Abstract
Objectives
While validated suicide screening tools exist for use among children and adolescents presenting to emergency departments (EDs), the associations between screening positive for suicide risk and immediate psychiatric hospital admission or subsequent ED utilization, stratified by age, have not been examined.
Methods
A retrospective cohort study of a consecutive case series of patients aged 8–18 years presenting with psychiatric chief complaints over a 9 month period to a single urban tertiary care pediatric ED. Eligible patients were administered a subset of questions from the Risk of Suicide Questionnaire. Outcomes included the odds of psychiatric hospitalization at the index visit and repeat ED visits for psychiatric complaints within the following year, stratified by age.
Results
Of the 568 patients presenting during the study period, responses to suicide screening questions were available for 442 patients (78%). A total of 159/442 (36%) were hospitalized and 130/442 (29%) had one or more ED visits within the following year. The proportion of patients providing positive responses to one or more suicide screening questions did not differ between patients aged 8–12 years and those aged 13–18 years [77/154 (50%) vs. 137/288 (48%), p = .63]. A positive response to one or more of the questions was significantly associated with increased odds of psychiatric hospitalization in the older age group [adj OR = 3.82 (95% CI 2.24–6.54)] and with repeat visits to the ED in the younger age group [adj OR = 3.55 (95% CI 1.68–7.50)].
Conclusions
Positive responses to suicide screening questions were associated with acute psychiatric hospitalization and repeat ED visits. Suicide screening in a pediatric ED may identify children and adolescents with increased need of psychiatric resources.
Keywords: suicide, screening, psychiatric emergency
INTRODUCTION
Identification of children and adolescents at risk for suicide in emergency departments (EDs) is a national concern.1,2 Increasing numbers of youth utilize the ED for mental health care,3 and the most common psychiatric-related presenting concern for these children and adolescents is suicidal ideation and behavior.4 Young people with such complaints are at greater risk to die by suicide than adolescents who present to the ED for other reasons.5 As a result, systematic screening for suicide risk in EDs has been proposed to connect at-risk youth with appropriate resources.6,7
Age is an important consideration in screening for suicide risk; specifically, how young is too young to be screened? Because suicide is a leading cause of death in adolescents,8 suicidal adolescents (ages 13–18 years) have been the focus of surveillance,9 screening6,7 and intervention efforts.10 In contrast, little data exist on suicidality in children younger than 12 years.11 Although death by suicide is rarely reported in children under the age of 12, suicide and suicide attempts do occur in this age group.11,12 Furthermore, researchers suggest that suicidal behavior in this younger population may often be mislabeled as accidental, and thus under-reported.12 While screening for suicide risk in children under the age of 12 years may identify new cases for clinical management, there are few resources to aid clinicians in the assessment of suicidal thoughts and behaviors in these children. Additionally, the association of suicidal thoughts and behaviors before age 12 with healthcare utilization outcomes such as psychiatric hospitalization and repeated hospital visits are not known.
An important obstacle to screening both children and adolescents for suicide risk in the ED has been a lack of validated suicide screening instruments. In 2001, Horowitz and colleagues developed a brief suicide screening tool, the Risk of Suicide Questionnaire (RSQ), for use with patients ages 8 to 21 years who present to ED triage with psychiatric chief complaints.13 The RSQ was validated utilizing the Suicide Ideation Questionnaire14 as a gold standard. It consists of four questions:
Are you here today because you tried to hurt yourself?
In the past week, have you been having thoughts about killing yourself?
Have you ever tried to hurt yourself in the past (other than this time)?
Has something very stressful happened to you in the past few weeks (a situation very hard to handle)?
Whereas the original RSQ validation sample included children as young as eight years, there was no stratification of the data by age. Additionally, the validation study did not investigate the relationship between responses to RSQ questions and immediate psychiatric hospitalization or repeated ED visits. Associations between positive responses to suicide screening items and healthcare utilization have implications for how EDs assess, manage and treat patients at increased suicide risk.
Therefore, the purpose of this study was to evaluate whether suicide screening items from the RSQ could predict psychiatric hospitalization at the index visit and repeated ED visits when they were regularly administered in a pediatric ED setting. In particular, the study aimed to evaluate whether the association of the RSQ with these outcomes when administered by nurses at triage differed between samples of younger (8–12 years) and older (13–18 years) ED patients.
