Wild waterfowl form the main reservoir of influenza A viruses, from which transmission occurs directly or indirectly to various secondary hosts, including humans 1. Direct avian-to-human transmission has been observed for viruses of subtypes A/H5N1, A/H7N2, A/H7N3, A/H7N7, A/H9N2, and A/H10N7 upon human exposure to poultry 2-7 but a lack of sustained human-to-human transmission has prevented these viruses to cause new pandemics. Recently, avian A/H7N9 viruses were transmitted to humans, causing severe respiratory disease and deaths in China 8. Since transmission via respiratory droplets and aerosols (hereafter referred as “airborne” transmission) is the main route for efficient transmission between humans, it is important to gain insight on airborne transmission of the A/H7N9 virus. Here we show that, although A/Anhui/1/2013 A/H7N9 virus harbours determinants associated with human adaptation and transmissibility between mammals, its airborne transmissibility in ferrets was limited, intermediate between that of typical human and avian influenza viruses. Multiple A/H7N9 virus genetic variants were transmitted. Upon ferret passage, variants with higher avian receptor binding, higher pH of fusion, and lower thermostability were selected, potentially resulting in reduced transmissibility. This A/H7N9 virus outbreak highlights the need for increased understanding of determinants of efficient airborne transmission of avian influenza viruses between mammals.
At the end of March 2013, the World Health Organization was notified by the Chinese authorities of three human cases of infection with a novel avian-origin influenza A/H7N9 virus 9. All three cases developed bilateral pneumonia with progression to acute respiratory distress syndrome and death 10,11. As of July 2013, 133 A/H7N9 laboratory-confirmed cases have been reported in ten different provinces of China, including 43 deaths 8. This novel A/H7N9 virus emerged in humans after reassortment between viruses of poultry and wild bird origin. The hemagglutinin (HA) and neuraminidase (NA) genes are genetically related to H7 and N9 of viruses isolated from wild ducks while the other genes are closely related to A/H9N2 viruses circulating in poultry 12. It is most likely that the new A/H7N9 viruses have circulated undetected in domestic birds because of their low pathogenicity for poultry. A/H7N9 viruses were isolated from specimens at live poultry markets, pointing to domestic birds as a potential source of human infections 13.
Although A/H7N9 viruses harbour genetic traits associated with human adaptation of avian viruses and increased transmission between mammals, such as the Q217L substitution in HA (H7 numbering, 226 in H3 numbering) conferring a human receptor preference 14 and the E627K substitution in PB2 15, no sustained human-to-human transmission of A/H7N9 viruses has been reported to date. Apart from two confirmed cases that might have arisen from family clusters and for which human-to-human transmission cannot be ruled out, human cases of A/H7N9 infection were epidemiologically unrelated and identified in different parts of China 11.
Gaining knowledge on the ability of animal viruses to transmit via the airborne route is crucial to be able to mitigate future pandemics. Recently, the airborne transmissibility of the human isolate A/Shanghai/2/2013 was evaluated in ferrets and in pigs and was found to be less robust than for the 2009 pandemic A/H1N1 (pH1N1) virus 16. Here, we assessed the airborne transmissibility of a different human isolate, A/Anhui/1/2013 (AN1) in the ferret model as described 17,18. Both A/Shanghai/2/2013 and A/Anhui/1/2013 possess human receptor specificity and are of particular interest regarding transmission. Four donor ferrets were inoculated intranasally with 106 50% tissue culture infectious doses (TCID50) of AN1 virus isolate and the following day, four recipient ferrets were placed in adjacent cages, designed to prevent direct contact between animals but to allow transmission via the airborne route. Throat and nasal swabs were collected at 1, 3, 5 and 7 days post inoculation (dpi) from the donor ferrets and at 1, 3, 5, 7 and 9 days post exposure (dpe) from the recipient ferrets. Virus shedding from the donor ferrets was detected from 1 dpi onwards with infectious virus titers up to 106.5 TCID50/ml (Fig. 1, Panel A-D). AN1 virus was transmitted to 3 out of 4 recipient ferrets (F1, F2 and F3). Transmission was detected at 3 dpe for two ferrets (F2 and F3) and at 5 dpe for one ferret (F1) with infectious virus titers in respiratory swabs up to 106 TCID50/ml. All three animals infected via the airborne route seroconverted by two weeks after exposure, while recipient ferret F4 did not seroconvert. Using the same experimental set-up and protocol, we previously tested the transmissibility of the human pH1N1 virus, seasonal human A/H1N1 virus, and avian influenza A/H5N1 virus. While A/H5N1 virus was not transmitted between ferrets via the airborne route, human influenza viruses were transmitted in all donor-recipients pairs 17,18. Replication in donor ferrets inoculated with the AN1 virus and pandemic and seasonal A/H1N1 viruses was comparable, but virus shedding from recipient ferrets was less abundant and delayed for the AN1 virus as compared to the A/H1N1 viruses.
Figure 1.
