURE 1.
Hospice Use Model: modified conceptual framework. Shaded areas show examples of variables that were tested in the study. Davidson et al.14 Reprinted with permission.
In contrast to the BMHSU,14 the Hospice Use Model included community services in the list of safety-net services within community characteristics. Community services are local places offering formal services to people with AD and their families, typically within their neighborhood. Community characteristics are important because physicians’ knowledge of hospice services and the Medicare hospice benefit have been shown to influence hospice use at the end of life.16 Moreover, providers’ propensity to discuss or refer patients to hospice has been associated with hospice use.3,17
The Hospice Use Model also includes the concept individual (caregiver) characteristics borrowed from the RAB.15 These are attributes of the caregiver that influence whether he/she will seek hospice services for their care recipient at the end of life. Individual (caregiver) characteristics, such as gender, race, beliefs, and health condition, have been shown to influence hospice use. For example, in a focus group study of minority caregivers (n = 53), strong religious beliefs were found to decrease the likelihood of using hospice because the caregivers depended more on spirituality as means to cope with end-of-life issues.18 Lack of awareness of hospice also contributed to lack of hospice use in this sample. Similar to all three models, the Hospice Use Model includes the individual (care recipient) characteristics that are attributes of the care recipient that influence whether he/she will seek hospice care.14
We developed the Hospice Use Model to reflect a comprehensive array of factors that may influence hospice use. An important contribution of this study is that we were able to test predictors of hospice use from each of the three major concepts shown in Figure 1 within a single study (community characteristics, individual caregiver characteristics, and individual care-recipient characteristics). However, our use of secondary data meant that we were able to test only a limited number of factors from each of these major concepts. Examples of these factors are shown in the shaded areas of Figure 1. As such, this analysis does not reflect a comprehensive test of the Hospice Use Model.
METHODS
Design
This secondary analysis used previously collected data from a parent study entitled, “Longitudinal Study of Day Care in Alzheimer’s Disease” (R01 AG10315) to explore caregiver factors and safety-net services associated with hospice use at the end of life among persons with AD.
Description of the Data Source
The parent study, referred to as the Adult Day Care Study (ADCS), is a longitudinal observational study that examined the impact of adult day care and other home- and community-based services on nursing home placement among community-dwelling individuals with AD, adjusting for caregiver and care-recipient factors.19 The study and consent procedures were approved by the institutional review board at Rush University Medical Center, and signed consent was obtained from each participant with AD and a family member.
The ADCS sample included 588 caregivers and community-dwelling care recipients with AD 65 years or older (73% of eligible individuals) who either used one of the 16 identified adult day-care services or enrolled at the federally funded Rush Alzheimer Disease Center clinic but not both. Excluded from the ADCS sample were caregivers of care recipients who were no longer living in the community (were in assisted-living or nursing home facilities) at the time of data collection. Primary caregivers of the care recipients with AD were interviewed either face-to-face or by telephone about their respective care recipients and their caregiving experience at baseline and every 3 months for up to 4 years, using standardized measures. The mode effect of survey data collection was addressed by checking and maintaining interrater reliability at 90% or greater, every 6 months during the data collection period.19 Follow-up ended at time of care-recipient death, nursing home placement, or study completion. An average of 85% of survivors participated at each follow-up (range, 77%-100%).
Analytic Sample
For purposes of this exploratory study, the sample was limited to care recipients who died during the ADCS period (n = 145). Care-recipient death was confirmed using two sources: the caregiver’s self-report of care-recipient death and the Centers for Disease Control and Prevention National Death Index files. For care recipients who died, caregivers were asked whether their care recipient used hospice prior to death. The analyses reported here focus on the relation of caregiver factors and community safety-net services to hospice use among the 145 care recipients with AD prior to death.
Measures
Outcome Variable
The outcome, hospice use, was identified by the caregiver’s “yes” or “no” response to the question: “Prior to his/her death, did you use hospice?”
Predictor Variables
The use of secondary data limited the number of predictor variables we were able to test from the Hospice Use Model. Consistent with the Hospice Use Model, this limited set of variables was grouped according to the following concepts: community characteristics, individual (care recipient) characteristics, and individual (caregiver) characteristics. Community characteristics focused on two safety-net services available to people with AD living in the community: an AD diagnostic and referral clinic and adult day-care centers.
Individual (care recipient) characteristics focused on care-recipient predisposing, need, and enabling factors. Predisposing factors included demographic and social characteristics of age, race, gender, education, and marital status. Need factors were operationalized using the cognitive measure Mini-Mental State Examination (MMSE),20 the caregiver’s report of care recipient’s comorbid health conditions, and three measures of physical function. Comorbid health conditions included any diagnosis of stroke, cancer, heart attack, hypertension, or diabetes. Measures of physical function included Katz Index of Activities of Daily Living,21 which assesses the ability to perform, without assistance, six basic activities—eating, bathing, dressing, getting from bed to chair, using the toilet, and walking across a room; Rosow-Breslau Functional Health Scale,22 which assesses three aspects of gross mobility—ability to do heavy work around the house, to walk up and down stairs, and to walk half a mile; and the Nagi Scale,23 which assesses difficulty in performing five activities of upper or lower extremity function—pulling or pushing large objects; carrying weights greater than 10 lb; stooping, crouching, and kneeling; reaching or extending arms above the shoulder level; and writing or handling small objects. For each physical function measure, we summed items to produce a score ranging from 0 (no disability) to the maximum score indicating disability on all items (6 for the Katz, 3 for the Rosow-Breslau, and 5 for the Nagi Scale). Enabling factors included any use of home healthcare services.