MATERIALS AND METHODS
We performed a retrospective cohort study of a consecutive case series of patients who were residents of the District of Columbia (DC) aged 8–18 years. Each eligible patient presented with a psychiatric chief complaint to the pediatric ED at Children’s National Medical Center (CNMC) in Washington DC from September 1, 2007 to May 17, 2008. The selected study period was when screening questions from the RSQ were routinely administered by triage nurses in the CNMC ED. CNMC is an urban tertiary care, academic pediatric medical center with an annual patient volume which exceeded 75,000 visits during the study period. CNMC is the site of >75% of all ED visits made by children and adolescents living in DC.15 No patients were excluded on the basis of gender, minority status or insurance type. The Institutional Review Board at CNMC approved the study.
Screening Measure
The Risk of Suicide Questionnaire (RSQ) is a psychometrically validated four-item suicide screening instrument13 designed to be administered by triage nurses in the ED to children and adolescents aged 8–21 years. A “yes” response to any of the four questions is considered to be a positive screen. This instrument was created utilizing data from 144 young patients entering an urban pediatric teaching hospital for psychiatric reasons. The tool was validated using a “gold standard” assessment for suicidal ideation, the Suicidal Ideation Questionnaire (SIQ), a 30-item suicide assessment for patients in 10th grade and above, and the SIQ-Jr,14 a 15-item suicide assessment for those patients in seventh through ninth grade. Reported psychometric properties of the RSQ include a sensitivity of 98%, a specificity of 37%, positive predictive value of 55%, a negative predictive value of 97%, and a c-statistic of .87.11
Procedures
We performed a retrospective chart review by first querying the ED’s electronic patient database to identify patients presenting with psychiatric chief complaints during the study period, September 1, 2007 to May 17, 2008. The patient’s first visit during the study period was considered the index visit; all subsequent visits after the initial visit were counted as repeat visits. From this electronic database, eligible patients’ ages, gender, presenting complaints, dispositions, diagnoses, insurance types, residential zip codes, and lengths of stay were extracted. Each medical record was then individually reviewed to determine race, ethnicity, foster care status, type of hospitalization and suicide screening responses.
Of note, not all four suicide screening questions were asked at each visit due to the existence of different suicide screening forms during the study period. Specifically, the RSQ question “has something very stressful happened to you in the past few days, a situation very hard to handle?” was not administered at all visits. The cohort was examined with (n = 177) and without (n = 442) responses to this question included.
The number of ED visits by each participant over the year after the index visit were recorded, with presenting complaints and discharge diagnosis. These additional visits were coded by two independent raters as a psychiatric visit or non-psychiatric visit according to presenting chief complaint and discharge diagnoses. Inter-rater agreement ranged from 84%–97%. Any discrepancies in coding were settled by consensus.
Statistical Analysis
The statistical package SPSS version 15.0 was used to conduct all quantitative analyses. Univariate regression analysis was used for the descriptive statistics. As the dependent variable was dichotomous, logistic regression was used. Guidance on performing logistic regression was obtained from Peng’s synopsis of logistic regression in psychosocial research.16 Variables entered into the model included suicide screening positive, gender, foster care status, insurance status and race; variables were chosen as they have a demonstrated association with healthcare utilization 17–19 and/or suicide risk20. Odds ratios are presented with 95% confidence intervals (CIs). P-values of less than .05 were considered to be statistically significant.
Sample Size
In the original study developing and validating the RSQ, the overall positive response rate was 40%. In univariate analysis, the available sample for each age group (154 in the 8–12 year age group and 288 in the 13–18 year age group) provides 83% power to detect a 15% absolute difference in the rates of a positive suicide screen between the two groups (two-sided, alpha = 0.05).
