Abstract
Background
Small intestinal bacterial overgrowth (SIBO) is an under-recognized diagnosis with important clinical implications when untreated. However, optimal treatment regimen remains unclear.
Aim
Systematic review and meta-analysis to compare clinical effectiveness of antibiotic therapies for treatment of symptomatic patients with documented SIBO.
Methods
Four databases were searched to identify clinical trials comparing effectiveness of: (1) different antibiotics, (2) different doses of the same antibiotic, and (3) antibiotics compared with placebo. Data were independently extracted according to predetermined inclusion and exclusion criteria. Study quality was independently assessed. Primary outcome was normalization of post-treatment breath testing. Secondary outcome was post-treatment clinical response.
Results
Of 1,356 articles identified, ten met inclusion criteria. Rifaximin was the most commonly studied antibiotic (8 studies) with overall breath test normalization rate of 49.5% (95% CI 44.0–55.1). Antibiotic efficacy varied by antibiotic regimen and dose. Antibiotics were more effective than placebo, with a combined breath test normalization rate of 51.1% (95% CI 46.7–55.5) for antibiotics compared with 9.8% (95% CI 4.6–17.8) for placebo. Meta-analysis of 4 studies favored antibiotics over placebo for breath test normalization with odds ratio 2.55 (95% CI 1.29–5.04). Clinical response was heterogeneously evaluated among six studies, but tended to correlate with breath test normalization.
Conclusions
Antibiotics appear to be more effective than placebo for breath test normalization in patients with symptoms attributable to SIBO, and breath test normalization may correlate with clinical response. Studies were limited by modest quality, small sample size, and heterogeneous design. Additional higher-quality clinical trials of SIBO therapy are warranted.
Keywords: small intestinal bacterial overgrowth, antibiotics, meta-analysis, systematic review
Introduction
Small intestinal bacterial overgrowth (SIBO) is an under-recognized diagnosis with varied and often protean manifestations.(1–3) Because the clinical presentation of SIBO can range from mild, non-specific symptoms (such as abdominal pain, bloating, and flatulence) to less common but severe manifestations (such as malabsorption, weight loss, and hypoalbuminemia), a delay in diagnosis is not uncommon.(2,4,5) Although epidemiologic data describing SIBO are limited, there appears to be increased prevalence of SIBO in patients with risk factors such as hypochlorhydria, gastroparesis or other motility disorders, anatomical abnormalities (such as small bowel diverticulosis), post-surgical state (such as ileocecal resection), small bowel mucosal disease, metabolic diseases (such as diabetes), and other chronic diseases (such as end stage renal disease, cirrhosis, chronic pancreatitis).(2,6,7) Prevalence in the elderly may be as high as 15%(3), and even higher among elderly patients with additional risk factors(3,8–10)
Treatment of SIBO typically includes antibiotics and, when possible, addressing underlying predisposing conditions.(11) Although a diagnosis of SIBO is often entertained and empirically treated among at-risk patients with gastrointestinal symptoms, comparison trials of antibiotic regimens remain disparate, and the optimal antibiotic regimen is not known. To address this important knowledge gap, we performed a systematic review to compare the effectiveness of antibiotics for achieving breath test normalization among symptomatic patients with documented SIBO. When feasible, we performed meta-analyses to further characterize the role of antibiotics in SIBO treatment.
Materials and Methods
Systematic Review and Study Selection
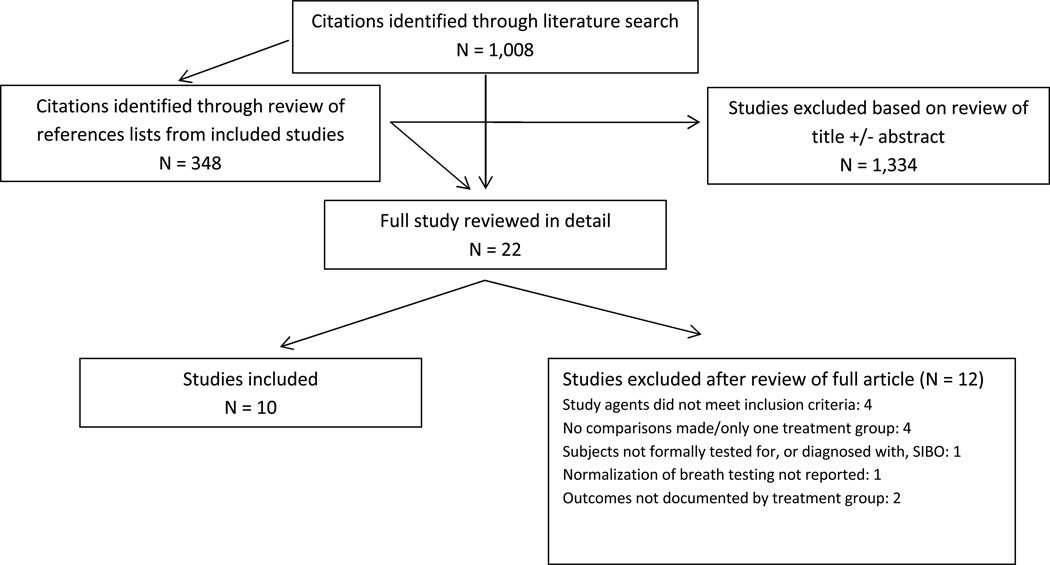
We performed a systematic review using four primary databases to identify clinical trials of antibiotic therapy among symptomatic patients with documented SIBO. No restrictions were applied to language or publication date. Databases searched were: (1) PubMed (original search date July 5, 2012; updated search July 3, 2013); (2) Web of Science (original search date July 5, 2012; updated search July 3, 2013); (3) Embase (original search date July 10, 2012; updated search July 3, 2013); and (4) Cochrane (search date July 3, 2013). Search strings were as follows. For PubMed: "bacterial overgrowth" OR "small intestinal bacterial overgrowth" OR "SIBO" AND Humans[Mesh] AND (Clinical Trial[ptyp] OR Comparative Study[ptyp] OR Randomized Controlled Trial[ptyp]). For Web of Science: clinical trial AND ("bacterial overgrowth" OR "small intestinal bacterial overgrowth" OR "SIBO"). For Embase: “bacterial overgrowth” OR sibo:ab,ti AND (“clinical trial”/exp OR “controlled study”/de OR “randomization”/de OR randomized:ab,ti) AND ([humans]/lim OR patient). For Cochrane: “small intestinal bacterial overgrowth”. We hand-searched reference lists from included studies to identify additional relevant studies for inclusion. Embase and Web of Science were used to search published abstracts. Because trials of SIBO therapy would likely be reported within several different types of professional society meetings (i.e., gastroenterology, infectious disease, general internal medicine, family medicine), we did not search the proceedings of any specific professional society meetings. See figure 1 for a summary of the literature search and study selection.