Individual (caregiver) characteristics focused on caregiver predisposing, need, and enabling factors. Predisposing factors included (1) demographic characteristics of age, race, gender, and education; (2) social characteristics of marital status, kin relationship to care recipient, quality of past relationship with care recipient, whether others provide care, and co-residence with care recipient; and (3) religious/spiritual practices (frequency of attending religious services and of praying/meditating).
Need factors were operationalized using standardized measures of caregiving burden scale,24 a 10-item Center for Epidemiological Studies–Depression scale,25 caregiving satisfaction scale,24 a summary measure of the time spent in caregiving activities in an average week (range 0-168 hours), and a summary index of the number of days in the previous month when physical or mental health was reported as not good (range, 0-30).26 Psychometric properties of the standardized measures are well established, and the Cronbach’s α scores for the ADCS sample are reported elsewhere.19
Enabling factors were operationalized using current caregiver employment status, frequency of care-recipient physician visits in the past 3 months, and the type of physician seen.
To use individual (caregiver) characteristics as a predictor of hospice use, we used data from a period substantially longer than 6 months before the care recipient’s death, which is the standard time covered under the Medicare hospice benefit. Thus, we used caregiver data collected from 8 months (245 days) to 16 months (485 days) prior to the care recipient’s death.
Data Analysis
Descriptive Statistics
Prior to analysis, care recipient and caregiver data were screened for accuracy and for missing values. The percentage of observations missing for specific variables ranged from 0% to 3%. The only exception was the variable about the type of healthcare provider seen that had missing data for 9% of observations. Because the percentage of missing values for predictors was extremely low, we deleted observations with missing values for any of the variables in each model. Descriptive statistics and graphical analysis were used to summarize the data in terms of measures of distribution, central tendency, dispersion, and association and to assess the fit between data distributions and assumptions of logistic regression analysis.
Logistic Regression Modeling
Multivariate logistic regression using the forward stepwise method was used to test four hypotheses:
 H1: Caregiver predisposing factors are significantly associated with care-recipient hospice use prior to death.
H1: Caregiver predisposing factors are significantly associated with care-recipient hospice use prior to death. H2: Caregiver need factors are significantly associated with care-recipient hospice use prior to death.
H2: Caregiver need factors are significantly associated with care-recipient hospice use prior to death. H3: Caregiver enabling factors are significantly associated with care-recipient hospice use prior to death.
H3: Caregiver enabling factors are significantly associated with care-recipient hospice use prior to death. H4: Community characteristics, specifically community safety-net services, are significantly associated with care-recipient hospice use prior to death.
H4: Community characteristics, specifically community safety-net services, are significantly associated with care-recipient hospice use prior to death.
Model development proceeded in four steps. In Step 1 of the modeling, we introduced care-recipient predisposing factors (age, race, gender, education), then used forward stepwise selection to identify significant predictors of hospice use from among care-recipient need factors (measures of cognitive function, physical function, and comorbidities) and the enabling factor (use of home healthcare services). The result served as the core model for testing the four stated hypotheses based on the Hospice Use Model.
In Step 2, we began with the core model, and in three separate models, we used forward stepwise selection to identify significant predictors from each of the three groups of caregiver factors—predisposing, need, and enabling. We then used forward stepwise selection to identify the significant predictors from among the three separate models of caregiver factors.
In Step 3, we began with the resulting model from Step 2 and introduced the community-services variable (Alzheimer clinic or adult day-care center). In Step 4, defined as exploratory, we examined interactions between each caregiver predisposing, need, and enabling factor and the community-services variable. Significant interactions were retained in the final model. All analyses concluded significance with P < .05.
RESULTS
Descriptive Statistics
Table 1 provides descriptive statistics for the caregivers and care recipients. The analytic sample included 145 caregivers of 145 care recipients with AD; about half were recruited from the Alzheimer clinic (n = 72, 49.7%) and the other half from the 16 adult day-care centers (n = 73, 50.3%). An almost equal number of care recipients used hospice prior to death (n = 71, 49%) compared with those who did not use hospice (n = 74, 51%). Care recipients had moderate to high levels of disability on the three measures of physical function and were severely cognitively impaired, with an average MMSE score of 9.0 (SD, 7.6). Cognitive function was significantly correlated with all three measures of physical function (P = .003 to .0001) and with education (P = .03).
TABLE 1.