RESULTS
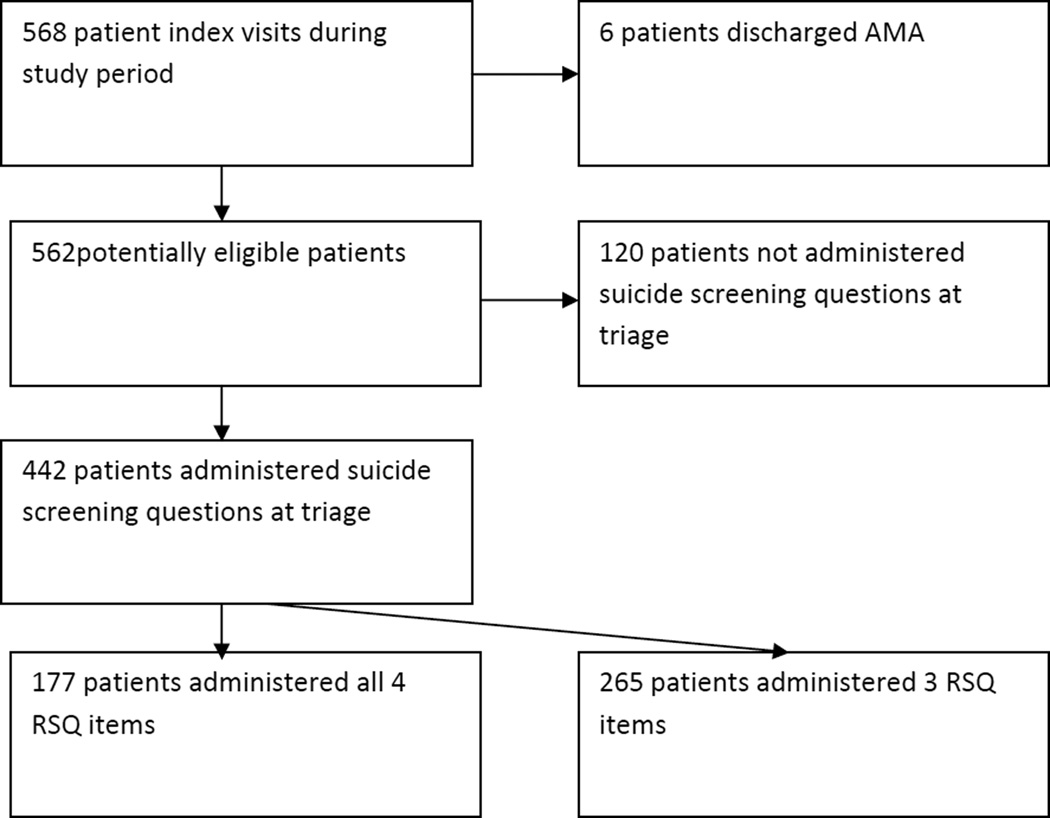
Of 568 potentially eligible patients making index visits during the study period, six left the ED against medical advice. Of the remaining 562, 442 (79%) had either three (265/442, 60%) or four (177/442, 40%) of the RSQ questions asked at triage (Figure). There were no significant differences between those who were administered suicide screening questions (n = 442) and those who were not (n = 120) in the following categories: age [mean age of 13 in both age groups, p = .72], gender [56/120 (47%) female compared to 208/442 (47%) female, p = .94] race/ethnicity, [109/120 (91%) African American compared to 404/442 (91%) African American, p = .85] insurance type [106/120 (88%) public insurance compared to 376/442 (85%) public insurance, p = .36], foster care status [20/120 (17%) compared to 92/442 (21%), p = .31] or psychiatric hospitalization [33/120 (28%) compared to 159/442 (36%), p = .08]. All hospitalizations related to the index ED visit were for psychiatric indications. The majority of psychiatric complaints were generally classified as requiring “psychiatric evaluation” (317/442, 71%). Suicidal thoughts or behaviors were listed in 73 (17%) of the 442 discharge diagnoses [23/154 (15%) in the younger age group and 50/288 (17%) in the older age group].
FIGURE 1.
Study flow
For the 442 patients included in this study, 47% were female and 91% were African American. The median age of the study sample was 14 years [IQR = 11–15]. Demographic information, stratified by age, is further presented in Table 1. There were no differences between age groups in race/ethnicity, foster care, insurance status or disposition. Patients in the younger age group were more likely to be male (73% among younger patients vs. 42% among older patients, p < .01).
Table 1.
