Abstract
BACKGROUND
Children in Appalachia are experiencing high levels of obesity, in large measure because of inferior diets. This study screened the dietary intake of third-graders residing in three rural Appalachian counties in Ohio and determined whether the Food, Math, and Science Teaching Enhancement Resource Initiative (FoodMASTER) curriculum improved their dietary intake.
METHODS
Dietary intake was measured for 238 third-graders at the beginning of the 2007-2008 school year and for 224 third-graders at the end of that year. The FoodMASTER curriculum was delivered to 204 students (test group). Intake was measured using the Block Food Frequency Questionnaire 2004. The final analysis included 138 students.
RESUTS
The FoodMASTER curriculum did not significantly affect the diets of the students in the test group, as no significant differences in intake of macronutrients, specific nutrients, or food groups were found between the test and control groups. Majorities of students did not meet the Recommended Dietary Allowance or Adequate Intakes for fiber, calcium, iron, vitamin A, and vitamin E. The students as a whole did not meet the MyPyramid recommendations for any food group, and nearly one-fifth of their calories came from sweets. Significant differences in percentages of kilocalories from protein and sweets and in servings of fats, oils, and sweets were seen between groups of higher and lower socioeconomic status.
CONCLUSIONS
Energy-dense foods are replacing healthy foods in the diets of Ohio children living in rural Appalachia. The prevalence of poor dietary intake in Appalachia warrants further nutrition interventions involving programming for nutrition, such as future FoodMASTER curricula.
Keywords: nutrition and diet, children and adolescent health, public health, curriculum
The United States has seen a steady climb in childhood obesity over the past 30 years, with rates now reaching alarming levels.1 In particular, obesity in youth aged 6-11 years has tripled during the last three decades.2, 3 Children living in rural communities, such as rural Appalachia, have a heightened risk for poor health outcomes related to overweight because they are more likely to be of low socioeconomic status (SES) and to have little education, and they have fewer means of obtaining adequate health care.4, 5 In a study conducted in West Virginia in 1998-1999, 46% of upper elementary students from three rural counties were classified as at risk of overweight or actually overweight,6 and, similarly, a study in Athens County, Ohio, found that 46% of children attending a summer campus program were either overweight or at risk of overweight.7 Overweight children, like overweight adults, often display signs of several comorbidities, including type 2 diabetes, formerly considered almost exclusively a disease of adults, and cardiovascular diseases.8
As rates of childhood obesity and type 2 diabetes rise, disorders such as coronary artery disease and coronary heart disease will be found in much earlier stages of life.8 Atherosclerosis is the most important underlying cause of coronary artery disease, and studies have reported the first signs of atherosclerosis as early as age 3 years.9 Progression of atherosclerosis can be identified in early childhood years by identifying fatty streaks on the arterial walls,9-12 but a change in diet can dramatically reverse signs of this disease.13 In the United States, Appalachia has one of the highest rates of mortality from coronary heart disease,14 but screening the diets of Appalachian children could lead to intervention programs aimed at reducing childhood obesity and its related comorbidities.
Displacing the basic food groups with foods high in saturated fat and sugar is a common practice among Appalachian children in Kentucky.15 Correspondingly, previous studies have shown that many children in both Appalachia and the United States as a whole fall short of the Recommended Dietary Allowance (RDA) for many key nutrients, like fiber and calcium.15, 16 Proper dietary practices, such as following the recommendations for food groups set by the USDA (United States Department of Agriculture) MyPyramid and exercising regularly, are ways of slowing the progression of obesity and its related conditions.15 However, barriers such as financial instability and the unavailability of resources have made it increasingly difficult for Appalachian children to manage their weight.17 Thus, introducing interventions that promote healthy food choices to young children in this region would be beneficial.18 Nutritional interventions based at schools are uniquely positioned to target a wide range of children for 180 days each year and to improve dietary behaviors in ways that could reduce childhood obesity.19
Currently, screening children for overweight and its associated health risks is primarily the responsibility of physicians, but in some impoverished areas, such as Appalachia, children rarely receive advice on weight management.20 Guidance is especially needed in these poverty-stricken regions because of the link between low SES and the likelihood of being overweight due to a poor-quality diet.21 Unfortunately, the weight status of children in regions such as Appalachia is often overlooked because of limited access to health care and a lack of awareness among caretakers.22, 23 This reality suggests the need for more emphasis on community- and school-based nutrition interventions for Appalachian communities.20
The purpose of the current study was to examine overall dietary intake in third-grade students in Appalachian Southeast Ohio and to determine whether a school-based intervention program, FoodMASTER (Food, Math, and Science Teaching Enhancement Resource Initiative), improved the dietary intake of these students. In addition, researchers were interested in comparing dietary intakes of male and female students and students from schools with lower and higher SES levels as indicated by participation in the free and reduced-price lunch program of the National School Lunch Program.