Descriptive Data for Sample
| Care Recipients | |||||||
|---|---|---|---|---|---|---|---|
| Variable | Valid Range |
Adult Day Care (n = 73) | Alzheimer Clinic (n = 72) | Total Sample (n = 145) | |||
| n (%)a | Mean (SD) | n (%)a | Mean (SD) | n (%)a | Mean (SD) | ||
| Predisposing characteristics | |||||||
| Age, y | 84.0 (6.8) | 80.3 (8.9) | 82.1 (8.1) | ||||
| Race | |||||||
| White/other | 50 (68) | 52 (72) | 102 (70) | ||||
| Black | 23 (32) | 20 (28) | 43 (30) | ||||
| Gender | |||||||
| Male | 25 (34) | 27 (37) | 52 (36) | ||||
| Female | 48 (66) | 45 (63) | 93 (64) | ||||
| Education (years of schooling completed) |
10.4 (3.9) | 11.7 (3.3) | 11.0 (3.7) | ||||
| Marital status | |||||||
| Married or living with partner |
20 (27) | 40 (56) | 60 (41) | ||||
| Not married | 53 (73) | 32 (44) | 85 (59) | ||||
| Need factors | |||||||
| Cognitive function | |||||||
| MMSE score | 0-30 | 10.1 (7.2) | 8.1 (7.9) | 9.0 (7.6) | |||
| Physical function | |||||||
| Katz score | 0-6 | 3.4 (1.9) | 3.4 (2.3) | 3.4 (2.1) | |||
| Nagi score | 0-5 | 3.1 (1.4) | 2.9 (1.6) | 3.0 (1.5) | |||
| Rosow-Breslau score | 0-3 | 2.2 (0.9) | 2.1 (1.0) | 2.2 (0.9) | |||
| Comorbidities (yes) | |||||||
| Stroke | 25 (34) | 11 (15) | 36 (25) | ||||
| Cancer | 14 (19) | 14 (19) | 28 (19) | ||||
| Heart attack | 13 (18) | 8 (11) | 21 (14) | ||||
| Hypertension | 37 (51) | 28 (39) | 65 (45) | ||||
| Diabetes | 13 (18) | 8 (11) | 21 (14) | ||||
| At least 1 or more | 55 (75) | 46 (64) | 101 (70) | ||||
| Enabling factor | |||||||
| Home health use (yes) | 29 (40) | 33 (46) | 62 (43) | ||||
| Predisposing characteristics | |||||||
| Age, y | 61.4 (11.5) | 64.2 (13.0) | 62.7 (12.3) | ||||
| Race | |||||||
| White/other | 49 (67) | 53 (75) | 102 (71) | ||||
| Black | 24 (33) | 18 (25) | 42 (29) | ||||
| Gender | |||||||
| Male | 8 (11) | 26 (36) | 34 (24) | ||||
| Female | 65 (89) | 46 (64) | 111 (76) | ||||
| Education (years of schooling completed) |
14.2 (2.8) | 14.0 (2.5) | 14.0 (2.6) | ||||
| Marital status | |||||||
| Married or living with partner |
47 (64) | 57 (80) | 104 (72) | ||||
| Not married | 26 (36) | 14 (20) | 40 (28) | ||||
| Kin relationship to care recipient |
|||||||
| Spouse | 16 (22) | 32 (44) | 48 (33) | ||||
| Child/other | 57 (78) | 40 (56) | 97 (67) | ||||
| Quality of past relationship with care recipient |
3-15b | 12.2 (2.9) | 13.1 (2.1) | 12.7 (2.6) | |||
| Others provide care to care recipient |
|||||||
| None | 24 (34) | 32 (44) | 56 (39) | ||||
| 1 person | 25 (36) | 24 (34) | 49 (35) | ||||
| 2 persons | 21 (30) | 16 (22) | 37 (26) | ||||
| Co-reside (yes) | 61 (84) | 51 (71) | 112 (77) | ||||
| Religious/spiritual practices |
|||||||
| Attend religious services |
|||||||
| Never | 20 (27) | 22 (31) | 42 (29) | ||||
| Once a year or less | 13 (18) | 12 (17) | 25 (17) | ||||
| A few times a year | 28 (38) | 32 (44) | 60 (41) | ||||
| 1-3 times a month | 4(6) | 0(0) | 4(3) | ||||
| 1-3 times a week | 8 (11) | 5(7) | 13 (9) | ||||
| Nearly every day | 0(0) | 1 (1) | 1 (1) | ||||
| Pray or meditate | |||||||
| Never | 8 (11) | 8 (11) | 16 (11) | ||||
| Once a year or less | 1 (1) | 1 (1) | 2 (1) | ||||
| A few times a year | 7 (10) | 10 (14) | 17 (12) | ||||
| 1-3 times a month | 44 (60) | 43 (60) | 87 (60) | ||||
| 1-3 times a week | 4(6) | 0(0) | 4(3) | ||||
| Nearly every day | 9 (12) | 10 (14) | 19 (13) | ||||
| Need factors | |||||||
| Caregiving burden | 10-40c | 15.9 (6.0) | 15.4 (6.4) | 15.7 (6.2) | |||
| Caregiver depression | 0-10c | 1.6 (2.0) | 1.9 (2.1) | 1.8 (2.0) | |||
| Caregiving satisfaction | 5-20c | 14.9 (4.1) | 16.1 (3.6) | 15.6 (3.9) | |||
| Caregiving time | |||||||
