Abstract
Objectives
In complex conditions such as cirrhosis, management of urgent issues can leave little time for patient education. However, efforts such as sodium restriction and lactulose titration require an informed patient. We aimed to understand and improve patient knowledge about disease self-management.
Study
150 outpatients with cirrhosis in a tertiary hepatology clinic were given a survey to test disease self-management knowledge. Patients were then provided education using a concise booklet, and three months later were invited to participate in a follow-up survey. Demographic and clinical correlates of baseline knowledge were analyzed with linear regression, and t-test for matched pairs was used to compare knowledge scores before and after the educational intervention.
Results
Only 53% of the 15 questions were answered correctly in the baseline survey. The most commonly missed items related to diet, such as the sodium content of sea salt, as well as the safety of medications such as acetaminophen and statins. The level of patient knowledge was not associated with age, gender, etiology or severity of liver disease, or length of time followed in the clinic. After the educational intervention, 115/150 (77%) returned the follow-up survey. In this group, the median knowledge score improved from 53% to 67% (p<0.001), and improvement occurred across all domains tested.
Conclusions
Cirrhosis patients lack the knowledge required to effectively manage their disease. A simple educational intervention may improve patient knowledge. Further studies are needed to determine whether improved knowledge translates into better outcomes.
Introduction
Cirrhosis is the final common pathway for the majority of liver diseases, and is a complex chronic condition which causes population mortality rates of approximately 5-10/100,000 person-years worldwide.(1) Advances in medical care have identified numerous interventions to improve patient outcomes: randomized-controlled trials have demonstrated benefit from prophylaxis of variceal hemorrhage(2) and spontaneous bacterial peritonitis,(3) and there exists a long list of evidence-based preventive care recommendations including vaccination against hepatitis A and B, and screening for hepatocellular carcinoma.(4) However, while physicians can make recommendations, it is up to the patients to carry them out. Patients must take their medications properly, titrate their lactulose, watch their diet, and show up to their appointments. Successful cirrhosis management, therefore, requires that patients be educated on why and how to perform these duties.(5)
In most healthcare settings, patient education consists of whatever can be squeezed in to the clinic visit, supplemented by the occasional handout as well as (mis)information on the Internet. It has been estimated that 90 percent of chronic disease care occurs outside of the clinic visit,(6) and the literature in other chronic diseases suggests that patients are often non-adherent or poorly manage their medical conditions.(7) This is likely to be especially true in cirrhosis, a complex condition that is poorly understood by many people. In a prior study, we found that patient involvement in their healthcare was associated with higher rates of screening for hepatocellular carcinoma.(8) However, no data exists on patient knowledge about other critical aspects of cirrhosis management such as diet, over-the-counter medications, and important health maintenance activities. Therefore, the aim of this study was to measure levels and correlates of patient knowledge, as well as to determine whether this knowledge can be improved by a simple educational intervention.
Materials and Methods
This was a cross-sectional survey, followed by an educational intervention and then repeated survey (pre-post design). Consecutive patients with cirrhosis were recruited over a period of 4 months from a general hepatology clinic at a liver transplant referral center. Patients were identified as having cirrhosis by an attending hepatologist, for enrollment into a database used as part of routine clinical care for disease management and quality improvement. The diagnosis of cirrhosis was made by liver biopsy or clinical manifestations of portal hypertension in the setting of underlying liver disease. The only exclusion criteria were inability to read and write in English, or Grade 2 or higher hepatic encephalopathy. Clinical and demographic characteristics were obtained from the medical record. 150 out of 171 (88%) patients approached provided informed consent to participate in this study, which was approved by our Institutional Review Board and conformed to the 1975 Declaration of Helsinki.
Patients who agreed to participate were given a 15-item paper and pencil survey covering topics such as diet, over-the-counter medications, and health maintenance activities. The full survey can be seen in Table 2. Patients were then provided with a concise educational booklet on cirrhosis self-management that we developed, along with a brief overview of its contents. This 14-page booklet, which covers prevention and management of complications of cirrhosis as well as miscellaneous health management topics such as surgery and hospitalizations, can be seen in Appendix A. The booklet also contains sections for patients to keep track of their medications, appointments, and weight. Patients were asked to take the booklet to every appointment, in order to emphasize its importance.