Figure 1.
Results of literature search.
Studies were eligible for inclusion if they reported prospective clinical trials of antibiotic therapy for documented SIBO among human subjects. We included trials comparing two or more antibiotics, trials comparing two or more dosing strategies for the same antibiotic, or trials comparing one or more antibiotics with placebo. Retrospective studies, case reports, and case series were excluded due to the high risk of publication bias. Although we did not plan to exclude studies based on language, our literature search did not produce any non-English studies meeting inclusion criteria. Table 1 details inclusion criteria, and figure 1 describes reasons for study exclusion.
Table 1.
Study inclusion criteria.
| Inclusion Criteria |
|---|
| Prospective clinical trial comparing two or more antibiotics, two or more doses of the same antibiotic, or comparing an antibiotic versus placebo, for the treatment of human subjects with documented SIBO |
| Primary study goal of evaluating medical therapy among symptomatic patients with SIBO |
| SIBO formally diagnosed with lactulose, glucose, sucrose, or xylose hydrogen or methane breath test, and/or quantitative small bowel culture |
| Study agents and dosing schedule clearly defined |
| “Cure” or “treatment response” defined as normalization of repeat hydrogen breath testing |
| Treatment outcomes clearly documented for each study group |
Data Abstraction
The primary outcome assessed was normalization of either lactulose or glucose breath testing. Additional data abstracted included country of origin, study design, dates of enrollment, types of patients enrolled, antibiotic and dietary restrictions, method for diagnosing SIBO, definition of breath test normalization, antibiotic regimen used, number enrolled in each treatment arm, number with response/cure in each treatment arm, and adverse events. When both intention-to-treat and per-protocol data were reported, we used intention-to-treat data. For trials with more than two treatment arms, each of the treatment arms was considered separately for purposes of pooled data analysis and possible inclusion in meta-analysis. Two authors (JLS, LWD) independently extracted data using a set of inclusion and exclusion criteria and pre-specified definitions. The two authors independently abstracted and entered data into separate spreadsheets. The data were subsequently compared. Disagreement between the two authors was resolved by consensus. If consensus could not be reached, a third party (MS) served as arbiter. No data were found to be missing from any of the included studies.
Outcomes
The primary outcome was normalization of repeat breath testing, confirming eradication of SIBO. This was chosen as the most objective outcome. We also sought to assess clinical response as a secondary outcome. Due to significant heterogeneity in methods for measuring and reporting symptoms pre- and post-treatment, meta-analysis of symptoms was not possible, but we report on clinical response descriptively, based on the methods used to measure clinical response in each included article.
Quality Assessment
We used guidance from the Cochrane Handbook for Systematic Reviews of Interventions(12) to assess quality in the following areas: sequence generation, allocation concealment, blinding (of participants, personnel, and outcome assessment), incomplete outcome data, selective outcome reporting, and other sources of bias. Two authors (JLS, LWD) independently assessed study quality across the above categories. Independently abstracted quality scores were entered by the two authors into separate spreadsheets and then compared. Differences in scoring were resolved via consensus. If consensus could not be reached, a third party (MS) served as arbiter.
Statistical Analysis
The rate of breath test normalization was determined for each study. Because numerous different antibiotic comparisons were studied, we calculated the pooled rate of breath test normalization for different antibiotics. For rifaximin, this was calculated across varying doses: low-dose (600–800 mg per day), medium-dose (1200 mg per day), and high-dose (1600–1650 mg per day). Data from individual studies were pooled and weighted by sample size. The mean rate of breath test normalization was calculated along with the 95% confidence interval (CI) using the confidence interval calculator in Stata.
When feasible, meta-analysis was performed to compare breath test normalization among different treatment regimens. A random-effects model estimated the weighted average of the breath test normalization rate ratio between treatment interventions.(13) Relative risk ratios (RRR) for normalization of breath tests with 95% confidence intervals were calculated for each analysis, and a forest plot was generated to graphically represent the available studies. Due to the small number of studies that were appropriate for meta-analysis, sensitivity analyses were not possible. A statistically significant result was observed with a 95% CI not crossing 1.0 and a P-value <0.05. Heterogeneity was calculated using Mantel-Haenszel χ2 test with a p<0.10 representing significant heterogeneity. Because it was only possible to meta-analyze four relatively small studies, we did not assess for publication bias, because the small sample size made such analysis unreliable. All statistical analyses were calculated using Stata 11.0 (Stata Corp®, College Station, Texas).
Results
Search results
Primary literature search and review of citations from included articles produced 1,356 articles. 1,334 of these were excluded based on review of the title and/or abstract. Twenty-two full articles were reviewed in detail. Ten of these met criteria for inclusion, and 12 were excluded for various reasons (figure 1).
Characteristics of included studies
The ten included studies are summarized in tables 2 and 3.(6,14–21) Seven of the studies were performed in Italy and 3 were performed in the United States. Most studies were open-label, randomized trials. Five studies included adults with symptoms of SIBO, 2 included patients with Crohn’s disease, 1 included patients with formally diagnosed irritable bowel syndrome, 1 included subjects with celiac disease, and 1 included children with chronic abdominal pain. The mean sample size per study was 63 subjects (range 14 to 142), and mean number per treatment arm was 30 (range 7 to 71). Rifaximin was the most commonly studied antibiotic (8 of 10 studies). Only two antibiotics were evaluated in more than one study. Pre-enrollment restrictions varied. Testing for eradication was performed between 3 and 30 days after completing the treatment course.