| Hours per day | 0-24 | 8.7 (6.9) | 9.6 (8.5) | 9.1 (7.7) | |||
| Days per week | 0-7 | 6.6 (1.8) | 6.2 (2.0) | 6.4 (1.9) | |||
| Total hours per week | 0-168 | 60.1 (50.4) | 64.9 (61.1) | 62.5 (55.8) | |||
| Unhealthy days per 30 d | 0-30 | 8.2 (10.0) | 7.9 (10.8) | 8.0 (10.3) | |||
| Enabling factors | |||||||
| Currently employed | |||||||
| Yes | 39 (53) | 29 (41) | 68 (47) | ||||
| No | 34 (47) | 42 (59) | 76 (53) | ||||
| Frequency of care recipients physician visits in past 3 mo |
|||||||
| None | 9 (12) | 21 (30) | 30 (21) | ||||
| 1 | 25 (34) | 17 (24) | 42 (29) | ||||
| 2 | 16 (22) | 14 (20) | 30 (21) | ||||
| >2 | 23 (32) | 18 (26) | 41 (29) | ||||
| Physician specialty | |||||||
| Geriatrician | 26 (36) | 9 (12) | 35 (24) | ||||
| Family practitioner | 25 (34) | 27 (38) | 52 (36) | ||||
| Internist | 16 (22) | 20 (28) | 36 (25) | ||||
| Cardiologist | 1 (1) | 3 (4) | 4(3) | ||||
| Other | 1 (1) | 4(6) | 5(3) | ||||
| Missing | 4(6) | 9 (12) | 13 (9) | ||||
Abbreviation: MMSE, Mini-Mental State Examination.
Percent rounded to nearest whole number.
Higher value indicates a more positive relationship.
Higher value indicates a greater level of the variable.
The majority of white men (57%) were caring for a spouse, and the majority of the white women (66%) were caring for parents or another relative (χ21 [n = 102]) = 4.61, P = .03). Approximately 80% of black caregivers were caring for parents or another relative regardless of gender (χ21 [n = 42] = .05, P = .83). In both races, all spouse caregivers lived with the care recipient. However, among nonspouse caregivers, more black caregivers than white caregivers lived with the care recipient (80% vs 59%, respectively).
Logistic Regression
The starting model for the regression analysis consisted of care-recipient age, race, gender, and education. Forward selection from among care-recipient need factors (cognitive function, three measures of physical function, and five types of comorbidities) and the enabling factor of home healthcare use resulted in selection of only the Rosow-Breslau measure of functional health/disability. The core model (Table 2, Model 1) indicated that, among care recipients, older age, male gender, black race, and better functional health (fewer disabilities) were associated with a decreased likelihood of using hospice (model χ25 = 23.5, P = .0003). For each additional item of functional disability, the odds ratio of care recipients using hospice at the end of life was 1.54. Figure 2 graphically displays these results and shows that, regardless of race, women have a higher probability of hospice use as functional disabilities increase compared with men.
TABLE 2.
Modeling Hospice Use Before Death Using Logistic Regression, Odds Ratio (95% Confidence Interval; P Values)
| Model 1: Core Model | Model 2 | Model 3: Final Model | |
|---|---|---|---|
| Care recipient | |||
| Age 80 y | 0.95 (0.90-0.99; .03a) | 0.95 (0.90-1.00; .07) | 0.94 (0.88-0.99; .03a) |
| 12 years’ education | 0.92 (0.82-1.02; .11) | 0.90 (0.81-1.01; .07) | 0.85 (0.75-0.96; .01a) |
| Male gender | 0.36 (0.16-0.78; .01a) | 0.35 (0.16-0.77; .01a) | 0.35 (0.15-0.81; .01a) |
| Black race | 0.28 (0.12-0.66; .004a) | 0.27 (0.1 1-0.65; .004a) | 0.23 (0.09-0.60; .002a) |
| No. of functional disabilities (0-3) |
1.54 (1.03-2.32; .04a) | 1.56 (1.03-2.36; .03a) | 1.56 (1.01-2.39; .04a) |
| Community: safety-net services | |||
| Alzheimer clinic recruitment site |
2.17 (1.02-4.60; .04a) | 1.24 (0.53-2.89; .61) | |
| Caregiver | |||
| Caregiving intensity per week (0-168 h) |
0.99 (0.98-1.00; .07) | ||
| Caregiving intensity per week × recruitment site |
1.02 (1.00-1.03; .02a) | ||
Significant at P < .05.
FIGURE 2.