Table 2.
Percentage of subjects (n=150) who answered each question correctly in the baseline survey. Items are grouped by clinical domain.
| Item | Question | Percentage correct |
|---|---|---|
| Ascites | ||
| 2 | In order to follow a “low sodium” diet, all I have to do is avoid adding salt to my food | 81% |
| 3 | Sea salt has less sodium than regular table salt | 48% |
| 5 | Patients with cirrhosis who develop swelling (retaining fluid) in the abdomen and legs, should cut down on drinking fluids to help this problem | 76% |
| 6 | A low sodium diet means eating less than 5,000 mg of sodium per day | 44% |
| 7 | Patients with cirrhosis and ascites (fluid in the belly) who develop a hernia at their belly button should have this surgically repaired | 44% |
| 13 | If the sodium level in my blood is low, this means I should eat more salt | 88% |
| Hepatic encephalopathy | ||
| 8 | Which is the best answer: (a) lactulose should be taken at a fixed dose every day, or (b) the dose of lactulose should be adjusted based on the number of bowel movements | 56% |
| 9 | Patients with hepatic encephalopathy (confusion related to cirrhosis) should reduce their intake of (a) total protein, (b) animal protein, or (c) fatty foods | 12% |
| 10 | Patients with cirrhosis have a higher rate of car accidents than people without cirrhosis | 24% |
| Concomitant medications | ||
| 1 | Medications to lower cholesterol (“statins”) such as Lipitor or Zocor are safe for patients with cirrhosis | 29% |
| 4 | For patients with cirrhosis who have minor aches and pains, the safest over-the-counter medication is (a) Motrin, (b) Tylenol, (c) Aleve, (d) Aspirin | 44% |
| Health maintenance | ||
| 11 | Patients with cirrhosis get an ultrasound every six months in order to (a) determine liver function, (b) look for gallstone, (c) look for liver cancer | 58% |
| 12 | Patients with cirrhosis should get the flu shot every year | 87% |
| 14 | Patients with cirrhosis should be vaccinated against hepatitis A and hepatitis B | 79% |
| 15 | Patients with cirrhosis always have abnormal liver enzymes | 44% |
Three months after their initial survey, each patient was then mailed a repeat survey, in order to determine whether the booklet had improved their knowledge. The correct answers were not made available until after the follow-up survey. The patients were allowed to refer to their booklet when answering the follow-up survey, in keeping with modern educational philosophies on “just-in-time” learning.(9)
Survey responses were transcribed to a computer database in duplicate fashion so as to limit errors. Patient knowledge was quantified as the percentage of questions answered correctly. Fewer than 5% of items were not answered; a missing answer was counted as incorrect. Linear regression was used to determine demographic and clinical correlates of baseline patient knowledge. Although patient knowledge scores were not normally distributed, examination of residuals demonstrated no evidence of heteroskedasticity, thus supporting the use of parametric methods. Finally, t-test for matched pairs was used to compare patient knowledge scores before and after receiving the educational intervention. All calculations were performed using StataSE v11.0 (Statacorp, College Station TX).
Results
As shown in Table 1, the 150 patients with cirrhosis were mostly middle-aged, predominately white, and nearly half had viral hepatitis as the etiology of their liver disease. The majority (70%) had Child A cirrhosis, and they had been followed in the hepatology clinic for a median of two years. One third of patients were on diuretics, and one quarter were on medications for hepatic encephalopathy. None of the patients were on the transplant list, and only 3 had hepatocellular carcinoma, as these patients are followed in other clinics at our institution.
Table 1.
Demographic and clinical characteristics of cirrhosis subjects (n=150).