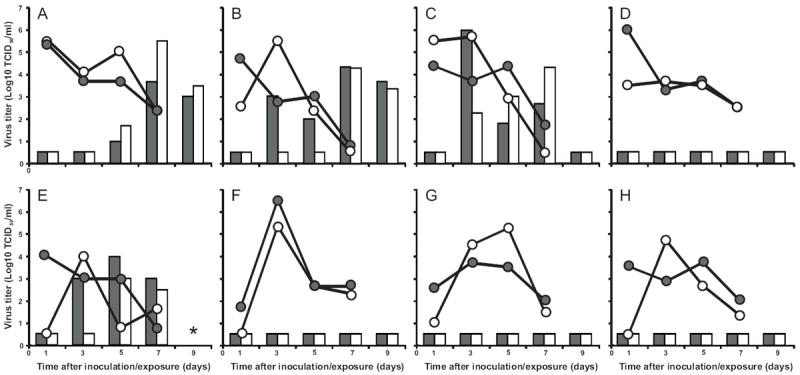
Airborne transmission of AN1 viruses between ferrets. Transmission experiments are shown for AN1 virus isolate in four ferret pairs (F1-F4) in panels A-D. A nose swab sample from the recipient ferret F1 at 7 dpe was used for the transmission experiments in four ferret pairs (F5-F8) shown in panels E-H. Data for individual transmission experiments is shown in each panel, with virus shedding in inoculated and airborne virus–exposed animals shown as lines and bars, respectively. Black circles and bars represent shedding from the throat; white circles and bars represent shedding from the nose. The asterisk indicates the lack of swab collection at 9 dpe for the recipient ferret euthanized at 8 dpe. The lower limit of detection is 0.5 log10 TCID50/mL.
Sanger sequencing was used to determine the consensus genome sequence of the three airborne-transmitted AN1 viruses isolated from recipient ferrets F1, F2 and F3 (Table 1) and substitutions were detected in all gene segments. Several of these were already present in the inoculum, demonstrating the presence of a mixture of viruses in the AN1 virus isolate. Consultation with other laboratories revealed that heterogeneous virus mixtures were present in A/H7N9 virus isolates shipped to others also. Viruses with different genotypes were transmitted (Table 1). Only two substitutions, N123D and N149D in HA, were consistently found in all three airborne-transmitted viruses. These substitutions are not part of potential N-linked glycosylation sites. Virus recovered from the recipient ferret F1 at 7 dpe, which contained the lowest number of substitutions compared to the AN1 virus isolate and had a high virus load, was used to inoculate four additional ferrets. One day later, these animals were paired with 4 recipient ferrets in transmission cages (Fig. 1, Panel E-H), of which one became infected (F5).
Table 1.
Sanger sequence analysis of full viral genomes of the AN1 virus inoculum and airborne transmitted viruses.
| Segment | nt position |
nt wt |
nt mut |
aa position |
aa wt |
aa mut |
Inoculum | Transm 1 | Transm 2 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| Recipients | |||||||||||
| F1 | F2 | F3 | F5 | ||||||||
|
|
|||||||||||
| PB2 | 411 | A | G | 128 | Gly | S1 | X | ||||
| PB2 | 1017 | C | T | 330 | Phe | S | X2 | X | |||
| PB2 | 1309 | C | T | 428 | Leu | S | X | X | |||
| PB2 | 1846 | C | T | 607 | Leu | S | X2 | X | |||
| PB1 | 1593 | G | A | 523 | Met | Ile | X | X | |||
| PB1 | 2055 | G | A | 678 | Ser | Asn | X | ||||
| PA | 1070 | A | G | 349 | Glu | Gly | X | ||||
| PA | 1167 | C | T | 380 | Asp | S | X | ||||
| PA | 1380 | C | T | 452 | His | S | X | ||||
| PA | 1616 | G | A | 531 | Arg | Lys | X | ||||
| PA | 1674 | G | T | 550 | Leu | S | X2 | ||||
| PA | 1776 | C | T | 584 | Cys | S | X2 | ||||
| HA | 442 | A | G | 123 | Asn | Asp | X2 | X | X2 | X | X |
| HA | 520 | A | G | 149 | Asn | Asp | X2 | X | X2 | X | X |
| HA | 704 | C | A | 210 | Ala | Glu | X2 | ||||
| NP | 718 | A | C | 225 | Ile | Leu | X2 | ||||
| NA | 46 | C | T | 10 | Thr | Ile | X2 | X2 | X2 | ||
| M | 652 | T | C | 225 | Ala | S | X2 | ||||
| NS | 180 | C | T | 52 | Leu | S | X2 | ||||
S; silent substitution
Mixture of wildtype and mutant nucleotides. Substitutions in bold were found in two subsequent transmission experiments and were phenotypically characterized.
None of the donor ferrets developed clinical signs upon intranasal inoculation. Two recipient ferrets were also without clinical signs, but one recipient ferret (F2) showed loss of appetite, ruffled fur, lethargy and breathing difficulties from 7 dpe onwards. Recipient ferret F5 became moribund and was euthanized at 8 dpe. Infectious virus titers up to 104.9 TCID50/g in the lungs and 105.8 TCID50/g in nasal turbinates were detected in ferret F5. Based on pathological analysis, this animal was suffering from a moderate multifocal suppurative rhinitis with associated virus antigen expression in the nasal respiratory and olfactory epithelium (Supplementary Table 4). No lesions or virus antigen expression were seen in the other parts of the respiratory tract, liver or brain that could explain the lethargic state of the ferret.