METHODS
Program
FoodMASTER is a compilation of projects aimed at using food as a tool to teach mathematics and science. In 2005, a Science Education Partnership Award from the National Center for Research Resources of the National Institutes of Health funded a 3-year project aimed at creating and assessing a third-grade FoodMASTER curriculum for rural Appalachian Ohio students. The 45-lesson hands-on curriculum was developed by a team of experts, including teachers and dietitians, and was implemented in classrooms in Athens, Meigs, and Washington counties during the 2007-2008 school year. One of the goals was to assess the nutrient intake of the participating third-graders as a means of directing future educational interventions aimed at improving dietary intake.
Subjects
A letter was sent to all third-grade teachers in the three counties, inviting their participation in the FoodMASTER project. The project investigators conducted site visits with each interested teacher to explain the details of participation. Teachers interested in participating signed an agreement to express their commitment to the project. The classrooms of the first 10 teachers to return the agreement were assigned to the intervention group, i.e., the group that received the 45-lesson curriculum (FoodMASTER).
Teachers implementing the FoodMASTER curriculum in their classrooms (N = 10) participated in a four-day training workshop at Ohio University in July 2007 to prepare for implementation during the academic year. The teachers were given educational materials for their students, were introduced to the content, and spent time working through the lesson in the university test kitchens. In addition, they were instructed on the project’s protocol for academic year 2007, were provided assessment tools, and were formatively evaluated on the materials presented to them.
In the beginning of academic year 2007, one teacher from Athens County and one from Meigs County, who were not participating in the project, volunteered their classrooms as control classrooms (N = 2). Students and parents in all 12 classrooms (10 participating, two controls) received explanatory materials and signed a consent form. All third-grade students with a signed consent form were entered into the study.
Instrument and Procedure
The Block Kids Food Frequency Questionnaire 2004 (BKFFQ) was selected to measure the dietary intake of third-graders because of its suggested age range of 8 to 17 years and the fact that it could be administered in about 25 minutes. The BKFFQ, which was designed by NutritionQuest (Berkeley, Calif), has been used in previous studies and has been validated for specific nutrients.24-26 The BKFFQ includes 77 food items and requires students to report the number of days in the past week each item was consumed and the average portion size consumed on those days. Pictures were provided by NutritionQuest to enhance the accuracy of reporting on portion sizes. The BKFFQ food lists were developed using the USDA Nutrient Database for Dietary Studies, Version 1.0. The completed BKFFQs were sent to NutritionQuest for analysis of nutrients and food group servings. Demographic information was self-reported on the BKFFQ. Schools in which 60% or more of students received free or reduced-price lunches were categorized as lower SES; those with a lower percentage were categorized as higher SES (this decision was based on the cutoff point of 60% for additional federal funding for the National School Lunch Program and on previous research).6,27
Project investigators made an appointment with each teacher at the beginning of the academic year to make a site visit to the classrooms and do a pretest on intake. Teachers in the test group taught all 45 FoodMASTER lessons during the year. At the end of the academic year, investigators returned to the classrooms to collect a set of repeated measures of nutrient intake using the BKFFQ (posttest). Each student was assigned a subject number, which was used to match pretests and posttests. Only subjects with complete and correct BKFFQ pretest and posttest data were entered into the sample.
Data Analysis
The independent t test was used to establish that there were no significant differences (p<.05) between the intervention group and the control group in intake of nutrients at pretest. Paired-samples t tests were used to test significant differences (p<.05) between the pretest and posttest in both the intervention (test) group and the control group in terms of nutrient intake. The independent t test was used to detect differences between the control group and intervention group at posttest. Because for both groups the pretest and posttest data were found to be homogeneous and posttests for the control and intervention groups were homogeneous, researchers used the posttest information, mean score, and frequency statistics to describe the intake of nutrients.