Table 2.
Characteristics of included studies.
| Study | Country | Study design |
Study dates |
Patient population1 |
Trial agents | Method of SIBO diagnosis |
Test of SIBO eradication |
Days of antibiotic restriction before testing |
Dietary restrictions2 | Other restrictions |
|---|---|---|---|---|---|---|---|---|---|---|
| Collins 2011 | United States | DB, RCT | Not reported | Children with chronic abdominal pain | Rifaximin versus placebo | LBT | LBT normal 14 days after treatment | 60 | Light meal the night before | No probiotics for 60 days |
| Chang 2011 | United States | DB, RCT | 2006–2008 | Celiac patients with abdominal symptoms | Rifaximin versus placebo | LBT | LBT normal 4 days after treatment | 30 | Multiple food exclusions the day before | None |
| Furnari 2010 | Italy | OL, RT | 2007–2010 | Adults with SIBO symptoms | Rifaximin versus Rifaximin plus PHGG | GBT | GBT normal 30 days after treatment | 10 | Boiled rice, meat and water the night before | No probiotics or proton pump inhibitors for 10 days |
| Lauritano 2009 | Italy | OL, RT | 2005–2007 | Adults with SIBO symptoms | Rifaximin versus metronidazole | GBT | GBT normal 30 days after treatment | 90 | Carbohydrate restricted the night before | No laxatives for 30 days |
| Scarpellini 2007 | Italy | OL, RT | 2004–2006 | Adults with SIBO symptoms | Rifaximin (compared multiple doses) | GBT | GBT normal 30 days after treatment | 90 | Carbohydrate restricted the night before | No laxatives for 30 days |
| Lauritano 2005 | Italy | OL, RT | 2003–2004 | Adults with SIBO symptoms | Rifaximin (compared multiple doses) | GBT | GBT normal 30 days after treatment | 30 | Carbohydrate restricted the night before | No laxatives for 30 days |
| Castiglione 2003 | Italy | OL, RT | 2000–2002 | Adults with Crohn’s disease | Metronidazole versus ciprofloxacin | LBT followed by GBT | GBT normal 7 days after treatment | 30 | No starch for 48 hours | None |
| Pimentel 2003 | United States | DB, RCT | Not reported | Adults meeting Rome I criteria for IBS | Neomycin versus placebo | LBT | LBT normal 7 days after treatment | 90 | No legumes or heavy foods the night before | “All use prohibited” |
| Biancone 2000 | Italy | Blinded3, RT | Not reported | Adults with Crohn’s disease | Rifaximin versus placebo | GBT | GBT normal 14 days after treatment | Not reported | No specific restrictions | None |
| DiStefano 2000 | Italy | DB, RT | Not reported | Adults with SIBO symptoms | Rifaximin versus chlortetracycline | GBT | GBT normal 3 days after treatment | 30 | Rice, meat and olive oil the evening before | None |
DB, double-blinded; GBT, glucose breath test; IBS, irritable bowel syndrome; LBT, lactulose breath test; OL, open-label; PHGG, partially hydrolyzed guar gum; RCT, randomized controlled trial; RT, randomized trial; SIBO, small intestinal bacterial overgrowth
These data are meant to be descriptive and do not represent analytical subgroups
Unless otherwise stated, subjects were NPO for 12 hours before testing
Unclear whether single- or double-blinded
Table 3.
Treatment arms and outcomes by study.
| Study | Treatment arm 11 | Subjects in treatment arm 1, No. |
Cures in treatment arm 1, No. (%) |
Treatment arm 21 | Subjects in treatment arm 2, No. |
Cures in treatment arm 2, No. (%) |
Statistical significance |
|---|---|---|---|---|---|---|---|
| Collins 2011 | Rifaximin 1650 mg per day × 10 days | 49 | 9 (18.4) | Placebo three times daily × 10 days | 26 | 3 (11.5) | NS |
| Chang 2011 | Rifaximin 1200 mg per day × 10 days | 11 | 2 (18.2)2 | Placebo three times daily × 10 days | 16 | 3 (18.8)2 | NS |
| Furnari 2010 | Rifaximin 1200 mg per day × 10 days | 37 | 23 (62.2) | Rifaximin 1200 mg per day plus PHGG 5g daily × 10 days | 40 | 34 (85.0) | P<.05 |
| Lauritano 2009 | Rifaximin 1200 mg per day × 10 days | 71 | 45 (63.4) | Metronidazole 250 mg three times daily × 10 days | 71 | 31 (43.7) | P<.05 |
| Scarpellini 2007 | Rifaximin 1600 mg per day × 7 days | 40 | 32 (80.0) | Rifaximin 1200 mg per day × 7 days | 40 | 23 (57.5) | P<.05 |
| Lauritano 20052 | Rifaximin 600 mg per day × 7 days | 30 | 5 (16.7) | Rifaximin 800 mg per day × 7 days | 30 | 8 (26.7) | P<.05 for arm 33 compared with arms 1 and 2 |
| Castiglione 2003 | Metronidazole 250 mg three times daily × 10 days | 15 | 13 (86.7) | Ciprofloxacin 500 mg twice daily × 10 days | 14 | 14 (100.0) | NS |
| Pimentel 2003 | Neomycin 500 mg twice daily × 10 days | 41 | 8 (19.5) | Placebo twice daily × 10 days | 43 | 1 (2.3) | Not reported |
| Biancone 2000 | Rifaximin 1200 mg per day × 7 days | 7 | 7 (100.0) | Placebo three times daily × 7 days | 7 | 2 (28.6) | P<.05 |
| DiStefano 2000 | Rifaximin 1200 mg per day × 7 days | 10 | 7 (70.0) | Chlortetracycline 333 mg three times daily × 7 days | 11 | 3 (27.3) | P<.05 |
NS, not significant; PHGG, partially hydrolysed guar gum
For rifaximin, dose is total daily dose. Unless otherwise stated, these were divided into three times daily dosing.
Number of cures for each treatment arm not extractable from published manuscript; data obtained through communication with study authors.
Study had a third treatment arm, which included 30 subjects treated with Rifaximin 1200mg/day for 7 days. There were 18 cures (60%).