Consensus virus genome sequences as determined by Sanger sequencing of the airborne transmitted viruses recovered from recipient ferrets F1 and F5 were identical (Table 1). Substitutions N123D and N149D in HA and M523I in the basic polymerase 1 (PB1) were found consistently in two subsequent transmission experiments. Since mixed populations were detected in the inoculum using Sanger sequencing, next-generation sequencing was performed with respiratory samples of the donor/recipient pairs for which airborne transmission was observed. The entire HA gene and the PB1 part that contained the M523I substitution (nt positions 1126-1616) were sequenced using a 454 sequencing platform (Roche). None of the airborne-transmitted viruses possessed consensus genome sequences identical to that of the AN1 virus isolate (Table 2). Interestingly, an L217Q substitution, conferring a receptor switch from human to avian specificity (α2.6 to α2.3 linked sialic acids respectively), was detected in donor ferrets F1, F2, and F3 in 9.1%, 15.7%, and 24.5% of the total number of reads, respectively, but this substitution was not detected in any of the viruses isolated from the ferrets upon airborne exposure. By setting the detection threshold at 1%, we confirmed that the number of variable nucleotide positions in the genome of the AN1 virus isolate was high, and that a rapid gain in clonality occurred after two transmission experiments (Table 2 and Supplementary Table 1). The double substitution N123D+N149D in HA appeared to be selected in most airborne-transmitted viruses and constituted the main viral population after two subsequent transmission experiments (Supplementary Table 2). Although there appeared to be selection of N123D and N149D, it was not possible to determine whether the selection occurred at the level of individual or double substitutions. However, the rapid selection of substitutions in the HA and PB1 genes and the gain in clonality did not change transmission substantially enough to be detectable with the current group size of 4 ferrets.
Table 2.
Amino acid substitutions in the HA gene and the PB1 gene (nt positions 1126-1616) in AN1 viruses before and after transmission in ferrets as determined by 454 sequencing
| Gene | nt pos |
nt wt |
nt mut |
aa pos |
aa wt |
aa mut |
Inoculum | Donor F1 |
Recipient F1 |
Donor F2 |
Recipient F2 |
Donor F3 |
Recipient F3 |
Donor F5 |
Recipient F5 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HA | 117 | C | T | 14 | Thr | S1 | 19.52/66293 | 12.5/7954 | 20.3/10349 | 7.2/4763 | 9.6/5364 | ||||
| HA | 257 | C | T | 61 | Thr | Ile | 5,6/8142 | ||||||||
| HA | 442 | A | G | 123 | Asn | Asp | 48,7/8648 | 14.4/9183 | 99.8/6224 | 37.4/11196 | 28.5/12139 | 36.5/6810 | 90.1/8417 | 99.8/11576 | 99.9/10182 |
| HA | 448 | G | A | 125 | Ala | Thr | 1.8/7740 | 14.7/10044 | 20.5/10733 | 7.6/6088 | 10.4/7250 | ||||
| HA | 520 | A | G | 149 | Asn | Asp | 62.5/6163 | 17.9/6737 | 99.9/3622 | 50.4/8447 | 28.6/7818 | 61.2/5266 | 90.4/6840 | 99.7/9229 | 99.7/9047 |
| HA | 704 | C | A | 210 | Ala | Glu | 72.5/3903 | 28.4/4804 | 56.4/4109 | 8.5/3359 | |||||
| HA | 725 | T | A | 217 | Leu | Gln | 9.1/3831 | 15.7/4749 | - | 24.5/3322 | |||||
| HA | 1032 | G | T | 319 | Lys | Asn | 8.3/6447 | ||||||||
| HA | 1218 | C | T | 381 | Asn | S | 5.2/2102 | 23.4/1963 | |||||||
| HA | 1396 | G | A | 441 | Glu | Lys | 14.5/2299 | ||||||||
| HA | 1422 | G | A | 449 | Glu | S | 12.6/4027 | ||||||||
| HA | 1575 | C | T | 500 | Ser | S | 6.1/6532 | 15.5/2245 | 7.8/2387 | ||||||
| HA | 1706 | T | C | NCR4 | 93.0/470 | ||||||||||
| PB1 | 1404 | G | A | 460 | Gln | S | 6.8/603 | 11.9/1024 | |||||||
| PB1 | 1593 | G | A | 523 | Met | Ile | 100/256 | 82.2/1795 | 99.9/1064 |
S; silent substitution
Percentage variant present with a detection threshold of 5%
Number of reads
NCR; non coding region. Substitutions in bold were found in two subsequent transmission experiments and were phenotypically characterized. Substitution in italic and underlined (L217Q) corresponds to the receptor switch from α2.6 to α2.3 linked sialic acids preference.
Residues N123 and N149 are adjacent to the receptor binding site but do not interact directly with α2.3 and α2.6 linked sialic acids (Fig. 2). Recombinant viruses were generated based on seven gene segments of A/Puerto Rico/8/1934 (PR/8) with the wildtype AN1 HA and the AN1 HA with amino acid substitutions N123D (AN1N123D), N149D (AN1N149D) and N123D+N149D (AN1N123D,N149D). Binding to α2.3 linked sialic acids of AN1N123D, AN1N149D and AN1N123D,N149D viruses as assessed using a modified turkey red blood cell (TRBC) assay 19 was increased slightly by 2 to 4-fold compared to AN1 virus (Supplementary Table 3).
Figure 2.

Cartoon representation of a model of the trimer structure of HA of AN1 (green) and AN1N123D,N149D(cyan) bound to α2.6 (A) and α2.3 linked sialic acids (B). The structure of the three-sugar glycan NeuAcα2,6Galβ1-4GlcNAc (A) and NeuAcα2,3Galβ1-4GlcNAc (B) were docked into the H7 receptor binding site (RBS). The glycans and the amino acids substitutions discussed in the text are shown as sticks. Amino acids N123 and N149 are adjacent to the RBS and, in AN1, do not interact directly with the three-sugar glycans that are depicted in the figure. The mutations cause small changes in the position of some of the residues around the receptor binding site, notably R121 and D148, and additionally for the α2,6 linked glycan, residues S128 and Q213. The D123 mutant can form stronger interactions with the sidechain of R121 restricting the movement and orientating its sidechain to point towards the RBS and interact with the glycan. In AN1, N149 interacts with the neighbouring residue, D148, restricting its orientation. The D149 mutant allows the sidechain of D148 to rearrange and interact with the glycan. These changes allow both the α2,6- and α2,3-linked glycans to alter position and form more interactions with the HA. All residues are labelled in H7 numbering.