Means and standard deviations for intake were compared with Dietary Reference Intake (DRI) tables using RDAs, Adequate Intakes (AI), and Acceptable Macronutrient Distribution Ranges (AMDR), as appropriate, to determine the frequency of students who fell below these recommendations. Values from the most recent DRI table of the National Academy of Sciences for boys and girls aged 4–8 years were used as a reference for comparison (Dietary Reference Intakes, 2006).28 The seven nutrients selected for this study (calcium, iron, zinc, vitamin A, vitamin C, vitamin E, and fiber) were chosen based on previous research suggesting a low intake in this age group.1, 15, 16, 29, 30
In addition to data on the intake of nutrients, the BKFFQ generates data on the daily number of servings for vegetables; fruits; grains; meats and beans; milk; and fats, oils, and sweets. Information on the daily number of servings was recoded into cups or ounces for consistency with recommendations for food groups set forth in MyPyramid for Kids (6-11 years).31
To examine the data further, tests were performed to detect whether there were differences between socioeconomic groups and genders for the variables of interest. Independent t tests were performed to compare such differences in the mean scores for RDAs, AIs, and AMDRs. Normality of the continuous variables was examined using the Kolmogorov-Smirnov single-sample goodness-of-fit test. While most measures differed significantly from normal, the assumption of normality is not required for the t test when the sample is sufficiently large, even when it has fewer than 100 students.32 Statistical analyses were performed using Statistical Packages for the Social Sciences 16.0 (SPSS).
RESULTS
The BKFFQ was handed out at the beginning of academic year 2007 to 238 students, 204 in the test group classrooms (N = 10) and 34 in the control group classrooms (N = 2). Usable BKFFQs totaled 156 in the test classrooms and 22 in the control classrooms, for inclusion rates of 76% and 65%, respectively, for the pretest. At the end of the academic year the BKFFQ was issued to 224 students, 193 in the test group classrooms (N = 10) and 31 in the control group classrooms (N = 2). Usable BKFFQs for the posttest numbered 161 in the test classrooms and 27 in the control classrooms, for inclusion rates of 83% and 87%, respectively. There were 122 students in the test group classrooms and 16 in the control group classrooms whose questionnaires were used in the final analysis, for inclusion rates of 60% and 47%, respectively. These were the only students with complete and correct BKFFQ data on both the pretest and posttest. In all, 58% of the original sample remained. Demographic characteristics of the participants are presented in Table 1.
Table 1.
Demographic Characteristics of Participants by Gender
| Total Sample |
Male | Female | |
|---|---|---|---|
|
| |||
| Item | N/n (%) | n (%) | n (%) |
| Total participants | 138 | 62 (45) | 76 (55) |
| Race or ethnicity | |||
| African American | 1 (0.7) | 0 | 1 (13) |
| White | 111 (80.4) | 54 (87.1) | 57 (75.0) |
| Hispanic | 1 (0.7) | 0 | 1 (13) |
| Asian | 1 (0.7) | 1(16) | 0 |
| American Indian/Alaska Native | 1 (0.7) | 0 | 1 (13) |
| Other/multiethnic | 23 (16.7) | 7 (11.3) | 16 (21.1) |
| Group | |||
| Test (intervention) | 122 (88) | 57 (92) | 65 (86) |
| Control | 16 (12) | 5 (8) | 11 (14) |
| Socioeconomic status* | |||
| Higher | 101 (73) | 46 (74) | 55 (72) |
| Lower | 37 (27) | 16 (26) | 21 (28) |
| Age in years | 8.5±0.6┼ | 8.7±0.6 ┼ | 8.32±0.6┼ |
Socioeconomic status determined by the school-level proportion of students receiving free or reduced-price lunch. Higher: <60% of students. Lower: ≥60% of students.
Mean +/− standard deviation.
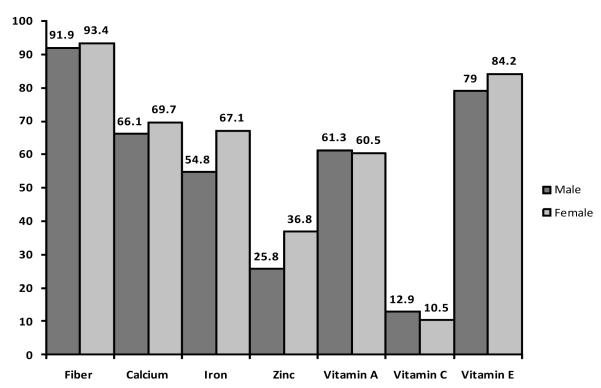
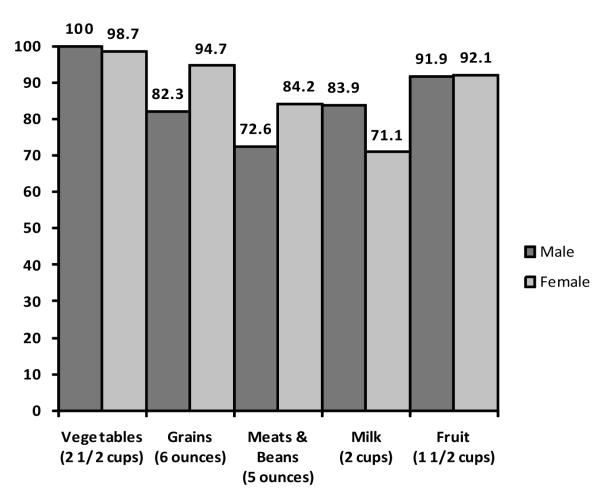
The intake of macronutrients, specific nutrients, and food groups was examined to determine whether FoodMASTER had an impact on the third-graders’ diets. No significant differences in intake of macronutrients, specific nutrients, or food groups were found between the pretest and posttest for either the test group or the control group or in the posttest between the test and control group. Thus, researchers aggregated the posttest data for test and control groups to describe the dietary intake of the population. Overall, the majority of students (data not shown) fell within the AMDRs for carbohydrates (81%), proteins (83%), and fats (61%). However, 32% exceeded the AMDR for fat, and 17% fell below the AMDR for protein. Many students, both male and female, did not meet the RDAs/AIs for key nutrients, especially fiber and vitamin E (Figure 1). Figure 2 shows the percentages of male and female students not meeting the recommendations for food groups set forth in MyPyramid for Kids (6-11 years); in the case of vegetables, 100% of boys and 98.7% of girls did not meet the recommendation.