Frequencies for Demographic Factors Stratified by Age
| Total sample (n = 442) |
8–12 years ( n =154) |
13–18 years (n = 288) |
|||||
|---|---|---|---|---|---|---|---|
| Characteristic | n | % | n | % | n | % | P |
| Gender | |||||||
| Male | 234 | 53 | 113 | 73 | 121 | 42 | <.001 |
| Female | 208 | 47 | 41 | 27 | 167 | 68 | |
| Race/Ethnicity | |||||||
| African American | 404 | 91 | 139 | 90 | 265 | 92 | .53 |
| Other Race/Ethnicity | 38 | 9 | 15 | 10 | 23 | 8 | |
| Insurance Type | |||||||
| Public or No Insurance | 376 | 85 | 138 | 90 | 238 | 83 | .05 |
| Private Insurance | 66 | 15 | 16 | 10 | 50 | 17 | |
| Foster Care | |||||||
| Not in Foster Care | 350 | 79 | 126 | 82 | 224 | 78 | .32 |
| In Foster Care | 92 | 21 | 28 | 18 | 64 | 22 | |
| Disposition | |||||||
| Discharged | 283 | 64 | 99 | 64 | 184 | 64 | .93 |
| Admitted | 159 | 36 | 55 | 36 | 104 | 36 | |
Responses to suicide screening questions are presented in Table 2. There was a significant difference by age in the proportion of positive responses to “Have you ever tried to hurt yourself in the past?” [23% among younger patients vs. 33% among older patients, p=0.04]. There was no difference by age to the other suicide screening items. Overall positive screens did not differ between the younger and older patients [77/154 (50%) vs. 137/288 (48%), p = .63].
Table 2.
Positive responses to questions from the RSQ stratified by Age
| Variable | 8–12 years (n= 154) N(%) |
13–18 years (n = 288) N(%) |
p |
|---|---|---|---|
| Are you here because you tried to hurt yourself? | 34(22%) | 63(22%) | .91 |
| In the past week, have you been having thoughts about killing yourself? | 41(27%) | 71(25%) | .61 |
| Have you ever tried to hurt yourself in the past (other than this time)? | 35(23%) | 94(33%) | .04 |
| Positive response to at least one of the previous three items | 77(50%) | 137(48%) | .63 |
| **Has something very stressful happened to you in the past few weeks (a situation very hard to handle)? | 23(44%) | 62(50%) | .09 |
This question was asked on only 177 patient visits.
Hospitalization
Of the entire patient sample, 159/442 (36%) were hospitalized for psychiatric reasons on the index visit. For the younger age group (Table 3), being in foster care was significantly associated with increased odds of psychiatric hospitalization (adj OR = 4.27, 95% CI 1.74–10.47). For the older age group, screening positive on one or more of the three suicide questions was significantly associated with increased odds of hospitalization (adj OR = 3.82, 95% CI 2.24–6.54).
Table 3.
Logistic Regression Analysis of Hospitalization Stratified by Age
| 8–12 years (n = 154) |
13–18 years (n = 288) |
|||
|---|---|---|---|---|
| Predictor | Adjusted Odds Ratio |
95% CI | Adjusted Odds Ratio |
95% CI |
| Positive Suicide Screen* | 1.99 | [.95–4.17] | 3.82 | [2.24–6.54] |
| Male gender | 1.22 | [0.55–2.70] | 1.65 | [.96–2.82] |
| Foster Care Status | 4.27 | [1.74–10.47] | 1.14 | [.61–2.19] |
| Public or no insurance | 1.38 | [0.40–4.81] | 0.91 | [.46–1.81] |
| African American Race | 0.76 | [0.24–2.41] | 0.83 | [.34–2.15] |
At least one “yes” to the three-item RSQ
Repeat ED Visits
Of the entire patient sample, 130/442 (29%) returned to the ED within one year of their index visit for a psychiatric reason. For the younger age group (Table 4), screening positive on one or more of the three suicide screening questions was significantly associated with increased odds of returning to the ED for a psychiatric reason (adj OR = 3.55, 95% CI 1.68–7.50) as was being in foster care (adj OR = 2.89, 95% CI 1.17–7.17). For the older age group, being on public insurance was significantly associated with increased odds of a repeat visit (adj OR = 2.99, 95% CI 1.22–7.33).
Table 4.