| Median age (years) | 57 (range 20 – 78) |
| Gender | 59 % male |
| Race/ethnicity | |
| White | 82% |
| Black | 3% |
| Hispanic | 4% |
| Other | 17% |
| Etiology of liver disease | |
| Alcohol | 16% |
| Viral hepatitis | 48% |
| Cryptogenic/fatty liver | 19% |
| Other | 17% |
| Median MELD score | 8 (range 6 – 19) |
| Child-Pugh class | |
| A | 70% |
| B | 27% |
| C | 3% |
| Hepatocellular carcinoma | 2% |
| Median length followed in liver clinic (months) | 23 (range 0 – 198) |
| Medications | |
| Diuretics | 37% |
| For encephalopathy | 23% |
MELD=Model for End-stage Liver Disease
Baseline knowledge
The median score on the baseline knowledge survey was 53% (range 2%-87%). In other words, only half of the questions were answered correctly. The percentage of patients who answered each individual question correctly is shown in Table 2, grouped by clinical domain. The most commonly missed questions related to risk of motor vehicle accidents, dietary management of hepatic encephalopathy, and the safety of statin medications. Strikingly, fewer than half of patients correctly identified Tylenol as being the safest over-the-counter pain medication, and the majority of patients thought that sea salt contains less sodium than table salt.
Patients on diuretics scored slightly higher on questions in the ascites domain (70% vs 60%, p=0.006), and there was a trend toward higher scores in the encephalopathy domain by those patients on medications for hepatic encephalopathy (35% vs 29%, p=0.2). In regards to correlates of overall patient knowledge, only Hispanic ethnicity was weakly associated with a lower score (coefficient= -.12, p=0.35). Otherwise the level of patient knowledge was not associated in bivariate analysis with age, gender, etiology or severity of liver disease, or length of time followed in the clinic.
Follow-up survey
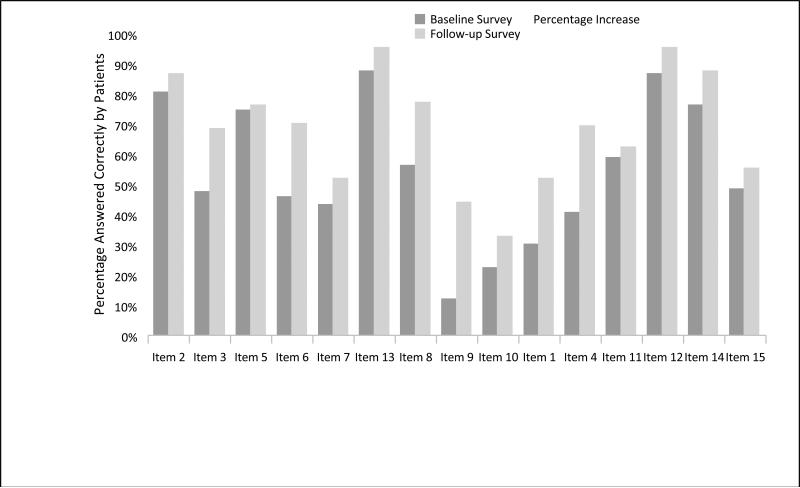
Among the 150 subjects who completed the baseline survey, 115 (77%) responded to the follow-up survey three months after receiving the educational intervention. There were no differences in demographic or clinical characteristics or baseline knowledge between responders and non-responders to the follow-up survey (data not shown). Among these 115 subjects, the median knowledge score improved from 53% to 67% (p<0.001), suggesting that the education was effective. All of the items were answered correctly more often in the follow-up survey than the baseline survey. As shown in Figure 1, the most significant improvement was seen with items #1, 3, 4, 6, 8, and 9, which were answered correctly by at least 20% more subjects on the follow-up survey than at baseline. However, correct responses to questions #9 and 10 remained suboptimal at <50%.
Figure 1.
Percentage of patients who answered each question correctly in the baseline and follow-up surveys.
Discussion
This study found that cirrhosis patients lack adequate knowledge about important information needed to self-manage their disease. For example, more than half of patients thought that sea salt has less sodium than regular table salt. Additionally, more than half of patients thought that nonsteroidal anti-inflammatory medications are safer than acetaminophen. The confusion regarding the safety of acetaminophen products may in part be due to media reports regarding their known dose-dependent hepatotoxicity.(10) At therapeutic doses, however, the available data suggests that acetaminophen is preferred over nonsteroidals due to lower risk of gastrointestinal bleeding and improved renal safety profile.(11) Similarly, more than two-thirds thought that statins are unsafe in patients with liver disease. The difficulty in this area may in part relate to the Food and Drug Administration labeling of these agents which states ”Patients with liver disease should not take these medications before consulting with their doctor.”(12) However, there are several clinical trials demonstrating the safety and perhaps even efficacy of statin use in patients with compensated chronic liver disease.(13, 14) Finally, awareness of the risk of car accidents among patients with cirrhosis was quite low. Several recent studies have shown the accident risk to be many times higher in cirrhosis patients, even those without overt encephalopathy, than in age-matched controls.(15, 16)
This study also showed that a simple educational intervention – providing a concise booklet and emphasizing its importance – was associated with a 26% improvement in patient knowledge. This degree of improvement is particularly noteworthy since the intervention required very few resources. Whether this improved knowledge would translate into improved patient outcomes is unknown, and these findings provide impetus for further studies on this topic.