Figure 1.
Percentage (%) of Male and Female Third-Grade Students in Appalachian Ohio Not Meeting the RDA/AIs for Specified Nutrients
Figure 2.
Percentage (%) of Male and Female Third-Grade Students in Appalachian Ohio Not Meeting the MyPyramid for Kids (6-11 years) Recommendations for Food Groups
No significant differences in the intake of macronutrients were found between boys and girls, but there were significant differences in the intake of micronutrients and food groups by gender. For example, boys consumed significantly more iron (p = 0.01), sodium (p = 0.02), and zinc (p = 0.03) than girls (Table 2). Boys also consumed more ounces of meat and beans (p = 0.03); girls, on the other hand, consumed a higher percentage of saturated fat (p = 0.02) than boys. When the sample was split into higher- and lower-SES groups, the gender differences for iron, sodium, zinc, and ounces of meat and beans remained significant only for children in the higher-SES group (data not shown).
Table 2.
Micronutrient Intake of Male and Female Third-Grade Students
| Parameter (M±SD) | Total Sample | Male | Female | P Value for Difference |
|---|---|---|---|---|
| Energy (kcals) | 1437.78±774.75 | 1617.75±876.49 | 1290.96±650.38 | 0.02* |
| % kcals from carbohydrate |
56.13±7.99 | 56.80±8.69 | 55.57±7.37 | 0.37 |
| % kcals from protein | 13.09±3.02 | 12.82±3.23 | 13.30±2.83 | 0.36 |
| % kcals from fat | 32.63±5.71 | 32.27±6.30 | 32.93±5.19 | 0.50 |
| % kcals from saturated fat |
11.32±0.02 | 10.77±0.02 | 11.77±0.03 | 0.02* |
| % kcals from sweets | 18.18±10.30 | 17.99±11.10 | 18.34±9.67 | 0.84 |
| Fiber (g) | 11.23±7.48 | 12.43±8.77 | 10.25±6.11 | 0.09 |
| Calcium (mg) | 646.70±342.70 | 651.90±329.52 | 642.45±355.20 | 0.87 |
| Iron (mg) | 10.05±5.70 | 11.44±6.63 | 8.93±4.54 | 0.01* |
| Sodium (mg) | 2006.31±1117.65 | 2261.21±1322.86 | 1798.38±872.32 | 0.02* |
| Zinc (mg) | 7.65±4.42 | 8.59±5.06 | 6.89±3.68 | 0.03* |
| Vitamin A, RAE (mcg) | 400.06±246.31 | 406.50±323.41 | 394.81±258.50 | 0.78 |
| Vitamin C (mg) | 88.13±79.33 | 86.68±70.43 | 89.31±86.37 | 0.85 |
| Vitamin E (mg) | 5.26±5.35 | 5.94±6.12 | 4.72±4.60 | 0.18 |
| Cups of vegetables | 0.44±0.51 | 0.43±0.52 | 0.45±0.51 | 0.85 |
| Ounces of grains | 3.52±2.10 | 3.87±2.51 | 3.23±1.67 | 0.09 |
| Ounces of meats & beans |
3.51±2.69 | 4.04±3.04 | 3.07±2.29 | 0.03* |
| Cups of milk | 1.20±0.89 | 1.11±0.83 | 1.28±0.93 | 0.26 |
| Cups of fruit | 0.71±0.54 | 0.73±0.54 | 0.68±0.54 | 0.58 |
| Servings of fats, oils, sweets |
2.92±0.54 | 3.17±2.73 | 1.87±1.25 | 0.12 |
Significant at p < 0.05. M: mean; SD: standard deviation; RAE: retinol activity equivalents.