Breath test normalization
The pooled rate of breath test normalization varied widely across different antibiotics and doses (table 4). Rifaximin monotherapy was evaluated in 8 studies with pooled rate of breath test normalization ranging from 21.7% (95% CI 12.1–34.2) at low doses to 46.1% (95% CI 35.4–57.0) at high doses to 60.8% (95% CI 53.2–68.1) at medium doses. For all trials of rifaximin monotherapy combined, the aggregate breath test normalization rate was 49.5% (95% CI 44.0–55.1). Rifaximin combined with partially hydrolyzed guar gum was used in one study with a breath test normalization rate of 85% (95% CI 70.2–94.3). Metronidazole was used in two studies, with a combined breath test normalization rate of 51.2% (95% CI 40.1–62.1). Ciprofloxacin had the highest rate of breath test normalization (100%, 95% CI 76.8–100.0), but this was based on a single study with only 14 subjects in each treatment arm. For all antibiotic regimens combined, breath test normalization occurred in 51.1% (95% CI 46.7–5.5). Conversely, only 9.8% (95% CI 4.6–17.8) of placebo-treated subjects among 4 studies had breath test normalization.
Table 4.
Pooled breath test normalization rates.
| Treatment | Number of studies | Total number of subjects |
Number with breath test normalization |
Percent with breath test normalization |
95% confidence interval1 |
|---|---|---|---|---|---|
| Rifaximin 1600 or 1650 mg per day | 2 | 89 | 41 | 46.1 | 35.4 – 57.0 |
| Rifaximin 1200 mg per day | 6 | 176 | 107 | 60.8 | 53.2 – 68.1 |
| Rifaximin 600 or 800 mg per day | 1 | 60 | 13 | 21.7 | 12.1 – 34.2 |
| Rifaximin monotherapy (all doses combined) | 8 | 325 | 161 | 49.5 | 44.0 – 55.1 |
| Rifaximin plus PHGG | 1 | 40 | 34 | 85.0 | 70.2 – 94.3 |
| Metronidazole | 2 | 86 | 44 | 51.2 | 40.1 – 62.1 |
| Neomycin | 1 | 41 | 8 | 19.5 | 8.8 – 34.9 |
| Ciprofloxacin | 1 | 14 | 14 | 100.0 | 76.8 – 100.0 |
| Chlortetracycline | 1 | 11 | 3 | 27.3 | 6.0 – 61.0 |
| All antibiotics | 10 | 517 | 264 | 51.1 | 46.7 – 55.5 |
| Placebo | 4 | 92 | 9 | 9.8 | 4.6 – 17.8 |
PHGG, partially hydrolyzed guar gum
Calculated using the confidence interval function of Stata.
Clinical response
Two studies objectively documented clinical response depending on whether subjects had breath test normalization. Furnari et al reported “clinical improvement” as a global symptom score reduction of ≥ 50%.(15) For the rifaximin arm, 87% of subjects with breath test normalization achieved clinical improvement versus only 7% with persistently abnormal breath tests. For the rifaximin plus partially hydrolyzed guar gum arm, these proportions were 91% and 17%, respectively. Pimentel et al reported “true clinical response” as a ≥ 50% reduction in overall composite score of irritable bowel syndrome symptoms (including abdominal pain, diarrhea, and constipation).(6) 46% receiving neomycin had a true clinical response versus 15% receiving placebo. Subjects receiving neomycin with normalization of lactose breath testing had significantly greater reduction in their composite symptom score (61.7% reduction) compared with subjects receiving neomycin whose breath tests did not normalize (34.4% reduction) and subjects receiving placebo (4.1% reduction).
Four studies reported on symptomatic response, but did not stratify outcomes by breath test normalization. DiStefano et al reported greater reduction in a cumulative symptom score among subjects treated with rifaximin compared with chlortetracycline (mean score 6.3 pre-treatment to 5.2 post-treatment for rifaximin versus 6.6 to 6.4 for chlortetracycline).(21) Castiglione et al found no differences in bloating, stool quality, or abdominal pain comparing metronidazole to ciprofloxacin (composite score not reported).(19) The Chang and Collins studies reported no differences in symptoms for subjects treated with rifaximin versus placebo, but objective data were not reported in either study.(14,22)
Four of the studies(16–18,20) reported no data regarding symptoms.
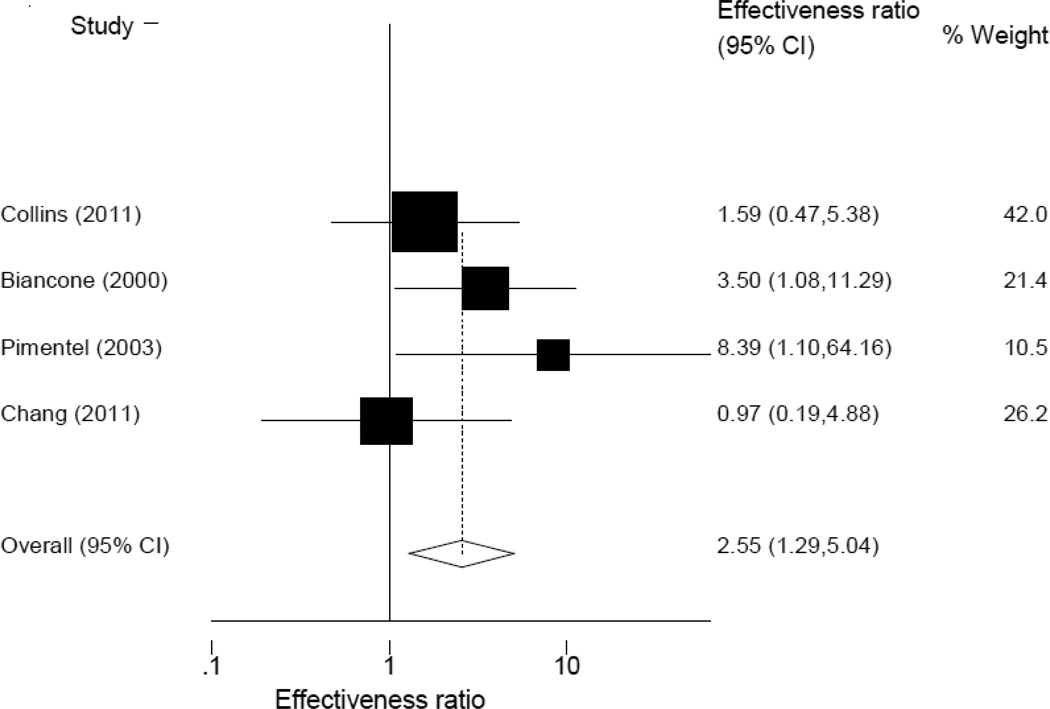
Meta-analysis
Two meta-analyses were possible. The first included four studies(6,14,20,22) comparing any antibiotic therapy to placebo (figure 2). Although these studies included heterogeneous populations, there was no evidence of statistical heterogeneity (P=0.32 for heterogeneity). Treatment of SIBO with any antibiotic was associated with higher rate of breath test normalization compared to placebo (effectiveness ratio 2.55, 95% CI 1.29 – 5.04, P=0.03).