No prior data exists on patient education in cirrhosis, and the literature on patient education in other chronic diseases is surprisingly sparse. In one landmark randomized study of pre-dialysis patients with chronic kidney disease, a 75-minute educational intervention led to longer survival and a delay in the time until dialysis was required.(17) On the basis of this literature and the results of our study, we encourage others to adapt our booklet for use in their clinics. Providing such a booklet is cheap and easy, and we can anecdotally report that patients are very appreciative of this information. However, it remains to be seen whether improved patient knowledge will transplant into better outcomes. Therefore, more intensive educational interventions should require longitudinal randomized trials to determine their incremental effectiveness and cost-effectiveness. In addition, given the frequent cognitive impairment of patients with cirrhosis, it may be useful to investigate whether educating informal caregivers (family and friends) could facilitate optimal disease management.(18)
Our study is limited by its single-center nature. Patients referred to a transplant center may have higher levels of education, social support, or self-efficacy than patients in a community setting. For the purpose of maximizing response rates we did not collect detailed information about subjects’ formal educational background, nor did we formally assess cognitive function. Thus, the absolute level of knowledge may not be generalized to other settings. Additionally, the pre-post design may have magnified the impact of the educational booklet, since subjects knew they would be tested on the material. Of note, the follow-up survey was an “open book” test, in that nothing prevented the subjects from looking up the answers to the questions in their booklet. From the design of the study, it is impossible to know whether patients had memorized the information or had to look it up. However, even if they did need to look it up, this means they would be able to find relevant information when they need it to manage their care. In this regard, the assessment method satisfies modern educational philosophies on “just-in-time” learning.(9) Finally, some of the questions pertained to complications of cirrhosis that some patients may have not experienced, and thus they would not be expected to know this information (e.g. titration of lactulose). Nonetheless, the patterns were consistent across all questions including those that every patient with cirrhosis should know (e.g. safest over-the-counter pain medication).
In conclusion, we found that patients with cirrhosis lack important knowledge about disease self-management. This lack of knowledge may pose a barrier to physicians who are attempting to maximize outcomes for their patients. We found that patient knowledge, or at least their ability to access the necessary information, was improved by a simple educational intervention. We speculate that future efforts in this area could lead to decreased hospitalizations and resource utilization. Further studies are needed to determine whether more intensive educational interventions, particularly those that involve informal caregivers, can effectively and cost-effectively improve outcomes in patients with cirrhosis.
What is current knowledge?
- Cirrhosis is a complex condition
- Medical management requires patient cooperation
- The extent of patient knowledge about disease self-management is unknown
What is new here?
- Patients with cirrhosis lack critical self-management knowledge
- Current strategies for patient education in most clinics are inadequate
- A simple systematic educational intervention can improve patient knowledge
Acknowledgments
Financial support: this study was funded in part by K23DK085304 from the National Institutes of Health (MLV)
Footnotes
Guarantor of the article: Michael Volk
All of the authors contributed to design of the study, data collection and analysis, and manuscript preparation
Disclosures: none of the authors has any conflict of interest to disclose
References
- 1.Bosetti C, Levi F, Lucchini F, et al. Worldwide mortality from cirrhosis: an update to 2002. J Hepatol. 2007;46:827–39. doi: 10.1016/j.jhep.2007.01.025. [DOI] [PubMed] [Google Scholar]
- 2.Garcia-Tsao G, Sanyal AJ, Grace ND, et al. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology. 2007;46:922–38. doi: 10.1002/hep.21907. [DOI] [PubMed] [Google Scholar]
- 3.Runyon BA. Management of adult patients with ascites due to cirrhosis: an update. Hepatology. 2009;49:2087–107. doi: 10.1002/hep.22853. [DOI] [PubMed] [Google Scholar]
- 4.Riley TR, Smith JP. Preventive care in chronic liver disease. J Gen Intern Med. 1999;14:699–704. doi: 10.1046/j.1525-1497.1999.11188.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Volk ML, Piette JD, Singal AS, et al. Chronic disease management for patients with cirrhosis. Gastroenterology. 2010;139:14–6. e1. doi: 10.1053/j.gastro.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.CHCF. Chronic Disease Care 2009 [cited; Available from: http://www.chcf.org.