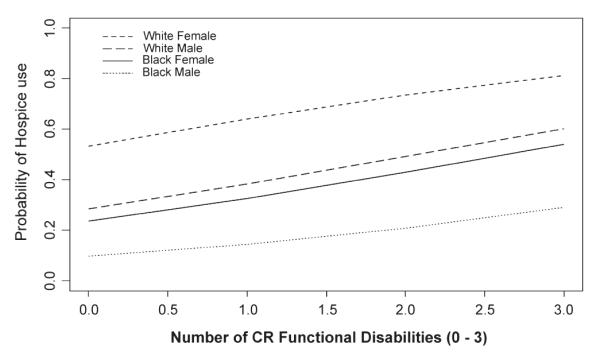
Probability of hospice use by functional disability using the Rosow-Breslau Scale (model based on age of 80 years and 12 years of education).
In Step 2, we added caregiver predisposing, need, and enabling factors to the core model in separate stepwise regression models. Three of the caregiver scale measures had substantial numbers of values throughout the distribution: caregiving satisfaction, caregiving time, and number of unhealthy days. For the other three measures (quality of past relationship with care recipient, caregiver depression, and caregiving burden), there were few caregivers at the extreme negative end of the scale, but a fair distribution for at least half of the scale. None of the caregiver variables were significant predictors of hospice use, and none substantially altered the results from the core model (results are not shown in Table 2).
In Step 3, forcing in the community-services variable (Alzheimer clinic or adult day-care center) resulted in selection of the Alzheimer clinic as significantly associated with hospice use. Results of this step are shown in Table 2 as Model 2. The odds of hospice use for care recipients recruited from the Alzheimer clinic were twice that for recipients recruited from day-care centers, but this variable did not alter the effect of gender, race, and functional disability on hospice use. Results (Table 2, Model 2) indicated that male gender, black race, better functional health (fewer disabilities), and being recruited from an adult day-care center were associated with a decreased likelihood of using hospice (model χ26 = 27.7, P = .0001).
In the final model, we conducted exploratory tests of interaction between each caregiver predisposing, need, and enabling factor and the community-services variable. Even though none of the caregiver variables were significantly associated with hospice use, we wanted to explore the possibility that results might differ in a subgroup of caregivers based on recruitment site. Results shown in Table 2 as Model 3 indicated a significant interaction between caregiving intensity (hours of care provided each week) and the Alzheimer clinic recruitment site.
Among caregivers from the Alzheimer clinic, the probability of using hospice increased as caregiving intensity increased, but this relationship was reversed in caregivers from the day-care center (Wald χ28 = 23.05, P = .003). With the exception of education, this interaction did not substantially alter the risk of hospice use associated with other variables in the model (Table 2, Model 3). The Hosmer and Lemeshow test indicated good fit in the logistic regression model (χ28 = 5.20, P = .74). Figure 3 graphically displays these results and shows that, regardless of gender, as caregiving time increases over 25 hours per week, the probability of hospice use increases for care recipients with AD attending the Alzheimer clinic compared with those attending the day-care center.
FIGURE 3.
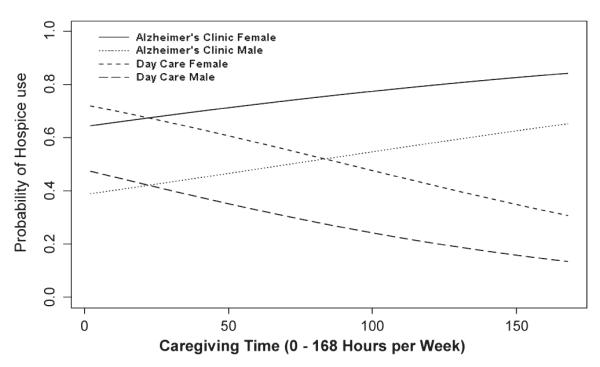
Probability of hospice use by total caregiving time per week (model based on age of 80 years, 12 years of education, white race, and Rosow-Breslau score of 2).
DISCUSSION
In this secondary analysis, we examined whether community characteristics and caregiver characteristics were associated with hospice use at the end of life among older people with AD, after controlling for the effect of care-recipient characteristics. Guided by the Hospice Use Model, we hypothesized that caregiver predisposing, need, and enabling factors and community safety-net services (community services) would be significantly associated with hospice use prior to death.
Similar to other studies, our study found that the probability of hospice use varied with care recipient’s age,5 education,7 gender,5 race,5-8 and level of functional disability.27 However, the direction of association of these variables with hospice use was not always consistent with what we found. For example, in a study of patients with cancer, the authors found that lower levels of functional dependency were associated with greater use of hospice before death,27 whereas our study of patients with AD found the opposite relation of functional dependency to hospice use. Unlike other studies,5,6 ours found that caregiver demographic factors and measures of caregiving burden, health, and work did not influence hospice use prior to death among people with AD. There was substantial variation in each of the caregiver measures, suggesting that lack of variation was not the reason for lack of a significant association of these variables with hospice use.