Figure 2.
Meta-analysis of any antibiotic versus placebo.
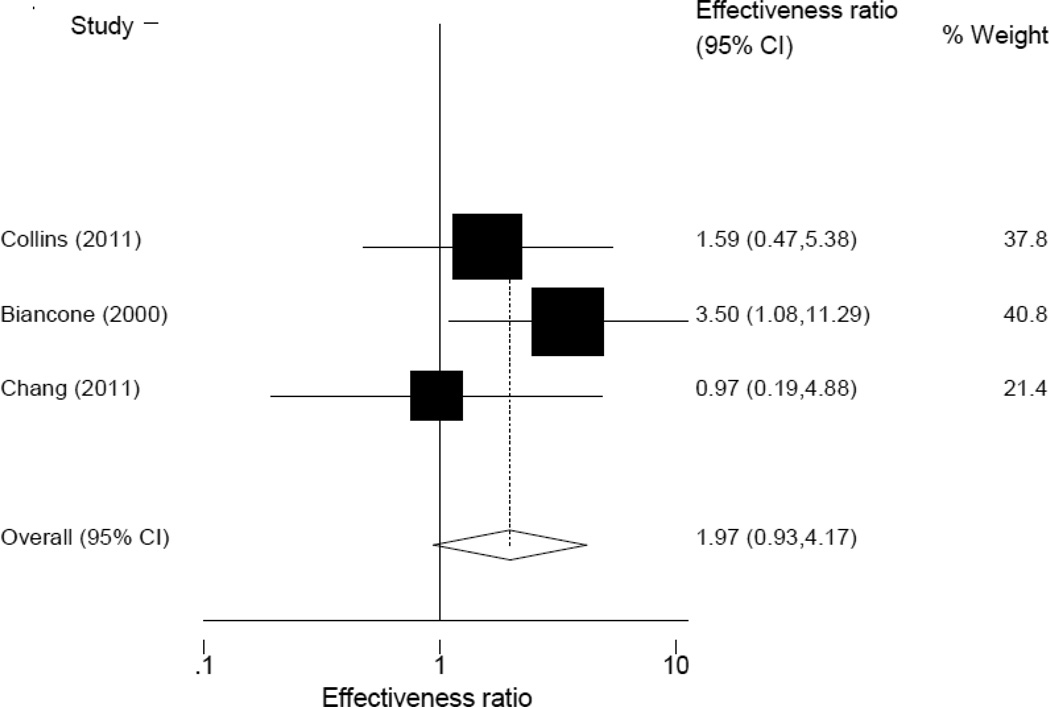
The second meta-analysis included three studies(14,20,22) comparing rifaximin to placebo (figure 3). Although these studies included heterogeneous populations, there was no evidence of statistical heterogeneity (P=0.41 for heterogeneity). Treatment with rifaximin was associated with a higher rate of breath test normalization compared to placebo, though this was not statistically significant (effectiveness ratio 1.97, 95% CI 0.93,4.17, P=0.08).
Figure 3.
Meta-analysis of rifaximin versus placebo.
Quality assessment
Quality of reporting across the studies varied. No studies showed evidence of selective outcome reporting, and two studies had incomplete outcome data. The protocol for sequence generation of antibiotic and/or placebo was high-quality in 6 studies, but reporting was inadequate to characterize sequence generation in the other 4 studies. Seven studies had high-quality allocation concealment, while 3 studies did not provide enough information to classify allocation concealment. Reporting of blinding was adequate in 9 of 10 studies; however, only 4 studies had high-quality blinding of participant, personnel, and outcome. Six studies reported funding that did not indicate any apparent conflict of interest. Two studies did not report a funding source, while two studies reported pharmaceutical company funding. See supplemental table for more details.
Discussion
Given the prevalence of SIBO and its potential for significant consequences when left untreated, we found a surprising lack of depth in the literature describing antibiotic therapy for SIBO. Our extensive literature search produced only ten studies describing antibiotic trials for SIBO meeting inclusion criteria. The majority of studies were of modest size, and most were open-label randomized trials. Only two antibiotics (metronidazole and rifaximin) were evaluated in more than one study. Only four studies compared antibiotics to placebo, and meta-analysis of these studies suggested modest benefit of antibiotic over placebo. Our findings call attention to several important issues and considerations for SIBO therapy and research moving forward.
In the meta-analyses, we were unable to reject the null hypothesis of no statistical heterogeneity, likely due to the small number of studies meta-analyzed. For the ten studies included in our overall review, though, there was evident heterogeneity in study design, including populations studied, pre-study restrictions, treatment regimens used, type and timing of breath testing, and assessment of clinical response (table 2). This limits our ability to draw firm conclusions regarding choice of antibiotics for breath test normalization among patients with SIBO.
Measurement of symptoms pre- and post-treatment was even more heterogeneous. Only two studies(6,15) reported symptom data using objective, composite clinical scores. Unfortunately, the remaining eight studies were much more limited, with four studies reporting on clinical response in a limited fashion,(14,19,21) and the other four reporting no data regarding symptoms and clinical response.(16–18,20) Since SIBO therapy is most frequently driven by a desire to reduce or eliminate bothersome symptoms, this is an important gap in the literature that should be addressed. Specifically, additional large, randomized, double-blind trials assessing both breath test normalization and objectively measured symptomatic response are needed.