In the overall analysis comparing higher- and lower-SES groups, significant differences were found for intake of one macronutrient, percentage of kilocalories from sweets, and for servings of fats, oils, and sweets, but no significant differences were found for specified micronutrients. Children from the higher-SES group had a greater percentage of their kilocalories coming from protein (p = 0.04), and children in the lower-SES group had a higher percentage of kilocalories coming from sweets (p = 0.03) and a higher number of servings of fats, oils and sweets (p = 0.03) (Table 3). Overall, children in the study derived about one-fifth of their kilocalories from sweets.
Table 3.
Dietary Intake of Students from Schools with Lower and Higher Socioeconomic Status (SES)
| Parameter (M±SD) | Higher SES | Lower SES | P Value for Difference |
|---|---|---|---|
| Energy (kcals) | 1413.31±785.67 | 1504.57±750.55 | 0.54 |
| % kcals from carbohydrate |
56.07±7.76 | 56.29±8.69 | 0.88 |
| % kcals from protein | 13.40±2.97 | 12.24±3.00 | 0.04* |
| % kcals from fat | 32.36±5.54 | 33.38±6.15 | 0.35 |
| % kcals from saturated fat |
11.33±0.03 | 11.29±0.02 | 0.92 |
| % kcals from sweets | 17.04±9.97 | 21.30±10.68 | 0.03* |
| Fiber (g) | 11.32±7.93 | 10.96±6.13 | 0.80 |
| Calcium (mg) | 663.40±358.67 | 603.83±294.95 | 0.38 |
| Iron (mg) | 10.18±5.84 | 9.70±5.34 | 0.67 |
| Sodium (mg) | 2013.02±1183.78 | 1988.03±927.70 | 0.91 |
| Zinc (mg) | 7.75±4.64 | 7.39±3.84 | 0.68 |
| Vitamin A, RAE (mcg) | 418.35±256.26 | 359.13±212.03 | 0.15 |
| Vitamin C (mg) | 90.94±86.09 | 80.45±57.26 | 0.49 |
| Vitamin E (mg) | 5.17±5.26 | 5.55±5.67 | |
| Cups of vegetables | 0.48±0.56 | 0.34±0.34 | 0.18 |
| Ounces of grains | 3.65±2.23 | 3.16±1.71 | 0.23 |
| Ounces of meats & beans |
3.48±2.73 | 3.56±2.59 | 0.88 |
| Cups of milk | 1.22±0.93 | 1.16±0.78 | 0.73 |
| Cups of fruit | 0.72±0.57 | 0.67±0.47 | 0.66 |
| Servings of fats, oils, sweets |
2.75±1.47 | 3.41±1.73 | 0.03* |
Significant at p < 0.05. M: mean; SD: standard deviation; RAE: retinol activity equivalents.
Socioeconomic status determined by the school-level proportion of students receiving free or reduced-price lunches: Higher: <60% of students. Lower: ≥60% of students.
DISCUSSION
From this study we can conclude that the diets of third-graders in Appalachian Southeast Ohio are rather poor, as few students met RDA or AI values for fiber, calcium, iron, vitamin A, and vitamin E. On the other hand, more than two-thirds of students met the recommendation for zinc, and the great majority met the recommendation for vitamin C. Previous research using a sample of children aged 7-10 years produced similar findings for calcium, vitamin A, and vitamin E but found that the children were meeting the RDA for iron but not for zinc.29 The findings for low fiber, calcium, iron, and vitamin A are consistent with a smaller study of third-to fifth-graders in Massachusetts.1 Intake of iron along with the other nutrients where intake was poor in the present study could be improved by encouraging consumption of lean meats, green leafy vegetables, and whole grains.
The failure to find significant differences between the test and control groups for intake of specific nutrients or of food groups was somewhat surprising but might have several explanations. One possibility is that overall dietary intake as assessed by the BKFFQ did not target all of the specific dietary changes emphasized by FoodMASTER. For example, one FoodMASTER lesson focused on eating whole-grain pastas, but the BKFFQ does not distinguish between whole-grain and refined pastas. Using a tool that looked more specifically at behavioral objectives related to the FoodMASTER intervention may have made a difference in the results. Other possible explanations for the lack of observed differences between the test and control groups are that the teachers may have stressed the mathematics and science objectives of FoodMASTER over the nutrition content or that students learned facts about nutrition but did not use their newly acquired knowledge to make dietary changes.