It was recently hypothesized that stability of HA in an acidic environment - such as mammalian nasal mucosa - is a determinant for airborne transmissibility of influenza viruses 20. It has also been noted that viruses that fuse at low pH have higher thermostability than those fusing at higher pH 21. We observed that fusion for AN1 HA occurred at pH 5.6, a higher pH than reported previously for human viruses 22. Neither the single N123D and N149D substitutions nor the double N123D+N149D substitution reduced the threshold pH for HA-mediated membrane fusion compared to the wildtype AN1 HA (Supplementary Fig. 1). Both single substitutions N123D and N149D and the double substitution N123D+N149D decreased the temperature stability compared to AN1 (Supplementary Fig. 2).
We also assessed the effect of the M523I substitution on the polymerase complex activity in mammalian cells using a minigenome assay at 33°C, the temperature of the mammalian upper respiratory tract, and at 37°C as previously described 23. No differences in polymerase activity were observed for the polymerase complex with or without the M523I substitution in PB1 (Supplementary Fig. S3).
Here we report that airborne transmission of AN1, as for A/Shanghai/2/2013, can occur between ferrets. Keeping in mind that quantitating transmission in our current experimental model is difficult, and that any transmission may not be directly extrapolated to transmission between humans, these data suggest that AN1 transmission is more efficient than for other avian influenza viruses, which are not airborne transmitted in ferrets, but less robust - with fewer animals becoming infected, and less and delayed virus shedding – as compared to seasonal and pandemic A/H1N1 virus transmission 17. Despite efficient virus replication in ferrets (Fig. 1) and attachment to α2.6 linked sialic acids (Supplementary Table 3), we speculate that the residual binding to α2.3 linked sialic acids (Supplementary Table 3), the fusion occurring at a relatively high pH (Supplementary Fig. S1), and instability of HA (Supplementary Fig. S2) may be responsible, at least in part, for limited transmission of AN1 A/H7N9 virus. Contrary to what was observed for A/H5N1 virus 18,20, the substitutions selected upon ferret passage and transmission of A/H7N9 virus - N123D and N149D – increased binding to α2.3 linked sialic acids, increased the pH threshold for membrane fusion, and decreased the thermostability of HA, thus not contributing to increased virus transmission.
Influenza viruses carrying human adaptation markers can arise in poultry. This appears to be the case for the newly emerged A/H7N9 viruses, but also during the 2003 A/H7N7 outbreak in the Netherlands 24 and for A/H5N1 viruses currently circulating in poultry 25. Fortunately, additional changes to e.g. further tune receptor preference, lower the pH for HA fusion, and increase HA stability, may be needed for the A/H7N9 viruses to transmit efficiently in mammals 18,20. Increased understanding of the mechanisms and molecular determinants that facilitate crossing the species barrier and airborne transmission of avian influenza viruses between mammals is urgently needed.
METHODS
Biocontainment
All experiments were conducted within the enhanced animal biosafety level 3 (ABSL3+) facility of Erasmus MC. The ABSL3+ facility consists of a negative pressurized (-30Pa) laboratory in which all in vivo and in vitro experimental work is carried out in class 3 isolators or class 3 biosafety cabinets, which are also negative pressurized (< -200Pa). Although the laboratory is considered ‘clean’ because all experiments are conducted in closed class 3 cabinets and isolators, special personal protective equipment, including laboratory suits, gloves and FFP3 facemasks is used. Air released from the class 3 units is filtered by High Efficiency Particulate Air (HEPA) filters and then leaves via the facility ventilation system, again via HEPA filters. Only authorized personnel that have received the appropriate training can access the ABSL3+ facility. For animal handling in the facilities, personnel always work in pairs. The facility is secured by procedures recognized as appropriate by the institutional biosafety officers and facility management at ErasmusMC and Dutch and United States government inspectors. Antiviral drugs (oseltamivir and zanamivir) are directly available 18.
Viruses
Influenza virus A/Anhui/1/2013 (AN1) was isolated from a human case of infection and passaged three times in embryonated chicken eggs and once in Madin-Darby Canine Kidney (MDCK) cells. The virus was kindly provided by the Chinese CDC via the WHO collaborating centre in the UK in the context of the WHO PIP framework. A synthetic construct of the AN1 HA gene segment was kindly provided by Dr Richard Webby. The PB2, PB1, PA and NP gene segments were amplified by reverse transcription polymerase chain reaction (RT-PCR) from the AN1 virus isolate and cloned in a modified version of the bidirectional reverse genetics plasmid pHW2000 26,27. In addition, the HA gene segment was cloned in pCAGGs expression plasmid. Mutations of interest (M523I in PB1, D123N, and D149N in HA) were introduced in reverse genetics and pCAGGs vectors using the QuikChange multi-site-directed mutagenesis kit (Stratagene, Leusden, the Netherlands) according to the instructions of the manufacturer. Recombinant viruses containing 7 gene segments of A/Puerto-Rico/8/1934 and wildtype AN1 HA or AN1 HA containing the mutations N123D and N149D were produced upon transfection of 293T cells. Virus stocks were propagated and titrated in MDCK cells as described previously 26.