Because case series and observational studies carry significant risk of publication bias, we chose a priori to include only clinical trials comparing placebo and/or antibiotics. Given the limited nature of our meta-analysis, we chose to calculate pooled rates of breath test normalization for the various treatment regimens, including varying doses of rifaximin (table 4). The purpose of this analysis was to provide summative data that would be more clinically useful. Rifaximin was the most commonly studied antibiotic, with eight of ten studies evaluating monotherapy at varying doses. The overall breath test normalization rate for rifaximin monotherapy was only 49.5% (95% CI 44.0–55.1), but this ranged widely from 16.7% to 100%. This wide range may be attributable to variability in study populations, dosing strategies, and timing of post-treatment breath testing. In meta-analysis (figure 3), rifaximin had an effectiveness ratio of 1.97 compared with placebo, but this was not statistically significant (95% CI 0.93–4.17, P=0.08). The lack of statistical significance likely relates to relatively small numbers of subjects (67 subjects received rifaximin and 49 received placebo among all three studies combined), and it is possible that a true benefit for rifaximin exists compared with placebo.
Other antibiotics were notably less studied, with metronidazole being most common after rifaximin, and still limited to only two studies. Since rifaximin is costly and may be unavailable to many patients, more thorough investigation of alternate antibiotic choices is warranted, ideally double-blind studies comparing other antibiotics to rifaximin. Such data would be useful not only for primary treatment of SIBO, but also to inform therapeutic choices for patients with recurrent or refractory SIBO, which are not uncommon clinical entities.(10,23)
Numerically, the most effective antibiotic was ciprofloxacin, with a 100% breath test normalization rate, but the single study included only 14 subjects in each arm.(19) Aside from this small trial, the most effective treatment regimen was rifaximin plus partially hydrolyzed guar gum, which was associated with an 85% breath test normalization rate.(15) Partially hydrolyzed guar gum is a prebiotic agent that favors growth of Bifidobacteria and Lactobacillus spp., among others.(24) Treatment with antibiotics alone does not fully address the microbial dysbiosis associated with SIBO, since antibiotics do not restore normal flora.(15) Accordingly, the addition of pre- or probiotics is an attractive option.(25) Probiotics are postulated to enhance gut barrier function, decrease inflammatory response, stabilize gut flora, and potentially modulate visceral hypersensitivity.(26) Their use has been best described among patients with irritable bowel syndrome and Clostridium difficile infection,(27–30) and our understanding of these therapies in SIBO remains limited. Prebiotics, in contrast, alter gut microbiota indirectly by favoring growth of certain bacterial species via provision of metabolites. The therapeutic profile of prebiotics is less well-defined and available data are generally of poor quality.(31) As noted above, the Furnari study(15) was the only study meeting inclusion criteria that included a prebiotic, and none of the studies meeting inclusion criteria included a probiotic arm. In our overall search of the literature, only one other fully reviewed article included a probiotic arm.(32) In this small study (which did not meet inclusion criteria), the administration of oral Lactobacillus spp. did not reduce symptoms or result in breath test normalization among patients with SIBO.(32) The role of microbiome-related therapy for SIBO is intuitive. As techniques to study the human microbiome advance, this will become an increasingly important area for further attention and research.
We chose to assess breath test normalization as our primary outcome of interest due to its ubiquity in SIBO trials and the aforementioned lack of standardization in symptom reporting. Proximal intestinal aspirates were previously accepted as the gold standard for diagnosing SIBO, but methodological considerations (such as obtaining a representative sample, culturing fastidious bacteria, and differentiating culprit strains from contamination or non-pathogenic strains) limits the utility of this test, particularly if repeat testing after treatment is desired.(3) Indirect tests for SIBO, such as breath test analysis, are therefore appealing.(3) The sensitivity and specificity of breath testing varies, but glucose breath testing (sensitivity 63%, specificity 82%, diagnostic accuracy 72%) is thought to be more accurate than lactulose breath testing (sensitivity 52%, specificity 86%, diagnostic accuracy 55%).(2)
The transition from an abnormal breath test to a normal breath test provides biological evidence of a treatment’s effectiveness in eradicating bacteria in the small intestine, which is necessary to “cure” SIBO. The two studies documenting clinical response by breath test normalization(6,15) clearly demonstrate that breath test normalization is highly associated with reduction in symptoms attributable to SIBO. This is further supported by the four studies reporting limited clinical response data. The one study identifying differences in breath test normalization between treatment arms(21) found analogous differences in clinical response, while the three studies without differences in breath test normalization between treatment arms(14,19,22) failed to find differences in clinical response. These data suggest that breath test normalization may correlate with symptomatic response. Repeat breath testing among patients who have been treated for SIBO, yet remain symptomatic may therefore have utility in clinical practice, as it may help clarify whether persistent SIBO is the source of ongoing symptoms, or if other etiologies, such as irritable bowel syndrome, should be considered. There are strong data supporting a robust association between SIBO and irritable bowel syndrome, with two meta-analyses identifying a 3.5- to 9.6-fold increased odds of SIBO in patients with irritable bowel syndrome.(33,34) That rifaximin has been shown to be an effective therapy for irritable bowel syndrome patients without constipation, further supports the role of SIBO in irritable bowel syndrome.(35)
In summary, we identified ten studies comparing antibiotic therapies for SIBO. Antibiotic therapy appears to be superior to placebo for the eradication of SIBO, but the small number of heterogeneously designed studies prevented more detailed meta-analyses of different treatment regimens. Future studies of SIBO should address the shortcomings of these studies. Trials involving larger patient populations, comparing a greater diversity of antibiotics to one another and to placebo, are needed. The use of objective measures of clinical response among patients being treated for SIBO is critical, as is longer-term follow-up assessing durability of response and risk of relapse among patients successfully treated.
Supplementary Material
Acknowledgments
Funding/Support: MS is supported by the NIH K23 CA157929 award. The funder played no role in the design, execution, interpretation, or manuscript preparation.