The third-graders in our study fell short of meeting the MyPyramid for Kids recommendations for all the basic food groups, and past studies, such as a national inquiry conducted by Kennedy and Goldberg, had comparable results.16 A failure to consume the recommended amounts of the five food groups is consistent with the low intakes of the nutrients identified above. In the present study, the food groups tended to be replaced with fat, oils, and sweets; indeed, nearly one-fifth of the kilocalories consumed by the third-graders were from sweets. This high intake of sweets was even more pronounced among students from the lower-SES schools, with 21.3% of their total kilocalories coming from sweets.
We found that girls had a greater intake (by percentage of kilocalories) of saturated fat than did boys; a similar study analyzing intake of saturated fat among rural West Virginia children did not show significant differences between boys and girls,6 but the author did find a noteworthy difference between boys and girls for total intake of fat, but with the boys, not girls, consuming more. Replacing servings of fat, oils, and sweets with whole foods such as fruits, vegetables, and whole grains would improve the diet quality of many Appalachian populations regardless of gender or SES. Our finding that boys consumed significantly more sodium, iron, and zinc than girls is partially consistent with the earlier study on children aged 7-10, in which white boys consumed significantly more vitamin A, iron, and zinc than white girls29 (in our study most participants were white).
Overall, more than 80% of students had intakes of carbohydrate and of protein that were within the AMDR, which is encouraging. Our findings of connections between higher SES and getting a higher proportion of kilocalories from protein and between lower SES and a higher proportion of kilocalories from sweets were both not surprising, as associations between SES and quality of diet are widely known. Moreover, our findings of higher intakes of sweets and more servings of fats, oils, and sweets among low-SES populations are consistent with other similar studies conducted in the Appalachian region.6, 16 The low cost of energy-dense foods may help explain the higher consumption of these foods among students with a low SES.
Limitations
This study had several possible limitations. First, accurately measuring dietary intake, especially in third-grade students, is a complex and rather challenging undertaking. Third-graders may have difficulty recalling the foods they have eaten, and in the present study the BKFFQ of numerous students could not be used because of inaccuracy in reporting. Second, assigning SES using school-level participation rates in the program for free and reduced-price lunches, while a method used by previous researchers, is no more than a rough estimate of SES for the particular students involved.6 Third, the study did not measure the students’ knowledge of nutrition. Conceivably, the students’ knowledge levels here may have improved during the course of this study even though their food intake did not change significantly, but the study was not equipped to make such a finding.
Conclusion
In conclusion, it appears that third-grade students living in Appalachian Southeast Ohio are not meeting the recommended levels for specific nutrients or the recommendations for food groups set forth in MyPyramid for Kids. Energy-dense foods consisting of sugar and fat are replacing healthy foods from the main food groups in the diets of these children. Additional interventions are indicated to improve the dietary intake of this population. Increased efforts to reduce the intake of sugar and fat among children in Southeast Ohio, especially children from lower-SES schools, are warranted. Findings from this study underscore the importance of programs that focus on changing individual and family dietary behaviors. Future FoodMASTER programs should include a stronger family component and focus more specifically on behavioral changes to limit the intake of sugar and fat while increasing intake of recommended food groups. To achieve long-term effects on children’s food choices, nutrition education programs focusing on dietary behaviors, such as the FoodMASTER programs envisioned for the future, should be mainstays in the classroom over multiple grade levels.
IMPLICATIONS FOR SCHOOLS
Improving dietary quality could reduce the incidence of obesity and its co-morbidities in communities within Appalachia, and school-based initiatives in health promotion in this region should be aimed at increasing intake of fruits, vegetables, whole grains, milk, and lean meat and beans. Specific nutrients such as fiber, calcium, iron, vitamin A, and vitamin E should be targeted as well. Some differences in dietary intake between boys and girls indicate a potential need to create or present gender-specific messages on nutrition. For examples, girls may need more encouragement to consume meats and beans, because in our study we found that they consumed a smaller amount of these foods than did boys, and they also consumed less iron and zinc, both of which are found in lean meats and dried beans. Future research is indicated to explore the potential causes of dietary differences between boys and girls.
Finally, teachers, school nurses, administrators, and health care professionals need to work together to research the dietary habits of students and seek ways to improve them. Future research could include studying the effects of the FoodMASTER curriculum on school-age children’s knowledge and testing the effects of adding a stronger family component to this curriculum.
Acknowledgments
Human Subjects Approval Statement: This study was approved by the Ohio University Institutional Review Board (IRB).
Contributor Information
Jana A. Hovland, (hovland@marshall.edu), Department of Dietetics, Marshall University, One John Marshall Drive, Huntington, WV 25755.