The community-services variable was significantly associated with hospice use. Specifically, care recipients recruited from the Alzheimer clinic were more likely to use hospice compared with those recruited from day-care centers, noting that care recipients recruited from the clinic were not concurrently attending day care. In addition, there was a significant interaction between hours of care provided each week and recruitment site (Alzheimer clinic or day-care center). In brief, care recipients from the Alzheimer clinic requiring more than 25 hours of care each week had a higher probability of using hospice, a formal service, compared with care recipients from the adult day-care centers. However, results of this interaction must be interpreted with caution because of the number of comparisons involved and interactions can produce small groups with idiosyncratic results. Therefore, the significant interaction we report may be due to chance.
Implications of findings about differences in hospice use between the Alzheimer clinic and adult day-care centers suggest that there are alternative interpretations. One explanation may be that adult day-care centers provide services that support caregivers as care intensity increases, thus reducing caregivers’ perception of need for hospice care. In a previous analysis using this same sample, more day-care use was associated with lower use of home-based formal services over time, suggesting that adult day-care services may substitute for specific types of home-based formal services.28
Another explanation may be that the Alzheimer clinic was more likely than adult day-care centers to refer caregivers to hospice services. The Alzheimer clinic provides comprehensive evaluation and care management of people with AD. This includes a medical and neurological examination offered by a physician, diagnostic tests, and case management with a nurse practitioner, among others. Multidisciplinary staff in Alzheimer clinics may better understand that AD is a progressive and ultimately terminal illness. Therefore, they work closely with caregivers to address the changing needs of the individual with AD, suggesting that hospice is introduced as an appropriate option at the end of life.
Adult day-care centers, on the other hand, care for older adults with a variety of chronic conditions, including AD. The overall objective is to provide older adults an opportunity to get out of the house, receive mental and social stimulation, and allow caregivers to take a break to attend to personal or other needs. Adult day-care centers function using one or a combination of the following models: social, medical, or specialized.29 Adult day-care centers that use either a combination social and medical model where skilled nursing services are offered29 or a specialized model that targets individuals with dementia29 may be more likely to meet the needs of people with AD, including referral to hospice.
Staff of adult day-care centers that use a purely social model are less likely to view AD as a terminal illness and may be less likely to discuss hospice as an option with caregivers. Although most adult day-care centers provide services for individuals with late-stage AD, only 4.3% of the centers reported they “work with hospice programs.”30 These results suggest a need for adult day-care centers to partner with hospice programs within the community to coordinate and ensure that appropriate hospice services are offered to individuals with AD at the end of life.
Our study has several limitations. First, the question about hospice use was asked only of caregivers whose care recipients had died during the study period so the sample was limited to those who died, and we did not capture hospice use among care recipients who were alive when the study ended. Second, caregivers’ self-report of hospice use did not include information about when hospice enrollment occurred, the type of hospice service used, or length of stay in hospice. Third, our ability to test some aspects of the Hospice Use Model was limited by our reliance on previously collected data. For example, caregiver factors known to influence hospice use such as knowledge of hospice, previous experience with hospice, and whether a hospice referral was made31 were not available in the primary data. Fourth, the study sample was limited in comparison to the number of variables tested. It is possible that lack of association of some variables that were associated with hospice use in other studies was due to insufficient power in this study. The importance of interactions is particularly questionable given the small sample size. Finally, the sample size was small and limited to a convenience sample of informal caregivers of community-dwelling care recipients with AD in a defined geographic area, limiting the external validity of the study findings. Findings from this study cannot be generalized to all community-dwelling persons with AD.
The primary strength of this study is that it used a comprehensive health services model, the Hospice Use Model, to examine predictors of hospice use at the end of life in individuals with AD. In addition, we used data from a time period substantially longer than 6 months before the care recipient’s death, which is the standard time covered under the Medicare hospice benefit. This allowed us to examine predictors of hospice use from 8 to 16 months before the care recipient’s death. Evidence suggests that it is challenging to define the end-of-life period for people with dementia,32,33 that dementia patients tend to have the longest lengths of stay in hospice,3,34 and that Medicare guidelines may not be valid predictors of survival in hospice patients with dementia.35 The progressive and terminal nature of AD qualifies it as a condition appropriate for hospice care, yet hospice is underutilized in this group. Our data may be useful in the design and implementation of interventions and policies aimed at optimal use of hospice in persons with AD. Although the use of secondary data limited our ability to examine all factors in the Hospice Use Model, results from this study highlight factors associated with hospice use in persons with AD. Our results suggest that community, caregiver, and care-recipient factors influence hospice use prior to death. As such, we need to be more aware of these factors when designing future interventions focused on increasing hospice use among people with AD.
In addition, the Hospice Use Model provides a comprehensive framework for future studies of hospice in a variety of health conditions. Use of a common framework will permit replications and comparisons of study findings to advance the science of hospice use and hospice outcomes. More importantly, it provides policy makers and hospice administrators a better understanding of community services, caregiver, and care-recipient factors that might influence hospice use among people with AD, to inform the Medicare hospice benefit program.
Acknowledgments
The authors thank Rosemary Camilleri, PhD, for editorial assistance. They also thank Mr Todd Beck for statistical programming.
This study was supported by the Longitudinal Study of Day Care in Alzheimer’s Disease (R01 AG10315).