Logistic Regression Analysis of Psychiatric ED Visits within One Year, Stratified by Age
| 8–12 years (n = 154) |
13–18 years (n = 288) |
|||
|---|---|---|---|---|
| Predictor | Adjusted Odds Ratio |
95% CI | Adjusted Odds Ratio |
95% CI |
| Positive Suicide Screen* | 3.55 | [1.68–7.50] | 1.25 | [0.71–2.19] |
| Male gender | 1.19 | [0.54–2.62] | 1.35 | [0.77–2.36] |
| Foster Care Status | 2.89 | [1.17–7.17] | 0.73 | [0.37–1.43] |
| Public or no insurance | 0.84 | [0.25–2.83] | 2.99 | [1.22–7.33] |
| African American Race | 3.39 | [0.86–13.41] | 0.41 | [0.16–1.04] |
At least one “yes” to the three-item RSQ
Four-Item RSQ
Finally, we ran the same model in the smaller sample of patients (n =177) who were administered all four RSQ questions during the ED triage process. There were 32/177 (18%) patients who did not screen positive on the first 3 RSQ items, but endorsed the fourth item, “Has something very stressful happened to you in the past few weeks?” When the same model was run with the 177 participants, foster care status was no longer associated with repeated visits for psychiatric reasons in the younger age group and no variable was significantly associated with repeated psychiatric ED visits in the older age group.
DISCUSSION
The current study, through an ED medical record review, investigated the association of positive responses to suicide screening questions in predicting psychiatric hospitalization on index visit and repeat ED visits for psychiatric complaints in the year following the index visit. We found that a positive suicide screen was associated with psychiatric hospitalization in the patient sample in the older age group (13–18 years), but not the younger age group (8–12 years). Foster care was associated with both psychiatric hospitalization and repeated ED visits in the younger patient sample. A positive suicide screen was also associated with repeat ED visits for psychiatric reasons in the younger patients, but not the older patients. Having public insurance was associated with repeated visits in the older patient sample.
Suicide screening appears to be a useful measurement tool in the prediction of service variables in a pediatric ED. These findings have implications for patient management, flow and ED staffing, including the implementation of clinical practice guidelines, such as connecting a patient who screens positive for suicide risk to specific actions (searching for weapons, obtaining an observational monitor while the patient is in the ED, or requiring a psychiatric evaluation). Additionally, these findings have implications for future ED research. The use of validated suicide screening instruments can also allow for multi-site research on suicidal thoughts and behaviors across ED settings. This ED sample included a high proportion of African American youth, individuals in foster care and families on public assistance when compared to the initial validation sample; populations with these demographics are not often the focus of suicide research, but may be at-risk for suicidal thoughts and behaviors.22 Prospective studies with larger and more diverse samples could uncover trends in hospitalization and, in particular, repeated ED visits, which strain already overburdened healthcare resources.17,23,24
Of note, there were few differences in responses to suicide screening questions between the two age groups. Responses differed on the question, “have you ever tried to hurt yourself in the past,” which is expected, as younger patients have had less time to engage in self-harm behaviors. In the younger age group, a positive response to suicide screening questions was associated with additional ED visits for psychiatric complaints in the following year, indicating that younger children who endorse suicidal thoughts may be in particular need of mental health resources and follow-up; however, repeated visits can also be related to differences in primary care physician referral practices or the availability of inpatient resources for this population. Developmentally, younger children have a different understanding of death, suicide, lethal means and coping skills than adolescents and adults,21 which will affect how clinical assessments and interventions are implemented. Of note, over the course of the study period, nurses screened 50 patients for suicide risk between the ages of 5 and 7. While the RSQ is not a validated instrument for this age group, interestingly, 27 (54%) of these patients screened positive for suicide risk. While further discussion is beyond the scope of this paper, this finding, in combination with other results highlights that patients under the age of 12 years report suicidal thoughts and behaviors when asked, emphasizing the need for further research on clinical guidelines for identifying and managing suicide risk specifically in this population.
This study has several limitations. First, it utilized a retrospective approach that suffered from an inconsistent application of the RSQ in the study population. The utility of the omitted RSQ item has been questioned in other retrospective evaluation studies.25,26 Moreover, in a recent study designed to create an updated version of the RSQ for both psychiatric and non-psychiatric patients, the fourth item was re-compared the SIQ. 27 After further analyses, this item was deleted from the most recent version, due to decreased sensitivity and specificity.27 Second, it is possible that patients attended the CNMC ED in the year before their index visit or other EDs after their index visit, resulting in our underestimating repeated ED visits. Of note, however, CNMC accounted for over 75% of all pediatric ED visits made by DC residents in 2007.15 Third, 135 of the 627 eligible patients (21.3%) were not asked the suicide screening questions during the triage process, which may have biased the findings although there were no demographic differences in these two groups. Fourth, these findings are from a single urban pediatric center with a unique patient population, outpatient services and procedures for psychiatric hospitalization and may not be generalizable to other populations and settings. Finally, RSQ items were administered at triage and often in the presence of a caregiver; it is not known whether responses would have differed if suicide screening items were administered in private.