Cells
MDCK cells were cultured in Eagle’s minimal essential medium (EMEM, Lonza Benelux BV, Breda, the Netherlands) supplemented with 10% fetal bovine serum (FBS), 100U/ml penicillin (Lonza), 100U/ml streptomycin (Lonza), 2mM glutamine (Lonza), 1.5mg/ml sodiumbicarbonate (Lonza), 10mM Hepes (Lonza), and non-essential amino acids (MP Biomedicals Europe, Illkirch, France). 293T cells were cultured in Dulbecco modified Eagle’s medium (DMEM, Lonza) supplemented with 10% FBS, 100U/ml penicillin, 100U/ml streptomycin, 2mM glutamine, 1mM sodium pyruvate (Gibco), and non-essential amino acids. Vero cells were cultured in Iscove’s modified Dulbecco’s medium + L-glutamine (IMDM, Lonza) supplemented with 10% FBS, 100IU/ml penicillin, 100mg/ml streptomycin, and 2mM glutamine.
Virus titration in MDCK cells
Virus titrations were performed as described previously 17. Briefly, MDCK cells were inoculated with tenfold serial dilutions of virus stocks, nose swabs, throat swabs and homogenized tissue samples. Cells were washed with PBS one hour after inoculation and cultured in 200μl of infection media, consisting of EMEM supplemented with 100U/ml penicillin, 100U/ml streptomycin, 2mM glutamine, 1.5mg/ml sodiumbicarbonate, 10mM Hepes, non-essential amino acids, and 20μg/ml trypsin (Lonza). Three days after inoculation, supernatants of cell cultures were tested for hemagglutinating activity using turkey erythrocytes as an indicator of virus replication in the cells. Infectious virus titers were calculated from four replicates each of the homogenized tissue samples, nose swabs, and throat swabs and for ten replicates of the virus stocks by the method of Reed and Munch 28.
Ferret models
An independent animal experimentation ethical review committee approved all animal studies. The Animal Experiments Committee (Dier Experimenten Commissie – DEC) judges ethical aspects of projects in which animals are involved. Research projects or educational projects involving laboratory animals can only be executed if they are approved by the DEC. The DEC considers the application and pays careful attention to the effects of the intervention on the animal, its discomfort, and weighs this against the social and scientific benefit to humans or animals. The researcher is required to keep the effects of the intervention to a minimum, based on the three Rs (Refinement, Replacement, Reduction). All experiments with ferrets were performed under animal biosafety level 3+ conditions in class 3 isolator cages.
Airborne transmission experiments were performed as described previously 17,18. In short, 4 female influenza virus and Aleutian Disease Virus seronegative adult ferrets, 1 to 2 years of age, were inoculated intranasally with 106 TCID50 of virus by applying 250μL of virus suspension to each nostril. The sample size of 4 is based on earlier calculations for this type of experiments 29. Each donor ferret was then placed in a transmission cage. One day after inoculation, one naïve recipient ferret was placed opposite each donor ferret. Each transmission pair was housed in a separate transmission cage designed to prevent direct contact but allowing airflow from the donor to the recipient ferret. Nose and throat swabs were collected on 1, 3, 5, and 7 dpi for donor ferrets and on 1, 3, 5, 7 and 9 dpe for the recipient ferrets. Virus titers in swabs were determined by end-point titration in MDCK cells. A nose swab sample of recipient ferret F1 at 7 dpe was used for the second transmission experiment, with a final dose of approximately 104 TCID50 for each ferret. All animals were monitored daily for clinical signs. Necropsy was performed on 1 ferret that was moribund and due to ethical reasons was removed before the end of the experiment. Nasal turbinates, trachea, lungs, brain, and liver were collected, homogenized in 3 ml of virus transport medium, after which the supernatant was collected and stored at -80°C. Virus titers in the supernatant were determined by end-point titration in MDCK cells. Duplicate samples of these tissues were fixed in 10% neutral-buffered formalin for pathological analysis.
Serology
The exposure of recipient ferrets to AN1 viruses was confirmed by an hemagglutination inhibition assay using standard procedures 30. Briefly, blood of the recipient ferrets was collected 12-14 dpe. Antisera were pre-treated overnight with receptor destroying enzyme (Vibrio cholerae neuraminidase) at 37°C and incubated at 56°C for 1h the next day. Twofold serial dilutions of the antisera, starting at a 1:20 dilution, were mixed with 25μl of a virus stock containing 4 hemagglutinating units and were incubated at 37°C for 30 minutes. Subsequently, 25μl 1% turkey erythrocytes were added and the mixture was incubated at 4°C for 1h. Hemagglutination inhibition was expressed as the reciprocal value of the highest dilution of the serum that completely inhibited agglutination of virus and erythrocytes.
Sequencing
Viral RNA was extracted from respiratory swab samples collected from the ferrets that were infected via the airborne route and the virus inoculum, using the High Pure RNA Isolation Kit (Roche). All eight gene segments of the influenza viruses were amplified by RT-PCR using 8 primer sets that cover the full viral genome which specifically amplify each gene segment 31 and sequenced using a BigDye Terminator v3.1 Cycle sequencing kit (Applied Biosystems, Nieuwerkerk a/d IJssel, the Netherlands) and a 3130XL genetic analyzer (Applied Biosystems), according to the instructions of the manufacturer. The consensus sequence was determined for viruses isolated from the following samples: virus inoculum obtained after three egg passages and one MDCK passage, recipient F1: nose swab 7 dpe, recipient F2: throat swab 5 dpe, recipient F3: nose swab 5 dpe, and recipient F5: nose swab 5 dpe. Primer sequences are available upon request. Sequences were compared to reference sequences obtained from the GISAID EpifluTM database (accession numbers EPI439503 through EPI439510).