Footnotes
Author Contributions:
Drs. Sewell, Day and Somsouk had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. All authors approved the final version of the manuscript.
Study concept and design: Sewell, Day, Somsouk
Acquisition of data: Sewell
Analysis and interpretation of data: Sewell, Day, Somsouk, Shah
Drafting of manuscript: Sewell, Shah
Critical revision of manuscript for important intellectual content: Day, Somsouk, Sewell
Statistical analysis: Sewell, Day, Somsouk
Obtained funding: N/A
Administrative, technical, and material support: N/A
Study supervision: Sewell, Day, Somsouk
Financial Disclosures: MS has received research grant support from Salix Pharmaceuticals, Inc.
Additional Contributions: We thank Gloria Won, MLIS, for her assistant with the literature search.
References
- 1.Lappinga PJ, Abraham SC, Murray JA, Vetter EA, Patel R, Wu TT. Small intestinal bacterial overgrowth: histopathologic features and clinical correlates in an underrecognized entity. Arch Pathol Lab Med. 2010 Feb;134(2):264–270. doi: 10.5858/134.2.264. [DOI] [PubMed] [Google Scholar]
- 2.Bures J, Cyrany J, Kohoutova D, Forstl M, Rejchrt S, Kvetina J, et al. Small intestinal bacterial overgrowth syndrome. World J Gastroenterol. 2010 Jun 28;16(24):2978–2990. doi: 10.3748/wjg.v16.i24.2978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dukowicz AC, Lacy BE, Levine GM. Small intestinal bacterial overgrowth: A comprehensive review. Gastroenterol Hepatol. 2007;3(2):112–122. [PMC free article] [PubMed] [Google Scholar]
- 4.Teo M, Chung S, Chitti L, Tran C, Kritas S, Butler R, et al. Small bowel bacterial overgrowth is a common cause of chronic diarrhea. J Gastroenterol Hepatol. 2004;19(8):904–909. doi: 10.1111/j.1440-1746.2004.03376.x. [DOI] [PubMed] [Google Scholar]
- 5.Gasbarrini A, Corazza GR, Gasbarrini G, Montalto M, Di Stefano M, Basilisco G, et al. Methodology and indications of H2-breath testing in gastrointestinal diseases: the Rome Consensus Conference. Aliment Pharmacol Ther. 2009 Mar 30;29(Suppl 1):1–49. doi: 10.1111/j.1365-2036.2009.03951.x. [DOI] [PubMed] [Google Scholar]
- 6.Pimentel M, Chow EJ, Lin HC. Normalization of lactulose breath testing correlates with symptom improvement in irritable bowel syndrome. a double-blind, randomized, placebo-controlled study. Am J Gastroenterol. 2003 Feb;98(2):412–419. doi: 10.1111/j.1572-0241.2003.07234.x. [DOI] [PubMed] [Google Scholar]
- 7.Su J, Smith MB, Rerknimitr R, Morrow D. Small intestine bacterial overgrowth presenting as protein-losing enteropathy. Dig Dis Sci. 1998 Mar;43(3):679–681. doi: 10.1023/a:1018848132369. [DOI] [PubMed] [Google Scholar]
- 8.Kerlin P, Wong L. Breath hydrogen testing in bacterial overgrowth of the small intestine. Gastroenterology. 1988 Oct;95(4):982–988. doi: 10.1016/0016-5085(88)90173-4. [DOI] [PubMed] [Google Scholar]
- 9.Corazza GR, Menozzi MG, Strocchi A, Rasciti L, Vaira D, Lecchini R, et al. The diagnosis of small bowel bacterial overgrowth. Reliability of jejunal culture and inadequacy of breath hydrogen testing. Gastroenterology. 1990 Feb;98(2):302–309. doi: 10.1016/0016-5085(90)90818-l. [DOI] [PubMed] [Google Scholar]
- 10.Singh VV, Toskes PP. Small bowel bacterial overgrowth: Presentation, diagnosis, and treatment. Curr Gastroenterol Rep. 2003;5(5):365–372. doi: 10.1007/s11894-003-0048-0. [DOI] [PubMed] [Google Scholar]
- 11.Van Citters GW, Lin HC. Management of small intestinal bacterial overgrowth. Curr Gastroenterol Rep. 2005 Aug;7(4):317–320. doi: 10.1007/s11894-005-0025-x. [DOI] [PubMed] [Google Scholar]
- 12.Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0. Available online at www.cochrane-handbook.org. [Google Scholar]
- 13.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986 Sep;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 14.Collins BS, Lin HC. Double-blind, placebo-controlled antibiotic treatment study of small intestinal bacterial overgrowth in children with chronic abdominal pain. J Pediatr Gastroenterol Nutr. 2011 Apr;52(4):382–386. doi: 10.1097/MPG.0b013e3181effa3b. [DOI] [PubMed] [Google Scholar]
- 15.Furnari M, Parodi A, Gemignani L, Giannini EG, Marenco S, Savarino E, et al. Clinical trial: The combination of rifaximin with partially hydrolysed guar gum is more effective than rifaximin alone in eradicating small intestinal bacterial overgrowth. Aliment Pharmacol Ther. 2010;32(8):1000–1006. doi: 10.1111/j.1365-2036.2010.04436.x. [DOI] [PubMed] [Google Scholar]
- 16.Lauritano EC, Gabrielli M, Scarpellini E, Ojetti V, Roccarina D, Villita A, et al. Antibiotic therapy in small intestinal bacterial overgrowth: rifaximin versus metronidazole. Eur Rev Med Pharmacol Sci. 2009 Mar-Apr;13(2):111–116. [PubMed] [Google Scholar]
- 17.Lauritano EC, Gabrielli M, Lupascu A, Santoliquido A, Nucera G, Scarpellini E, et al. Rifaximin dose-finding study for the treatment of small intestinal bacterial overgrowth. Aliment Pharmacol Ther. 2005;22(1):31–35. doi: 10.1111/j.1365-2036.2005.02516.x. [DOI] [PubMed] [Google Scholar]