Sara M. McLeod, (smm0602@ecu.edu), Department of Nutrition& Dietetics, East Carolina University, 4130 Bostic Dr. Apt. 303, Greenville, NC 27834.
Melani W. Duffrin, (duffrinm@ecu.edu), Department of Nutrition & Dietetics, East Carolina University, 272 Rivers Building, Greenville, NC 27858.
George Johanson, (johanson@ohio.edu), Department of Educational Research and Evaluation, Ohio University, McCracken Hall 314 A, Athens, OH 45701.
Darlene E. Berryman, (berrymad@ohio.edu), Department of Food and Nutrition, Ohio University, W357 Grover Center, Athens, OH 45701.
REFERENCES
- 1.Vadiveloo M, Zhu L, Quatromoni PA. Diet and physical activity patterns of school aged children. J Am Diet Assoc. 2009;109:145–151. doi: 10.1016/j.jada.2008.10.012. [DOI] [PubMed] [Google Scholar]
- 2.Institute of Medicine, Committee on Progress in Preventing Childhood Obesity . Progress in Preventing Childhood Obesity: How Do We Measure Up? National Academies Press; Washington, DC: 2006. [Google Scholar]
- 3.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. J Am Diet Assoc. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 4.Duncan GJ, Brooks-Gunn J, Klebanov PK. Economic deprivation and early childhood development. Child Dev. 1994;65:296–318. [PubMed] [Google Scholar]
- 5.Galloway T. Gender differences in growth and nutrition in a sample of rural Ontario school children. Am J Hum Biol. 2007;19:774–788. doi: 10.1002/ajhb.20637. [DOI] [PubMed] [Google Scholar]
- 6.Gonzales EN, Marshall JA, Heimendinger J, Crane LA, Neal WA. Home and eating environments are associated with saturated fat intake in children in rural West Virginia. J Am Diet Assoc. 2002;102:657–663. doi: 10.1016/s0002-8223(02)90151-3. [DOI] [PubMed] [Google Scholar]
- 7.Tulkki LA, Berryman DE, Rana S, Denham S, Holben DH, Nisbett N. Elevated body image dissatisfaction relates to body size of Appalachian children. Top Clin Nutr. 2006;12:101–107. [Google Scholar]
- 8.Daniels SR, Arnett DK, Eckel RH, et al. Overweight in children and adolescents: pathophysiology, consequences, prevention, and treatment. Circulation. 2005;111:1999–2012. doi: 10.1161/01.CIR.0000161369.71722.10. [DOI] [PubMed] [Google Scholar]
- 9.Holman RI, McGill HC, Strong JP, Geer JC. The natural history of atherosclerosis: the early aortic lesions as seen in the middle of the 20th century. Am J Pathol. 1958;34:209–345. [PMC free article] [PubMed] [Google Scholar]
- 10.Donker GA, Goff DC, Jr, Ragan JD, Jr, Killinger RP, Harrist RB, Labarthe DR. Factors associated with serum cholesterol level in cholesterol screening in a pediatric practice. Cholesterol screening in a pediatric practice. Ann Epidemiol. 1993;3:49–56. doi: 10.1016/1047-2797(93)90009-s. [DOI] [PubMed] [Google Scholar]
- 11.Berenson GS, Srinivasan SR, Bao W, Newman WP, 3rd, Tracy RE, Wattigney WA. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The Bogalusa Heart Study. N Engl Med. 1998;338:1650–1656. doi: 10.1056/NEJM199806043382302. [DOI] [PubMed] [Google Scholar]
- 12.Aggoun Y. Obesity, metabolic syndrome, and cardiovascular disease. Pediatr Res. 2007;61:653–659. doi: 10.1203/pdr.0b013e31805d8a8c. [DOI] [PubMed] [Google Scholar]
- 13.American Heart Association [Accessed January 29, 2009];Cholesterol and atherosclerosis in children. Available at: http://www.americanheart.org/presenter.jhtml?identifier=4499.