Conclusions
In two populations of urban children and adolescents (aged 8–12 years and 13–18 years) presenting to a pediatric ED with psychiatric complaints, positive responses to suicide screening questions were common and associated with psychiatric hospitalization in the older age group and with repeated ED visits for psychiatric reasons in the younger age group. In addition, rates of positive responses to one or more of the suicide screening questions were similar between age groups, although older adolescents reported higher rates of hurting themselves in the past. Suicide screening of children and adolescents in the ED may identify patients in greatest need of mental health resources.
Acknowledgments
The research in this article was supported by the Intramural Research Program of the National Institutes of Health and the National Institute of Mental Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The opinions expressed in the article are the views of the authors and do not reflect the views of the Department of Health and Human Services or the United States government.
Contributor Information
Elizabeth D. Ballard, Department of Psychiatry and Behavioral Sciences, Johns Hopkins University School of Medicine.
Lisa M. Horowitz, Office of the Clinical Director, National Institute of Mental Health, NIH.
David A. Jobes, Department of Psychology, Catholic University of America.
Barry M. Wagner, Department of Psychology, Catholic University of America.
Maryland Pao, Office of the Clinical Director, National Institute of Mental Health, NIH.
Stephen J. Teach, Division of Emergency Medicine, Children’s National Medical Center.
REFERENCES
- 1.U.S. Department of Health and Human Services (HHS) Office of the Surgeon General and National Action Alliance for Suicide Prevention. 2012 National Strategy for Suicide Prevention: Goals and Objectives for Action. Washington, DC: HHS; 2012. Sep, [PubMed] [Google Scholar]
- 2.D’Onofrio G, Jauch E, Jagoda A, et al. NIH roundtable on opportunities to advance research on neurologic and psychiatric emergencies. Ann Emerg Med. 2010;56(5):551–564. doi: 10.1016/j.annemergmed.2010.06.562. [DOI] [PubMed] [Google Scholar]
- 3.Grupp-Phelan J, Harman JS, Kelleher KJ. Trends in mental health and chronic condition visits by children presenting for care at U.S. emergency departments. Public Health Rep. 2007;122(1):55–61. doi: 10.1177/003335490712200108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grupp-Phelan J, Mahajan P, Foltin GL, et al. Referral and resource use patterns for psychiatric-related visits to pediatric emergency departments. Pediatr Emerg Care. 2009;25(4):217–220. doi: 10.1097/pec.0b013e31819e3523. [DOI] [PubMed] [Google Scholar]
- 5.Crandall C, Fullerton-Gleason L, Aguero R, LaValley J. Subsequent suicide mortality among emergency department patients seen for suicidal behavior. Acad Emerg Med. 2006;13(4):435–442. doi: 10.1197/j.aem.2005.11.072. [DOI] [PubMed] [Google Scholar]
- 6.Horowitz L, Ballard ED, Pao M. Suicide screening in schools, primary care and emergency departments. Curr Opin Pediatr. 2009;21:620–627. doi: 10.1097/MOP.0b013e3283307a89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pena JB, Caine ED. Screening as an approach for adolescent suicide prevention. Suicide Life Threat Behav. 2006;36(6):614–637. doi: 10.1521/suli.2006.36.6.614. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention National Center for Injury Prevention and Control. [Accessed 10-8-12];Web-based Injury Statistics Query and Reporting System (WISQARS) Available at: www.cdc.gov/ncipc/wisqars.
- 9.Centers for Disease Control and Prevention. [Accessed 11-4-2012];Youth Risk Behavior Surveillance—United States. 2011 Available at: http://www.cdc.gov/mmwr/pdf/ss/ss6104.pdf.