Viral RNA was extracted from the virus inoculum and respiratory swabs of ferrets using the High Pure RNA Isolation Kit (Roche). RNA was subjected to RT-PCR, using 5 primer sets (for HA: set 1; AGCAAAAGCAGGGGATACAA and GTATGACTTAGTCATCTGCGG, set 2; GGCGGAATTGACAAGGAAGC and CCACTATGATAGCAATCTCCTTCAC, set 3; GTGACTTTCAGTTTCAATGGGGC and GATTCTCCATTGCTACCAAGAGTTC, set 4; CTAACCAACAATTTGAGTTAATAGAC and AGTAGAAACAAGGGTGTTTT, for PB1; CAGCGGAAATGCTCGCAAAT and TTGAGCTGTTGCTGGTCCAA) that amplify the region containing the PB1 M523I mutation and the complete HA gene segment. These fragments, approximately 500-600 nucleotides in length, were sequenced using the Roche 454 GS Junior sequencing platform. The fragment library was created for each sample according to the manufacturer’s protocol without DNA fragmentation (GS FLX Titanium Rapid Library Preparation, Roche). The emulsion PCR (Amplification Method Lib-L) and GS Junior sequencing run were performed according to instructions of the manufacturer (Roche). Sequence reads from the GS Junior sequencing data were sorted by bar code and aligned to reference sequence A/Anhui/1/2013 using CLC Genomics software 6.0.2. Primers used to amplify the fragments were trimmed at the 3’ and 5’ ends of the sequence reads. For quality control, sequence reads were trimmed at the 3’ end for Phred scores less than 30. The threshold for the detection of single nucleotide polymorphisms was manually set at 1% and 5%.
Model Generation
A model of the structure of the HA of AN1 was built by using MODELLER 32 based upon the crystal structure of HA of H7N3 virus A/turkey/Italy/02 (PDB code 1TI8). The N123D and N149D mutations were introduced into the structure using the program Andante 33. Three-sugar glycans NeuAcα2,6Galβ1-4GlcNAc and NeuAcα2,3Galβ1-3GlcNAc were docked into the binding site of the AN1 HA structure and that of the AN1N123D,N149D HA structure. Several strategies were then used to explore the docking of the glycan within the binding pocket. Alternative glycan conformations were produced by altering the phi angle of the glycosidic bond between the second and third sugars and the exploration of alternative side chain conformations of amino acids within the binding pocket was performed by using a rotamer search 33. Lower energy structures were produced iteratively, until no further energy changes were seen. All simulations were performed using the University of Cambridge CAMGRID computing cluster 34.
Modified TRBC hemagglutination assay
Modified TRBC assays were performed as described previously 35. Briefly, all α2,3-, α2,6, α2,8-, and α2,9-linked sialic acids were removed from the surface of TRBC by incubating 62.5μl of 1% TRBC in PBS with 50mU Vibrio cholerae NA (VCNA; Roche, Almere, Netherlands) in 8mM calcium chloride at 37°C for 1 hour. Removal of sialic acids was confirmed by observation of complete loss of hemagglutination of the TRBC by control influenza A viruses. Subsequently, resialylation was performed using 0.25mU of α2,3-(N)-sialyltransferase (COSMOBIO, bio-connect, Huisen, Netherlands) or 12mU of α2,6-(N)-sialyltransferase (COSMOBIO, bio-connect, Huisen, Netherlands) and 1.5mM CMP-sialic acid (Sigma-Aldrich, Zwijndrecht, Netherlands) at 37°C in 75μl for 2h to produce α2,3-TRBC and α2,6-TRBC, respectively. After a washing step, the TRBC were resuspended in PBS containing 1% bovine serum albumin to a final concentration of 0.5% TRBC. Resialylation was confirmed by hemagglutination of viruses with known receptor specificity; recombinant viruses with six or seven gene segments of influenza virus A/PR/8/1934 and the HA and NA of A/Vietnam/11/2004 H5N1 without the basic cleavage site or the HA of A/Netherlands/213/2003 H3N2. The receptor specificity of mutant viruses (recombinant viruses with seven gene segments of influenza virus A/PR/8/1934 and the HA of AN1 with or without the substitutions D123N and or D149N) was tested by performing a standard hemagglutination assay with the modified TRBC. In brief, serial two-fold dilutions of virus in PBS were made in a 50μl volume; 50 μl of 0.5% TRBC were added, followed by incubation for 1h at 4°C before determining the hemagglutination titer.
Fusion assay
Influenza virus HA induced cell fusion was tested in Vero-118 cells transfected with 5μg of pCAGGs-HA using Xtremegene transfection reagent (Roche). One day after transfection, cells were harvested using trypsin-EDTA and plated in 6-wells plates. The next morning, cells were washed and medium was replaced with IMDM medium containing 10μg/ml of trypsin. After one hour, cells were washed with PBS and exposed to PBS at pH 5.0, 5.2, 5.4, 5.6, 5.8, or 6.0 for 10 minutes at 37°C. Subsequently, the PBS was replaced by IMDM supplemented with 10% FBS. Eighteen hours after the pH shock, cells were fixed using 80% ice-cold acetone, washed, and stained using a 20% Giemsa solution (Merck Millipore, Darmstadt, Germany).
HA stability assay
The stability of HAs from the mutant viruses (recombinant viruses with seven gene segments of influenza virus A/PR/8/1934 and the HA of AN1 with or without the substitutions N123D and/or N149D and the HA of H5N1 A/Indonesia/5/2005 (INDO) with and without the substitution T318I) was evaluated by performing a thermostability assay. In short, viruses were diluted to 64 HA units/25μl using PBS. The samples were incubated in a thermal cycler for 30 minutes at temperature of 50°C, 52°C, 54°C, 56°C, and 58°C. Subsequently, the HA titer was determined by performing a hemagglutination assay using turkey erythrocytes.