- 14.Cooper R, Cutler J, Desvigne-Nickens P, et al. Trends and disparities in coronary heart disease, stroke and other cardiovascular diseases in the United States: findings of the National Conference on Cardiovascular Disease Prevention. Circulation. 2000;102:3137–3147. doi: 10.1161/01.cir.102.25.3137. [DOI] [PubMed] [Google Scholar]
- 15.Crooks DL. Food consumption, activity, and overweight among elementary school children in an Appalachian Kentucky community. Am J Phys Anthropol. 2000;112:159–170. doi: 10.1002/(SICI)1096-8644(2000)112:2<159::AID-AJPA3>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 16.Kennedy E, Goldberg J. What are American children eating? Implications for public policy. Nutr Rev. 1995;53:111–126. doi: 10.1111/j.1753-4887.1995.tb01534.x. [DOI] [PubMed] [Google Scholar]
- 17.Crooks DL. Child growth and nutritional status in a high-poverty community in eastern Kentucky. Am J Phys Anthropol. 1999;109:129–142. doi: 10.1002/(SICI)1096-8644(199905)109:1<129::AID-AJPA10>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 18.Hopper CA, Munoz KD, Gruber MB, Nguyen KP. The effects of a family fitness program on the physical activity and nutrition behaviors of third-grade children. Res Q Exerc Sport. 2005;76:130–139. doi: 10.1080/02701367.2005.10599275. [DOI] [PubMed] [Google Scholar]
- 19.Muth ND, Chatterjee A, Williams D, Cross A, Flower K. Making an IMPACT: effect of a school-based pilot intervention. N C Med J. 2008;69:432–440. [PubMed] [Google Scholar]
- 20.Demerath E, Muratova V, Spangler E, Li J, Minor VE, Neal WA. School-based obesity screening in rural Appalachia. Prev Med. 2003;37:553–560. doi: 10.1016/j.ypmed.2003.09.013. [DOI] [PubMed] [Google Scholar]
- 21.Crooks DL. American children at risk: poverty and its consequences for children’s health, growth, and school achievement. Am J Phys Anthropol. 1995;38:57–86. [Google Scholar]
- 22.Galuska DA, Will JC, Serdula MK, Ford SE. Are health care professionals advising obese patients to lose weight? JAMA. 1999;282:1576–1578. doi: 10.1001/jama.282.16.1576. [DOI] [PubMed] [Google Scholar]
- 23.Halpern-Felsher BL, Ozer EM, Millstein SG, et al. Preventive services in a health maintenance organization: how well do pediatricians screen and educate adolescent patients? Arch Pediatr Adolesc Med. 2000;154:173–179. doi: 10.1001/archpedi.154.2.173. [DOI] [PubMed] [Google Scholar]
- 24.Kruzich LA, Marquis GS, Carriquiry AL, Wilson CM, Stephensen CB. US youths in the early stages of HIV disease have low intakes of some micronutrients important for optimal immune function. J Am Diet Assoc. 2004;104:1095–1101. doi: 10.1016/j.jada.2004.04.021. [DOI] [PubMed] [Google Scholar]
- 25.Marshall TA, Eichenberger-Gilmore JM, Broffitt B, Stumbo PJ, Levy SM. Relative validity of the Iowa Fluoride Study targeted nutrient semi-quantitative questionnaire and the Block Kids’ Food Questionnaire for estimating beverage, calcium, and vitamin D intakes by children. J Am Diet Assoc. 2008;108:465–472. doi: 10.1016/j.jada.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 26.Cullen KW, Watson K, Zakeri I. Relative reliability and validity of the Block Kids Questionnaire among youth aged 10 to 17 years. J Am Diet Assoc. 2008;108:862–866. doi: 10.1016/j.jada.2008.02.015. [DOI] [PubMed] [Google Scholar]
- 27.United States Department of Agriculture [Accessed September 20, 2007];Food and Nutrition Service National School Lunch, Special Milk, and School Breakfast Programs, national average payments/maximum reimbursement rates. Available at: http://www.fns.usda.gov/cnd/Governance/notices/naps/NAPs07-08.pdf.
- 28.Food and Nutrition Board, Institute of Medicine . Dietary Reference Intakes: The Essential Guide to Nutrient Requirements. The National Academies Press; 2006. [Google Scholar]
- 29.Ganji V, Hampi JS, Betts NM. Race-, gender- and age-specific differences in dietary micronutrient intakes of US children. Int J Food Sci Nutr. 2003;54:485–490. doi: 10.1080/09637480310001622341. [DOI] [PubMed] [Google Scholar]
- 30.Kelley C, Krummel D, Gonzales EN, Neal WA, Fitch CW. Dietary intake of children at high risk for cardiovascular disease. J Am Diet Assoc. 2004;104:222–225. doi: 10.1016/j.jada.2003.11.014. [DOI] [PubMed] [Google Scholar]
- 31.United States Department of Agriculture, Food and Nutrition Service [Accessed January 29, 2009];MyPyramid for kids. 2005 Available at: http://www.mypyramid.gov/kids/
- 32.Lumley T, Diehr P, Emerson S, Chen L. The importance of the normality assumption in large public health data sets. Annu Rev Public Health. 2002;23:151–169. doi: 10.1146/annurev.publhealth.23.100901.140546. [DOI] [PubMed] [Google Scholar]