- 7.Bodenheimer T, Lorig K, Holman H, et al. Patient self-management of chronic disease in primary care. JAMA. 2002;288:2469–75. doi: 10.1001/jama.288.19.2469. [DOI] [PubMed] [Google Scholar]
- 8.Singal AG, Volk ML, Rakoski MO, et al. Patient Involvement in Healthcare is Associated With Higher Rates of Surveillance for Hepatocellular Carcinoma. J Clin Gastroenterol. 2011;45:727–32. doi: 10.1097/MCG.0b013e31820989d3. [DOI] [PubMed] [Google Scholar]
- 9.Just-in-time teaching : across the disciplines, across the academy. 1st ed. Stylus Pub.; Sterling, Va.: 2010. [Google Scholar]
- 10.USA-Today [December 12, 2011];Too much acetaminophen over time can damage liver. http://yourlife.usatoday.com/health/story/2011-11-23/Too-much-acetaminophen-over-time-may-damage-liver/51369772/1. 2011; Available from: http://yourlife.usatoday.com/health/story/2011-11-23/Too-much-acetaminophen-over-time-may-damage-liver/51369772/1.
- 11.Chandok N, Watt KD. Pain management in the cirrhotic patient: the clinical challenge. Mayo Clin Proc. 2010;85:451–8. doi: 10.4065/mcp.2009.0534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.FDA [December 12, 2011];Controlling cholesterol with statins. http://www.fda.gov/ForConsumers/ConsumerUpdates/ucm048496.htm#StateoftheStatins. 2011; Available from: http://www.fda.gov/ForConsumers/ConsumerUpdates/ucm048496.htm#StateoftheStatins.
- 13.Calderon RM, Cubeddu LX, Goldberg RB, et al. Statins in the treatment of dyslipidemia in the presence of elevated liver aminotransferase levels: a therapeutic dilemma. Mayo Clin Proc. 2010;85:349–56. doi: 10.4065/mcp.2009.0365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lewis JH, Mortensen ME, Zweig S, et al. Efficacy and safety of high-dose pravastatin in hypercholesterolemic patients with well-compensated chronic liver disease: Results of a prospective, randomized, double-blind, placebo-controlled, multicenter trial. Hepatology. 2007;46:1453–63. doi: 10.1002/hep.21848. [DOI] [PubMed] [Google Scholar]
- 15.Bajaj JS, Hafeezullah M, Hoffmann RG, et al. Minimal hepatic encephalopathy: a vehicle for accidents and traffic violations. Am J Gastroenterol. 2007;102:1903–9. doi: 10.1111/j.1572-0241.2007.01424.x. [DOI] [PubMed] [Google Scholar]
- 16.Bajaj JS, Hafeezullah M, Hoffmann RG, et al. Navigation skill impairment: Another dimension of the driving difficulties in minimal hepatic encephalopathy. Hepatology. 2008;47:596–604. doi: 10.1002/hep.22032. [DOI] [PubMed] [Google Scholar]
- 17.Devins GM, Mendelssohn DC, Barre PE, et al. Predialysis psychoeducational intervention extends survival in CKD: a 20-year follow-up. Am J Kidney Dis. 2005;46:1088–98. doi: 10.1053/j.ajkd.2005.08.017. [DOI] [PubMed] [Google Scholar]
- 18.Rakoski MO, McCammon RJ, Piette JD, et al. Burden of cirrhosis on older americans and their families: Analysis of the health and retirement study. Hepatology. 2011 doi: 10.1002/hep.24616. [DOI] [PMC free article] [PubMed] [Google Scholar]