Minigenome assay
A model viral RNA (vRNA), consisting of the firefly luciferase open reading frame flanked by the noncoding regions (NCRs) of segment 8 of influenza A virus, under the control of a T7 RNA polymerase promoter was used for minigenome assay 36. The reporter plasmid (0.5μg) was transfected into 293T cells in 6-well plates, along with 0.5μg of each of the pHW2000 plasmids encoding PB2, PB1, PA, and NP; 1μg of pAR3132 expressing T7 RNA polymerase and 0.02μg of the Renilla luciferase expression plasmid pRL (Promega, Leiden, Netherlands) as an internal control. 48 hours after transfection, luminescence was measured using the Dual-Glo Luciferase Assay System (Promega) according to instructions of the manufacturer in a TECAN Infinite F200 machine (Tecan Benelux bv, Giessen, Netherlands). Relative light units (RLU) were calculated as the ratio of Firefly and Renilla luciferase luminescences.
Pathology & Immunohistochemistry
After fixation in 10% neutral-buffered formalin, tissues were embedded in paraffin, sectioned at 3μm, and stained with hematoxylin and eosin (HE) for the detection of histological lesions by light microscopy. For the detection of virus antigen by immunohistochemistry, tissues were stained with a monoclonal antibody against influenza A virus nucleoprotein as the primary antibody as described previously 37. After determining the cell types expressing viral antigen, the percentage of positively staining cells per tissue was estimated and ranked on an ordinal scale: 0, 0% of cells; 1, 1-25%; 2, 25-50%; 3, >50%.
Supplementary Material
Acknowledgments
We thank Peter van Run, Stefan van der Vliet and Anne Reiners for technical assistance. We thank the Chinese CDC for providing the A/Anhui/1/2013 isolate and Dr. Richard Webby for the synthetic construct of HA. This work was financed through NIAID-NIH contract HHSN266200700010C and EU FP7 programs EMPERIE and ANTIGONE.
Footnotes
Author Contributions: M.R., E.J.A.S. and R.A.M.F. designed the experiments. M.R., E.J.A.S, M.G., M.S., T.M.B., S.B., D.M., P.L., M.L. and S.H. performed the experiments, M.R., E.J.A.S., T.M.B., S.B., J.M.B. and D.F.B. analyzed the data, M.R., E.J.A.S., D.J.S., T.K., G.F.R., A.D.M.E. and R.A.M.F. wrote the manuscript.
Supplementary Information is linked to the online version of the paper.
The authors declare no competing financial interest.
References
- 1.Webster RG, Bean WJ, Gorman OT, Chambers TM, Kawaoka Y. Evolution and ecology of influenza A viruses. Microbiol Rev. 1992;56:152–179. doi: 10.1128/mr.56.1.152-179.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beigel JH, et al. Avian influenza A (H5N1) infection in humans. N Engl J Med. 2005;353:1374–1385. doi: 10.1056/NEJMra052211. [DOI] [PubMed] [Google Scholar]
- 3.Hirst M, et al. Novel avian influenza H7N3 strain outbreak, British Columbia. Emerg Infect Dis. 2004;10:2192–2195. doi: 10.3201/eid1012.040743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fouchier RA, et al. Avian influenza A virus (H7N7) associated with human conjunctivitis and a fatal case of acute respiratory distress syndrome. Proc Natl Acad Sci USA. 2004;101:1356–1361. doi: 10.1073/pnas.0308352100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ostrowsky B, et al. Low pathogenic avian influenza A (H7N2) virus infection in immunocompromised adult, New York, USA, 2003. Emerg Infect Dis. 2012;18:1128–1131. doi: 10.3201/eid1807.111913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen Y, et al. Human infections with the emerging avian influenza A H7N9 virus from wet market poultry: clinical analysis and characterisation of viral genome. Lancet. 2013;381:1916–25. doi: 10.1016/S0140-6736(13)60903-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arzey GG, et al. Influenza virus A (H10N7) in chickens and poultry abattoir workers, Australia. Emerg Infect Dis. 2012;18:814–816. doi: 10.3201/eid1805.111852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.WHO. Avian influenza A(H7N9) virus. 2013 http://www.who.int/influenza/human_animal_interface/influenza_h7n9/en/index.html.
- 9.WHO. Human infection with influenza A(H7N9) virus in China. 2013 Apr 1; http://www.who.int/csr/don/2013_04_01/en/index.html.