- 10.Asarnow JR, Baraff LJ, Berk M, et al. An emergency department intervention for linking pediatric suicidal patients to follow-up mental health treatment. Psychiatr Serv. 2011;62(11):1303–1309. doi: 10.1176/appi.ps.62.11.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wyman PA, Gaudieri PA, Schmeelk-Cone K, et al. Emotional triggers and psychopathology associated with suicidal ideation in urban children with elevated aggressive-disruptive behavior. J Abnorm Child Psychol. 2009;37(7):917–928. doi: 10.1007/s10802-009-9330-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tishler CL, Reiss NS, Rhodes AR. Suicidal behavior in children younger than twelve: a diagnostic challenge for emergency department personnel. Acad Emerg Med. 2007;14(9):810–818. doi: 10.1197/j.aem.2007.05.014. [DOI] [PubMed] [Google Scholar]
- 13.Horowitz L, Wang PS, Koocher GP, et al. Detecting suicide risk in a pediatric emergency department: development of a brief screening tool. Pediatrics. 2001;107(5):1133–1137. doi: 10.1542/peds.107.5.1133. [DOI] [PubMed] [Google Scholar]
- 14.Reynolds W. Suicidal Ideation Questionnaire. Odessa, FL: Psychological Assessment Resources; 1987. [Google Scholar]
- 15.Chandra A, Gresenz CR, Blanchard JC, et al. Health and Health Care Among District of Columbia Youth. Santa Monica, CA: RAND Corporation, TR-751-CNMC; 2009. [Google Scholar]
- 16.Peng C-YJ, Nicols RN. Using multinomial logistic models to predict adolescent behavioral risk. J Mod App Stat Methods. 2003;2(1):177–188. [Google Scholar]
- 17.Huffman LC, Wang NE, Saynina O, et al. Predictors of hospitalization after an emergency department visit for California youths with psychiatric disorders. Psych Serv. 2012;63:896–905. doi: 10.1176/appi.ps.201000482. [DOI] [PubMed] [Google Scholar]
- 18.Riera A, Walker DM. The impact of race and ethnicity on care in the pediatricemergency department. Curr Opin Pediatr. 2010;22:284–289. doi: 10.1097/MOP.0b013e32833973a5. [DOI] [PubMed] [Google Scholar]
- 19.Goldstein AB, Frosch E, Davarya S, Leaf PJ. Factors associated with a six-month return to emergency services among child and adolescent psychiatric patients. Psych Serv. 2007;58:1489–1492. doi: 10.1176/ps.2007.58.11.1489. [DOI] [PubMed] [Google Scholar]
- 20.Bridge JA, Goldstein TR, Brent DA. Adolescent suicide and suicidal behavior. J Child Psychol Psychiatry. 2006;47:372–394. doi: 10.1111/j.1469-7610.2006.01615.x. [DOI] [PubMed] [Google Scholar]
- 21.Pfeffer CR. Diagnosis of childhood and adoelscent suicidal behavior: unment needs for suicide prevention. Biol Psychiatry. 2001;49(12):1055–1061. doi: 10.1016/s0006-3223(01)01141-6. [DOI] [PubMed] [Google Scholar]
- 22.Joe S, Baser RS, Neighbors HW, et al. 12-month and lifetime prevalence of suicide attempts among black adolescent sin the National Survey of American Life. J Am Acad Child Adolesc Psychiatry. 2009;48(3):271–282. doi: 10.1097/CHI.0b013e318195bccf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yu AY, Rosychuk RJ, Newton AS. Clinical acuity of repeat pediatric mental health presentations to the emergency department. J Can Acad Child Adolesc Psychiatry. 2011;20(3):208–213. [PMC free article] [PubMed] [Google Scholar]
- 24.Larkin GL, Beautrais AL. Emergency departments are underutilized sites for suicide prevention. Crisis. 2010;31(1):1–6. doi: 10.1027/0227-5910/a000001. [DOI] [PubMed] [Google Scholar]
- 25.Hopper SM, Woo JW, Sharwood LN, Babl FE, Long EJ. Prevalence of suicidality in asymptomatic adolescents in the paediatric emergency department and utility of a screening tool. Emergency Medicine Australasia. 2012 doi: 10.1111/j.1742-6723.2012.01576.x. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 26.Folse VN, Eich KN, Hall AM, Ruppman JB. Detecting suicide risk in adoelscents and adults in an emergency department: a pilot study. J Psychoc Nuse Ment Health Serv. 2006;44(3):22–29. doi: 10.3928/02793695-20060301-08. [DOI] [PubMed] [Google Scholar]
- 27.Horowitz L, Bridge JA, Teach SJ, et al. Ask Suicide-Screening Questions (ASQ)A Brief Instrument for the Pediatric Emergency Department. Arch Ped Adolesc Med. 2012;166(12):1170–1176. doi: 10.1001/archpediatrics.2012.1276. [DOI] [PMC free article] [PubMed] [Google Scholar]