Footnotes
The authors have no conflict of interest to disclose.
This article was accomplished by authors Ms Karikari-Martin’s and Dr Haffer’s personal capacity. The opinions expressed in this article are the authors’ own and do not reflect the views of the Centers for Medicare & Medicaid Services, the Department of Health and Human Services, the US Government, College of Nursing, Rush University Medical Center, Chicago, IL, or Rush Institute for Healthy Aging.
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Pauline Karikari-Martin, College of Nursing, Rush University Medical Center, Chicago, Illinois; US Public Health Service, Rockville, Maryland; Centers for Medicare & Medicaid Services, Baltimore, Maryland..
Judith J. McCann, College of Nursing, Rush Institute for Healthy Aging, Rush University Medical Center, Chicago, Illinois..
Liesi E. Hebert, Rush Institute for Healthy Aging, Rush University Medical Center, Chicago, Illinois..
Samuel C. Haffer, Centers for Medicare & Medicaid Services, Baltimore, Maryland..
Marcia Phillips, College of Nursing, Rush University Medical Center, Chicago, Illinois..
References
- 1.Alzheimer’s Association [Accessed December 16, 2010]; Updated 2010. http://www.alz.org/alzheimers_disease_what_is_alzheimers.asp.
- 2.Kochanek KD, Xu J, Murphy SL, Miniño AL, Kung H. [Accessed September 21, 2011];Deaths: preliminary data for 2009. Natl Vital Stat Rep. 2011 59(4):1–51. http://www.cdc.gov/nchs/data/nvsr/nvsr59/nvsr59_04.pdf. [PubMed] [Google Scholar]
- 3.Jennings B, Ryndes T, D’Onofrio C, Baily MA. What is hospice care? Hastings Center Rep (Special Suppl) 2003;33:S7. [PubMed] [Google Scholar]
- 4.National Hospice and Palliative Care Organization [Accessed February 28, 2011];NHPCO Facts and Figures: Hospice Care in America. Updated 2010. http://www.nhpco.org/files/public/Statistics_Research/Hospice_Facts_Figures_Oct-2010.pdf.
- 5.Connor SR, Elwert F, Spence C, Christakis NA. Geographic variation in hospice use in the United States in 2002. J Pain Symptom Manage. 2007;34(3):277–285. doi: 10.1016/j.jpainsymman.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 6.Forcina Hill J. Factors associated with hospice use after referral. J Hosp Palliat Nurs. 2008;10(4):240–525. [Google Scholar]
- 7.Greiner KA, Perera S, Ahluwalia JS. Hospice usage by minorities in the last year of life: results from the National Mortality Followback Survey. J Am Geriatr Soc. 2003;51(7):970–978. doi: 10.1046/j.1365-2389.2003.51310.x. [DOI] [PubMed] [Google Scholar]
- 8.Locher JL, Kilgore ML, Morrisey MA, Ritchie CS. Patterns and predictors of home health and hospice use by older adults with cancer. J Am Geriatr Soc. 2006;54(8):1206–1211. doi: 10.1111/j.1532-5415.2006.00833.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Iwashyna TJ, Zhang JX, Christakis NA. Disease-specific patterns of hospice and related healthcare use in an incidence cohort of seriously ill elderly patients. J Palliat Med. 2002;5(4):531–538. doi: 10.1089/109662102760269760. [DOI] [PubMed] [Google Scholar]
- 10.Van Houtven CH, Taylor DH, Jr, Steinhauser K, Tulsky JA. Is a home-care network necessary to access the Medicare hospice benefit? J Palliat Med. 2009;12(8):687–694. doi: 10.1089/jpm.2008.0255. [DOI] [PubMed] [Google Scholar]
- 11.Prigerson HG. Determinants of hospice utilization among terminally ill geriatric patients. Home Health Care Serv Q. 1991;12(4):81–112. doi: 10.1300/j027v12n04_07. [DOI] [PubMed] [Google Scholar]
- 12.Vig EK, Starks H, Taylor JS, Hopley EK, Fryer-Edwards K. Why don’t patients enroll in hospice? Can we do anything about it? J Gen Intern Med. 2010;25(10):1009–1019. doi: 10.1007/s11606-010-1423-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang AY, Zyzanski SJ, Siminoff LA. Differential patient-caregiver opinions of treatment and care for advanced lung cancer patients. Soc Sci Med. 2010;70(8):1155–1158. doi: 10.1016/j.socscimed.2009.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Davidson PL, Andersen RM, Wyn R, Brown ER. A framework for evaluating safety-net and other community-level factors on access for low-income populations. Inquiry. 2004;41(1):21–38. doi: 10.5034/inquiryjrnl_41.1.21. [DOI] [PubMed] [Google Scholar]
- 15.Radina ME, Barber CE. [Accessed February 25, 2011];Utilization of formal support services among Hispanic Americans caring for aging parents. J Gerontol Soc Work. 2004 43(2):5. http://www.informaworld.com/10.1300/J083v43n02_02. [Google Scholar]