- 10.Gao R, et al. Human infection with a novel avian-origin influenza A (H7N9) virus. N Engl J Med. 2013;368:1888–1897. doi: 10.1056/NEJMoa1304459. [DOI] [PubMed] [Google Scholar]
- 11.Li Q, et al. Preliminary Report: Epidemiology of the Avian Influenza A (H7N9) Outbreak in China. N Engl J Med. 2013 doi: 10.1056/NEJMoa1304617. [DOI] [Google Scholar]
- 12.Liu D, et al. Origin and diversity of novel avian influenza A H7N9 viruses causing human infection: phylogenetic, structural, and coalescent analyses. Lancet. 2013;381:1926–32. doi: 10.1016/S0140-6736(13)60938-1. [DOI] [PubMed] [Google Scholar]
- 13.Cowling BJ, et al. Comparative epidemiology of human infections with avian influenza A H7N9 and H5N1 viruses in China: a population-based study of laboratory-confirmed cases. Lancet. 2013;382:129–137. doi: 10.1016/S0140-6736(13)61171-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xiong X, et al. Receptor binding by an H7N9 influenza virus from humans. Nature. 2013 doi: 10.1038/nature12372. [DOI] [PubMed] [Google Scholar]
- 15.Steel J, Lowen AC, Mubareka S, Palese P. Transmission of influenza virus in a mammalian host is increased by PB2 amino acids 627K or 627E/701N. PLoS Pathog. 2009;5:e1000252. doi: 10.1371/journal.ppat.1000252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhu H, et al. Infectivity, Transmission, and Pathology of Human H7N9 Influenza in Ferrets and Pigs. Science. 2013;341:183–6. doi: 10.1126/science.1239844. [DOI] [PubMed] [Google Scholar]
- 17.Munster VJ, et al. Pathogenesis and transmission of swine-origin 2009 A(H1N1) influenza virus in ferrets. Science. 2009;325:481–483. doi: 10.1126/science.1177127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Herfst S, et al. Airborne transmission of influenza A/H5N1 virus between ferrets. Science. 2012;336:1534–1541. doi: 10.1126/science.1213362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chutinimitkul S, et al. In vitro assessment of attachment pattern and replication efficiency of H5N1 influenza A viruses with altered receptor specificity. J Virol. 2010;84:6825–6833. doi: 10.1128/JVI.02737-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Imai M, et al. Experimental adaptation of an influenza H5 HA confers respiratory droplet transmission to a reassortant H5 HA/H1N1 virus in ferrets. Nature. 2012;486:420–428. doi: 10.1038/nature10831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ruigrok RW, et al. Conformational changes in the hemagglutinin of influenza virus which accompany heat-induced fusion of virus with liposomes. Virology. 1986;155:484–497. doi: 10.1016/0042-6822(86)90210-2. [DOI] [PubMed] [Google Scholar]
- 22.Galloway SE, Reed ML, Russell CJ, Steinhauer DA. Influenza HA subtypes demonstrate divergent phenotypes for cleavage activation and pH of fusion: implications for host range and adaptation. PLoS Pathog. 2013;9:e1003151. doi: 10.1371/journal.ppat.1003151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Subbarao EK, London W, Murphy BR. A single amino acid in the PB2 gene of influenza A virus is a determinant of host range. J Virol. 1993;67:1761–1764. doi: 10.1128/jvi.67.4.1761-1764.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jonges M, et al. Comparative analysis of avian influenza virus diversity in poultry and humans during a highly pathogenic avian influenza A (H7N7) virus outbreak. J Virol. 2011;85:10598–10604. doi: 10.1128/JVI.05369-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Russell CA, et al. The potential for respiratory droplet-transmissible A/H5N1 influenza virus to evolve in a mammalian host. Science. 2012;336:1541–1547. doi: 10.1126/science.1222526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.de Wit E, et al. Efficient generation and growth of influenza virus A/PR/8/34 from eight cDNA fragments. Virus research. 2004;103:155–161. doi: 10.1016/j.virusres.2004.02.028. [DOI] [PubMed] [Google Scholar]
- 27.Hoffmann E, Neumann G, Kawaoka Y, Hobom G, Webster RG. A DNA transfection system for generation of influenza A virus from eight plasmids. Proc Natl Acad Sci USA. 2000;97:6108–6113. doi: 10.1073/pnas.100133697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Reed LJ, Munch H. A simple method of estimating fifty percent endpoints. Am J Hyg. 1938;27:493–497. [Google Scholar]
- 29.Nishiura H, Yen HL, Cowling BJ. Sample size considerations for one-to-one animal transmission studies of the influenza A viruses. PLoS One. 2013;8:e55358. doi: 10.1371/journal.pone.0055358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hirst GK. Studies of Antigenic Differences among Strains of Influenza a by Means of Red Cell Agglutination. J Exp Med. 1943;78:407–423. doi: 10.1084/jem.78.5.407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hoffmann E, Stech J, Guan Y, Webster RG, Perez DR. Universal primer set for the full-length amplification of all influenza A viruses. Arch Virol. 2001;146:2275–2289. doi: 10.1007/s007050170002. [DOI] [PubMed] [Google Scholar]
- 32.Sali A, Blundell TL. Comparative protein modelling by satisfaction of spatial restraints. J Mol Biol. 1993;234:779–815. doi: 10.1006/jmbi.1993.1626. [DOI] [PubMed] [Google Scholar]
- 33.Smith RE, Lovell SC, Burke DF, Montalvao RW, Blundell TL. Andante: reducing side-chain rotamer search space during comparative modeling using environment-specific substitution probabilities. Bioinformatics. 2007;23:1099–1105. doi: 10.1093/bioinformatics/btm073. [DOI] [PubMed] [Google Scholar]
- 34.Calleja M, Blanshard L, Bruin R, Chapman C, Thandavan A, Tyer R, Wilson P, Alexandrov V, Allen RJ, Brodholt J, Dove MT, Emmerich W, Kleese van Dam K. Grid tool integration within the eMinerals project. Proceedings of the UK e-Science All Hands Meeting 2004; 2004. [Google Scholar]
- 35.Nobusawa E, Ishihara H, Morishita T, Sato K, Nakajima K. Change in receptor-binding specificity of recent human influenza A viruses (H3N2): a single amino acid change in hemagglutinin altered its recognition of sialyloligosaccharides. Virology. 2000;278:587–596. doi: 10.1006/viro.2000.0679. [DOI] [PubMed] [Google Scholar]
- 36.de Wit E, et al. Molecular determinants of adaptation of highly pathogenic avian influenza H7N7 viruses to efficient replication in the human host. J Virol. 2010;84:1597–1606. doi: 10.1128/JVI.01783-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.van Riel D, Rimmelzwaan GF, van Amerongen G, Osterhaus AD, Kuiken T. Highly pathogenic avian influenza virus H7N7 isolated from a fatal human case causes respiratory disease in cats but does not spread systemically. Am J Pathol. 2010;177:2185–2190. doi: 10.2353/ajpath.2010.100401. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