- 18.Scarpellini E, Gabrielli M, Lauritano CE, Lupascu A, Merra G, Cammarota G, et al. High dosage rifaximin for the treatment of small intestinal bacterial overgrowth. Aliment Pharmacol Ther. 2007;25(7):781–786. doi: 10.1111/j.1365-2036.2007.03259.x. [DOI] [PubMed] [Google Scholar]
- 19.Castiglione F, Rispo A, Di Girolamo E, Cozzolino A, Manguso F, Grassia R, et al. Antibiotic treatment of small bowel bacterial overgrowth in patients with Crohn's disease. Aliment Pharmacol Ther. 2003;18(11–12):1107–1112. doi: 10.1046/j.1365-2036.2003.01800.x. [DOI] [PubMed] [Google Scholar]
- 20.Biancone L, Vernia P, Agostini D, Ferrieri A, Pallone F. Effect of rifaximin on intestinal bacterial overgrowth in Crohn's disease as assessed by the H2-glucose breath test. Curr Med Res Opin. 2000;16(1):14–20. doi: 10.1185/0300799009117003. [DOI] [PubMed] [Google Scholar]
- 21.Di Stefano M, Malservisi S, Veneto G, Ferrieri A, Corazza GR. Rifaximin versus chlortetracycline in the short-term treatment of small intestinal bacterial overgrowth. Aliment Pharmacol Ther. 2000;14(5):551–556. doi: 10.1046/j.1365-2036.2000.00751.x. [DOI] [PubMed] [Google Scholar]
- 22.Chang MS, Minaya MT, Cheng J, Connor BA, Lewis SK, Green PH. Double-blind randomized controlled trial of rifaximin for persistent symptoms in patients with celiac disease. Dig Dis Sci. 2011 Oct;56(10):2939–2946. doi: 10.1007/s10620-011-1719-6. [DOI] [PubMed] [Google Scholar]
- 23.Lauritano EC, Gabrielli M, Scarpellini E, Lupascu A, Novi M, Sottili S, et al. Small intestinal bacterial overgrowth recurrence after antibiotic therapy. Am J Gastroenterol. 2008;103(8):2031–2035. doi: 10.1111/j.1572-0241.2008.02030.x. [DOI] [PubMed] [Google Scholar]
- 24.Tuohy KM, Kolida S, Lustenberger AM, Gibson GR. The prebiotic effects of biscuits containing partially hydrolysed guar gum and fructo-oligosaccharides--a human volunteer study. Br J Nutr. 2001 Sep;86(3):341–348. doi: 10.1079/bjn2001394. [DOI] [PubMed] [Google Scholar]
- 25.Quigley EMM, Quera R. Small intestinal bacterial overgrowth: Roles of antibiotics, prebiotics, and probiotics. Gastroenterology. 2006;130(2):S78–S90. doi: 10.1053/j.gastro.2005.11.046. [DOI] [PubMed] [Google Scholar]
- 26.Spiller R. Review article: probiotics and prebiotics in irritable bowel syndrome. Aliment Pharmacol Ther. 2008 Aug 15;28(4):385–396. doi: 10.1111/j.1365-2036.2008.03750.x. [DOI] [PubMed] [Google Scholar]
- 27.Guglielmetti S, Mora D, Gschwender M, Popp K. Randomised clinical trial: Bifidobacterium bifidum MIMBb75 significantly alleviates irritable bowel syndrome and improves quality of life--a double-blind, placebo-controlled study. Aliment Pharmacol Ther. 2011 May;33(10):1123–1132. doi: 10.1111/j.1365-2036.2011.04633.x. [DOI] [PubMed] [Google Scholar]
- 28.Kajander K, Hatakka K, Poussa T, Farkkila M, Korpela R. A probiotic mixture alleviates symptoms in irritable bowel syndrome patients: a controlled 6-month intervention. Aliment Pharmacol Ther. 2005 Sep 1;22(5):387–394. doi: 10.1111/j.1365-2036.2005.02579.x. [DOI] [PubMed] [Google Scholar]
- 29.Kajander K, Myllyluoma E, Rajilic-Stojanovic M, Kyronpalo S, Rasmussen M, Jarvenpaa S, et al. Clinical trial: multispecies probiotic supplementation alleviates the symptoms of irritable bowel syndrome and stabilizes intestinal microbiota. Aliment Pharmacol Ther. 2008 Jan 1;27(1):48–57. doi: 10.1111/j.1365-2036.2007.03542.x. [DOI] [PubMed] [Google Scholar]
- 30.Pillai A, Nelson R. Probiotics for treatment of Clostridium difficile-associated colitis in adults. Cochrane Database Syst Rev. 2008 Jan;23M(1) doi: 10.1002/14651858.CD004611.pub2. CD004611. doi(1):CD004611. [DOI] [PubMed] [Google Scholar]
- 31.Dughera L, Elia C, Navino M, Cisaro F ARMONIA Study Group. Effects of symbiotic preparations on constipated irritable bowel syndrome symptoms. Acta Biomed. 2007 Aug;78(2):111–116. [PubMed] [Google Scholar]
- 32.Stotzer PO, Blomberg L, Conway PL, Henriksson A, Abrahamsson H. Probiotic treatment of small intestinal bacterial overgrowth by Lactobacillus fermentum KLD. Scand J Infect Dis. 1996;28(6):615–619. doi: 10.3109/00365549609037970. [DOI] [PubMed] [Google Scholar]
- 33.Shah ED, Basseri RJ, Chong K, Pimentel M. Abnormal breath testing in IBS: A meta-analysis. Dig Dis Sci. 2010;55(9):2441–2449. doi: 10.1007/s10620-010-1276-4. [DOI] [PubMed] [Google Scholar]
- 34.Ford AC, Spiegel BM, Talley NJ, Moayyedi P. Small intestinal bacterial overgrowth in irritable bowel syndrome: systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2009 Dec;7(12):1279–1286. doi: 10.1016/j.cgh.2009.06.031. [DOI] [PubMed] [Google Scholar]
- 35.Pimentel M, Lembo A, Chey WD, Zakko S, Ringel Y, Yu J, et al. Rifaximin therapy for patients with irritable bowel syndrome without constipation. N Engl J Med. 2011 Jan 6;364(1):22–32. doi: 10.1056/NEJMoa1004409. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.