- 16.Ogle KS, Mavis B, Wyatt GK. Physicians and hospice care: attitudes, knowledge, and referrals. J Palliat Med. 2002;5(1):85–92. doi: 10.1089/10966210252785042. [DOI] [PubMed] [Google Scholar]
- 17.Keating NL, Landrum MB, Rogers SO, Jr, et al. Physician factors associated with discussions about end-of-life care. Cancer. 2010;116(4):998–1006. doi: 10.1002/cncr.24761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Born W, Greiner KA, Sylvia E, Butler J, Ahluwalia JS. Knowledge, attitudes, and beliefs about end-of-life care among inner-city African Americans and Latinos. J Palliat Med. 2004;7(2):247–256. doi: 10.1089/109662104773709369. [DOI] [PubMed] [Google Scholar]
- 19.McCann JJ, Hebert LE, Li Y, et al. The effect of adult day care services on time to nursing home placement in older adults with Alzheimer’s disease. Gerontologist. 2005;46(6):754–763. doi: 10.1093/geront/45.6.754. [DOI] [PubMed] [Google Scholar]
- 20.Folstein MF, Folstein SE, McHugh PR. “Mini-Mental State”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 21.Katz S, Akpom CA. A measure of primary sociobiological functions. Int J Health Serv. 1976;6(3):493–508. doi: 10.2190/UURL-2RYU-WRYD-EY3K. [DOI] [PubMed] [Google Scholar]
- 22.Rosow I, Breslau N. A Guttman health scale for the aged. J Gerontol. 1966;21(4):556–559. doi: 10.1093/geronj/21.4.556. [DOI] [PubMed] [Google Scholar]
- 23.Nagi SZ. An epidemiology of disability among adults in the United States. Milbank Mem Fund Q Health Soc. 1976;54(4):439–467. [PubMed] [Google Scholar]
- 24.Lawton MP, Moss M, Kleban MH, Glicksman A, Rovine M. A two-factor model of caregiving appraisal and psychological well-being. J Gerontol. 1991;46(4):181–189. doi: 10.1093/geronj/46.4.p181. [DOI] [PubMed] [Google Scholar]
- 25.Kohout FJ, Berkman LF, Evans DA, Cornoni-Huntley J. Two shorter forms of the CES-D (Center for Epidemiological Studies Depression) depression symptoms index. J Aging Health. 1993;5(2):179–193. doi: 10.1177/089826439300500202. [DOI] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention [Accessed March 11, 2011];2000 Measuring healthy days. http://www.cdc.gov/hrqol/pdfs/mhd.pdf.
- 27.Tang ST. Determinants of hospice home care use among terminally ill cancer patients. Nurs Res. 2003;52(4):217–225. doi: 10.1097/00006199-200307000-00003. [DOI] [PubMed] [Google Scholar]
- 28.Skarupski KA, McCann JJ, Bienias JL, Wolinsky FD, Aggarwal NT, Evans DE. Use of home-based formal services by adult day care clients with Alzheimer’s disease. Home Health Care Serv Q. 2008;27(3):217–239. doi: 10.1080/01621420802320009. PMCID:PMC2745645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.O’Keeffe J, Siebenaler K. [Accessed April 6, 2011];Adult day services: a key community service for older adults. 2006 Contract HHS-100-03-0025:1-81. http://aspe.hhs.gov/daltcp/reports/2006/keyADS.pdf.
- 30.Silverstein NM, Wong CM, Brueck KE. [Accessed April 6, 2011];Living with Alzheimer’s disease: a study of adult day health services in Massachusetts. 2008 :1–36. http://www.nadsa.org/assets/library/313_alzheimersresearchmaadhc.pdf.
- 31.Chung K, Essex E, Samson L. Does caregiver knowledge matter for hospice enrollment and beyond? Pilot study of minority hospice patients. Am J Hosp Palliat Care. 2009;26(3):165–171. doi: 10.1177/1049909109331883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Doberman DJ, Yasar S, Durso SC. Would you refer this patient to hospice? An evaluation of tools for determining life expectancy in end-stage dementia. J Palliat Med. 2007;10(6):1410–1419. doi: 10.1089/jpm.2007.9838. [DOI] [PubMed] [Google Scholar]
- 33.Marsh GW, Prochoda KP, Pritchett E, Vojir CP. Predicting hospice appropriateness for patients with dementia of the Alzheimer’s type. Appl Nurs Res. 2000;13(4):187–196. doi: 10.1053/apnr.2000.7654. [DOI] [PubMed] [Google Scholar]
- 34.Hospice Association of America [Accessed January 31, 2011];Hospice Facts & Statistics. http://www.nahc.org/facts/HospiceStats10.pdf. Updated 2010.
- 35.Schonwetter RS, Han B, Small BJ, Martin B, Tope K, Haley WE. Predictors of six-month survival among patients with dementia: an evaluation of hospice Medicare guidelines. Am J Hosp Palliat Care. 2003;20(2):105–113. doi: 10.1177/104990910302000208. [DOI] [PubMed] [Google Scholar]